Crestpark Helena, LLC
Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Crestpark Helena, LLC has a Trust Grade of C+, indicating it is slightly above average among nursing homes. It ranks #103 out of 218 facilities in Arkansas, placing it in the top half of the state. The facility has shown improvement recently, with issues decreasing from 8 in 2023 to 7 in 2024. Staffing is a strong point, with a 5-star rating and only a 23% turnover rate, significantly lower than the state average. However, there are concerns, such as $8,193 in fines, which is average but still indicates some compliance issues. Additionally, reports highlighted specific problems, including dietary staff failing to wash hands during meal preparation, non-functional call lights in bathrooms, and maintenance issues affecting residents’ living conditions. While staffing and overall care show promise, families should consider these weaknesses when researching this facility.
- Trust Score
- C+
- In Arkansas
- #103/218
- Safety Record
- Low Risk
- Inspections
- Getting Better
- Staff Stability ✓ Good
- 23% annual turnover. Excellent stability, 25 points below Arkansas's 48% average. Staff who stay learn residents' needs.
- Penalties ✓ Good
- $8,193 in fines. Lower than most Arkansas facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 40 minutes of Registered Nurse (RN) attention daily — about average for Arkansas. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 25 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Staffing Rating · Excellent nurse staffing levels
-
Low Staff Turnover (23%) · Staff stability means consistent care
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover is low (23%)
25 points below Arkansas average of 48%
Facility shows strength in staffing levels, staff retention, fire safety.
The Bad
Near Arkansas average (3.1)
Meets federal standards, typical of most facilities
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 25 deficiencies on record
Jun 2024
7 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to ensure a comprehensive assessment was completed to provide the resident with the proper type of call light to accommodate the...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interviews, the facility failed to ensure the container used to store controlled substances was perman...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected multiple residents
2. Review of Resident #1's Care Plan revealed diagnoses of a seizure disorder, osteoporosis, and fracture of femur. The care plan had a Disease Diagnosis section that indicated the resident was at ris...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure the medication error rate was less than 5 percent (%) during the medication administration observation of 3 (Residents...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to ensure the facility remained free of a significant me...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
Based on observations and interviews, the facility failed (1) to ensure the ceiling was in good repair in 1 (Resident #9) resident's room, (2) to ensure the two sofas and a chair in the dayroom were i...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation and interview, the facility failed to ensure dietary staff performed hand hygiene during the preparation of a meal and during the meal service, and failed to ensure food was prope...
Read full inspector narrative →
Apr 2023
8 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure a resident's urinary catheter drainage bag was kept in a privacy bag to promote dignity for 1 (Resident #11) of 5 (Res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure resident's right to self-determination, as evidenced by the lack of accommodation of a resident's choice to be escorte...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, and interview, the facility failed to ensure medical devices were plugged into a properly grounded electri...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
Based on observation, and interview, the facility failed to adequately maintain and repair the resident call light system to ensure there was a functioning communication system between the residents a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, and interview, the facility failed to ensure the heating system was in good working order for 1 (room [ROO...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected multiple residents
Based on interview, and record review, the facility failed to develop and implement a Quality Assurance Performance Improvement (QAPI) Plan to include identification of problems, implementation of cor...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, and interview, the facility failed to ensure resident personal care equipment was properly cleaned and sto...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, and interview, the facility failed to ensure personal hygiene items were stored in a sanitary manner for 4...
Read full inspector narrative →
Nov 2022
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure a bathroom light was maintained and functioned to provide adequate lighting for one restroom utilized by two residents. The findings a...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation and interview the facility failed to ensure that medications were placed in a secure location to prevent residents from accidentally ingesting them which could cause a potential a...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected most or all residents
Based on observation, and interview the facility failed to ensure call lights were maintained and functioning to meet the needs of residents who required assistance and to aid in prevention of possibl...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected most or all residents
Based on observation and interview the facility failed to ensure a safe, functional, sanitary, and comfortable environment for residents and staff and failed to ensure maintenance services were provid...
Read full inspector narrative →
Jan 2022
6 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure a Level I Pre-admission Screening and Resident Review (PASRR...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to ensure broken glass was removed from a glass-encased fire extinguisher on the wall near 1 (Station 1 Hall) of 3 halls (Station 1, 2 and 3 Hal...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected multiple residents
Based on observation, record review and interview, the facility failed to ensure sufficient fluid intake was provided in accordance with physician orders to maintain proper hydration for 1 (Resident #...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, record review and interview, the facility failed to ensure proper infection prevention and control practices were implemented to prevent potential development and transmission of...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to ensure 2 of 2 clothes dryers remained free of lint build-up to decrease the potential for fire and loss of laundry services for 1 of 1 laundr...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected most or all residents
Based on observation and interview, the facility failed to ensure trash was properly contained within 3 of 3 trash dumpsters, to minimize the presence of foul odors and decrease the potential for pest...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 23% annual turnover. Excellent stability, 25 points below Arkansas's 48% average. Staff who stay learn residents' needs.
- • 25 deficiencies on record. Higher than average. Multiple issues found across inspections.
About This Facility
What is Crestpark Helena, Llc's CMS Rating?
CMS assigns Crestpark Helena, LLC an overall rating of 3 out of 5 stars, which is considered average nationally. Within Arkansas, this rating places the facility higher than 0% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Crestpark Helena, Llc Staffed?
CMS rates Crestpark Helena, LLC's staffing level at 5 out of 5 stars, which is much above average compared to other nursing homes. Staff turnover is 23%, compared to the Arkansas average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Crestpark Helena, Llc?
State health inspectors documented 25 deficiencies at Crestpark Helena, LLC during 2022 to 2024. These included: 25 with potential for harm.
Who Owns and Operates Crestpark Helena, Llc?
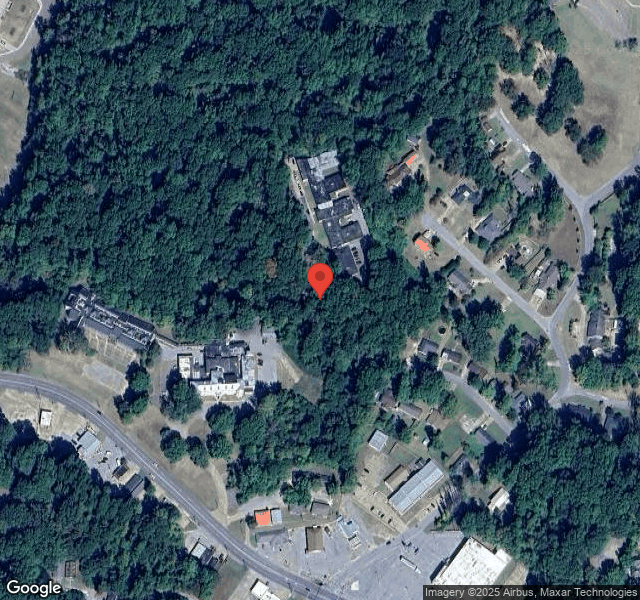
Crestpark Helena, LLC is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by CRESTPARK, a chain that manages multiple nursing homes. With 100 certified beds and approximately 36 residents (about 36% occupancy), it is a mid-sized facility located in HELENA, Arkansas.
How Does Crestpark Helena, Llc Compare to Other Arkansas Nursing Homes?
Compared to the 100 nursing homes in Arkansas, Crestpark Helena, LLC's overall rating (3 stars) is below the state average of 3.1, staff turnover (23%) is significantly lower than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Crestpark Helena, Llc?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Crestpark Helena, Llc Safe?
Based on CMS inspection data, Crestpark Helena, LLC has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #100 of 100 nursing homes in Arkansas. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Crestpark Helena, Llc Stick Around?
Staff at Crestpark Helena, LLC tend to stick around. With a turnover rate of 23%, the facility is 22 percentage points below the Arkansas average of 46%. Low turnover is a positive sign. It means caregivers have time to learn each resident's needs, medications, and personal preferences. Consistent staff also notice subtle changes in a resident's condition more quickly.
Was Crestpark Helena, Llc Ever Fined?
Crestpark Helena, LLC has been fined $8,193 across 1 penalty action. This is below the Arkansas average of $33,161. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Crestpark Helena, Llc on Any Federal Watch List?
Crestpark Helena, LLC is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.