GOLDEN SAN ANDREAS CARE CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Golden San Andreas Care Center has received a Trust Grade of F, indicating significant concerns about the quality of care provided. Ranking #1031 out of 1155 facilities in California places it in the bottom half, although it is the only option in Calaveras County. The facility is showing signs of improvement, with issues decreasing from 36 to 21 over the past year. Staffing is average with a 3-star rating, but the 50% turnover rate is concerning compared to the state average of 38%. Serious incidents have been reported, including a failure to protect a resident from sexual abuse and inadequate care leading to pressure ulcers and falls, which resulted in injuries. While there are some improvements in trends, families should be aware of the significant challenges this facility faces.
- Trust Score
- F
- In California
- #1031/1155
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 50% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $99,362 in fines. Lower than most California facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 27 minutes of Registered Nurse (RN) attention daily — below average for California. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 90 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below California average (3.1)
Significant quality concerns identified by CMS
Near California avg (46%)
Higher turnover may affect care consistency
Well above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 90 deficiencies on record
Jul 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview, and record review, the facility failed to ensure treatment and care was provided in accordance with professional standards of practice for two of three sampled residents (Resident ...
Read full inspector narrative →
May 2025
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0678
(Tag F0678)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that nursing staff followed established protocols for the in...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure that adequate supervision and safety interventions were implemented for one out of three residents (Resident 3) when Resident 2 grab...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to maintain a complete and accurate medical record for one of three sampled residents (Resident 1) when, Resident 1's Activity of Daily Living...
Read full inspector narrative →
May 2025
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure two of three sampled residents (Resident 1 and Resident 2) received care to prevent the development of pressure ulcers...
Read full inspector narrative →
Feb 2025
15 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to accommodate the needs of 3 of 25 sampled residents (Resident 16, Resident 58, and Resident 83) when:
1.
Resident 16's call l...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure one of three residents (Resident 91) sampled for a closed r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure proper hydration (process of providing fluid to the body) for 1 of 25 sampled residents (Resident 16) per facility pol...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure respiratory care was provided in accordance with professional standards of practice for 2 of 19 residents when:
1. Oxy...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure 1 of 25 sampled residents (Resident 3) was pro...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure 2 of 25 sampled residents' (Resident 3 and Res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to maintain a closed garbage dumpster bin.
This failure had the potential to lead to insect and rodent (mice and rats) infestati...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on interview, and record review, the facility failed to maintain complete and accurate medical records for 2 of 25 sampled residents (Resident 43 and Resident 77) when:
1. Protected Health Infor...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure 1 of 25 sampled residents (Resident 75) was offered the Pne...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to maintain kitchen equipment for 89 residents who received food from the kitchen when the steamer (small appliance that cooks f...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure 7 of 25 sampled residents (Resident 56, Resident 69, Reside...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to develop and implement care plans (a list of resident ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure food from the kitchen was prepared and served to meet the needs of 3 out of 13 Residents (Resident 8, Resident 42, and...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to provide safe food storage and preparation, as well as maintain kitchen equipment and food contact surfaces in accordance with...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to maintain its infection prevention and control program, for a census of 89 residents, when:
1. Physical therapy assistant (PTA...
Read full inspector narrative →
Jan 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on interview, and record review, the facility failed to ensure one of four sampled residents (Resident 1) remained free of accidents and hazards when Certified Nursing Assistant (CNA) 1 gave Res...
Read full inspector narrative →
Oct 2024
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one of five sampled residents (Resident 1) rec...
Read full inspector narrative →
Mar 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to protect the rights of Resident 3 to be free from physical abuse, wh...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure professional standards were met when Licensed Nurse (LN2) left refused medications scheduled for the morning administration at Resid...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide an environment free of accident hazards for o...
Read full inspector narrative →
Feb 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure professional standards of care were met for Resident 1, when neurological checks (neuro checks, assessment of nerve and motor respon...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure fall prevention measures were implemented according to the plan of care for Resident 1, when Resident 1 ' s anti-slip ...
Read full inspector narrative →
Jan 2024
30 deficiencies
1 IJ
CRITICAL
(J)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
Based on interview and record review, the facility failed to protect the right of Resident 45, 1 of 25 female residents in the facility with a diagnosis of dementia (impaired ability to remember or ma...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0688
(Tag F0688)
A resident was harmed · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide the necessary care and services to ensure that two of twenty-one sampled residents (Resident 64 and Resident 49) func...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation and interview the facility failed to ensure 2 of 21 sampled residents (Resident 6 and Resident 67) needs were accommodated when their call lights were not in reach.
These failures...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to report a change of condition (COC, a change in the residents normal physical, mental, or behavioral state) to the responsible party (RP) and...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to provide one of three sampled Residents (Resident 273) a Notice of Me...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure one of three sampled residents' (Resident 273) discharge inf...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to issue a transfer/discharge notice for one of three closed record re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure the Pre-admission Screening and Resident Review (PASARR- a federal requirement to screen all potential nursing home residents for me...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to develop and/or implement a person-centered care plan for 3 of 21 sampled residents (Resident 10, Resident 44, and Resident 49...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure neurological checks (neuro checks, assessing mental status, pupil response, strength, and sensation) were completed for one of three...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure interventions were in place for the prevention of pressure ulcers (PU, areas of damaged skin typically caused by stayi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to implement interventions to prevent falls and accidents for 1 of 21 sampled residents (Resident 45) when:
1. Resident 45's bed...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure respiratory care was provided in accordance with professional standards of practice for 2 of 16 residents (Resident 5 a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to complete annual performance evaluations for 2 of 3 sampled nursing assistants when Certified Nurse Assistant (CNA) 3 and CNA 4 did not have ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one out of ten residents (Resident 30) on anti-psychotic medication had an appropriate diagnosis obtained by a comprehensive assessm...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0800
(Tag F0800)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide the correct portion size for one of five residents (Resident 12) during dinner tray line on 1/23/24, when Resident 12...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facilty failed to implement an antibiotic stewardship program and monitor antibiotic use when 1 of 21 sampled residents (Resident 14) received an antibiotic w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure residents received vaccine education and residents were offe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to ensure one of five sampled residents (resident 30) received education regarding the COVID-19 vaccine when Resident 30's clinical record did ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview the facility failed to ensure equipment utilized by residents received preventative maintenan...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility did not implement its abuse program for 1 of 21 sampled residents (Resident 45) when Resident 45 was involved in sexual interactions wi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility did not implement its abuse program for 1 of 21 sampled residents (Resident 45) when Resident 45 was subjected to sexual interactions w...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
Based on interview and record review the facility failed to consistently complete Interdisciplinary Team (IDT, care team consisting of different disciplines who assess and coordinate care) care plan c...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure professional standards of quality were met when:
1. One of five sampled residents' (Resident 15) medical record was ma...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on interview and record review the facility failed to provide adequate and sufficient nursing staff to ensure the Restorative Nursing Aide program (RNA, nursing aide who helps residents to maint...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure narcotic medication patches were disposed of and accounted for appropriately, non-narcotic medications were disposed o...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure a medication rate of less than 5 % when 5 of 33 opportunities resulted in an error rate of 15.15 % as follows:
1. A me...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure medications were labeled and stored appropriately when:
1. The facility did not ensure consistent temperature monitori...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure safe food production when:
1. Multiple food items were found not labeled with a use by date in the refrigerator, freez...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the failed to maintain and implement its infection protection and control pr...
Read full inspector narrative →
Dec 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure a safe environment free of accidents and hazards when:
1 of 16 residents at risk for falls did not have all the requir...
Read full inspector narrative →
Nov 2023
2 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure quality care was provided to one of three sampled residents (...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to evaluate resident specific risk factors and changes in health condit...
Read full inspector narrative →
Oct 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to implement person centered care planned interventions including the use of a seat belt alarm and sensory blanket to prevent ac...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to consistently implement care planned interventions including the use of a wheelchair seatbelt alarm and a sensory lap blanket ...
Read full inspector narrative →
Sept 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure one of three sampled residents (Resident 1), who was assessed at a high risk for falls due to a history of falls, rece...
Read full inspector narrative →
Sept 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interviews and record reviews the facility failed to provide two of two sampled residents (Resident 1 and 2) with quality care in accordance with professional standards when:
1. Staff did not...
Read full inspector narrative →
Apr 2023
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure the cigarettes and lighters of three of six sam...
Read full inspector narrative →
Mar 2023
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that one of two sampled residents (Resident 1) with a pressu...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure one of two sampled residents (Resident 3) was free from any ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Laboratory Services
(Tag F0770)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure laboratory services were available for a census of 69 and la...
Read full inspector narrative →
Feb 2023
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0692
(Tag F0692)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to maintain acceptable parameters of nutrition for one of three sample...
Read full inspector narrative →
Jun 2022
21 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure the needs were accommodated for one of 20 sampled residents (Resident 1) when Resident 1's hearing aids were not acces...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to implement a fall care plan to prevent falls for one of 20 sampled residents (Resident 1), when a fall risk care plan interven...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0661
(Tag F0661)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a discharge summary was completed for one of three sampled c...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow up medically related hearing evaluation for one of 20 sampled residents (Resident 36).
This failure had the potential to result in ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure one of twenty sampled residents (Resident 57) received restorative nursing services to provide range of motion (ROM; t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0691
(Tag F0691)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of one residents (Resident 14) who had a colostomy (an opening that connects the digestive tract to the surface of the belly to ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on interview, and record review, the facility failed to administer the prescribed antibiotics to Resident 36 for ten days with facility's census of 57.
This failure may have resulted in worsenin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility failed to maintain kitchen equipment when:
1. The stove lacked the bottom cover.
2. The steamer was not working properly.
3. The freezer ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0567
(Tag F0567)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure that petty cash was available for 11 of 15 residents (Resident 61, Resident 20, Resident 59, Resident 36, Resident 10, Resident 58, ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow their policy/procedure for Advance Directives (legal documen...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to complete four consecutive quarterly Interdisciplinary Team (IDT, a team of professional staff or a care team consisting of different discip...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
2.A review of Resident 49's admission Record indicated Resident 49 was admitted to the facility in early 2022 with multiple diagnoses including generalized muscle weakness, difficulty in walking, alte...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure respiratory care was provided in accordance wi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure safe medication monitoring for high risk medications (medications that may pose harm without monitoring) in four resid...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure safe medication storage and handling for a cen...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to provide safe food storage and preparation, in accordance with professional standards when:
1. Food preparation containers were...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. During an observation on 6/6/22, at 11:40 a.m. a visitor entered room [ROOM NUMBER]-2 without wearing an isolation gown, face...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected multiple residents
Based on interview and record review the facility failed to ensure that five of five sampled resident's medical records (Resident 40, Resident 64, Resident 6, Resident 16, and Resident 215) included d...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0583
(Tag F0583)
Minor procedural issue · This affected multiple residents
The facility failed to protect resident personal and medical information when dietary tray tickets were thrown into the general trash. This had the potential of personal information being seen by non-...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected most or all residents
Based on observation and interview the facility failed to ensure nurse staffing information (total number and the actual hours worked by licensed and unlicensed staff and the facility census) was post...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Safe Environment
(Tag F0921)
Minor procedural issue · This affected most or all residents
Based on observation, interview, and record review the facility failed to provide a safe environment for residents, staff and the public for a census of 57 when there was no oxygen in use signs posted...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 1 life-threatening violation(s), 6 harm violation(s), $99,362 in fines, Payment denial on record. Review inspection reports carefully.
- • 90 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $99,362 in fines. Extremely high, among the most fined facilities in California. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Golden San Andreas Care Center's CMS Rating?
CMS assigns GOLDEN SAN ANDREAS CARE CENTER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within California, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Golden San Andreas Care Center Staffed?
CMS rates GOLDEN SAN ANDREAS CARE CENTER's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 50%, compared to the California average of 46%. RN turnover specifically is 69%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Golden San Andreas Care Center?
State health inspectors documented 90 deficiencies at GOLDEN SAN ANDREAS CARE CENTER during 2022 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 6 that caused actual resident harm, 80 with potential for harm, and 3 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
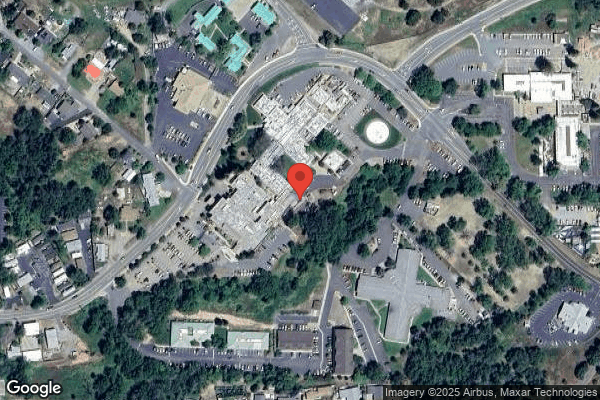
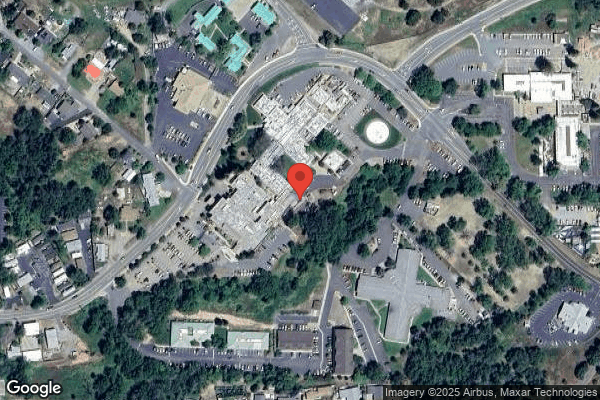
Who Owns and Operates Golden San Andreas Care Center?
GOLDEN SAN ANDREAS CARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by GOLDEN SNF OPERATIONS, a chain that manages multiple nursing homes. With 99 certified beds and approximately 87 residents (about 88% occupancy), it is a smaller facility located in SAN ANDREAS, California.
How Does Golden San Andreas Care Center Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, GOLDEN SAN ANDREAS CARE CENTER's overall rating (1 stars) is below the state average of 3.1, staff turnover (50%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Golden San Andreas Care Center?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's Immediate Jeopardy citations.
Is Golden San Andreas Care Center Safe?
Based on CMS inspection data, GOLDEN SAN ANDREAS CARE CENTER has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in California. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Golden San Andreas Care Center Stick Around?
GOLDEN SAN ANDREAS CARE CENTER has a staff turnover rate of 50%, which is about average for California nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Golden San Andreas Care Center Ever Fined?
GOLDEN SAN ANDREAS CARE CENTER has been fined $99,362 across 4 penalty actions. This is above the California average of $34,072. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Golden San Andreas Care Center on Any Federal Watch List?
GOLDEN SAN ANDREAS CARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.