CRITICAL
(J)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, the facility failed to keep residents safe from accident hazards related to elopement for...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, the facility failed to keep residents safe from accident hazards related to elopement for two (#43 and #10) of two residents reviewed out of 25 sample residents.
Specifically, the facility failed to keep residents safe from elopement with the potential for serious injury on two back-to-back occasions.
Resident #43 had severe dementia, was at risk for and had a history of elopement, and was discovered missing from the facility on 4/3/22 at 1:00 p.m. She had left the building at 9:35 a.m. and staff were unaware she was gone until they viewed camera footage more than four hours later. She was found by a neighbor and former staff member and returned by law enforcement to the facility at 3:35 p.m. She had been found sitting on the neighbor's front porch. Resident #43 was not injured. She had been missing for more than six hours.
The facility failed to immediately implement effective measures to keep residents at risk safe from elopement, causing a second resident to elope.
On both occasions, the facility's wander guard system failed to keep residents safe from elopement.
Resident #10 had severe dementia, was at risk for and had a history of elopement, and was discovered missing from the facility on 4/5/22 at 12:00 a.m. At 12:35 a.m., the manager on duty saw staff looking for something and when asked, they said they had not seen Resident #10 when they conducted midnight rounds. Camera footage revealed the resident left the building at approximately 8:00 p.m. via the chapel door. Law enforcement marked the resident as missing and sent out an alert at 3:40 a.m. on 4/5/22. The resident was not found until 7:55 a.m. the next day, on 4/5/22. He had been taken by a community member to a local hotel, spent the night there, and was found by law enforcement and escorted back to the facility at 8:30 a.m. He was not injured.
The facility's failure to take immediate action for residents identified for elopement created the likelihood of serious injury or death.
Findings include:
Record review and interviews confirmed the facility corrected the deficient practice prior to the onsite investigation on 9/12-9/15/22, resulting in the deficiency being cited as past noncompliance with a correction date of 4/5/22.
I. Immediate jeopardy for potential serious harm or death
A. Situation of Immediate Jeopardy
Resident #43 had severe dementia, was at risk for and had a history of elopement, and was discovered missing from the facility on 4/3/22 at 1:00 p.m. She had left the building at 9:35 a.m. and staff were unaware she was gone until they viewed camera footage more than four hours later. She was found by a neighbor and former staff member and returned by law enforcement to the facility at 3:35 p.m. She had been found sitting on the neighbor's front porch. Resident #43 was not injured. She had been missing for more than six hours.
The facility failed to immediately implement effective measures to keep residents at risk safe from elopement, causing a second resident to elope.
On both occasions, the facility's wander guard system failed to keep residents safe from elopement.
Resident #10 had severe dementia, was at risk for and had a history of elopement, and was discovered missing from the facility on 4/5/22 at 12:00 a.m. At 12:35 a.m., the manager on duty saw staff looking for something and when asked, they said they had not seen Resident #10 when they conducted midnight rounds. Camera footage revealed the resident left the building at approximately 8:00 p.m. via the chapel door. Law enforcement marked the resident as missing and sent out an alert at 3:40 a.m. on 4/5/22. The resident was not found until 7:55 a.m. the next day, on 4/5/22. He had been taken by a community member to a local hotel, spent the night there, and was found by law enforcement and escorted back to the facility at 8:30 a.m. He was not injured.
The facility's failure to take immediate action for residents identified for elopement created the likelihood of serious injury or death.
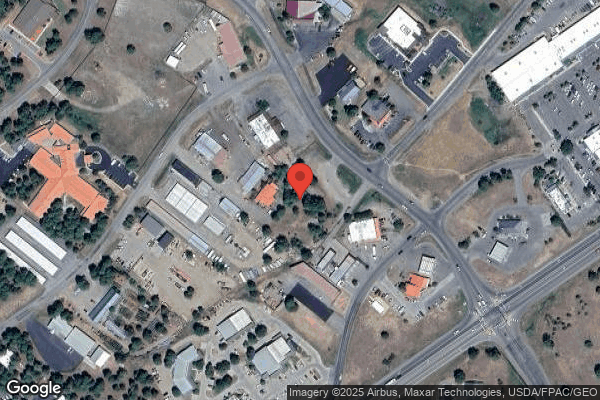
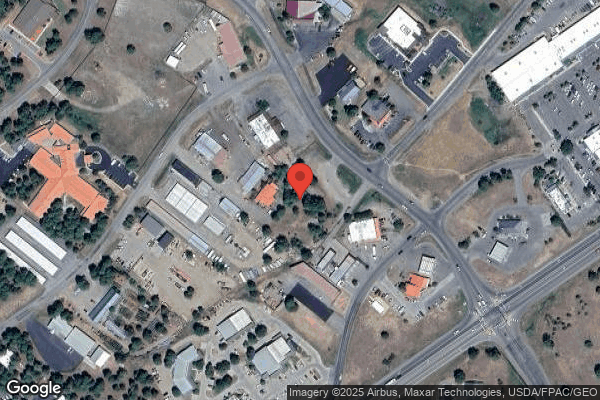
The nursing home administrator (NHA) was notified of the immediate jeopardy determination on 9/15/22 at 1:00 p.m. because serious adverse outcome was likely to occur in the case of both Residents #43 and #10 due to the delay in identifying they were missing, and how long they were missing. The facility was close to several busy streets. The residents could have been lost, injured or victimized due to their status as at-risk adults with severe dementia.
The facility was notified of the need to take immediate action to ensure residents who wandered or were at risk of elopement were supervised and their safety was ensured. The facility reported they took immediate action after the second resident elopement. The decision to cite at past non-compliance was pending the record of the facility's self-initiated plan of correction.
B. Facility plan to remove the Immediate Jeopardy situation
The facility submitted their Plan for Immediate Jeopardy Removal on 9/15/22 at 7:07 p.m., which read as follows:
1. Address how corrective action will be accomplished for those residents found to have been affected by the deficient practice.
The first incident on 4/3/22 was human error. The security door was not re-activated due to the 60 second wait time to re-activate. The second was also human error thinking only one resident was leaving not two, however they (staff) should have double checked outside.
Corrective action began April 4, 2022, after deficient practice. Upon notification, elopement of Resident #43 due to improper activation of alarm system.
Corrective action began April 5, 2022, when notified of deficient practice regarding the elopement of Resident #10 after failure to do a head count.
Immediate action/resident safety:
-When residents returned to the facility, they were immediately assessed (head to toe assessment). No injuries.
-Education completed 4/3 and 4/4 with staff to educate on alarm system, frequent checks and frequent resident monitoring.
-4/4/22 MDS (minimum data set) coordinator and administrator (NHA) looked at all residents to assess need for wander guard, updated care plans or other interventions due to occurrence.
-Frequent alarm checks were done to ensure the alarm was activated between 4/5 and 4/12/22. All staff were educated, and all staff were to check the alarm (to ensure it was red not green) and active. Sign off was next to the alarm to sign off checks. If activated, staff also signed off to re-activate the alarm. Sign-off sheets in occurrence binder.
-Increased monitoring of all wandering/elopement risk residents and documentation of interventions to deter wandering.
-Between 4/5 and 7/5/22 (even after wander guard system/double alarms on doors installed) resident head count completed on all residents if any door alarms active. Resident count sheets in occurrence binder.
2. Address how the facility will identify other residents have the potential to be affected.
Facility identifies residents who are an elopement/wander risk have the potential to be affected by same deficient practice.
3. Address what measures will be put into place or systemic change made to ensure that the deficient practice will not reoccur.
Measures put into place are that re-education of staff was started the evening of 4/3/22 regarding the activation of the alarm system - education of alarm system also completed. Formal training began on 4/4/22 and implementation of checks of alarm system put into place and behavior monitoring of wandering residents and documentation. List of all wandering residents provided to nursing staff so they can be identified if not already known. Following second incident on 4/4/22, on the morning of 4/5/22 an additional intervention was implemented. Further education of staff regarding alarm system, following resident to the door, and implementation of head count of all residents following alarm activation was started. On 4/5/22 and after multiple attempts to reach (security company name) alarm system activation time was decreased from 60 seconds to 15 seconds on 4/12/22. On 4/6/22 call placed to (technology company name) to initiate purchase for wander management system (wander guard system for all fire doors). On 4/8/22 (brand name) Airtags were ordered for GPS tracking of residents. Tracking policy created 5/5/22 for approval by (facility corporation). On 6/10/22 GPS tracking was implemented on four residents to include Residents #43 and #10.
4. Indicate how the facility plans to monitor its performance to make sure that solutions are sustained. The facility must develop a plan for ensuring that correction is achieved and sustained. This plan must be implemented and the corrective action evaluated for its effectiveness. The plan of correction must be integrated into the quality assurance system. The correction date will be the latest completion day on your accepted plan of correction.
a. The facility shall monitor its performance by having the Administrator and/or Director of Nursing and/or designee monitor alarm system to ensure employees are activating the system and checks are being done to ensure system is activated. Check off sheet created 4/4/22 with implementation.
b. On 4/4/22 at 11:56 a.m., contacted (security company name) to change the time to re-arm security system. A second call was placed on 4/5/22 as call had not yet been returned. Activation from 60 seconds to 15 seconds with implementation of text with picture to Administrator phone on 4/12/22 any time an alarm is activated. This will not stop.
c. All residents with the potential to wander (those with wander guard) have behavior monitoring (per policy and procedure) to monitor number of times exit seeking per day. Attempts will be documented daily (if necessary) and redirection of resident and frequent checks, interventions documented in notes.
d. Staff educated on Missing Person/Elopement Drill (Policy 1-6.13) for review 4/4/22 or when coming on to shift.
e. Re-education on use of alarm system completed for employees (employees know there is a 60 second wait time).
f. Head count of residents when alarm system activated implemented 4/5/22, documentation in med room and reviewed by Administrator, Director of Nursing and/or designee.
g. On 4/6/22 quote and purchase of wander guard system initiated for all fire doors (doors without current wander guard system). Pending installation (June 22, 2022 completion date).
h. (Brand name) Airtag trackers ordered 4/8/22 for GPS tracking of high-risk elopement residents and received.
i. GPS tracking of residents was implemented on 6/10/22 on all high-risk wander/elopement residents per policy. They will be monitored by nursing, DON (director of nursing) and Administrator. Tracking will be on Administrator phone and only used when necessary and checked per policy.
5. Include dates when the corrective action will be completed. The corrective action unacceptable for any reason you will be notified by this office. If the plan of correction is ultimately accountable for compliance and that responsibility is not alleviated in cases where notification regarding the acceptability of the facility plan of correction is not made timely.
Completion date 7/5/2022.
6. Interventions still in place:
All security doors (all 7 doors in facility) are always alarmed. Once all staff were educated on 4/4 and 4/5 with the following plans and interventions to include: staff education on the alarm system, staff must wait the 60 seconds to re-arm all doors to re-activate the security doors, staff must frequently check the alarm to ensure the security system is activated, resident monitoring was increased (especially those who were high-wander risk), those residents were offered distraction - direction and more to do to keep them from wandering and on 4/5/22 staff were required to count ALL residents any time an alarm was activated,. These were monitored by Administrator, DON and supervisor staff who assisted in monitoring of counting residents, and the sign off on the alarm system and doors/alarms in proper working order. On 4/5/22 the facility was in compliance.
-All doors have double alarms - fire activations with 15 second re-set (since 4/12/22)
-Administrator receives text with picture whenever alarm is activated/re-activated (since 4/12/22)
-GPS (global positioning system) tracking on high-risk residents in place (since 6/10/22)
-Continue to provide re-direction, frequent checks and diversion for wandering residents
-QA (quality assurance) and QAPI (quality assurance process improvement) done.
C. Removal of Immediate Jeopardy
Upon follow-up interviews with the NHA and corporate maintenance (CM) staff and review of door alarm and wander guard monitoring documentation, it was determined the facility had removed the immediacy of the IJ situation on 4/5/22. Documentation of weekly monitoring and testing of the door alarm system and individual residents' wander guards was reviewed. Upon review of the facility's plan of correction and implemented measures to keep facility residents safe, it was determined that the facility failures and corrective actions constituted immediate jeopardy past non-compliance. The facility's correction plan was reviewed and approved as of 7:15 p.m. on 9/15/22. Therefore, the deficient practice was corrected prior to the recertification survey and represented past noncompliance at D level, potential harm that was isolated.
II. Failure to ensure residents were safe from elopement
A. Resident status
1. Resident #43, age [AGE], was admitted on [DATE]. According to the September 2022 computerized physician orders (CPO), diagnoses included Alzheimer's disease, dementia with behavioral disturbance, tremor unspecified, depressive episodes, insomnia, and anxiety disorder.
The 8/24/22 minimum data set (MDS) assessment documented severe dementia with a brief interview for mental status (BIMS) score of one out of 15. She had delirium symptoms of inattention and disorganized thinking, and mood symptoms of trouble sleeping and concentrating. She exhibited wandering behavior one to three days out of the review period, but the impact to the resident and others was not documented. She needed supervision, oversight, cueing or limited assistance for most activities of daily living (ADLs). She needed extensive assistance for toilet use and personal hygiene. She had unsteady balance and gait, and had a fall with injury since the last review period.
The 2/23/22 MDS assessment documented she exhibited wandering behavior daily, posing a significant risk to herself, and intruding on the privacy and activities of others. The 5/25/22 MDS documented wandering one to three days during the review period.
The care plan, initiated 4/4/22 (two months after the resident's MDS identified she wandered on a daily basis), identified wandering into unsafe situations, tendency to seek out exits of facility, attempts to leave facility have been made. The goal was close monitoring by staff and wandering would not contribute to injury. Interventions were: place resident in area where frequent observation is possible; provide diversional activities; place monitoring device on resident that sounds alarms when resident leaves building; note which exits resident favors for elopement from facility and alert staff working those areas; monitor and document target behaviors; implement facility protocol for locating an eloped resident; if wandering away from unit, instruct staff to stay with resident, converse and gently persuade to walk back to designated area with them; designate staff to account for resident whereabouts throughout the day; approach wandering resident in a positive, calm and accepting manner; and alert staff to wandering behavior.
-The care plan did not document that the resident had actually eloped from the building and was not found and returned home until more than six hours later.
2. Resident #10
Resident #10, age [AGE], was admitted on [DATE]. According to the September 2022 CPO, diagnoses included dementia with behavioral disturbance, heart disease, hypertension, type 2 diabetes and anxiety disorder.
His 6/29/22 MDS assessment documented severe cognitive impairment with a BIMS score of five out of 15. No behavioral symptoms including wandering were documented. He needed supervision/oversight or was independent for most ADLs. He was unsteady with transfers.
-Although his 6/29/22 MDS documented no wandering behavior, his prior MDS assessment on 3/30/22 documented wandering daily, posing a risk to the resident.
-The MDS assessments did not consistently document wandering behavior and/or risks.
The care plan, initiated 4/5/22 and not revised, identified wandering into unsafe situations. The goal was wandering would not contribute to injury. Interventions were: place resident in area where frequent observation is possible; provide diversional activities; place monitoring device on resident that sounds alarms when resident leaves building; note which exits resident favors for elopement from facility and alert staff working near those areas; monitor and document behaviors; implement facility protocol for locating an eloped resident; if wandering away from unit, instruct staff to stay with resident, converse and gently persuade to walk back to designated area with them; designate staff to account for resident whereabouts throughout the day; approach wandering resident in a positive, calm, and accepting manner; and alert staff to wandering behavior.
-The care plan did not document that the resident actually eloped from the building and was not found and returned home until 24 hours later.
B. Record review and interviews regarding resident elopements
1. Resident #43's elopement on Sunday, 4/3/22
The facility investigation regarding Resident #43 revealed she attempted to exit the 500 hallway door on 4/3/22 at 9:18 a.m. Staff successfully brought the resident back inside the door and deactivated the alarm. The staff walked away during the 60-second waiting period to reactivate, and did not reactivate the door alarm, leaving six of nine facility door alarms disengaged.
Camera footage revealed at 9:33 a.m. Resident #43 entered the dining room, exited the building and walked into the back staff parking lot at 9:35 a.m. She attempted to re-enter the building but could not get back in, and was seen on camera footage walking away from the facility towards a nearby street and out of the camera view.
At approximately 12:45 p.m. dining room staff noticed Resident #43's tray card was not pulled for lunch, prompting nursing staff to search the facility and grounds for Resident #43. A resident head count revealed Resident #43 was missing and all other residents were accounted for.
The manager on duty (MOD) was notified at 1:00 p.m. that Resident #43 was missing. The MOD reviewed camera footage and notified the nursing home administrator (NHA) at approximately 1:20 p.m. that Resident #43 was missing. A neighborhood search was initiated and community members and law enforcement were notified. Law enforcement located the resident, who had been sitting on a community member's front porch. Law enforcement and the community members returned Resident #43 to the facility at 3:35 p.m. Resident #43 was assessed to have no trauma or injuries.
At 4:30 p.m. the NHA educated staff regarding the alarm system, and not leaving doors unattended until they were reactivated.
2. Resident #10's elopement on Monday 4/4/22 until Tuesday 4/5/22
On 4/4/22 at 7:54 p.m. Resident #10 exited the facility via the chapel door according to video footage. Staff were unaware Resident #10 had left. Video footage reviewed later (see below) revealed Resident #10 and another resident were walking in the hall toward the chapel; the other resident returned from the chapel area but Resident #10 did not.
-There was no evidence in the investigative report that staff heard an alarm from the chapel door at that time.
At 12:35 a.m. on 4/5/22 a facility nurse noticed staff were looking for something, and when asked said they were unable to lay eyes on Resident #10 since 12:00 a.m. rounding. All staff looked in all rooms, cafeteria, common areas and hallways, then searched outside the property in a one-block radius, then viewed camera footage. The former director of nursing (DON) saw on camera footage that Resident #10 and another resident had walked toward the chapel (see above) and did not return to the hallway with the other resident. Per camera footage it was determined Resident #10 left the building at approximately 8:00 p.m. The NHA and local police were notified and the search for Resident #10 continued throughout the community. The resident's out-of-town family and police department were notified.
On 4/5/22 at 3:40 a.m. a local deputy advised that law enforcement had marked Resident #10 as missing and an alert was issued. At 5:00 a.m. the deputy called to advise the search continued and his supervisor possibly saw Resident #10 at 8:30 p.m. walking toward the north part of town so they would be focusing more in town for the search. The official alert went out at 6:06 a.m.
On 4/5/22 at 7:31 a.m. the NHA got a call stating a community member knew where Resident #10 was. He had walked into a local caregiver agency across the street from the facility at about 8:30 p.m. on 4/4/22 and said he was trying to get to a town in a nearby state but didn't have his car. The community members were going to give him a ride but soon realized Resident #10 did not know where he was going. They booked Resident #10 a hotel room on the other side of town and stated he should still be there. They named the hotel and the room number.
On 4/5/22 at 8:30 a.m. Resident #10 was escorted back to the facility accompanied by four deputies from the county sheriff's department. The resident was assessed to have no trauma or injuries.
III. Administrator interview and facility plan of correction
On the afternoon of 9/13/22, interview with the NHA and review of the facility's plan of correction revealed Resident #43 eloped due to improper activation of the alarm system and Resident #10 eloped and was missing overnight after staff failed to do a resident head count.
Measures implemented were:
-Staff re-education started the evening of 4/3/22 regarding operation and activation of the alarm system.
-Formal staff training began 4/4/22 and implementation of checks of alarm system put into place along with behavior monitoring of wandering residents and documentation. A list of wandering residents provided to nursing staff so they could be identified if not already known.
-Following the 4/4/22 incident, on the morning of 4/5/22 an additional intervention was implemented. Further education of staff regarding alarm system, following resident to the door, and implementation of head count of all residents following alarm activation was started.
-On 4/6/22 the alarm company was contacted regarding installation of wander guard system for all alarmed doors with only one door alarm. This would double alarm all facility doors. The exact date of installation was not yet known.
The NHA said during the 9/13/22 interview that all the facility doors had since been double-alarmed with security alarms and wander guard systems. Residents identified at risk for elopement wore wander guards, and residents who were at risk for elopement and exiting the facility grounds had additional GPS systems added to their wander guards.
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review the facility failed to ensure residents were free of abuse for six (#17, #45, #26, #28, #4...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review the facility failed to ensure residents were free of abuse for six (#17, #45, #26, #28, #41 and #16) of eight out of 25 sample residents.
Specifically, the facility failed to ensure:
-Residents #17 and #45 were free from verbal abuse from staff;
-Repeated resident-to-resident physical abuse incidents by Resident #16 directed toward other residents including Residents #26, #28 and Resident #41; and,
-Physical abuse by Resident #22 against Resident #16 on two occasions.
Cross-reference F610: failure to investigate an allegation of abuse.
Findings include:
I. Facility policy and procedure
The Resident Safety policy, no date of inception or revision, provided by the nursing home administrator (NHA) on 9/14/22 at 5:50 p.m. documented in part, it was the policy of the facility to maintain a work and living environment that was professional and free from threat and/or occurrence of harassment, abuse, (verbal, mental, or sexual), neglect, corporal punishment, involuntary seclusion and misappropriation of property. Making reasonable efforts to provide a safe environment for the residents was one of the most basic and essential duties of the facility. Employees have a unique position of trust with vulnerable residents. Having access to private information, being in a physically intrusive position and having elevated status and special relations with residents makes ethical and professional behavior essential. Our facility promotes an atmosphere of sharing with residents and staff without fear of retribution. Residents must not be subjected to abuse by anyone, including but not limited to, facility staff, other residents, consultants or volunteers, staff of other agencies serving the residents, family members or legal guardians, friends, or other individuals.
II. Resident #17 and #45 kept free from staff abuse
A. Resident #17
1. Resident status
Resident #17, age [AGE], was admitted on [DATE]. According to the September 2022 computerized physician orders (CPO) diagnoses included Meniere's disease (disorder of inner ear), difficulty in walking, and muscle weakness.
According to the 7/14/2022 minimum data set (MDS) the resident has 13 out of 15 on the brief interview for mental status exam indicating the resident was cognitively intact.
2. Resident interview
Resident #17 was interviewed on 9/12/2022 at 2:47 p.m. He said a certified nurse aide (CNA) at the facility was mean to him purposefully (referring to CNA #3). He said he had chronic pain in his legs since losing the ability to walk, and when she would come in and change his brief she would purposefully push on his legs to cause him pain and discomfort. He said he asked her not to push on his legs several times but she did anyway. He said the CNA would not knock on the door when she entered and would bark orders at him, and would call him crybaby and tell him she hated taking care of him.
Resident #17 said he had reported the CNA purposefully pushing on his legs and her name calling to a registered nurse (RN) at the facility a couple months ago, and nothing came of it because he later found out the RN was friends with the CNA. He said he continued to report these issues to staff and finally a few weeks ago the director of nursing (DON) came down to talk to him, and he thought that was about three weeks ago. He said he expressed his concerns to the DON at that time about the staff member and reported the issues with her pushing on his legs purposefully. He said the staff member was moved to day shift and now was getting more supervision from staff in an attempt he thought to salvage her because they could not afford to lose any staff. He said he was afraid the staff member would attempt to try to get even with him. He said the staff member despite being moved to a different shift would still come in his room, but with a second staff member now.
B. Resident #45
1. Resident status
Resident #45, age [AGE], was admitted on [DATE]. According to the September 2022 computerized physician orders (CPO) diagnosis included adult failure to thrive, chronic pain syndrome, and anxiety disorder.
According to the 5/25/22 minimum data set (MDS) the resident scored a 12 of 15 on the brief interview for mental status exam indicating the resident's cognition was moderately impaired.
2. Resident interview
Resident #45 was interviewed on 9/14/22 at 8:30 a.m. She said she did not like certified nurse aide (CNA) #3 because she was mean and rough (no specifics were given by the resident but the resident was tearful). She said she felt it did feel like abuse and she was afraid of the staff member. She said she had reported these concerns to the director of nursing (DON) and nursing home administrator (NHA) but nothing had been done about it.
C. NHA/DON notification
The NHA and DON were notified of the abuse allegations on 9/14/22 at 8:38 a.m. They said they were unaware of the abuse allegations by residents and would cancel/suspend CNA #3 and begin and investigation.
D. Record review
The facility investigation related to the allegations was provided by the NHA. It detailed as follows:
First known time following discussion with state surveyor who made DON and NHA aware of allegations of two residents (#17 and #45).
CNA #3 was immediately suspended upon being made aware of allegations until investigation was complete and a final decision was made.
9/14/22 at 8:47 a.m. Resident #45's interview with DON and NHA. Resident #45 was interviewed regarding CNA. The DON and NHA assured the resident actions would be taken and DON/NHA were not aware she was fearful of the CNA. Resident #45 stated, I didn't know I was afraid of her until this morning. I never expressed it. She signed her statement. She reiterated she's mean, it's her personality. Resident #45 reported she did not like the way she talked to her as she was impatient and did things quickly and she knew she did this to other residents. She said she had not seen it with other residents but a staff member had told her. Resident #45 stated, I want CNA #3 fired.
The facility entered the occurrence into the state system on 9/14/22 at 10:01 a.m. with two resident allegations of the CNA being impatient, gruff, and mean with one resident expressing fear of staff member.
Resident #17 was noted to be interviewed. There were no notes detailing the staff's interview with the resident.
The facility contacted local law enforcement with the allegations on 9/14/22 at 11:00 a.m. The deputy assigned had interviewed both residents (#17 and #45) on 9/14/22 at 1:00 p.m.
Resident #6 was interviewed on 9/14/22 at 1:54 p.m. and stated the staff were wonderful. He said he had a problem with a nurse in the past, but she apologized and has had no issues since. He reported no issues with CNAs and was not fearful of staff and felt safe in the facility.
RN #1 was interviewed on 9/14/22 at 2:13 p.m. and she stated a resident had told her in the past she did not like CNA #3. The RN stated the resident (unknown) was crying but did not report an allegation of abuse. The RN said CNA #3 could come off as abrasive and it was just her personality.
Resident #27 was interviewed on 9/14/22 at 2:30 p.m. by the social services director (SSD). The resident denied any complaints about staff.
A resident interviewed on 9/14/22 at 3:30 p.m. that was not listed in the sample reported I don't like the ugly aide, she is rude and hateful. She complains that I am hard to take care of. He reported he was not fearful of her but stated, fire that (expletive). The resident did not report concerns regarding any other staff.
CNA #4 was interviewed on 9/14/22 at 3:56 p.m. who worked partial nights with CNA #3. He had not heard of any complaints regarding CNA #3 or any other staff members.
Resident #4 was interviewed on 9/14/22 at 5:06 p.m. and had no concerns with staff.
This concluded the investigative summary provided by the facility.
E. Interviews
The NHA was interviewed on 9/15/2022 at 7:30 p.m. The NHA said she did follow up with Resident #17 and he let it all go, and he reported he was very upset from his interactions with CNA #3. The NHA said she was the abuse officer for the facility and she had substantiated verbal abuse for Resident #17 and #45 by CNA #3. She said she did not have enough in the course of her investigation to substantiate physical abuse for Resident #17. She said she confirmed the resident identifying the staff member as the ugly aide in the course of her investigation was CNA #3. She said she was pursuing termination for CNA #3.
III. Resident-to-resident abuse involving Residents #16, #22, #26, #28 and #41
A. Resident status
1. Resident #16, age [AGE], was admitted on [DATE]. According to the September 2022 CPO, diagnoses included dementia with behavioral disturbance, restlessness and agitation, generalized anxiety disorder and brain stem stroke syndrome. The 7/11/22 MDS assessment documented severe cognitive impairment with a BIMS score of three out of 15 and delirium symptoms involving inattention. No behavioral symptoms were documented. She needed extensive assistance with most activities of daily living (ADLs) and used a wheelchair for ambulation.
2. Resident #22, age [AGE], was admitted on [DATE]. September 2022 CPO diagnoses included dementia with behavioral disturbance and anxiety disorder. The 7/22/22 MDS assessment documented severe dementia with a BIMS score of three out of 15 and no behavioral symptoms. She needed limited assistance with most ADLs and used a wheelchair or walker for ambulation.
3. Resident #26, age [AGE], was admitted on [DATE]. The 7/25/22 MDS assessment included a diagnosis of dementia and documented moderate cognitive impairment with inattention and no BIMS score. She needed extensive assistance with most ADLs and used a wheelchair.
4. Resident #28, age [AGE], was admitted on [DATE]. The 7/29/22 MDS assessment included a dementia diagnosis and severe cognitive impairment with a BIMS score of four out of 15. One behavioral symptom, care rejection occurring óne to three days over the review period, was documented. She needed supervision and/or limited assistance for most ADLs and used a wheelchair.
5. Resident #41, age [AGE], was admitted on [DATE] with diagnoses including history of traumatic brain injury and convulsions. The 8/17/22 MDS assessment documented she was cognitively intact with a BIMS score of 15 out of 15 and no behavioral symptoms. She needed supervision/limited assistance or was independent with most ADLs and used a walker.
B. Physical abuse by Resident #16 against Resident #41
Resident #41 was interviewed on 9/13/22 at 9:00 a.m. She said another facility resident picks on me, pinches and scratches me. She named and described Resident #16, said she had received injuries from Resident #16 including a black spot on my arm, it had happened four times and she had reported it to her nurse. She said she was not afraid but she liked to stay in her room to avoid Resident #16, although she had to be in the dining room at the same time as her.
Review of progress notes and facility investigations for the past six months revealed on 5/2/22 Resident #26 grabbed Resident #41 by the arm when she was near her in the dining room, leaving red marks that turned into bruising.
Interviews with medical records, director of nursing (DON) and nursing home administrator (NHA) during late afternoon on 9/14/22 revealed none had heard the allegation this had occurred four times, or that Resident #41 did not want to leave her room. They said they had residents with behavioral issues and tried to keep them separated. Residents #41 and #16 did not sit close together in the dining room. The NHA said there was a previous incident between the two residents where Resident #41's forearm was injured, but that was the only altercation she was aware of. She said in light of this new information she would initiate an investigation. The social services director interviewed Resident #41 who said Resident #22 used to pinch her but she had not had any problems with her for about three weeks. She said she knew to avoid Resident #22 and she had no concerns with any other residents.
C. Physical abuse by Resident #16 against Resident #28
Review of facility investigations revealed on 1/31/22, Resident #16 attacked Resident #28 in the common area without prior provocation, scratching her right forearm and leaving red marks. The certified nurse aide (CNA) was in line of sight and intervened immediately. Resident #28 had red marks on her arm but her skin was not broken, she said she was fine, and she did not voice fear of Resident #16, saying She's just like that.
D. Physical abuse by Resident #22 against Resident #16
Review of facility investigations revealed on 4/11/22, Residents #22 and #16 were yelling, name calling, cursing and attempting to kick and hit each other. Resident #22 was named as the assailant and Resident #16 was the victim. Neither resident was physically injured. The plan going forward was to keep the residents in line of sight and separate from each other. However, the incident occurred when the residents were within line of sight of staff in a common area.
E. Physical abuse by Resident #16 against Resident #26
Facility investigations revealed on 6/5/22 Resident #16 backhanded Resident #26 across the face, causing swelling under her right eye. The response was that Resident #16 was closely monitored for behaviors and triggers, and was to be kept in line of sight by staff. However, staff were in line of sight and running to intervene when Resident #16 backhanded Resident #26.
F. Physical abuse by Resident #22 against Resident #16
Facility investigations revealed on 7/19/22 Resident #16 swung at Resident #26, who retaliated by slapping her across the face, leaving a red mark. The facility response was that both residents had very low BIMS and dementia diagnosis. Neither resident had a recollection of the event. Reviewed care plans, notes, and spoke with staff. Resident #16 had been stable on her medications, resident was very closely monitored for behaviors, triggers, etc. and kept in line of sight. Despite all of this, both residents very quickly became escalated but staff quickly intervened.
G. Staff interview
The NHA and DON were on 9/15/22 at 8:03 p.m. They said keeping Resident #16 in line of sight and away from other residents who also had strong personalities was key. She was easily redirectable with activities, but her reactions are quick, like if someone accidentally bumps into her and she reacts, then we intervene.
The facility failed to keep residents free from abuse. All the incidents above involved Resident #16. (Cross-reference F744, dementia care)
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to investigate allegations of abuse for two (#17 and #45) out of 25 sample residents.
Specifically, the facility failed to investigate abuse ...
Read full inspector narrative →
Based on interviews and record review, the facility failed to investigate allegations of abuse for two (#17 and #45) out of 25 sample residents.
Specifically, the facility failed to investigate abuse allegations against a staff member brought forward by Resident #17 and Resident #45.
Cross-reference F600 for abuse.
Findings include:
I. Facility policy and procedure
The Resident Safety policy, no date of inception or revision, provided by the nursing home administrator (NHA) on 9/14/22 at 5:50 p.m. documented in part, it was the policy of the facility to maintain a work and living environment that was professional and free from threat and/or occurrence of harassment, abuse, (verbal, mental, or sexual), neglect, corporal punishment, involuntary seclusion and misappropriation of property. Making reasonable efforts to provide a safe environment for the residents was one of the most basic and essential duties of the facility. Employees have a unique position of trust with vulnerable residents. Having access to private information, being in a physically intrusive position and having elevated status and special relations with residents makes ethical and professional behavior essential. Our facility promotes an atmosphere of sharing with residents and staff without fear of retribution. Residents must not be subjected to abuse by anyone, including but not limited to, facility staff, other residents, consultants or volunteers, staff of other agencies serving the residents, family members or legal guardians, friends, or other individuals.
Reporting suspected or reported violations:
Any suspected, observed or reported violation of this resident safety policy would be reported to the supervisor on duty immediately. The supervisor on duty shall report any suspected violations of this resident safety policy immediately to the administrator and to the director of nursing or their designee as soon as practicable.
Procedure for investigation:
-The quality assurance manager and/or supervisor on duty will assess the resident and document the date, time, and location of the reported or suspected incident.
-The supervisor would ensure that the resident was protected from harm during the investigation.
-An incident report would be completed.
-An employee suspected of violation of the resident safety policy may be suspended pending the results of the investigation.
-The quality assurance manager and/or supervisor on duty would attempt to interview the resident as well as all nursing, housekeeping, laundry, dietary, activity, social service staff, any visitors or others who may have knowledge of the occurrence or who may had been in the vicinity at the time the incident happened. The quality assurance manager and/or supervisor on duty would prepare a written summary of each interview.
II. Resident #17
Resident #17 was interviewed on 9/12/2022 at 2:47 p.m. He said a certified nurse aide (CNA) at the facility was mean to him purposefully (referring to CNA #3). Resident #17 said he had reported the CNA purposefully pushing on his legs and her name calling to a registered nurse (RN) at the facility a couple months ago, and nothing came of it because he later found out the RN was friends with the CNA. He said he continued to report these issues to staff and finally a few weeks ago the director of nursing (DON) came down to talk to him, and he thought that was about three weeks ago. He said he expressed his concerns to the DON at that time about the staff member and reported the issues with her pushing on his legs purposefully (cross-reference F600).
III. Resident #45
Resident #45 was interviewed on 9/14/22 at 8:15 a.m. She said she did not like certified nurse aide (CNA) #3 because she was mean and rough (no specifics were given by the resident but she was tearful during the interview). She said she felt it did feel like abuse and she was afraid of the staff member. She said she had reported these concerns to the director of nursing (DON) and nursing home administrator (NHA) previously but nothing had been done about it (cross-reference F600).
IV. Record review
A nursing progress note for Resident #17 by licensed practical nurse (LPN) #2 dated 7/10/22 at 3:30 a.m. read, Resident continues this evening to swear at staff, call staff names. Calls for assistance and is noted to immediately yell at staff, verbalize multiple complaints regarding his positioning, as well as all departments in the facility. States he expects his call light to be answered immediately, resident non receptive to any form of waiting. He has made multiple accusations this evening, he is advised to discuss these with administration, he follows this suggestion with comment that he has been in touch with his attorney and speaks to his attorney every Monday regarding his complaints. Staff has been instructed to provide care for this resident with 2 staff members present at all times.
A Complaint & Concern form dated 8/24/22 completed by the DON under nature of concern showed Resident #17 stated he was unhappy with care from a night shift CNA. Resident stated the staff member did not speak to him while providing care. He also stated the CNA did not help assist him with changing his hearing aids. The resident chose not to state the name of the CNA. Under response on the form the suspected CNA was moved to day shift per the CNA's request and for observation. The CNA was instructed to not enter Resident #17's room without another staff member. This change was made in early September and dated 9/1/22.
-The Complaint & Concern form did not include information about the staff member pushing on his legs or calling him names.
A Complaint & Concern form dated 9/9/22 completed by the NHA for Resident #45 showed the nature of the concern as Resident #45 reported CNA #3 was impatient and gruff. She stated stated she did not like CNA #3, and CNA #3 had walked into her room and shut off her call light without addressing the residents' needs. Under the response and action taken it was noted the staff member was educated and encouraged to slow down and approve the resident with a gentle voice and manner, and communicate and approach the resident with additional aid (staff member) if needed.
An Educational Forms document dated 9/9/22 showed CNA #3 was given a verbal warning for a resident stating she was impatient and gruff. The staff member verbalized understanding of resident dignity and was given a handout.
A statement by Resident #45 provided by the facility on 9/14/22 at 8:47 a.m. showed Resident #45 stated she did not know she was afraid of the staff member until this morning, and she never expressed it. The CNA was mean and it was her personality. The resident signed the statement.
V. Interviews
The DON and NHA were initially interviewed on 9/14/22 at 8:45 a.m. The DON said Resident #17 had reported to her some concerns about a CNA. The resident had not given her a name, but she was able to identify the staff member as CNA #3. She said the concerns were initially brought to her sometime in August 2022, and Resident #17 had reported the issues of CNA #3 pushing on his legs. She said she did not know if the staff member had been doing it on purpose or not. She said she did not complete an investigation at the time about it (cross-reference F600). She said the staff member was moved to day shift on 9/1/22 for more supervision and was not moved earlier because of staffing issues in the facility. She said it was not reported to her the staff member had called the resident cry baby or any other verbal issues.
The DON and NHA said they felt for Resident #45 the concerns brought forward to them from the resident did not meet the level of abuse, so an investigation was not done. Both staff acknowledged they felt it was the way and tone of the CNA when she spoke to the resident. They said the resident had not reported she was afraid of the staff member until it was brought to their attention during the survey.
The NHA said it was not ok for staff not to be cordial with residents.
They said they had interviewed some nurses about the CNA and they decided again the staff member should provide care in pairs with another staff member for Resident #45.
Both staff acknowledged they did not interview other residents about CNA #3, but said Resident #17 and #45 had come forward with concerns about the staff member and no investigation had been done (cross-reference F600).
LPN #2 was interviewed on 9/15/22 at 2:00 p.m. She said she was fairly certain the accusations being made from her note in July 2022 were about CNA #3. She said she knew it was about a CNA because if it were her she would have said in her note that it was about her, but that she did not name other staff in her notes. She said she thought it was about CNA #3 pushing on his legs purposefully, and she did not recall any verbal abuse accusations. She said she would have told whoever was coming on the next morning the resident was making accusations and she trusted they would follow up with administration as they were not on during the night and it was a Sunday night. She said she did not follow up with administration herself and notify them about the accusations from Resident #17, and she was unaware if an investigation was done. She said she was at fault and dropped the ball. She said she should have notified administration herself as that was the process at the facility. She said she did not remember who she asked to forward the allegation to administration the next morning, and she put her trust in them that it would be done and it was not.
The DON and NHA were interviewed on 9/15/22 at 7:30 p.m. The NHA said if the facility received an allegation she would immediately make sure the resident was safe. She would suspend the staff member pending an investigation. She said they would follow the reporting process with occurrences and notify law enforcement and the ombudsman. She said she would sometimes interview residents about the allegations first and right away because it was fresh in their minds. She said she would interview other residents as well to ensure the abuse was not spreading. She said the staff were educated to let her know immediately about allegations even if they were not sure it met the criteria of abuse as she would rather know about it than not.
She said the LPN #2 should have let them know right away about the allegations from July 2022 and an investigation should have been done right away. She said an investigation had been done into CNA #3 during the survey and she had substantiated verbal abuse for that staff member and she was pursuing termination of CNA #3 (cross-reference F600).
The NHA and DON both acknowledged if LPN #2 had come forward with her concerns in July 2022 the substantiated verbal abuse for Resident's #17 and #45 could have been possibly mitigated, and the importance of conducting investigations was to prevent and stop further abuse.
The DON said an investigation was not done in August 2022 when she spoke to Resident #17. It was only reported to her on the grievance form that CNA #3 was rude and did not speak to him when she performed care. She said he had called her the roughest CNA, but he did not report the issues with her pushing on his legs at that time.
-There was conflicting information provided by the DON interviews of the time of when she made aware of the staff member allegedly purposely pushing on Resident #17's legs.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, the facility failed to develop a comprehensive care plan for four (#14, #18, #24 and #39)...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, the facility failed to develop a comprehensive care plan for four (#14, #18, #24 and #39) of 12 out of 25 sample residents for services that were to be furnished to attain or maintain the resident's highest practicable physical, mental, and psychosocial well-being.
Specifically, the facility failed to:
-Develop a comprehensive, person-centered care plan to effectively address multiple falls and psychotropic medications for Resident #39;
-Continue to provide updated care planned fall interventions for Resident #14 after his multiple falls;
-Develop a comprehensive, person-centered care plan to effectively address multiple falls and weight loss for Resident #18; and,
-Develop a person-centered care plan for multiple falls, restorative services and activities needs for Resident #24.
Findings include:
I. Facility policy and procedure
The Resident Care Planning and admission policy, undated, was provided by the minimum data set coordinator (MDSC) on 9/15/22 at 6:11 p.m. The policy read, in pertinent part, Each resident has a resident care plan that is current, individualized, and consistent with the medical regimen. The plan of care is initiated within 24 hours after admission to fully develop within 7 days following resident arrival at the facility. Following interdisciplinary team conferences, which occurs 7 days after every 90 days thereafter, the nurse coordinates the resident care plan for all disciplines by updating goals and actions that were discussed. Action or nursing intervention is specific and related to each stated short-term goal. Times and actions are stated so that caregivers new to the resident can carry out care with complete continuity.
II Resident #39
A. Resident status
Resident #39, age [AGE], was admitted on [DATE]. According to the September 2022 computerized physician orders (CPOs), the resident's diagnoses included dementia with and without behavioral disturbances, and macular degeneration.
According to the 8/23/22 minimum data set (MDS) assessment, the resident was severely cognitively impaired with a brief interview for a mental status score of three out of 15. He required extensive assistance of more than two staff for transferring and toileting. He needed extensive assistance of one staff for bed mobility, dressing and personal hygiene. Resident #39 needed limited assistance from one person with locomotion on and off the unit. According to the MDS assessment, he had shortness of breath with exertion such as walking and transferring. The MDS assessment indicated the resident has had more than two falls since his admission to the facility.
B. Record review
The review of the September 2022 care plan for Resident #39 did not identify the resident at risk for falls, had history of falls, or had interventions specifically initiated to prevent future falls.
The mobility care plan, initiated on 8/23/22, identified Resident #39 had a decline in mobility and needed a wheelchair and was referred to physical therapy.
-The care plan did not identify the resident required extensive assistance of more than two staff for transferring and toileting, as indicated by the 8/23/22 MDS assessment.
The review of Resident #39's fall documentation 7/1/22 and 9/10/22 identified Resident #39 had nine falls between 7/1/22 and 9/10/22 without injury. According to incident reports, post fall assessments, and post-incident action reports, interventions were needed to prevent future falls. The identified interventions were not communicated on Resident #39's above care plan. The care plan did not direct staff to ensure Resident #39:
-Wore lace-up shoes instead of slip-on shoes;
-Needed a greater level of assistance with activities of daily living (ADLs);
-Had his call light in reach;
-Had a tab alarm/pressure alarm in place;
-Was educated and reminded to lock his breaks to before transferring;
-Had close monitoring, including providing the resident assistance to common area for additional monitoring;
-Had frequent rounding;
-A bed alarm to alert staff of unsafe transfers; and,
-A fall mat.
The 8/29/22 CPO identified Resident #39 had an order for a Risperdal (an antipsychotic medication) 0.5 milligrams tablet by mouth every night.
The September 2022 medication administration record (MAR) indicated Resident #39 was receiving Risperdal.
-The review of the comprehensive care plan for Resident #39 did not identify the resident had a care plan for psychotropic medication including Risperdal.
C. Staff interview
The therapy service director (TSD), also identified as certified occupational therapy assistant (COTA) was interviewed on 9/14/22 at 10:22 a.m. She said falls were discussed with the interdisciplinary (IDT) team and she received therapy referrals from the team. The TSD said Resident #39 was originally referred to therapies due to his reduction in mobility and had multiple falls. She said Resident #39 was discontinued from physical therapy in August 2022.
The MDSC was interviewed on 9/15/22 at 5:04 p.m. The MDSC said all residents at risk for falling, history of falling, issues with mobility, in physical therapy, and new medications such as psychotropics, should have a fall care plan. She said fall care plans should include assistive devices implemented, instructions how to monitor the resident and any other preventive interventions to limit potential future falls. The MDSC said she conducted a 90 day look back of the resident's medical record and interviewed staff, when completing an MDS assessment and determined interventions to add on the resident's care plan.The interventions would also be added to the care plan after a resident falls and reviewed by the interdisciplinary team. She said the fall committee met once a week.
The MDSC reviewed the care plan for Resident #39. The MSDC confirmed Resident #39 did not have a fall care plan with interventions to prevent falls other than the resident needed a wheelchair for mobility. The MSDC confirmed Resident #39 need for extensive assistance of more than two persons physical assistance for transferring and toileting should have also been included on his care plan. She said Resident #39 should have had a fall care plan with updated interventions to prevent further falls and potential injury.
She acknowledged the care plan was a care directive and said the care plan was part of the staff communication process to identify resident needs. The MDSC said she would complete a full review of residents' care plans.
Certified nurse aide (CNA) #1 was interviewed on 9/15/22 at 5:31 p.m. The CNA said Resident #39 needed two person max assistance with transfers from his bed to his wheelchair. She said he just needed limited assistance toileting because he used the wall mounted bar in the bathroom. The CNA said his transfer and toileting needs were not communicated to her. She said she just identified what he needed based on routinely working with him.
The social service director (SSD) was interviewed on 9/15/22 at 2:25 p.m. She reviewed the care plan and confirmed Resident #39 did not have a care plan for Resperdal but should have a care plan. She said she would create a care plan pertaining to his Resiperal use and related dementia and behavior interventions.
D. Facility follow-up
The SSD provided an updated dementia care plan for Resident #39 on 9/15/22 at 3:49 p.m. The care plan identified the resident had a diagnosis of dementia with behaviors and took Risperdal. According to the care plan, interventions initiated on 9/15/22 included:
-Monitor and document target behaviors every shift;
-Monitor for changes in condition that may warrant increased supervision/assistance and notify the physician;
-Divert or redirect attention if he becomes physically aggressive, provide one to one visits, offer snacks/fluids and provide verbal cues/reminders to not be physically aggressive;
-Encourage family support and visits; and,
-When offering assistance approach [NAME] in a comment or by calling him by name.
III. Resident #14
A. Resident status
Resident #14, age [AGE], was admitted on [DATE]. According to the September 2022 CPO, the resident's diagnoses included hemiplegia following a cerebral infarction (stroke) affecting left non-dominant side, insomnia, bipolar disorder, and schizoaffective disorder.
According to the MDS assessment, the resident had moderate cognitive impairment with a brief interview for a mental status score of 12 out of 15. He required limited assistance of one person with bed mobility, dressing, toileting, personal hygiene, locomotion, and transfers.
B. Record review
The review of the fall care plan, initiated 7/9/2020, identified Resident #14 was at risk for falls.
-The care plan did not indicate the resident had a history of falls, or a history of falls with injury.
-The care plan did not identify new interventions after each fall to prevent future falls. The care plan for falls included the following initiated interventions on 7/9/2020:
-Refer to physical therapy (PT) for evaluation if indicated; and,
-Monitor for changes in condition that may warrant increased supervision/assistance and notify the physician.
The fall care plan did not identify new interventions until 7/8/22, two weeks after the resident had a fall on 6/25/22 after a cardiovascular incident resulting in a hematoma (clotted blood). Falls between 7/9/22 and 9/9/22 did not result in an injury. Interventions added to the care plan on 7/8/22 included:
-Use of a wheelchair for long distance or ability related to a recent decline;
-Use of a tab alarm well in share related to impulsive behavior of standing up and it risk for fall;
-Reminder to ask staff for assistance with ambulation; and,
-Assist with one staff member for ambulation.
-The fall care plan did not identify additional interventions even though the resident continued to have seven more falls between 7/9/22 and 9/9/22.
The review of Resident #14's fall documentation identified Resident #14 had seven falls between 6/25/22 and 9/10/22.According to incident reports, post fall assessments, and post-incident action reports, interventions were needed to prevent future falls. The identified interventions were not communicated on Resident #14's above care plan. The care plan did not direct staff to ensure Resident #14:
-Continue PT and occupational therapy (OT);
-Room was clutter free;
-Bed in lowest position;
-Had his call light in reach;
-Had pressure alarm in place;
-Was educated on safety;
-Frequent visual checks;
-Had routine toileting;
-Was monitored and provided encouragement to remain in a public area; and,
-Had a fall mat.
C. Staff interviews
The TSD was interviewed on 9/14/22 at 10:22 a.m. She said Resident #14 was referred to therapy related to his change in gait and function and he had an increase in falls. She said therapy worked with caregivers/staff on transfer and mobility safety. She said he was not currently receiving therapy services.
The MDSC was interviewed on 9/15/22 at 5:04 p.m. She said Resident #14 was challenging because he was impulsive, very independent and continued to fall. She acknowledged he should have had new interventions added to the care plan to help prevent future falls. The MDSC said Resident #14 would be reviewed in the upcoming IDT meeting to review his past falls and determine what interventions were working for Resident #14 and what intervention could be added to his care plan. IV. Resident #18
A. Resident status
Resident #18, age [AGE], was admitted on [DATE]. According to the September 2022 CPO, diagnoses included Parkinson's disease, dementia without behavioral disturbance, adult failure to thrive and history of falling.
The 7/15/22 MDS assessment documented he was cognitively intact with a BIMS score of 12 out of 15, no behavioral symptoms and no rejection of care. He needed extensive assistance with activities of daily living except eating and personal hygiene, and used a wheelchair for ambulation. He had two or more falls since the last assessment, one with injury. He had significant weight loss and was not on a weight loss regimen. His 4/15/22 admission MDS documented he weighed 147 pounds, and his 7/15/22 MDS documented he weighed 117 pounds.
B. Resident interview
Resident #18 was interviewed on 9/12/22 at 4:30 p.m., and on 9/15/22 at 10:15 a.m. He said he had lost a lot of weight and was down to skin and bones, but he was gaining some of his weight and strength back, with good food and plenty of snacks. He acknowledged he had several falls, and said he did not like the personal alarms but was told they were necessary. He said he preferred to get up when he wanted to get up without a damn alarm going off. He indicated he was able to disengage the alarm, and said they had not really gotten his permission to administer personal alarms.
C. Record review
1. Failure to develop a comprehensive, person-centered care plan regarding falls and use of personal alarms
Resident #18's CPO listed a clip alarm for bed, wheelchair, recliner and bathroom check for placement every shift for poor safety awareness (ordered 4/4/22).
Resident #18 had 10 falls within five months according to nursing progress notes. His first fall occurred within an hour of his 4/4/22 admission to the facility. He was admitted on [DATE] at 6:02 p.m. with abrasions to his right elbow, abrasions and bruises to both hands and forearms, and soreness from broken ribs resulting from falls at home prior to admission.
-On 4/4/22 at 7:01 p.m. he was found on the floor in the bathroom with an abrasion to his knee.
-On 4/8/22 at 5:16 p.m. he was found on the floor beside his bed and fall mat with rib pain from prior falls at home.
-On 4/14/22 at 4:20 a.m. he was found on the floor of his room bleeding from previous injuries and rib pain.
-On 4/15/22 at 6:04 p.m. he had been found kneeling on his floor mat twice during the shift, with rib pain and an abrasion to his knee from a previous injury.
-On 5/11/22 at 3:00 p.m. he was found on the bathroom floor with an abrasion and bleeding to his upper arm and his wrist was swollen and tender to touch.
-On 5/16/22 at 2:53 a.m. he was found on the floor with his pillow repeatedly, having rolled out of bed, and was kept out at the nurses' station in line of sight.
-On 6/11/22 at 9:46 p.m. he was found on the floor next to his bed with no injuries.
-On 6/25/22 at 4:46 p.m. staff had transferred him from bed to wheelchair, and when she turned her back he attempted to stand up unassisted and slid to the floor. He was assisted back into his chair by a registered nurse (RN) and CNA and did not suffer any injuries.
-On 8/5/22 at 6:45 a.m. he was found on the bathroom floor and suffered a skin tear to his elbow. He was taken to the common area for monitoring.
-On 8/30/22 at 1:54 p.m. he fell forward out of his wheelchair onto the floor in the common area by the nurses' station. He had previously been observed sleeping in his wheelchair. He had a small area of redness to his right temple.
-After each fall, nursing staff documented that either a low bed, fall mat or personal alarm, or all the above, were in place. However, the care plan was not developed until 4/15/22 after the resident's third fall, and the only revision dated 8/2/22 read, Uses a Tab alarm while in the chair. According to the CPO and nursing notes, personal alarms had been in place since the resident's admission on [DATE]. The care plan identified poor safety awareness and frequent falls, but did not include the dates or circumstances of the resident's falls. New interventions were not documented in the care plan after each fall.
-Fall investigations and risk assessments were requested but were not provided.
-The personal alarm was not care planned as a potential restraint. The resident was typically found after each fall, indicating the personal alarm did not prevent or reduce falls.
2. Failure to develop a comprehensive care plan regarding weight loss and nutritional needs
The September 2022 CPO listed a nutritional supplement, 120 ml three times daily for dietary supplement (ordered 6/27/22).
The most recent registered dietitian note, dated 9/13/22, documented the resident ate 75-100% on average with some assistance, adaptive silverware and a plate guard. He was gaining weight, from 116.8 pounds on 7/7/22 to 124.4 pounds on 8/1/22 to 130.8 pounds on 8/26/22, but was below his regular weight range of 139-169 pounds and had abnormal labs. His BMI (body mass index) was at the low end of normal at 19.8. The plan was to continue supplements, continue to offer snacks between meals, and encourage and monitor meal and fluid intakes.
Review of weights since admission revealed Resident #18 had lost 11.26% of his body weight since admission and although he was gaining weight, he had not gained back to his admission weight (see MDS assessments above).
The dietary care plan goal was for Resident #18 to eat, drink and not be hungry. There were three interventions, initiated on 4/7/22 and not revised, as follows: Monitor and record all meals, snacks and fluid intakes daily; weigh weekly for four weeks, then monthly if stable, notify physician of weight changes of 5% in 30 days or 10% in 180 days; regular diet with nectar thick liquids and a regular texture, with chopped meats as needed for self-feeding.
-Although the facility had implemented measures to address the resident's weight loss, there was not a corresponding nutritional care plan to identify actual weight loss and the specific interventions provided for Resident #18.
D. Staff interviews
The MSDC was interviewed on 9/15/22 at 5:30 p.m. She said he did have a dietary care plan, but should have a weight loss care plan to include the current interventions he was given every day. Regarding falls, she said her thought was to add the fall mat, low bed, more frequent checks than they currently did just to check in, because he hardly ever used his call light. She said his care plan would definitely be reviewed and updated, and she suspected they would be doing away with personal alarms after the survey was completed.
V. Resident #24
Resident status
Resident #24, age [AGE], was admitted on [DATE]. According to the September 2022 CPO, diagnoses included Parkinson's disease, dementia, depression and chronic pain syndrome.
The 7/27/22 MDS assessment documented severe cognitive impairment with a BIMS score of three out of 15. She had no behavioral symptoms and no rejection of care. She needed extensive assistance with most ADLs, used a wheelchair for ambulation, and had range of motion limitations to her lower extremities. She had not had any falls since the prior assessment.
B. Observations
Resident #24 was observed throughout the survey, from 9/12 through 9/15/22, spending most of her time sitting in her wheelchair in the common areas or in her room alone. There was a tab alarm on the back of her wheelchair and she had a wander guard. She was typically not engaged in activities, and often had her head down with her eyes closed. On 9/13/22 at 12:02 p.m. and 12:13 p.m. she set off the alarm at the door leading from the common area into the therapy gym. Staff assisted her away from the door and back into the common area both times.
C. Record review
1. Eight falls within six months, most unwitnessed
Resident #24 had eight falls within the past six months as follows according to nursing notes and fall investigations:
-On 2/15/22 at 2:14 p.m. she was resting in bed then lowered herself to her floor mattress and scooted on her bottom towards the entry of her bedroom door. No injuries.
-On 3/20/22 at 2:11 a.m. she lowered herself to the mattress on her floor twice tonight. Nursing staff assisted the resident back to bed. No injuries voiced or noted. Will monitor frequently throughout the night.
-On 6/26/22 at 9:31 p.m. she was found on the fall mat at the side of her bed lying on her left side and both lower extremities under the bed. She had removed her pants, brief and socks, and her wheelchair was seven -10 feet away from the resident. She had a skin tear to her right pinky toe nail bed. It was not documented when she was last checked on.
-On 6/27/22 at 7:51 p.m. she was found by another resident lying on the floor in her room near her wheelchair flat on her back, no fall mat in place. Staff to ensure safety measures are in place: fall mat, low bed, tab alarm, and refer to physical therapy. This fall was not documented in nursing notes.
-On 7/6/22 at 3:50 a.m. she was found on the floor in her room beside her floor mat during 4:00 a.m. incontinence care rounds. The call light was on and the resident was soiled. She was assisted to the bathroom and back to bed. It was not documented when she was last checked on by staff.
-On 8/15/22 at 1:35 p.m. she was found lying on the bathroom floor on her back, brief and pants removed with incontinence of stool, appears to have attempted to transfer self on the toilet, states that the back of her right head, right elbow and big right toe hurt, bruising starting to form to right elbow. Tab alarm was on resident at time of fall to alert staff of her getting out of the wheelchair by herself. It was not documented when she was last checked on by staff.
-On 8/22/22 at 12:54 a.m. she was found having slid herself out of bed and onto the mattress next to the bed per her own admission. She was assisted back into her bed which had been and remained in low position, call light in reach. No injuries.
-On 9/9/22 she was found on the bathroom floor. Safety measures continue: low bed, fall mat, tab alarm to alert staff of unsafe transfers, staff to encourage resident to remain in common area for observation, offer routine toileting (per a 9/12/22 fall investigation). This fall was not documented in nursing notes.
-Although Resident #24 had a tab alarm, she was typically found on the floor after falls, indicating the tab alarm did not help to reduce or prevent falls.
2. Failure to develop comprehensive, person-centered care plans to engage the resident to prevent falls and improve quality of life
Her care plan, initiated 8/1/19 and revised on 12/10/21, identified risk for falls related to poor decision making, cognitive decline and unsteady gait/mobility. Interventions included call light within reach, encourage call light use, properly fitting non-skid footwear, clutter-free environment, mattress on floor when in bed, assist with transfers as she is not strong enough to transfer herself and ambulates throughout the facility by propelling her wheelchair.
Her activities care plan, initiated on 8/12/19 and not revised, identified minimal participation in activities. She would occasionally attend exercise group activities depending on her mood. Interventions included assess her response and modify as needed, remind and assist to activities, create activity plan based on resident preferences, and post activity calendar in her room.
-There was no restorative nursing or range of motion care plan or intervention, although the resident had limited range of motion. She was also referred by therapy to restorative services on 7/26/22 which was noted by the occupational therapist as not available at this facility but staff are encouraged to include resident in facility exercises and activities.
-A care plan regarding personal alarms could not be found.
-There was no care plan for actual falls and no care plan updates after falls over the past six months.
-A person-centered activities care plan to incorporate resident engagement to prevent falls was not developed. Moreover, review of activity participation records revealed the resident went for days or weeks without any documented activities from 3/21/22 to current. Her activity participation was documented as reminiscing, family and friend visits, beauty shop (once), aromatherapy (once) and music (once). Exercise activity participation was not documented at all.
D. Staff interview
The MSDC was interviewed on 9/15/22 at 5:43 p.m. She said Resident #24 did participate in exercise group twice a week, either actively or passively. All these things could be incorporated into her care plan. She said she would follow up and update her care plan accordingly. We'll probably get rid of tab alarms and continue to look at restorative and activities to help try to prevent falls.
VI. Additional staff interviews
The nursing home administrator (NHA) and the director of nursing (DON) was interviewed on 9/15/22 at 7:39 p.m. They said the MDSC had been pulled in a lot of different directions, impacting care plan development and needed more support. The DON said the IDT would start and complete fall care plan interventions in the IDT meetings.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observations, record review and interviews, the facility failed to ensure proper storage of medications for one of one medication storage rooms and one of two medication storage carts.
Speci...
Read full inspector narrative →
Based on observations, record review and interviews, the facility failed to ensure proper storage of medications for one of one medication storage rooms and one of two medication storage carts.
Specifically, the facility failed to ensure proper date of opening for a multi use tuberculin vial and an insulin pen.
Findings include:
I. Manufacturer instructions
Manufacturer instructions for Aplisol (tuberculin) solution retrieved 9/21/2022 from https://www.fda.gov/files/vaccines%2C%20blood%20%26%20biologics/published/Package-Insert---Aplisol.pdf, showed vials in use more than 30 days should be discarded due to possible oxidation and degradation which may affect potency.
Manufacturer instructions for Lantus insulin pens retrieved 9/21/2022 from https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/021081s072lbl.pdf, showed pens should be discarded 28 days after opening.
II. Facility policy and procedure
The Storage of medications policy, revised April 2007, provided by the nursing home administrator (NHA) on 9/19/2022 at 2:00 p.m. read the facility shall store all drugs and biologicals in a safe, secure, and orderly manner. Drug containers that have missing, incomplete, improper, or incorrect labels shall be returned to the pharmacy for proper labeling before storing. The facility shall not use discontinued, outdated, or deteriorated drugs or biologicals. All such drugs shall be returned to the dispensing pharmacy or destroyed.
III. Observations
The medication storage refrigerator was inspected with licensed practical nurse (LPN) #3 on 9/14/22 at 2:00 p.m. Inside the medication refrigerator an open bottle of Aplisol tuberculin solution was observed to be unlabeled with a date of open.
LPN #3's medication cart was inspected and inside was an in use Lantus insulin pen with no open date labeled.
IV. Interviews
LPN #3 was interviewed on 9/14/22 at 2:00 p.m. She said both the tuberculin solution and insulin pens were supposed to be labeled. She said she had no idea how long the tuberculin solution was in the refrigerator as it was not labeled. She says she believed both were good for 30 days after opening but she was not sure. She said both medications were supposed to be labeled with the day of opening. She said both medications were discarded since she did not know the open date.
The DON was interviewed on 9/15/22 at 7:30 p.m. She said both insulin pens and tuberculin solutions were to be labeled with the date of open and discarded she thought 30 days after opening or according to the manufacturer's instructions.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected multiple residents
Based on interviews and record review, the facility failed to take timely action to follow up on grievances of the resident council group.
Specifically, residents who regularly participated in residen...
Read full inspector narrative →
Based on interviews and record review, the facility failed to take timely action to follow up on grievances of the resident council group.
Specifically, residents who regularly participated in resident council said facility staff did not take action on their grievances involving:
-Residents who did not receive adequate staff supervision and dignified treatment, and repeatedly set off alarms and wandered into other residents' rooms; and,
-Food quality and palatability, snacks and dining room concerns/choices.
Residents said nothing ever gets done in resident council, and the concerns they brought forward were unresolved and ongoing. Residents further stated the concerns they discussed in resident council were not documented in the minutes.
Findings include:
I. Facility policies
The undated Resident Council policy, provided by the facility on 9/15/22, included the following: All residents had the right to a quality of life supportive of independent expression, decision making and independence of action. Staff and residents would work together to attempt to resolve any issues/problems within 60 days. The resident council format included that minutes would be taken to include if issues had been resolved or action was being taken, who was involved, what action was being taken, and ask for comments and concerns.
The undated Grievance Procedure policy, provided by the facility on 9/15/22, included the following: Ensure prompt resolution of all grievances regarding resident rights. The grievance official shall be responsible for the timely follow up (5 days) of the corrective action to ensure resolution of the recorded concern and the satisfaction of corrective action. The staff designee shall make contact with the complainant 14 days after the date of initial complaint to ensure full satisfaction with corrective measures.
II. Resident council minutes
Review of resident council minutes for the past six months revealed:
On 3/30/22, seven facility staff and 10 residents attended. The previous month's minutes were read and approved. Concerns about the dietary (department) voiced by residents were: coffee is cold, food is cold, the cooks were not reading the tickets, and the posted chalkboard menus were difficult to read. The staff's documented response was that kitchen staff were being retrained in their positions and white chalk was being used on the chalkboard menus for readability.
-No other resident concerns were documented in the minutes.
-There was no documented discussion of resident rights.
On 4/27/22, seven staff and four residents attended. The previous minutes were read and approved. There was no documentation of action taken on the previous resident concerns. Concerns about dietary voiced by residents were: food is served cold and the kitchen staff were not asking residents what they would like to eat. Staff's documented response was new staff training. Residents voiced that nursing staff were slow to respond to call lights. The staff response was more staff were hired to fix the problem.
-Repeated dietary concerns from the previous month were documented, but there was no evidence of discussion about the lack of action taken and resolution.
On 5/25/22, seven staff and eight residents attended. The previous minutes were read and approved. Concerns about dietary were voiced that food was cold for room trays. The staff response was that kitchen staff had hustled to get room trays out faster to solve the cold food problem.
On 6/29/22, seven staff and four residents attended. The residents voiced concerns again about cold food, said the meat was too tough to chew, and they would like smaller portions as there was too much wasted food. Staff responded that the dietary director had a meeting with staff.
On 7/27/22, seven staff and four residents attended. Residents said the meat was too tough to eat. The resolution was the dietary director stopped ordering the pork chops.
On 8/31/22, seven staff and three residents attended. Residents said they would like more snacks, cornbread without sugar, cornbread browned, and bacon in the beans. One resident said he would like bottled water as he did not like the filtered water in the facility. The staff response was they would purchase water for the resident who requested it. Plans for resolution of the other dietary concerns were not discussed.
-There was no evidence of grievances generated as a result of resident council discussions, and no evidence that staff discussed resolutions to resolve ongoing dietary concerns voiced by resident council.
III. Resident group interview
Residents #4, #6 and #23, including the resident council president and two residents who regularly attended, and were cognitively intact and interviewable, were interviewed on 9/13/22 at 2:30 p.m.
When asked if the facility considered the views of the resident group and acted promptly upon grievances and concerns, they responded, No. When asked if a rationale was provided when the facility was unable to make changes as requested, they said, No. They did not know how to file a grievance. They said, Nothing ever gets done and that resolutions to the concerns they brought up during resident council were always ongoing.
The residents said they sometimes felt like inmates because the door alarms were set off so frequently by confused residents who tried to elope. They said some certified nurse aides (CNAs) were not well trained and thought they had to make people do things, by saying to confused residents, No, you can't do that and the residents did not understand because they think they have to leave and there's really no place for them to go, but they're always testing the doors. They just want someone to walk around with them. They named Residents #3, #7, #22 and#43.
They said these residents wandered into other residents' rooms including theirs and you have to get them out. They said it was disturbing and disgusting to them at times, and that was why they had stop signs on their doors. They described examples where a resident urinated in their laundry basket, another resident dropped trash into their laundry basket, and a third resident entered their room and said she was going to take a nap in their roommate's bed and proceeded to do so. They said they did not feel that staff adequately supervised and engaged confused residents in activities to prevent them from encroaching on the privacy and rights of other residents.
The residents said there were unresolved food concerns, that food choices and food palatability were a problem. The corn bread was still a problem in that it had a sweet taste they did not like, foods were served that did not go well together, there was no bacon in the beans as requested, and the food was sometimes served cold. A resident said he saw his food sitting in the kitchen window for 10-15 minutes before being served to him, and it was cold. There was too much food waste and requests for small portions were not honored.
They said sufficient flavorful, substantial snacks of their choice were not provided, dinner was served early and from 4:00 p.m. until the next morning is a long time to go on soup and a sandwich. They said dinner was only served until 5:00 p.m. and that's it, and then the dining room was closed. They said several days could go by where there were no drinks, no sodas, no juices, the fridge will just be empty. They had requested specific snacks that were not provided, such as V8 juice, Oreos and Fig Newtons.
IV. Nursing home administrator follow-up
The nursing home administrator (NHA) was interviewed on the afternoon of 9/13 and 9/15/22. She said she was not previously aware of some of the above resident concerns, but she was aware of resident concerns involving food, snacks and dining room issues. She said she would follow up with the residents regarding their concerns, would follow up to engage wandering residents so they did not violate other residents' rights, and would establish a food committee to help with resolving food and dining room concerns.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0744
(Tag F0744)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review and interviews, the facility failed to effectively address the treatment and service needs ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review and interviews, the facility failed to effectively address the treatment and service needs of three (#16, #39 and #22) of five residents reviewed for dementia care of 25 sample residents.
Specifically, the facility failed to:
-Provide dementia care and services to ensure Resident #39 was provided an appropriate level of meal assistance while promoting a dignified meal experience.
-Provide dementia care and services to provide for resident needs and address repeated incidents of resident-to-resident aggression and abuse for Resident #16; and,
-Provide dementia care and services for Resident #22.
Findings include:
I. Facility policy
The Dementia-Clinical Care policy, March 2015, was provided by the nursing home administrator (NHA) on 9/19/22 via email. The policy read in pertinent part: For individuals with confirmed dementia, the IDT (interdisciplinary team) will identify a resident-centered care plan to maximize remaining function and quality of life. The facility will strive to optimize familiarity through consistent staff resident assignments. Direct care staff will support the resident in initiating and completing activities and tasks of daily living. Bathing, dressing, mealtimes, and therapeutic and recreational activities will be supervised and supported throughout the day as needed. The IDT will identify and document the residents condition and level of support needed during care planning and review changing needs as they arise. Resident needs will be communicated to direct care staff through care plan conferences, during change of shift communications and through written documentation. Progressive or persistent worsening of symptoms and increased need for staff support will be reported to the IDT.
II. Resident #39
A. Resident status
Resident #39, age [AGE], was admitted on [DATE]. According to the September 2022 computerized physician orders (CPO), the resident's diagnoses included dementia with and without behavioral disturbances, and macular degeneration.
According to the 8/23/22 minimum data set (MDS) assessment, the resident was severely cognitively impaired with a brief interview for a mental status score of three out of 15. Resident #39 required limited assistance from one person with eating.
B. Observations
Resident #39 was observed on 9/12/22 at 4:08 p.m. during the dinner meal. The resident's meal was placed in front of him. He picked up his fork in right hand. He proceeded to gently poke the napkin with prongs of the fork multiple times before he made his way to find the plate. After looking down at his meal for several moments, the resident was able to take a small bite of food using his fork. The resident lifted a large slice of tortilla with his fork to his mouth. Resident #39 took a bite of the tip of the tortilla but did not chew through it. The resident sat at the table for over a minute with a large slice of tortilla hanging from his mouth with multiple staff walking past the resident. The staff did not offer to assist Resident #39 in cutting up the tortilla. After a minute, the resident was able to chew through the tortilla hanging on his mouth and the remainder of the tortilla dropped down to the plate.
On 9/13/22 at 3:59 p.m. Resident #39 was assisted to his dining table. The resident was awake and alert.
-At 4:27 p.m. the resident still was not served his meal. Most of the other residents in the dining room were already served. The resident fell asleep at the table.
-At 4:32 p.m. Resident #39 was served. The dietary aide woke the resident up, poured his can of soda and pointed to the resident's utensils wrapped in a napkin. The resident looked at his plate and closed his eyes, opening his eyes a few moments later to look around the room.
-At 4:37 p.m. Resident #39 struggled to retrieve his fork from his folded napkin. Once the fork was free from the napkin, he attempted to lift the butter knife with the fork. The resident then poked at the napkin with the fork, holding the fork upside down. The resident was not offered assistance. After a few minutes focusing on the napkin, the resident moved the fork to the plate and proceeded to feed himself. Throughout the meal the resident stopped eating and looked at the plate and then would slowly start eating again.
C. Resident interview
A group interview was conducted on 9/13/22 at 3:12 p.m. with three residents (#4,#6, and #23) the facility assessed and deemed as alert, oriented, and interviewable. The sample group represented resident experience living in the facility. The residents expressed concerns with the delay in meal service and assistance. Members of the group said they have seen Resident #39 go hungry. They said Resident #39 had use of only one hand and fed himself. They said he would be served his meal but could not yell when he needed help. The residents said sometimes Resident #39 would have to sit and wait to be served while everyone else was eating. According to one of the group interview members, Resident #39 had told him he wanted speech therapy.
An exit interview on 9/15/22 at approximately 8:40 p.m. was conducted with two residents. A general overview of the survey findings were reviewed with the residents. The findings did not disclose resident names or resident details. One resident during the interview stated that he hoped for the facility to provide more meal assistance for Resident #39.
D. Record review
The 2/25/2020 long term stay care plan identified Resident #39 ate his in the dining room. The care plan directed staff to offer the resident snacks between meals, provide a regular diet, and monitor and record intake. The care plan did not identify what type of meal assistance the resident required.
The 8/31/22 nutrition evaluation under recommendations identified that staff should continue to encourage good meal intakes, encourage snacks of choice and encourage good fluid intakes with and in between meals and continue to monitor. The evaluation did identify recommendations to provide Resident #39 assistance with his meals.
The review of September 2022 care plan for Resident #39 identified the resident required assistance with bed mobility, ambulation, bathing, hand hygiene, and toileting assistance, however, the care plan did not identify the Resident #39 needed limited assistance from one staff member with eating as indicated by the 8/23/22 MDS assessment.
The MDS activities of daily living (ADL) question log also known as smart charting between 7/24/22 and 9/15/22, under Eating-ADL Self Performance. The log indicated the resident primarily required supervision and limited assistance with eating. The Eating-ADL Support Provided indicated the resident primarily received no set up or physical help from staff or received set help only. On 8/1/22, the resident was identified to need extensive assist and received one person's physical assistance. On 8/15/22, the resident was identified to need limited assistance and received one person's physical assistance.
-The review of the resident's medical record did not identify the resident had current or recent weight loss.
E. Staff interviews
The activity director (AD) was interviewed on 9/15/22 at 2:50 p.m. She said she and other staff had seen a recent change in Resident #39 and staff were still trying to figure out what would work best for him. The AD said during the IDT team meetings, it was discussed that Resident #39 has had a noticeable decline. She said they noticed when he ate, he would stop eating and then would have difficulty to start eating again. She said interventions have not been implemented because staff were still trying to figure out what was going on.
Licenced practical nurse (LPN) #1 was interviewed on 9/15/22 at 4:15 p.m. She said Resident #39 had a steady decline over the last couple of weeks. She said she was not aware of changes in the resident's eating. She said he needed to set up assistance and then could feed himself. The LPN said the resident needed to have his utensils and his drinks set out for him.
The minimum data set coordinator (MDSC) was interviewed on 9/15/22 at 4:23 p.m. She said when she completed the MDS assessment and coded a resident required limited assistance with one person physical assistance because she determined a resident needed partial assistance with eating and/or not safe eating on his own. She said a staff member should be physically present during the meal offering supervision, guidance, cueing and physical assistance as needed.
The MDSC reviewed the 8/23/22 MDS assessment for Resident #39 and confirmed she identified and coded the resident needing the higher level of assistance of limited physical assistance. She said she reviewed the smart charting, observed Resident #39 at meals and interviewed staff to determine he needed more assistance than supervision, or supervision with set up. She said he sometimes needed more cueing and support during his meals.
The MDSC said changes in resident ADL care needs as eating would be discussed with the IDT team. She said changes in care level would usually be communicated on the 24 hour report, the communication board and face-to-face communication at time when the need was identified. She said she did not know who she informed of the changes.
The MDSC said the changes in meal assistance should have also been discussed in the weekly nutrition at risk (NAR) meetings and documented in the progress notes. The MDSC reviewed the progress notes and said Resident #39 was not discussed in the past 30 days. The MDSC said he has not had weight loss but he should have been discussed in NAR because of the change in meal assistance needed. The MDSC said the high level of meal assistance needed should have been on the care plan. The MDSC reviewed the care plan and identified he did not have a care plan conveying to staff the level of meal assistance he currently needed. She said she would review him in the next NAR meeting, update the care plan and refer him to physical and occupational therapy.
Certified nurse aide (CNA) #1 was interviewed on 9/15/22 at 5:31 p.m. The CNA said Resident #39 usually needed meals to be set up but was not aware of any other meal assistance needed. She said sometimes he gets confused with his fork and spoon. She said he needs some cueing and handing him his coffee cup handle. She said he did not receive any other assistance with meals. The CNA said sometimes he would just look at his food.
The NHA and the director of nursing (DON) were interviewed on 9/15/22 at 7:35 p.m. They said the IDT team discussed the changing needs of Resident #39 during the week of the survey. They said they discussed referring the resident to speech therapy. They said the staff needed to provide Resident #39 with cueing during meals and they would provide staff education.
II. Resident #16
A. Resident status
Resident #16, age [AGE], was admitted on [DATE]. According to the September 2022 CPO, diagnoses included dementia with behavioral disturbance, restlessness and agitation, generalized anxiety disorder and brain stem stroke syndrome.
The 7/11/22 minimum data set (MDS) assessment documented severe cognitive impairment with a brief interview for mental status (BIMS) score of three out of 15 and delirium symptoms involving inattention. No behavioral symptoms were documented. She needed extensive assistance with most activities of daily living (ADLs) and used a wheelchair for ambulation.
B. Record review revealed failures in provision of dementia care and services
September 2022 physician orders documented Resident #16 took antidepressant and antipsychotic medications.
Review of facility investigative reports revealed Resident #16 was involved in all six resident-to-resident abusive incidents over the past eight months, which occurred on 1/31, 4/11, 5/2, 6/5 and 7/19/22.
Nursing progress notes reviewed for the same time period revealed Resident #16 was frequently verbally and physically abusive to staff, and needed line of sight monitoring by staff to prevent altercations from other residents.
Only three activity notes were found in the progress notes: on 3/16, 3/17 and 4/1/22, regarding her enjoyment of the St. Patrick's Day party, social events and movies, and live music.
Resident #16's most recent activities assessment, dated 7/11/22, identified she was a retired teacher. Her activity interests included socialization, one-on-ones (visits), hobbies, exercise and sports, religious/spiritual, television, movies, and musical activities. Her preferred activity time was late afternoon two to three times per week.
Activity participation records reviewed for the previous six months revealed Resident #16 was frequently not engaged in activities. Documented activities were reminisce, family and friend visits, nail care (one time on 3/16/22), beauty shop (one time on 8/15/22) and outside visiting (one time on 8/12/22). There were large gaps of days or weeks between documented activities. She participated in five activities during March, none in April, four in May, two in June, three in July, six in August, and none in September 2022.
The care plan for verbally (and occasionally physically) aggressive behavior, initiated on 7/19/21 and not revised, listed the following interventions: talk in calm voice when behavior is disruptive, remove from public area when behavior is disruptive and unacceptable, reinforce unacceptability of verbal abuse, praise for demonstrating desired behavior, monitor and document target behaviors, elicit family input for best approaches to resident, do not argue with resident, discuss options for appropriate channeling of anger, assist in selection of appropriate coping mechanisms, administer behavior medications as ordered by physician, provide diversional activities (magazines, offer cold drink, etc.).
The care plan for activities, initiated on 9/18/19 and not revised, listed the following interventions: assess resident's response to new activity plan, modify as needed; remind when activities are scheduled; assist to preferred activities; provide environment that respects privacy; create activity plan based on resident preferences; a monthly calendar is placed in her room.
-The care plans were not person-centered, were not updated following abusive incidents, did not identify triggers or specific methods to engage the resident to avoid or quickly diffuse potentially abusive situations, and did not include keeping the resident within line of sight in order to intervene before she became abusive to other residents. (Cross-reference F600, freedom from resident-to-resident abuse)
C. Staff interview
The NHA and DON were interviewed on 9/15/22 at 8:00 p.m. They said they would develop comprehensive plans and interventions to engage Resident #16 to meet her dementia care, behavioral and quality of life needs, and protect other residents' safety and quality of life.
III. Resident #22
A. Resident status
Resident #22, age [AGE], was admitted on [DATE]. September 2022 CPO diagnoses included dementia with behavioral disturbance and anxiety disorder.
The 7/22/22 MDS assessment documented severe dementia with a BIMS score of three out of 15 and no behavioral symptoms. She needed limited assistance with most ADLs and used a wheelchair or walker for ambulation.
B. Record review revealed failures in provision of dementia care and services
September 2022 physician orders documented Resident #22 took antidepressant and antipsychotic medications.
Review of facility investigative reports revealed Resident #22 was involved in two resident-to-resident abusive incidents over the past eight months, both with Resident #16, on 4/11/22 and 7/19/22.
Nursing progress notes revealed Resident #22 frequently disturbed other residents by wandering into their rooms, had loud verbal outbursts, exhibited verbal and physical aggression, tried to provide care for other residents, perseverated on looking for her dog, argued with other residents, attempted to hit other residents, and was difficult to redirect.
A few activity notes were included in the progress notes regarding enjoying the St Patrick's Day party on 3/17/22, enjoying bingo and social events on 3/16/22, live music on 4/1/22, socializing well with other residents on 5/31/22, at the round table with others watching television on 6/6/22, two movies and socialization with snacks on 7/15/22, socializing with others and looking at magazines on 7/30/22, snacks with TV and coloring on 8/13/22, and enjoying the luau on 8/26/22.
Her most recent activities assessment on 3/9/22 identified her activity interests as socialization activities and one-on-ones in the late afternoon.
The activity participation records, reviewed for the past six months, documented she attended reminisce, visits with family and friends, had outside visits twice and beauty shop once. There were large gaps of days or weeks between activities. She was documented to participate in activities five times in April, five times in May, 10 times in June, four times in July, eight times in August, and none in September 2022.
Resident #22's behavioral care plan, initiated 7/20/22 and not revised, included exactly the same title and interventions as Resident #16's (see above) and was not person-centered. No revisions, trigger identifications or specific methods to diffuse aggressive situations were included in the care plan.
Her dementia care plan, initiated 1/17/22 and not revised, listed the following interventions: monitor and document behaviors; divert or redirect attention; provide one-on-one; offer snacks/fluids; approach warmly and positively; encourage family visits and support; approach in a calm manner, calling her by name; encourage her to attend activities of choice; speak to her in clear concise sentences and allow for her to answer; do not hurry or rush.
-No activities care plan could be found.
C. Staff interviews
CNA #2 was interviewed on 9/15/22 at 2:00 p.m. and said they tried to keep Residents #16 and #22 apart and redirected or engaged in something more interesting than arguing or being aggressive, which tended to happen more in the evenings.
CNA #1 was interviewed on 9/15/22 at 5:10 p.m. and said they had enough staff to provide the necessary ADL care for residents, but not to engage with the residents, spend time with them, anticipate their needs to address behavioral symptoms
The NHA and DON were interviewed on 9/15/22 at 8:00 p.m. They said they would develop comprehensive plans and interventions to engage Resident #16 to meet her dementia care, behavioral and quality of life needs, and protect other residents' safety and quality of life.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review and interviews, the facility failed to ensure proper infection control practices for one of...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review and interviews, the facility failed to ensure proper infection control practices for one of one dining rooms and one of one laundry rooms.
Specifically, the facility failed to ensure:
-Residents were offered hand hygiene prior to meals; and,
-Proper personal protective equipment (PPE) was utilized in the laundry room.
Findings include:
I. Facility policy and procedures
The Infection Control policy, no date of inception or revision, provided by the infection and control preventionist (IP) on [DATE] at 12:00 p.m. read, there was an active facility wide infection control program with effective measure to control and prevent infections acquired or brought in the facility from the community or other health care facilities. There was a practical system for reporting, evaluating, and maintaining records of infections among residents, including assignment of responsibility for ongoing collection and analysis of data and required follow up.
II. Hand hygiene
A. Observations
Dinner meal service was observed on 9/12-[DATE] at 4:00 p.m. The dining room was divided into residents who required assistance with meals and residents who did not. The residents on the side who did not require assistance were not offered hand hygiene prior to their meals.
On [DATE] at 2:08 p.m a bottle of hand sanitizer on a resident dining room table upon entry on the non-assistance side of the dining room was expired as of [DATE].
B. Interviews
Dietary aides (DA) #3 and #4 were interviewed on [DATE] at 4:40 p.m. Both staff acknowledged that it was up to the certified nurse aides to assist residents with hand hygiene, and it was just their responsibility to ensure hand sanitizer was available on the table.
The IP was interviewed on [DATE] at 11:00 a.m. She said hand sanitizer was on all resident dining tables and all staff should be offering and encouraging residents to use it prior to all meals and this was important to prevent cross contamination.
The director of nursing (DON) was interviewed on [DATE] at 7:30 p.m. She said all residents were to be offered hand hygiene upon entering the dining room by any staff member. She said hand sanitizer should be on everything at the dining room table and utilized.
III. Laundry room
A. Observations
The laundry room was inspected with the housekeeping director (HKD) on [DATE] at 2:18 p.m The HKD demonstrated the process of which laundry was handled from start to finish. She demonstrated the process for sorting soiled laundry intake and said only gloves were worn by staff when sorting soiled laundry. She said aprons or additional PPE were not needed and only work for things like COVID rooms soiled laundry.
B. Interviews
The IP was interviewed on [DATE] at 11:00 a.m. She said laundry staff should be wearing gloves, aprons, and a mask when sorting any and all soiled laundry. She said this was important to prevent cross contamination.
The DON was interviewed on [DATE] at 7:30 p.m. She said laundry staff should be wearing gowns, gloves, and potentially goggles as well when sorting soiled laundry.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations, record review and staff interviews, the facility failed to prepare, distribute and serve food in a sanitary manner in one of one kitchen.
Specifically, the facility failed to:
-...
Read full inspector narrative →
Based on observations, record review and staff interviews, the facility failed to prepare, distribute and serve food in a sanitary manner in one of one kitchen.
Specifically, the facility failed to:
-Prevent potential cross contamination during meal preparation;
-Demonstrate appropriate use of gloves during the meal service;
-Ensure cold food items were stored and served at proper temperature to prevent potential food-borne illnesses; and,
-Ensure food surfaces were properly sanitized.
Findings include:
I. Professional reference
The Centers for Disease Control and Prevention (CDC) https://www.cdc.gov/handwashing/handwashing-kitchen.html, dated 7/18/22, retrieved on 9/19/22, read in pertinent part: Handwashing is one of the most important things you can do to prevent food poisoning when preparing food for yourself or loved ones. Your hands can spread germs in the kitchen. Some of these germs, like salmonella, can make you very sick. Washing your hands frequently with soap and water is an easy way to prevent germs from spreading around your kitchen and to other foods. According the CDC, handwashing was especially important during some key times when germs could spread easily:
-Before, during, and after preparing any food.
-After handling uncooked meat, poultry, seafood, flour, or eggs.
-Before and after using gloves to prevent germs from spreading to your food and your hands.
-Before eating.
-After touching garbage.
-After wiping counters or cleaning other surfaces with chemicals.
-After touching pets, pet food, or pet treats.
-After coughing, sneezing, or blowing your nose.
According to CDC guidance, Handwashing: Clean Hands Save Lives, https://www.cdc.gov/handwashing/campaign.html, dated 11/19/2020, retrieved on 9/19/22 read in part Germs are everywhere. Make handwashing with soap and water a healthy habit.
- Everything you touch has germs that stay on your hands.
-Your hands carry germs you can't see.
-Handwashing can help prevent one (1) in five (5) respiratory illnesses.
Additional CDC guidance for food safety, retrieved from
https://www.cdc.gov/foodsafety/people-at-risk-food-poisoning.html, dated 1/24/19, retrieved on 9/19/22, read in part:
Anyone can get food poisoning, but certain groups of people are more likely to get sick and to have a more serious illness. Their bodies' ability to fight germs and sickness is not as effective for a variety of reasons. Adults aged 65 and older have a higher risk because as people age, their immune systems and organs don't recognize and get rid of harmful germs as well as they once did. Nearly half of people aged 65 and older who have a lab-confirmed foodborne illness from salmonella, campylobacter, listeria or E. coli are hospitalized . People with weakened immune systems due to diabetes, liver or kidney disease, alcoholism, and HIV/AIDS; or receiving chemotherapy or radiation therapy cannot fight germs and sickness as effectively. For example, people on dialysis are 50 times more likely to get a listeria infection.
II. Facility policy
The following food policies were provided by the facility on 9/15/22:
The Dietary Department Infection Control policy, undated, read in part: Proper procedures are followed at all times in order to prevent the spread of infection. Proper techniques are employed to prevent the possibility of cross-contamination and foodborne illnesses including: washing hands with germicidal soap before preparing Foods, eating, after smoking, after using the restroom, after working with potentially hazardous food, and at any other time hands becomes contaminated in any way.
The Sanitary Condition of Dietary Department policy, undated, read in part: Sanitary conditions are maintained at all times in the Dietary Department. All surfaces used for the preparation of food are sanitized before the beginning of the preparation of food, between using the surface for the preparation of raw cooked food in order to prevent cross-contamination and after preparation is complete.
The Food Temperature policy, undated, read in part: Foods are prepared and served at proper temperature in order to assure the safety of the residents. Potentially hazardous foods are kept at an internal temperature of 45 degrees F (Fahrenheit) or below or at an internal temperature of 140 degrees F or above during display and service.
The Food Preparation and Service policy, undated, read in part: Equipment is provided and procedures established to maintain food at a proper temperature during storage and service.
III. Observations
On 9/12/22 at 2:10 p.m. during the initial kitchen tour, a sanitized cleaning bucket was observed in the kitchen. [NAME] #1 was unsure if he was to use the chlorine test strips or the quat test strips. [NAME] #1 decided on the chlorine test strips and tested the sanitized water with chlorine test strips. The test strip indicated the solution measured at 10 parts per million (ppm).
-However, the cook used the wrong testing strip, he should have used the quat test strips to test the solution (see the corporate regional dietary consultant interview).
According to the cook the solution was used to clean kitchen food surfaces. He said the buckets were changed out once per shift.
The dinner service in the kitchen was observed between 3:20 p.m. and 4:45 p.m.
-At 3:32 p.m. DA #1 pulled out a tray of plated pre-cut key lime pie slices out of the refrigerator and placed them on a cart to be included as the resident dinner dessert item. The slices were not covered or placed on or in a cooling surface to maintain a temperature appropriate for cold food items.
-At 3:34 p.m. cook #2 took the temperatures for the hot food items. [NAME] #2 did not take the temperature to the pre-cut key lime pie slices. The cook said the dietary manager (DM) usually obtained the food temperatures before service. He said he has not taken the food temperatures for over a year.
-At 3:42 p.m. cook #2 adjusted the back of his shirt with his gloved hands. He did not doff his gloves and perform hand hygiene.
-At 3:45 p.m. cook #2 placed his right gloved hand in his apron pocket slightly pulling out a white cloth while touching his left gloved hand of his face mask. He did not doff his gloves and perform hand hygiene.
-At 3:46 p.m. cook #2 left the steamline and walked to the back of the kitchen. He retrieved an open plastic water bottle out of the refrigerator with his gloved hands. He returned to the steamline. [NAME] #2 pulled his mask below his nose and mouth with his gloved hands and drank the remainder of the water in the bottle. [NAME] #2 pulled up his mask with his gloved hands and threw the empty bottle away. He did not doff his gloves and perform hand hygiene.
-At 3:48 p.m. cook #2 patted the regional dietary consultant on his back and returned to the steamline. He proceeded to plate resident meals. He did not doff his gloves and perform hand hygiene prior to plating the meals.
-At 3:49 p.m. cook #2 plated the resident first meal and DA #1 took the plated meal, beverages and a slice of key lime pie on a food tray. The DA expedited the meal out the kitchen service window.
-At 3:52 p.m. cook #2 wiped his hands on the back pants. He did not doff his gloves and perform hand hygiene prior to plating the meals.
-At 3:55 p.m. DA #1 retrieved a second tray of key lime pies from the refrigerator. As she placed the tray on the cart, her arm touched the surfaces of one of the pies. She wiped her elbow off with gloved hands, pulled her mask under her nose and mouth, walked to the other side of the kitchen and threw the pie slice away. She pulled the mask back over her nose and mouth with her gloved hands and returned to the service line. She did not doff her gloves and perform hand hygiene
-At 3:56 p.m. DA #1placed two pie slices on resident trays, with her gloved thumb in the center of the eating surface of the pie plates.
-At 3:59 p.m. cook #2 left the steam line and walked to the back of the kitchen. He retrieved a plastic bottle of water out of the refrigerator with his gloved hands. He returned to the steamline, pulled his mask below his nose and mouth with his gloved hands and took a sip of the water. He pulled his mask back up with his gloved hand and returned to plating food. He did not doff his gloves and perform hand hygiene.
-At 4:01 p.m. cook #2 adjusted his mask with his gloved hands without performing hand hygiene.
-At 4:03 p.m. cook #2 pulled his mask down with his gloved hands and took another drink of water from his water bottle. He pulled his mask back up. The corporate regional dietary consultant (CRDC) directed cook #2 to doff his gloves and perform hand hygiene.
-At 4:07 p.m. DA #1 placed her gloved right hand on the wall as she spoke to the DM.
-At 4:09 p.m. DA #1 touched her eye glasses with right hand then placed her gloved hand on the meal tray stack. She did not doff her gloves or perform hand hygiene.
-At 4:13 p.m. DA #1 placed her right hand over the drinking surface of a filled juice glass and placed the glass on a resident meal tray.
-At 4:15 p.m. DA #1 placed a plated guard over a plate of food.
-At 4:17 p.m. cook #2 pulled the back of his shirt down with his gloved hands as he plated a meal.
-At 4:43 p.m. a test tray was plated and prepared for sampling.
-At 4:46 p.m. the key lime pie slice temperature was collected. The pie's internal temperature was 50 degrees Fahrenheit (F.) The pie temperature was above 45 degrees F.
On 9/15/22 at 10:45 a.m. a red sanitizer bucket filled with sanitized water was on the counter in the dining room. The DM said the sanitizer was used to wipe down the resident dining room tables. The DM said he did not know when the water was last changed.
The CRDC dipped the hydro quat strip on the bucket of water. The strip did not change in color, indicating a very low amount of sanitizer solution.
The CRDC said the sanitizer did not show registered at appropriate levels and instructed the bucket to be changed with new sanitized water.
IV. Staff interview
The dietary director (DM), the CRDC and cook #2 introduced themself on 9/14/22 at 3:20 p.m. The DM said he recently was promoted to the position as dietary manager and was a cook prior to the promotion. The DM said he had been the facility's DM for less than a week.
The CRDC said the facility was new to the corporation and he was providing consultation and would establish a regional dietary consultant for the facility.
Cook #2 said he had been a cook for the past 10 years.
Cook #2 was interviewed on 9/14/22 at 4:20 p.m. The cook said he was trained annually on hand hygiene and he should change gloves anytime he was handling food, after doffing gloves and anytime he touched contaminated surfaces.
DA #1 was interviewed on 9/14/22 at 4:25 p.m The DA said she should change gloves anytime she stepped away from the service line and anytime she touched non-food surfaces. According to DA #1, surfaces such as the wall or her mask were items she should have changed her gloves and performed hand hygiene after touching.
The DM was interviewed on 9/15/22 at 10:01 a.m. The DM said the facility did not log when they changed the sanitizer buckets. He said the buckets should be changed every two to three hours or less if the water was cloudy.
The above infection control concerns during the meal were shared with the DM and the CRDC.
The CRDC confirmed he also observed breaks in infection control during the 5/19/22 dinner observations.
The key lime pie temperature on the test tray was shared with the DM and the CRDC.
The CRDC said cold food could not rise above 41 degrees F because of the risk of bacterial growth. He said they should have not had a cold food tray sit for long periods at a time till served. He said the dietary department would be changing the way they handled cold food and for now would have the DA retrieve the desserts out of the refrigerated one at a time and serve immediately.
The CRDC said cook #1 should have used the hydrion quaternary test strips not the chlorine test strips to test the red bucket on 9/12/22. He said the chlorine strips were to test the dishwasher. He said the sanitized solution in the read bucket should have registered at 200 ppm for adequate sanitation levels.
The DM and CRDC said he would provide education with staff immediately to address the identified concerns.
The CRDC said on 9/19/22 he would do an in-depth inservice with the dietary department on infection control procedures using the new corporation's training packets.
According to the DM and CRDC, infection control practices would change.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected most or all residents
Based on record review and interviews, the facility failed to develop and implement effective quality assurance/process improvement (QAPI) action plans to identify and address quality deficiencies reg...
Read full inspector narrative →
Based on record review and interviews, the facility failed to develop and implement effective quality assurance/process improvement (QAPI) action plans to identify and address quality deficiencies regarding resident rights and resident care.
Specifically, the facility failed to correct recurring deficiencies related to abuse, investigations, accident hazards, and infection control.
Findings include:
I. Record review
Cross-reference F600 abuse: the facility failed to protect residents' rights to be free from abuse by staff and other residents.
Cross-reference F610 investigations: the facility failed to investigate allegations of abuse and protect residents from further abuse during and after the investigations.
Cross-reference F689 accident hazards regarding elopement: the facility failed to ensure residents were safe from elopement at immediate jeopardy level, with potential for serious injury or death.
Cross-reference F880 infection control: the facility failed to maintain an effective infection control program to prevent the potential spread of infection.
The above deficiencies were repeated deficiencies cited during the prior recertification survey ending on 6/10/21. F689 was previously cited related to other accident hazards including falls, smoking safety and call light accessibility for residents at risk for falls.
II. Staff interview
The nursing home administrator (NHA) and director of nursing (DON) were interviewed on 9/15/22 at 8:15 p.m. They said their QAPI program was working on action plans for wandering/elopement, falls, weight loss, abuse, conducting thorough investigations, any resident concerns brought to their attention, food and vaccinations.
They said they needed something better in place to keep problems from occurring and reoccurring, and said their current process improvement was not effective.