WINDSOR SKYLINE CARE CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Windsor Skyline Care Center has received a Trust Grade of F, indicating significant concerns about the quality of care provided. It ranks #727 out of 1,155 facilities in California, placing it in the bottom half of nursing homes statewide, and #13 out of 14 in Monterey County, meaning only one local option is better. The facility is worsening, with the number of issues increasing from 2 in 2024 to 8 in 2025. Staffing is a relative strength, rated 4 out of 5 stars with a turnover rate of 31%, which is below the California average. However, the $63,850 in fines is concerning, as it is higher than 88% of California facilities, suggesting ongoing compliance problems. Additionally, there have been alarming incidents, including a critical failure where a resident at risk of elopement left the facility unnoticed and was later found unresponsive, leading to their death. Concerns have also been raised about food safety, with reports of unsanitary conditions in the kitchen that could lead to foodborne illnesses for residents. While the staffing levels are commendable, the serious issues regarding resident safety and sanitation cannot be overlooked.
- Trust Score
- F
- In California
- #727/1155
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ○ Average
- 31% turnover. Near California's 48% average. Typical for the industry.
- Penalties ✓ Good
- $63,850 in fines. Lower than most California facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 20 minutes of Registered Nurse (RN) attention daily — below average for California. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 41 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (31%)
17 points below California average of 48%
Facility shows strength in staffing levels, quality measures, fire safety.
The Bad
Near California average (3.1)
Meets federal standards, typical of most facilities
15pts below California avg (46%)
Typical for the industry
Above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 41 deficiencies on record
Apr 2025
1 deficiency
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide supervision for one of 14 residents (Resident 1) who was at...
Read full inspector narrative →
Mar 2025
7 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure dignity and privacy was upheld for two of four sampled residents (Resident 121 and Resident 226 ) when Resident 121 and...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on observation, interview, and policy review, the facility failed to protect resident's rights to confidentiality of protected health information (PHI, any information in the medical record that...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure the PASARR (a federal requirement to help ensure that indivi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure controlled medications (those with high potential for abuse and addiction) were fully accounted and given according to the physician...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to follow their policy and procedure (P&P) for proper labeling and storage of medications when food was stored on two of four me...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to implement infection control measures when:
1. Residen...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure sanitary conditions were maintained in the food and nutrition services when:
1. One plastic spatula (a kitchen utensi...
Read full inspector narrative →
Jan 2024
2 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
Based on observation, interview, and policy review, the facility failed to ensure that the facility environment remains free of accident hazards when the temperatures of hot water at the sinks of Room...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, interview, and policy review, the facility failed to implement infection control practices when:
1. Certified Nursing Assistant A (CNA A) placed soiled linen and towels on the re...
Read full inspector narrative →
Nov 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure the Notice of Medicare Non-Coverage (NOMNC, notice informing...
Read full inspector narrative →
Jul 2023
16 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based an interview, and record review, the facility failed to ensure the dignity of one of 17 sampled residents (Resident 317), when certified nursing assistant G (CNA G) did not use proper technique ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of 17 sampled residents (Resident 35) had been informed about having an advance directive (legal form directing their wishes abo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure 1. one of 17 sampled residents (Resident 35) or their responsible party (RP, person who is accountable in making decision on behalf ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to accurately complete the Minimum Data Set (MDS, an assessment tool) ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Review of Resident 20's clinical records indicated, he was admitted to the facility on [DATE], with diagnoses including hemip...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide activities for one of 17 sampled residents (R...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0740
(Tag F0740)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to monitor, evaluate and managed residents behavior for ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure controlled medications (those with high potential for abuse and addiction) were fully accounted and given according to the physician...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure the medication regimen for one of 17 sampled residents (Resident 57) was free from unnecessary medications. Resident 57 had been rec...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure one of 17 sampled residents (Resident 35) was free from unne...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected 1 resident
Based on observation, interview, and document review, the facility failed to ensure refuse (any disposable materials, which includes recyclable and non-recyclable materials) was stored properly when o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, licensed vocational nurse A (LVN A) failed to perform hand hygiene during wo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure the temperature (temp) in one of two medication refrigerators (Ref #2) was maintained within acceptable range from 36 ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure food palatability was maintained, when six of 1...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and document review, the facility failed to ensure food was stored and/or prepared under sanitary conditions when:
1. There was a crusty white substance on several are...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure their pest control program was effective when there were several fruit flies (small flying insects that have the poten...
Read full inspector narrative →
Jul 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and review, the facility failed to ensure one of three sampled residents (Resident 1) was protected from misa...
Read full inspector narrative →
Mar 2023
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to maintain the water circulating system in safe operating condition for 60 of 60 residents in the facility. This failure result...
Read full inspector narrative →
Jun 2019
12 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to promote resident's dignity when three certified nursing assistants (CNAs) were standing while assisting with meals for four of eight resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure two of three sampled residents (Residents 25 and 44) dischar...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. A review of the clinical record for Resident 9, the admission Record dated 6/26/19 indicated Resident 9 was admitted on [DATE...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0694
(Tag F0694)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure care of an intravenous (IV, within a vein) sit...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure dialysis (the clinical purification of blood as a substitute...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure adequate indication, behavioral and adverse/side-effects mon...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure that the Alprazolam (anti-anxiety) for one of 20 sampled residents (Resident 122) was limited to 14 days, which had the potential to...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure: 1) resident medications were sufficiently labeled; 2) unused narcotics were disposed of; and 3) discontinued narcotic...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0810
(Tag F0810)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to provide plateguard (stainless steel food guard to secure food spill) during lunch meal for one of seven residents (Resident 61...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to implement infection control practices when used lancets (a spring-loaded device that contains a needle) were stored in an unl...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2) A review of Resident 19's clinical record indicated he was admitted on [DATE] with diagnoses including repeated falls, muscle...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to store, prepare, and distribute food safely when:
1. refrigerator #1 had torn, dirty gaskets and racks with peeling coating a...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 31% turnover. Below California's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: 1 life-threatening violation(s), $63,850 in fines. Review inspection reports carefully.
- • 41 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $63,850 in fines. Extremely high, among the most fined facilities in California. Major compliance failures.
- • Grade F (38/100). Below average facility with significant concerns.
About This Facility
What is Windsor Skyline's CMS Rating?
CMS assigns WINDSOR SKYLINE CARE CENTER an overall rating of 3 out of 5 stars, which is considered average nationally. Within California, this rating places the facility higher than 0% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Windsor Skyline Staffed?
CMS rates WINDSOR SKYLINE CARE CENTER's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 31%, compared to the California average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Windsor Skyline?
State health inspectors documented 41 deficiencies at WINDSOR SKYLINE CARE CENTER during 2019 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death) and 40 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
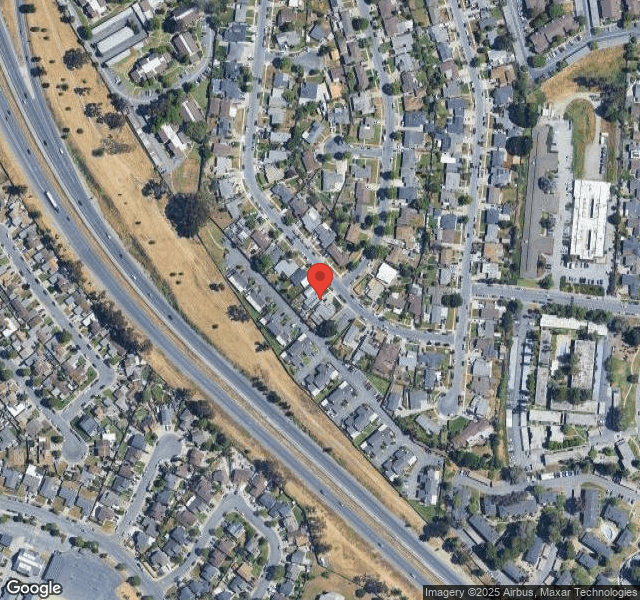
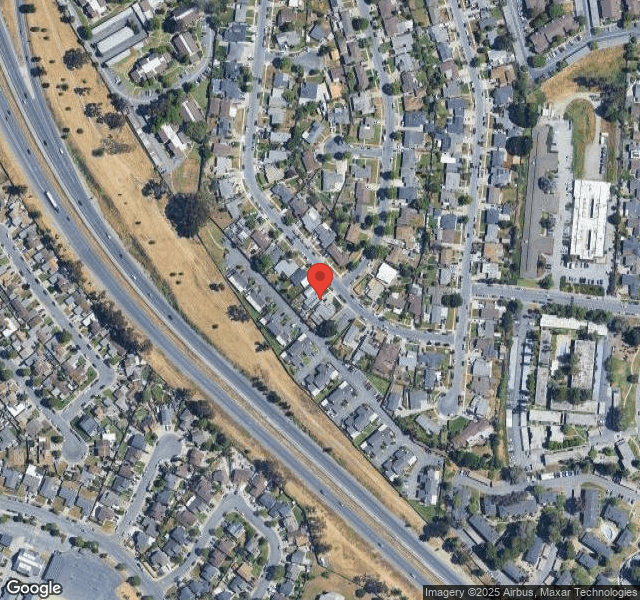
Who Owns and Operates Windsor Skyline?
WINDSOR SKYLINE CARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by WINDSOR, a chain that manages multiple nursing homes. With 80 certified beds and approximately 72 residents (about 90% occupancy), it is a smaller facility located in SALINAS, California.
How Does Windsor Skyline Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, WINDSOR SKYLINE CARE CENTER's overall rating (3 stars) is below the state average of 3.1, staff turnover (31%) is significantly lower than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Windsor Skyline?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's Immediate Jeopardy citations.
Is Windsor Skyline Safe?
Based on CMS inspection data, WINDSOR SKYLINE CARE CENTER has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 3-star overall rating and ranks #100 of 100 nursing homes in California. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Windsor Skyline Stick Around?
WINDSOR SKYLINE CARE CENTER has a staff turnover rate of 31%, which is about average for California nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Windsor Skyline Ever Fined?
WINDSOR SKYLINE CARE CENTER has been fined $63,850 across 1 penalty action. This is above the California average of $33,717. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Windsor Skyline on Any Federal Watch List?
WINDSOR SKYLINE CARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.