CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, staff interviews, resident, facility, and staff record reviews, and the facility's policy for Abuse Preve...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, staff interviews, resident, facility, and staff record reviews, and the facility's policy for Abuse Prevention/Reporting, the facility failed to protect the resident's right to be free from neglect. The facility failed to have a systematic process in place to protect Resident #1 and all residents identified as at risk, from harm or possible death. The facility failed to identify environmental risks, revise the plan of care, and develop and implement necessary and relevant interventions to protect vulnerable residents from exiting the facility without staff knowledge and supervision. This created a likelihood that Resident #1, or any other vulnerable at-risk resident, could leave the facility undetected and suffer serious physical harm. The facility census was 57 residents on 6/12/24; eight of whom had been identified as an elopement risk and fitted with a wander monitoring device.
On 2/9/23, Resident #1 was admitted to the facility and was assessed as at risk for elopement. On 2/11/23, a wander monitoring device was placed on the resident's left ankle. A 3/25/24 Minimum Data Set (MDS) assessment revealed a Brief Interview for Mental Status (BIMS) score of 00 out of 15 possible points, indicating severe cognitive impairment. On 3/29/24, at 12:50 a.m., the resident pushed open the fire exit door on the East Wing, sounding the alarm. No care plan interventions were reviewed or revised after this incident. On 4/25/24 at 2:30 p.m., Resident #1 was observed walking outside of the facility in the grass adjacent to the road. She was returned to the facility at 2:32 p.m. Her walker was discovered at the East Wing fire exit door, the same door she pushed open on 3/29/24. The door's alarm was disarmed. Keys to disarm the fire door were at the nursing station, and the door alarmed properly once armed correctly with the key. There was no investigation into why the fire exit door's alarm was disarmed. The Administrator speculated that families or staff were using the door to go outside. The key remained at the nursing station. There was no wander monitoring device sensor alarm on this door. Two of seven exits were fitted with wander monitoring device sensor alarms. Both were near the front entrance. The facility had no policy and procedure for wander monitoring devices. New orders were written for 15-minute safety checks of Resident #1 for three days. They began on 4/25 at 11:00 p.m., 8.5 hours after the event. Between 4/25 and 4/28, documentation of 15-minute checks over large blocks of time was missing. It is unknown whether safety checks were completed as ordered. No elopement drills were documented during the year preceding this event, and the only drill completed after the event was conducted almost three weeks later, on 5/15/24. Twenty-seven of 131 staff members participated. There were no additional drills between 5/15/24 and the date of survey commencement on 6/12/24. Staff orientation and annual training did not include information on elopement/wandering. After the event, 57 of 131 staff received elopement training, and 21 of 131 staff were trained in the proper use of the key for arming/disarming the fire door alarms.
Immediate Jeopardy (IJ) at a scope and severity of J (isolated) was identified at 11:10 a.m. on June 13, 2024.
On March 29, 2024 at 12:05 a.m., Immediate Jeopardy began.
On June 13, 2024 at 5:20 p.m., the Administrator was notified of the IJ determination, and Immediate Jeopardy was ongoing as of the survey exit on June 13, 2024.
The findings include:
Cross reference F689, F835, F867
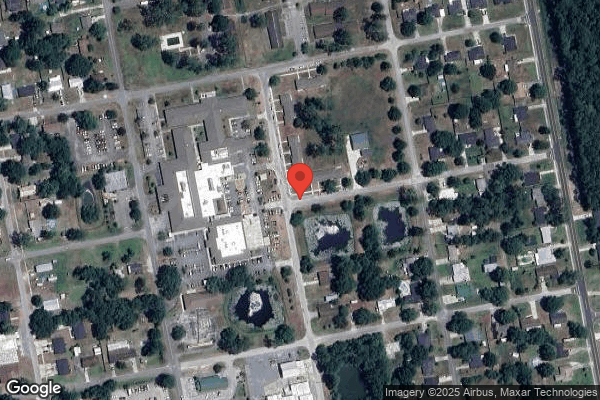
Surveyor observations made on 6/12/24 at 10:15 a.m. found the facility faced east on North 2nd Street, a residential road with no posted speed limit. East Ohio Avenue flanked the north side of the building. There was a mix of commercial and residential properties on these roads, including a detention center, rural health clinic, medical center, and the hospital, which shared a roof with the nursing home. Approximately 1/10th of a mile to the South was East Macclenny Avenue; a 2-lane commercial road with a speed limit of 30 mph. There was a detention center and additional commercial buildings on the corner of East Macclenny and 2nd Street. The facility shared a parking lot with the hospital. Upon arrival, the parking lot was full of cars, trucks, and commercial vehicles, and there were additional vehicles parked on the adjacent roadway and grassy area. Behind the building to the [NAME] was another parking lot. (Photographic evidence obtained) Upon entrance to the facility, the receptionist had to remotely unlock the front double glass sliding doors.
The surveyors began a tour of the facility on 6/12/24 at 10:30 a.m. on the south hall. The facility's residential halls were configured in a T shape. The south hall was the central hall and was just off the front lobby and administrative suites at the entrance of the building. There were two doors on the south hall near the front; one entered the hospital, and the other was a fire exit. Wander monitoring device sensors protected both doors and approximately 50 feet of the southernmost end of the hall. There were no resident rooms in the protected area. To the North was the main dining room and resident rooms. A glass fire exit door was located halfway up the hall on the west side. The door was a magnetic lock fire door and alarmed by use of a key. This door had no wander monitoring device alarm sensor. A red sticker on the door's press bar instructed, Push to open. Alarm will sound. This exit opened to an interior courtyard with an unlocked but latched gate which led to a parking lot. The hall dead-ended to the North in the restorative dining/activity room, which had two exits. One was a magnetic employee badge lock (not a fire exit) which led to a small outdoor patio with an approximately 3 1/2 foot high (unlocked but latched) gate. The second door was a magnetic lock fire door with a key-activated alarm and the same red sign instructing to press the press bar to open. Neither door was equipped with a wander monitoring device sensor. At this intersection, the east hall branched to the right, and the west hall branched to the left. Each hall ended at a glass fire door with the same key-operated magnetic lock and red sign. Neither was equipped with a wander monitoring device alarm sensor. The east door exited to a grassy area and sidewalk which went around the building to Ohio Avenue. The west door opened to a parking lot.
A record review for Resident #1 found she was admitted on [DATE] with diagnoses including, but not limited to, Alzheimer's disease, disorder of bone density and structure, hypertension, a history of falls, delusional disorder and sick sinus syndrome (a heart rhythm disorder resulting from the heart's natural pacemaker malfunctions).
A quarterly MDS assessment, dated 3/25/24, assessed Resident #1 with a brief interview for mental status (BIMS) score of 00 out of a possible 15 points, indicating severely impaired cognitive functioning for daily decision making. She had highly impaired hearing and used a hearing aid. She could walk 150 feet independently and had two falls since admission/most recent assessment. Antipsychotic medication was received routinely. A wander/elopement alarm was marked as not used, and no discharge planning to return to the community was occurring.
Resident #1 had a care plan dated 5/22/23, last revised on 3/28/24 for
Focus: Elopement Risk/Wanderer as evidenced by impaired safety awareness. The focus was revised on 4/29/24 for: Elopement on 4/25/24, returned safely to facility. The goal was to maintain her safety through the next review date of 9/11/24. Interventions included assessing for fall risk, distracting the resident from wandering by offering pleasant diversions, structured activities, food, and conversation, to identify patterns, monitor location frequently and use of a wander alert bracelet. A new intervention was added on 4/29/24 for the wander monitoring device function to be verified weekly by nursing staff. (Photographic evidence obtained)
Resident #1 had a physician's order dated 2/11/23, for Wanderguard system for safety, which was revised on 11/8/23 to include a system function test every Wednesday. Resident #1 routinely received Quetiapine Fumarate (an antipsychotic medication) 25 milligrams (mg) twice daily for paranoia and agitation (started on 11/28/23), and Zoloft (antidepressant) 25 mg every morning for depression (started 11/29/23). She also had a past order for Ativan (antianxiety) 0.5 mg every 6 hours as needed for anxiety, start on 4/5/24 and continue for 14 days (end 4/19/24). (Photographic evidence obtained)
On 4/25/24 at 11:00 p.m., the physician ordered every 15-minute visual checks for Resident #1 for three days (end 4/28/24).
Resident #1 was assessed for wandering risk on 2/9/23, 5/9/23, 8/9/23, 11/3/23, and most recently on 3/23/24 (moderate risk), 4/27/24 (high risk) and 6/9/24 (high risk). (Photographic evidence obtained)
A review of nursing progress notes for Resident #1 found the following:
On 12/9/23, Resident #1 tried to leave with another visitor, stating she had to go get her Cadillac.
On 12/4/23, Resident #1 wanted to go home, walking up and down the hall trying to find the girl who stole her radio.
On 1/2/2024, Resident #1 was yelling at staff and visitors that she wanted to leave with them and would pay them. She even asked another resident to leave with her and go to the bank. Another entry this day noted she was yelling about her Cadillac, she needed to pick her car up, she wasn't going to kill herself, but she would.
On 3/29/24, Resident #1 was attempting to get into another resident's room and was combative with staff and other residents when being redirected. She was noted as unsteady and attempted to elope out the east hall emergency exit, setting off the alarm. The physician was notified and there were pending PRN (as needed) orders. (There was no indication in the note of what those orders were.) (Photographic evidence obtained) There were no revisions to the care plan after the occurrence, and there was no further mention of the event in the electronic medical record (EMR).
On 4/18/24, Resident #1 was noted to be found sitting on the floor in the hallway with her walker in front of her. No injuries were sustained.
On 4/30/24 at 9:01 a.m., it was noted that the Interdisciplinary Team (IDT) reviewed Resident #1 having been found outside of the facility on 4/25/24. Per the review, staff observed the resident ambulating independently outside adjacent to the property on the road. The resident was returned to an activity of her choice without difficulty. Interventions included body audit, physician and family notification, verification of door alarm system, verification of wander monitoring device placement, staff education on wander monitoring devices and door checks, increased visual safety checks every 15 minutes as ordered, and door monitoring for alarm engagement as indicated.
(Photographic evidence of all nursing progress notes obtained)
Physician's progress notes dated 4/10/24 and 4/28/24, made no mention of Resident #1 pushing open the fire exit door on 3/29/24, or of her elopement on 4/25/24.
A psychiatric progress note dated 4/29/24, revealed that Resident #1 was seen for depression/refusing care, confusion, psychosis and insomnia. She was reported to be unstable with visual hallucinations and was diagnosed with neurotic depression, insomnia and anxiety disorder. The recommendation was for medications to be adjusted and monitored and continued psychiatric services for anxiety and depression. There was no mention of her attempt to exit the facility on 3/29/24, or her having exited the facility on 4/25/24.
Resident #1's medical record included a monitoring log which was utilized to document the 15-minute visual checks ordered by the physician on 4/25/24. Documentation commenced this day at 11:00 p.m. (The incident occurred at 2:30 p.m. this same day.) and continued until 4/26/24 at 9:00 p.m. then stopped. Checks resumed on 4/27/24 at 7:00 a.m. through 1:00 p.m., then stopped again. Documentation resumed on 4/28/24 at 7:00 a.m. then stopped at 1:30 p.m. In conjunction with the log, facility nurses were signing Resident #1's medication administration log/treatment administration log (MAR/TAR) on each of the two shifts daily that 15-minute checks were being completed despite no documentation on the monitoring log over large periods of time. (Photographic evidence obtained)
A review of a facility report, generated on 5/1/24 by the Nursing Home Administrator (NHA) alleging neglect, revealed that on 4/25/24, Resident #1 was seen ambulating outside the facility at 2:30 p.m. by Certified Nursing Assistant (CNA) A. She was on the facility grass and slightly on the road. CNA A asked CNA B for help and they retrieved and returned Resident #1 to the facility without difficulty. A body assessment was completed with no injuries identified, and the resident was returned to a preferred activity. The physician and family were notified. Wander monitoring device placement was verified on her left ankle, and frequent visual checks were put into place.
The facility's analysis and investigation of the incident determined that Resident #1 walked out the East wing exit door, leaving her walker inside beside the door. The east wing exit fire door alarm system required arming by key function. At the time of the resident's exit, the door alarm was found to be disengaged, therefore, it did not sound when the exit bar was pushed, and the door opened. Education was initiated for the management team and facility nurses on 4/26/24 about monitoring exit doors for alarm function. Resident #1 had a history of wandering behaviors and was already listed in the facility's elopement book. The facility verified the incident, although they included a disclaimer that they had to classify the incident as Neglect since elopement was not an option on the form. The summary of corrective actions taken included:
1. Frequent visual checks to monitor for increased wandering behaviors.
2. Education initiated for door monitoring and wander monitoring device use and function.
3. Ongoing education for elopement will be provided upon hire and annually.
4. All residents were re-evaluated for wandering risk.
(Photographic evidence obtained)
In a follow-up report generated by the NHA on 5/9/24, the incident was reclassified to Resident Elopement. It included new orders received by the physician for a 15-minute safety check for three days to monitor the resident's location and activity. It added that Resident #1 had a BIMS score of 00/15 on 3/25/24. The door was evaluated and found to be in proper working order once it was armed correctly with the key. All facility doors with alarms that required a key to alarm were also checked and found to be in proper functioning order. Education was provided to the management team and nursing staff on engaging the door alarm with the key to ensure proper functioning.
The corrective actions implemented by the facility post-incident (4/25/24) were as follows:
1. Facility reviews of the elopement policy and procedure.
2. Quotes obtained, and a project was initiated for providing upgraded wander guard (wander monitoring device) systems to the east wing, west wing, restorative dining room (doors), and south hall exit doors.
3. Verification of wander guard placement and use for all residents.
4. Review of monitoring tools for door checks, wander guard device checks.
5. Staff education on the arming of the door system with the key.
6. Continue with wander guard device checks and placement as ordered for those residents at wandering risk.
7. Staff education upon hire and quarterly of the Elopement policy and procedures.
8. Performance Improvement Plan (PIP) to assess and monitor progress of the initiatives put into place to avoid further occurrence. Review of PIP with QA&A committee for the next three-month period or until substantial compliance.
9. Review of Interdisciplinary Team (IDT) assessment upon resident admission for residents deemed to be at risk for wandering behaviors, and continuation of wandering resident assessments quarterly with updates to elopement book as required.
10. All residents re-evaluated for wandering resident risk assessment.
In response to the facility's alleged corrective actions, the facility's staff education plan and training was reviewed. Per the facility's annual in-service training calendar, abuse and neglect training were required every year in July. Elopement training was not a requirement at any time during the year. (Photographic evidence obtained)
The facility's All Staff New Hire Orientation training program/syllabus was reviewed and revealed that although it was three pages long, the facility's policies and procedures for elopement prevention and response were not included. Elder Abuse and Resident Rights training was reviewed during orientation.
A review of the facility's employee roster found there were a total of 84 staff dedicated to working in the facility, but a total of 131 shared staff between the hospital and the nursing facility. A review of employee training transcripts found that after the 4/25/24 elopement by Resident #1, only 57 of 84 facility staff and 131 combined staff had received any training in the facility's elopement prevention and response policies and procedures. (Photographic evidence obtained)
An elopement drill was conducted on 5/15/24. Only 27 of the facility's 84 staff members participated. No elopement drills were conducted in the year leading up to the incident. (Photographic evidence obtained)
Training titled Monitoring Exit Door for Alarm Function was provided between 4/26/24 and 5/15/24. Only 21 of 84 facility staff received the training. (Photographic evidence obtained)
Maintenance records were reviewed, revealing no fire door or wander monitoring device alarm system checks had been documented leading up to the incident on 4/25/24. A review of the fire door surveillance logs, which covered both the hospital and the nursing home fire doors, revealed that the fire doors were checked annually, most recently on 10/13/23.
An interview was conducted with CNA A on 6/12/24 at 11:00 a.m. She was sitting with several residents on the small, gated patio off the restorative dining room. CNA A explained that she was assigned to sit outside with the residents. The door from the dining room to the patio was locked when no one was outside; she let the residents in and out using her (magnetic) badge. The doors on the east and west residential halls sounded an alarm, then released, if you pushed them. She explained that residents must sign out and back in on the leave of absence (LOA) book at the nurse's station if they wanted to go out. She had never had to participate in an actual search for a missing resident, but stated there were approximately ten residents at risk for elopement. Elopement books were kept in the activity room, the nurses' stations, up at the front of the facility, and the social services director had one. The facility used wander monitoring devices; however, the only wander monitoring device sensor was up front on the south hall. There was a second one closer to the front lobby. The east, west and restorative dining room doors were locked but none had wander monitoring device sensors. In a second interview at 4:00 p.m., CNA A confirmed that she was the staff member who saw Resident #1 outside on 4/25/24. CNA A was sitting in the restorative/activity room when she saw Resident #1 walking along the sidewalk that went around the building. She got CNA B and they went out the patio gate and retrieved the resident. Resident #1 said she was going home. CNA A never heard an alarm sound. The nurses had the key to the exit doors at the nurses' station. She did not know why someone used it. The unit clerk checked those doors daily and always had. Resident #1 was exit-seeking and always said she wanted to go home. CNA A reported that she only recently received training in elopement and participated in one elopement drill since the 4/25/24 incident. Prior to that, she had not participated in an elopement drill in a long, long time. CNA A explained that the facility was trying to get things back up and running after changes in administration.
On 6/12/24 at 12:15 p.m., during an interview with the NHA, he explained that the east and west wing doors were alarmed fire exits that sounded when the doors were opened. The restorative dining room had two doors with the same alarm. If the door was pushed, it opened immediately and sounded the alarm. Staff did not use those doors; they only used the front door, even after hours. A new wander monitoring device system was being installed next month (July) on the east, west and south halls and on the restorative dining room doors. The current wander monitoring device system was for the main dining room and was located at the end of the south hall close to the front entrance. The NHA said his understanding was that there had been an elopement a long time ago. In response, a wander monitoring device system was installed in the front, but not the back, of the facility. There had been no other elopements since he had been employed by the facility. The maintenance department checked all fire doors and administration checked the wander monitoring device system sensors. He said the unit clerk checked the doors daily, Monday through Friday, to ensure they were armed. Before the elopement, no one was documenting those inspections. He thought the charge nurse checked the doors on the weekends. Now, wander zones and all exit door alarms were inspected daily and documented. The nurses kept the key to the fire doors at the east and west wing nurses' stations and maintenance had a key. When the fire exit door opened, the alarm sounded, and the door closed behind the person exiting. A key was required to deactivate the alarm. It made a beeping sound. The door must also be re-armed using the key. No one should go out those doors for any reason, and as far as he was aware, no one was. The NHA then admitted seeing a chair outside of the east wing door for some time, but he didn't really think anything about it. He never saw anyone out there and thought maybe family members liked to sit out there and watch the ducks. Now, in hindsight, he could only assume someone was going out that door to smoke. No one admitted using that door before the incident. He reviewed the facility's camera footage of the day before the event, but it did not reveal anyone using the door. The cameras at the end of the hall did not have a time stamp on the footage and he was not sure how much memory they had. When asked if he only reviewed one day of footage, the NHA confirmed that he had not reviewed prior days to see when the door may have been utilized. Upon suggestion, the NHA acknowledged the likelihood that the door was disarmed for longer than a day.
An interview was attempted with Resident #1 on 6/12/24 at 2:00 p.m. When asked what her name was and how she was doing, she was unable to answer. She spoke at length as though she could not hear, despite efforts to speak as loudly as possible. Resident #1 then asked, Where is the other one? She was advised, In the conference room. Resident #1 laughed, then asked if this surveyor had ever been upstairs (building is single story). She explained that it was beautiful up there. As the conversation continued, it was evident that Resident #1 had trouble understanding what was being said to her as well as disorganized thinking. As her confusion increased, the interview was concluded. Resident #1 then said, Tell your sister I love her. I hope you come back.
In an interview with the NHA on 6/12/24 at 2:55 p.m., he was asked if any additional elopement drills had been conducted, aside from the drill dated 5/15/24. He replied no but was asked to double-check over the last year to verify. He confirmed that there were no drills conducted in the last year; he had none to share.
CNA B was interviewed on 6/12/24 at 4:03 p.m. She confirmed that she assisted CNA A with retrieving Resident #1 from the sidewalk on 4/25/24. She had been on the south hall and never heard an alarm sound. CNA B stated she had not participated in an elopement drill until after the 4/25/24 incident. The key for the fire exit doors was kept at the nurses' station. Those doors would only be used in the event of a fire. The facility was admitting more and more residents who wandered compared to past admissions. Resident #1 wandered and wanted to go home or get her car. The wander monitoring device alarm was at the end of the south hall but there were none on the east or west halls.
CNA C was interviewed on 6/12/24 at 4:05 p.m. and stated she had not participated in an elopement drill in the past year until the drill on 5/15/24. The fire door alarm key was at the nurses' station and the alarm sounded when the door was opened. CNA C could not provide a reason for why the key would be used to disarm the doors. She assisted with daily door checks, and they had been conducting those for a long time. They were now documenting them.
During an interview with the NHA on 6/13/24 at 9:38 a.m., he was asked about his investigation into Resident #1's 4/25/24 elopement. He returned at 9:50 a.m. and explained that CNA A saw Resident #1 hovering by the road in the grass outside of the activities/restorative dining room. She called for CNA B, told her the resident was outside, and they got her safely back inside. In response, a body check was performed. The door function was checked, and it (the alarm) didn't sound. He said, Resident #1's wander guard bracelet was checked, although that bracelet means nothing for those doors; only for the front. The NHA stated that prompted him to inquire about the door checks, which there was no documentation for up to the event. Staff just reported they were conducting them. The NHA implemented daily fire and exit door checks that same day. He then began training staff on the Wandering Resident policy, which he had reviewed and updated on 4/26/24. He made it more user and reader-friendly and included a major change, which was that the search for a missing resident could not exceed 10 minutes prior to notification. That gave staff an opportunity to search for the resident prior to calling him. This change shortened the time from the previous 15-minute search. Staff should also check the LOA (leave of absence) book to see if the resident signed out with family. The NHA put this policy in the electronic staff training database and set a deadline for all staff to complete the training by 5/31/24. When he printed the transcripts for the survey team's review on 6/13/24, he realized not all staff had completed the required training. There was a total of 131 staff shared between the hospital and nursing home; shared staff included the dietary department, physical therapy, housekeeping and maintenance departments. Those were split departments and staff came over from the hospital to work at the nursing home. New staff orientation training was provided by Human Resources (HR). The NHA was asked if he noticed there was no elopement training included in the new hire orientation packet. He said yes and had already spoken with HR and planned to change that. The NHA said he reviewed the elopement policy with staff during the May elopement drill. When asked how he was keeping the residents at risk safe, he replied that a new wander monitoring device system would be installed, and he was making sure the doors were being checked and documented every morning. The Risk Manager (RM) received the log, checked it, and brought it to the Friday meeting for review. The Social Services Director (SSD) reviewed and updated the elopement books weekly, upon significant change or new admission, and reviewed those at the meeting. When asked how the facility identified residents at risk, the NHA stated risk was usually identified by family or hospital admission papers. He was not sure if nurses used a wandering or elopement assessment. He called the Director of Nursing (DON), who reported that residents were assessed on admission and quarterly. The NHA added as part of his investigation that he obtained a written statement from CNA A, the only direct witness to Resident #1's elopement. When asked about his investigation into how or why the door was unlocked, he said he was still trying to figure out when the nurse last locked it. He wondered if they waited for the beep, beep, beep sound that indicated it was armed, or if someone forgot to lock it altogether. They hadn't figured that out. He again asserted that doors should not be disarmed for any reason, and staff did not use those doors. When asked if he retrained nurses in situations where the fire doors should be used, he said no; just to check the doors, properly arm them and wait for the three beeps when turning the alarm back on. The nurses had the key to turn off the alarm if a resident exited through those doors. When asked if CNAs could use the key, he said yes, but usually a nurse did. The NHA was asked if he was made aware that Resident #1 successfully opened that door a month prior to the incident (on 3/29/24). He said he had not been told that, but she was a wanderer, so he believed that happened. The NHA said the day after the 4/25/24 incident, they happened to have a QAPI (Quality Assurance and Performance Improvement) meeting. They reviewed the incident and developed a Performance Improvement Plan (PIP). When asked if the facility had identified a root cause analysis (RCA), he did not know but said he would provide that information.
The Risk Manager (RM) was interviewed on 6/13/24 at 10:30 a.m. and shared the QAPI meeting information at that time. She explained that the committee, including the Medical Director, met on 4/26/24 and reviewed the 4/25/24 incident. They covered the facts of the situation and did a drill down for the time the resident was seen inside versus outside. The committee looked at recent changes in medications and increased behaviors. Resident #1 did experience anxiety, wanted to go home, and was functionally able to move around. They spoke with the activities staff about continuing to redirect Resident #1 (to activities) and spoke with her family to encourage their visits. Residents' locations were verified immediately following the event, and every door was inspected and armed, including the badge-in, badge-out doors. The committee also reviewed processes moving forward with the wander monitoring device system and door checks daily, as well as wander monitoring device checks. Those devices were checked for function weekly and for placement every shift. The RCA focused on the door that had been disarmed with the key, but facility management could not determine who disarmed the door alarm. It had not been re-armed correctly. We did all-staff education that day with the staff on duty. The RM was asked about staff not on duty and said she would have to look at the training records. Upon review of the training logs, the RM realized that only 21 staff had been trained in the use of the door alarm key. The RM was asked if the QAPI committee identified a lack of staff training on elopement prevention and response. She did not answer. The NHA interjected and implied that they had not. He said that outside of QAPI, they had reviewed and recognized the lack of elopement orientation and training for staff. They had nursing home-specific training in the works. The RM said the committee did look at education during the drill down. Since they were part of the hospital, there was a standardized orient[TRUNCATED]
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, staff interviews, resident, facility, and staff record reviews, and the facility's policy for Resident El...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, staff interviews, resident, facility, and staff record reviews, and the facility's policy for Resident Elopement, the facility failed to provide supervision and implement sufficient interventions to maintain resident safety, prevent elopement (leaving the premises without supervision or staff knowledge) and minimize the risk of injury or death for Resident #1 and all residents identified as at risk for elopement. The facility failed to have a systematic process in place to educate staff, identify environmental risks, revise plans of care, and develop, and implement relevant interventions to protect vulnerable residents from exiting the facility without staff knowledge and supervision. The resident census was 57 on 6/12/24, eight of whom had been identified as at risk for elopement and fitted with a wander monitoring device. Only two of the seven doors to the outside were equipped with wander monitoring device sensors.
On 2/9/23, Resident #1 was admitted to the facility and was assessed as at risk for elopement. On 2/11/23, a wander monitoring device was placed on the resident's left ankle. A 3/25/24 Minimum Data Set (MDS) assessment revealed a Brief Interview for Mental Status (BIMS) score of 00 out of 15 possible points, indicating severe cognitive impairment. On 3/29/24, at 12:50 a.m., the resident pushed open the fire exit door on the East Wing, sounding the alarm. No care plan interventions were reviewed or revised after this incident. On 4/25/24 at 2:30 p.m., Resident #1 was observed walking outside of the facility in the grass adjacent to the road. She was returned to the facility at 2:32 p.m. Her walker was discovered at the East Wing fire exit door, the same door she pushed open on 3/29/24. The door's alarm was disarmed. Keys to disarm the fire door were at the nursing station, and the door alarmed properly once armed correctly with the key. There was no investigation into why the fire exit door's alarm was disarmed. The Administrator speculated that families or staff were using the door to go outside. The key remained at the nursing station. There was no wander monitoring device sensor alarm on this door. Two of seven exits were fitted with wander monitoring device sensor alarms. Both were near the front entrance. The facility had no policy and procedure for wander monitoring devices. New orders were written for 15-minute safety checks of Resident #1 for three days. They began on 4/25 at 11:00 p.m., 8.5 hours after the event. Between 4/25 and 4/28, documentation of 15-minute checks over large blocks of time was missing. It is unknown whether safety checks were completed as ordered. No elopement drills were documented during the year preceding this event, and the only drill completed after the event was conducted almost three weeks later, on 5/15/24. Twenty-seven of 131 staff members participated. There were no additional drills between 5/15/24 and the date of survey commencement on 6/12/24. Staff orientation and annual training did not include information on elopement/wandering. After the event, 57 of 131 staff received elopement training, and 21 of 131 staff were trained in the proper use of the key for arming/disarming the fire door alarms.
Immediate Jeopardy (IJ) at a scope and severity of J (isolated) was identified at 11:10 a.m. on June 13, 2024.
On March 29, 2024 at 12:05 a.m., Immediate Jeopardy began.
On June 13, 2024 at 5:20 p.m., the Administrator was notified of the IJ determination, and Immediate Jeopardy was ongoing as of the survey exit on June 13, 2024.
The findings include:
Cross reference F600, F835, F867
Surveyor observations made on 6/12/24 at 10:15 a.m. found the facility faced east on North 2nd Street, a residential road with no posted speed limit. East Ohio Avenue flanked the north side of the building. There was a mix of commercial and residential properties on these roads, including a detention center, rural health clinic, medical center, and the hospital, which shared a roof with the nursing home. Approximately 1/10th of a mile to the South was East Macclenny Avenue; a 2-lane commercial road with a speed limit of 30 mph. There was a detention center and additional commercial buildings on the corner of East Macclenny and 2nd Street. The facility shared a parking lot with the hospital. Upon arrival, the parking lot was full of cars, trucks, and commercial vehicles, and there were additional vehicles parked on the adjacent roadway and grassy area. Behind the building to the [NAME] was another parking lot. (Photographic evidence obtained) Upon entrance to the facility, the receptionist had to remotely unlock the front double glass sliding doors.
The surveyors began a tour of the facility on 6/12/24 at 10:30 a.m. on the south hall. The facility's residential halls were configured in a T shape. The south hall was the central hall and was just off the front lobby and administrative suites at the entrance of the building. There were two doors on the south hall near the front; one entered the hospital, and the other was a fire exit. Wander monitoring device sensors protected both doors and approximately 50 feet of the southernmost end of the hall. There were no resident rooms in the protected area. To the North was the main dining room and resident rooms. A glass fire exit door was located halfway up the hall on the west side. The door was a magnetic lock fire door and alarmed by use of a key. This door had no wander monitoring device alarm sensor. A red sticker on the door's press bar instructed, Push to open. Alarm will sound. This exit opened to an interior courtyard with an unlocked but latched gate which led to a parking lot. The hall dead-ended to the North in the restorative dining/activity room, which had two exits. One was a magnetic employee badge lock (not a fire exit) which led to a small outdoor patio with an approximately 3 1/2 foot high (unlocked but latched) gate. The second door was a magnetic lock fire door with a key-activated alarm and the same red sign instructing to press the press bar to open. Neither door was equipped with a wander monitoring device sensor. At this intersection, the east hall branched to the right, and the west hall branched to the left. Each hall ended at a glass fire door with the same key-operated magnetic lock and red sign. Neither was equipped with a wander monitoring device alarm sensor. The east door exited to a grassy area and sidewalk which went around the building to Ohio Avenue. The west door opened to a parking lot.
A record review for Resident #1 found she was admitted on [DATE] with diagnoses including, but not limited to, Alzheimer's disease, disorder of bone density and structure, hypertension, a history of falls, delusional disorder and sick sinus syndrome (a heart rhythm disorder resulting from the heart's natural pacemaker malfunctions).
A quarterly MDS assessment, dated 3/25/24, assessed Resident #1 with a brief interview for mental status (BIMS) score of 00 out of a possible 15 points, indicating severely impaired cognitive functioning for daily decision making. She had highly impaired hearing and used a hearing aid. She could walk 150 feet independently and had two falls since admission/most recent assessment. Antipsychotic medication was received routinely. A wander/elopement alarm was marked as not used, and no discharge planning to return to the community was occurring.
Resident #1 had a care plan dated 5/22/23, last revised on 3/28/24 for
Focus: Elopement Risk/Wanderer as evidenced by impaired safety awareness. The focus was revised on 4/29/24 for: Elopement on 4/25/24, returned safely to facility. The goal was to maintain her safety through the next review date of 9/11/24. Interventions included assessing for fall risk, distracting the resident from wandering by offering pleasant diversions, structured activities, food, and conversation, to identify patterns, monitor location frequently and use of a wander alert bracelet. A new intervention was added on 4/29/24 for the wander monitoring device function to be verified weekly by nursing staff. (Photographic evidence obtained)
Resident #1 had a physician's order dated 2/11/23, for Wanderguard system for safety, which was revised on 11/8/23 to include a system function test every Wednesday. Resident #1 routinely received Quetiapine Fumarate (an antipsychotic medication) 25 milligrams (mg) twice daily for paranoia and agitation (started on 11/28/23), and Zoloft (antidepressant) 25 mg every morning for depression (started 11/29/23). She also had a past order for Ativan (antianxiety) 0.5 mg every 6 hours as needed for anxiety, start on 4/5/24 and continue for 14 days (end 4/19/24). (Photographic evidence obtained)
On 4/25/24 at 11:00 p.m., the physician ordered every 15-minute visual checks for Resident #1 for three days (end 4/28/24). A review of the monitoring log used to document the 15-minute visual checks found documentation started on 4/25/24 at 11:00 p.m. Visual checks continued until 4/26/24 at 9:00 p.m. then stopped. Checks resumed on 4/27/24 at 7:00 a.m. through 1:00 p.m., then stopped again. Documentation resumed on 4/28/24 at 7:00 a.m. then stopped at 1:30 p.m. In conjunction with the log, facility nurses were signing Resident #1's medication administration log/treatment administration log (MAR/TAR) on each of the two shifts daily that 15-minute checks were being completed, despite no documentation on the monitoring log for large periods of time. (Photographic evidence obtained)
Resident #1 was assessed for wandering risk on 2/9/23, 5/9/23, 8/9/23, 11/3/23, and most recently on 3/23/24 (moderate risk), 4/27/24 (high risk) and 6/9/24 (high risk). (Photographic evidence obtained)
A review of nursing progress notes for Resident #1 found the following:
On 12/9/23, Resident #1 tried to leave with another visitor, stating she had to go get her Cadillac.
On 12/4/23, Resident #1 wanted to go home, walking up and down the hall trying to find the girl who stole her radio.
On 1/2/2024, Resident #1 was yelling at staff and visitors that she wanted to leave with them and would pay them. She even asked another resident to leave with her and go to the bank. Another entry this day noted she was yelling about her Cadillac, she needed to pick her car up, she wasn't going to kill herself, but she would.
On 3/29/24, Resident #1 was attempting to get into another resident's room and was combative with staff and other residents when being redirected. She was noted as unsteady and attempted to elope out the east hall emergency exit, setting off the alarm. The physician was notified and there were pending PRN (as needed) orders. (There was no indication in the note of what those orders were.) (Photographic evidence obtained) There were no revisions to the care plan after the occurrence, and there was no further mention of the event in the electronic medical record (EMR).
On 4/18/24, Resident #1 was noted to be found sitting on the floor in the hallway with her walker in front of her. No injuries were sustained.
On 4/30/24 at 9:01 a.m., it was noted that the Interdisciplinary Team (IDT) reviewed Resident #1 having been found outside of the facility on 4/25/24. Per the review, staff observed the resident ambulating independently outside adjacent to the property on the road. The resident was returned to an activity of her choice without difficulty. Interventions included body audit, physician and family notification, verification of door alarm system, verification of wander monitoring device placement, staff education on wander monitoring devices and door checks, increased visual safety checks every 15 minutes as ordered, and door monitoring for alarm engagement as indicated.
(Photographic evidence of all nursing progress notes obtained)
Physician's progress notes dated 4/10/24 and 4/28/24, made no mention of Resident #1 pushing open the fire exit door on 3/29/24, or of her elopement on 4/25/24.
A psychiatric progress note dated 4/29/24, revealed that Resident #1 was seen for depression/refusing care, confusion, psychosis and insomnia. She was reported to be unstable with visual hallucinations and was diagnosed with neurotic depression, insomnia and anxiety disorder. The recommendation was for medications to be adjusted and monitored and continued psychiatric services for anxiety and depression. There was no mention of her attempt to exit the facility on 3/29/24, or her having exited the facility on 4/25/24.
A review of a facility report, generated on 5/1/24 by the Nursing Home Administrator (NHA) alleging neglect, revealed that on 4/25/24, Resident #1 was seen ambulating outside the facility at 2:30 p.m. by Certified Nursing Assistant (CNA) A. She was on the facility grass and slightly on the road. CNA A asked CNA B for help and they retrieved and returned Resident #1 to the facility without difficulty. A body assessment was completed with no injuries identified, and the resident was returned to a preferred activity. The physician and family were notified. Wander monitoring device placement was verified on her left ankle, and frequent visual checks were put into place.
The facility's analysis and investigation of the incident determined that Resident #1 walked out the East wing exit door, leaving her walker inside beside the door. The east wing exit fire door alarm system required arming by key function. At the time of the resident's exit, the door alarm was found to be disengaged, therefore, it did not sound when the exit bar was pushed, and the door opened. Education was initiated for the management team and facility nurses on 4/26/24 about monitoring exit doors for alarm function. Resident #1 had a history of wandering behaviors and was already listed in the facility's elopement book. The facility verified the incident, although they included a disclaimer that they had to classify the incident as Neglect since elopement was not an option on the form. The summary of corrective actions taken included:
1. Frequent visual checks to monitor for increased wandering behaviors.
2. Education initiated for door monitoring and wander monitoring device use and function.
3. Ongoing education for elopement will be provided upon hire and annually.
4. All residents were re-evaluated for wandering risk.
(Photographic evidence obtained)
In a follow-up report generated by the NHA on 5/9/24, the incident was reclassified to Resident Elopement. It included new orders received by the physician for a 15-minute safety check for three days to monitor the resident's location and activity. It added that Resident #1 had a BIMS score of 00/15 on 3/25/24. The door was evaluated and found to be in proper working order once it was armed correctly with the key. All facility doors with alarms that required a key to alarm were also checked and found to be in proper functioning order. Education was provided to the management team and nursing staff on engaging the door alarm with the key to ensure proper functioning.
The corrective actions implemented by the facility post-incident (4/25/24) were as follows:
1. Facility reviews of the elopement policy and procedure.
2. Quotes obtained, and a project was initiated for providing upgraded wander guard (wander monitoring device) systems to the east wing, west wing, restorative dining room (doors), and south hall exit doors.
3. Verification of wander guard placement and use for all residents.
4. Review of monitoring tools for door checks, wander guard device checks.
5. Staff education on the arming of the door system with the key.
6. Continue with wander guard device checks and placement as ordered for those residents at wandering risk.
7. Staff education upon hire and quarterly of the Elopement policy and procedures.
8. Performance Improvement Plan (PIP) to assess and monitor progress of the initiatives put into place to avoid further occurrence. Review of PIP with QA&A committee for the next three-month period or until substantial compliance.
9. Review of Interdisciplinary Team (IDT) assessment upon resident admission for residents deemed to be at risk for wandering behaviors, and continuation of wandering resident assessments quarterly with updates to elopement book as required.
10. All residents re-evaluated for wandering resident risk assessment.
In response to the facility's alleged corrective actions, the facility's staff education plan and training was reviewed. Per the facility's annual in-service training calendar, abuse and neglect training were required every year in July. Elopement training was not a requirement at any time during the year. (Photographic evidence obtained)
The facility's All Staff New Hire Orientation training program/syllabus was reviewed and revealed that although it was three pages long, the facility's policies and procedures for elopement prevention and response were not included. Elder Abuse and Resident Rights training was reviewed during orientation.
A review of the facility's employee roster found there were a total of 84 staff dedicated to working in the facility, but a total of 131 shared staff between the hospital and the nursing facility. A review of employee training transcripts found that after the 4/25/24 elopement by Resident #1, only 57 of 84 facility staff and 131 combined staff had received any training in the facility's elopement prevention and response policies and procedures. (Photographic evidence obtained)
An elopement drill was conducted on 5/15/24. Only 27 of the facility's 84 staff members participated. No elopement drills were conducted in the year leading up to the incident. (Photographic evidence obtained)
Training titled Monitoring Exit Door for Alarm Function was provided between 4/26/24 and 5/15/24. Only 21 of 84 facility staff received the training. (Photographic evidence obtained)
Maintenance records were reviewed, revealing no fire door or wander monitoring device alarm system checks had been documented leading up to the incident on 4/25/24. A review of the fire door surveillance logs, which covered both the hospital and the nursing home fire doors, revealed that the fire doors were checked annually, most recently on 10/13/23.
An interview was conducted with CNA A on 6/12/24 at 11:00 a.m. She was sitting with several residents on the small, gated patio off the restorative dining room. CNA A explained that she was assigned to sit outside with the residents. The door from the dining room to the patio was locked when no one was outside; she let the residents in and out using her (magnetic) badge. The doors on the east and west residential halls sounded an alarm, then released, if you pushed them. She explained that residents must sign out and back in on the leave of absence (LOA) book at the nurse's station if they wanted to go out. She had never had to participate in an actual search for a missing resident, but stated there were approximately ten residents at risk for elopement. Elopement books were kept in the activity room, the nurses' stations, up at the front of the facility, and the social services director had one. The facility used wander monitoring devices; however, the only wander monitoring device sensor was up front on the south hall. There was a second one closer to the front lobby. The east, west and restorative dining room doors were locked but none had wander monitoring device sensors. In a second interview at 4:00 p.m., CNA A confirmed that she was the staff member who saw Resident #1 outside on 4/25/24. CNA A was sitting in the restorative/activity room when she saw Resident #1 walking along the sidewalk that went around the building. She got CNA B and they went out the patio gate and retrieved the resident. Resident #1 said she was going home. CNA A never heard an alarm sound. The nurses had the key to the exit doors at the nurses' station. She did not know why someone used it. The unit clerk checked those doors daily and always had. Resident #1 was exit-seeking and always said she wanted to go home. CNA A reported that she only recently received training in elopement and participated in one elopement drill since the 4/25/24 incident. Prior to that, she had not participated in an elopement drill in a long, long time. CNA A explained that the facility was trying to get things back up and running after changes in administration.
On 6/12/24 at 12:15 p.m., during an interview with the NHA, he explained that the east and west wing doors were alarmed fire exits that sounded when the doors were opened. The restorative dining room had two doors with the same alarm. If the door was pushed, it opened immediately and sounded the alarm. Staff did not use those doors; they only used the front door, even after hours. A new wander monitoring device system was being installed next month (July) on the east, west and south halls and on the restorative dining room doors. The current wander monitoring device system was for the main dining room and was located at the end of the south hall close to the front entrance. The NHA said his understanding was that there had been an elopement a long time ago. In response, a wander monitoring device system was installed in the front, but not the back, of the facility. There had been no other elopements since he had been employed by the facility. The maintenance department checked all fire doors and administration checked the wander monitoring device system sensors. He said the unit clerk checked the doors daily, Monday through Friday, to ensure they were armed. Before the elopement, no one was documenting those inspections. He thought the charge nurse checked the doors on the weekends. Now, wander zones and all exit door alarms were inspected daily and documented. The nurses kept the key to the fire doors at the east and west wing nurses' stations and maintenance had a key. When the fire exit door opened, the alarm sounded, and the door closed behind the person exiting. A key was required to deactivate the alarm. It made a beeping sound. The door must also be re-armed using the key. No one should go out those doors for any reason, and as far as he was aware, no one was. The NHA then admitted seeing a chair outside of the east wing door for some time, but he didn't really think anything about it. He never saw anyone out there and thought maybe family members liked to sit out there and watch the ducks. Now, in hindsight, he could only assume someone was going out that door to smoke. No one admitted using that door before the incident. He reviewed the facility's camera footage of the day before the event, but it did not reveal anyone using the door. The cameras at the end of the hall did not have a time stamp on the footage and he was not sure how much memory they had. When asked if he only reviewed one day of footage, the NHA confirmed that he had not reviewed prior days to see when the door may have been utilized. Upon suggestion, the NHA acknowledged the likelihood that the door was disarmed for longer than a day.
An interview was attempted with Resident #1 on 6/12/24 at 2:00 p.m. When asked what her name was and how she was doing, she was unable to answer. She spoke at length as though she could not hear, despite efforts to speak as loudly as possible. Resident #1 then asked, Where is the other one? She was advised, In the conference room. Resident #1 laughed, then asked if this surveyor had ever been upstairs (building is single story). She explained that it was beautiful up there. As the conversation continued, it was evident that Resident #1 had trouble understanding what was being said to her as well as disorganized thinking. As her confusion increased, the interview was concluded. Resident #1 then said, Tell your sister I love her. I hope you come back.
In an interview with the NHA on 6/12/24 at 2:55 p.m., he was asked if any additional elopement drills had been conducted, aside from the drill dated 5/15/24. He replied no but was asked to double-check over the last year to verify. He confirmed that there were no drills conducted in the last year; he had none to share.
CNA B was interviewed on 6/12/24 at 4:03 p.m. She confirmed that she assisted CNA A with retrieving Resident #1 from the sidewalk on 4/25/24. She had been on the south hall and never heard an alarm sound. CNA B stated she had not participated in an elopement drill until after the 4/25/24 incident. The key for the fire exit doors was kept at the nurses' station. Those doors would only be used in the event of a fire. The facility was admitting more and more residents who wandered compared to past admissions. Resident #1 wandered and wanted to go home or get her car. The wander monitoring device alarm was at the end of the south hall but there were none on the east or west halls.
CNA C was interviewed on 6/12/24 at 4:05 p.m. and stated she had not participated in an elopement drill in the past year until the drill on 5/15/24. The fire door alarm key was at the nurses' station and the alarm sounded when the door was opened. CNA C could not provide a reason for why the key would be used to disarm the doors. She assisted with daily door checks, and they had been conducting those for a long time. They were now documenting them.
During an interview with the NHA on 6/13/24 at 9:38 a.m., he was asked about his investigation into Resident #1's 4/25/24 elopement. He returned at 9:50 a.m. and explained that CNA A saw Resident #1 hovering by the road in the grass outside of the activities/restorative dining room. She called for CNA B, told her the resident was outside, and they got her safely back inside. In response, a body check was performed. The door function was checked, and it (the alarm) didn't sound. He said, Resident #1's wander guard bracelet was checked, although that bracelet means nothing for those doors; only for the front. The NHA stated that prompted him to inquire about the door checks, which there was no documentation for up to the event. Staff just reported they were conducting them. The NHA implemented daily fire and exit door checks that same day. He then began training staff on the Wandering Resident policy, which he had reviewed and updated on 4/26/24. The NHA put this policy in the electronic staff training database and set a deadline for all staff to complete the training by 5/31/24. When he printed the transcripts for the survey team's review on 6/13/24, he realized not all staff had completed the required training. There was a total of 131 staff shared between the hospital and nursing home; shared staff included the dietary department, physical therapy, housekeeping and maintenance departments. Those were split departments and staff came over from the hospital to work at the nursing home. New staff orientation training was provided by Human Resources (HR). The NHA was asked if he noticed there was no elopement training included in the new hire orientation packet. He said yes and had already spoken with HR and planned to change that. The NHA said he reviewed the elopement policy with staff during the May elopement drill. When asked how he was keeping the residents at risk safe, he replied that a new wander monitoring device system would be installed, and he was making sure the doors were being checked and documented every morning. The Risk Manager (RM) received the log, checked it, and brought it to the Friday meeting for review. The Social Services Director (SSD) reviewed and updated the elopement books weekly, upon significant change or new admission, and reviewed those at the meeting. When asked how the facility identified residents at risk, the NHA stated risk was usually identified by family or hospital admission papers.
He was not sure if nurses used a wandering or elopement assessment. He called the Director of Nursing (DON), who reported that residents were assessed on admission and quarterly. The NHA added as part of his investigation that he obtained a written statement from CNA A, the only direct witness to Resident #1's elopement. When asked about his investigation into how or why the door was unlocked, he said he was still trying to figure out when the nurse last locked it. He wondered if they waited for the beep, beep, beep sound that indicated it was armed, or if someone forgot to lock it altogether. They hadn't figured that out. He again asserted that doors should not be disarmed for any reason, and staff did not use those doors. When asked if he retrained nurses in situations where the fire doors should be used, he said no; just to check the doors, properly arm them and wait for the three beeps when turning the alarm back on. The nurses had the key to turn off the alarm if a resident exited through those doors. When asked if CNAs could use the key, he said yes, but usually a nurse did. The NHA was asked if he was made aware that Resident #1 successfully opened that door a month prior to the incident (on 3/29/24). He said he had not been told that, but she was a wanderer, so he believed that happened. The NHA said the day after the 4/25/24 incident, they happened to have a QAPI (Quality Assurance and Performance Improvement) meeting. They reviewed the incident and developed a Performance Improvement Plan (PIP). When asked if the facility had identified a root cause analysis (RCA), he did not know but said he would provide that information.
The Risk Manager (RM) was interviewed on 6/13/24 at 10:30 a.m. and shared the QAPI meeting information at that time. She explained that the committee, including the Medical Director, met on 4/26/24 and reviewed the 4/25/24 incident. They covered the facts of the situation and did a drill down for the time the resident was seen inside versus outside. The committee looked at recent changes in medications and increased behaviors. Resident #1 did experience anxiety, wanted to go home, and was functionally able to move around. They spoke with the activities staff about continuing to redirect Resident #1 (to activities) and spoke with her family to encourage their visits. Residents' locations were verified immediately following the event, and every door was inspected and armed, including the badge-in, badge-out doors. The committee also reviewed processes moving forward with the wander monitoring device system and door checks daily, as well as wander monitoring device checks. Those devices were checked for function weekly and for placement every shift. The RCA focused on the door that had been disarmed with the key, but facility management could not determine who disarmed the door alarm. It had not been re-armed correctly. We did all-staff education that day with the staff on duty. The RM was asked about staff not on duty and said she would have to look at the training records. Upon review of the training logs, the RM realized that only 21 staff had been trained in the use of the door alarm key. The RM was asked if the QAPI committee identified a lack of staff training on elopement prevention and response. She did not answer. The NHA interjected and implied that they had not. He said that outside of QAPI, they had reviewed and recognized the lack of elopement orientation and training for staff. They had nursing home-specific training in the works. The RM said the committee did look at education during the drill down. Since they were part of the hospital, there was a standardized orientation training program. Moving forward, they would provide elopement training during the new hire orientation. When asked if the committee considered training current staff and having them participate in elopement drills, she deferred to the NHA who did not respond. Instead, the DON (also present in the room) answered. She stated nursing home staff training was now being separated from the hospital and infection control training. The Staff Development nurse would train new hires and conduct quarterly
CRITICAL
(L)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Administration
(Tag F0835)
Someone could have died · This affected most or all residents
⚠️ Facility-wide issue
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, staff interviews, resident, facility, and staff record reviews, the facility's policy Resident Elopement,...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, staff interviews, resident, facility, and staff record reviews, the facility's policy Resident Elopement, the Facility Assessment, and the Administrator's job description, the facility administration failed to provide sufficient oversight, identify needed resources and ensure staff were sufficiently equipped to provide adequate supervision and implement relevant measures to prevent elopement (leaving the premises without supervision or staff knowledge) and minimize the risk of injury or death for Resident #1 and all seven of the other residents identified as at risk for elopement. The facility failed to have a systematic process in place to educate staff, identify environmental risks, revise plans of care, and develop, and implement relevant interventions to protect residents from exiting the facility without staff knowledge or supervision. The resident census was 57 on 6/12/24, eight of whom had been identified as at risk for elopement and fitted with a wander monitoring device.
On 2/9/23, Resident #1 was admitted to the facility and was assessed as at risk for elopement. On 2/11/23, a wander monitoring device was placed on the resident's left ankle. A 3/25/24 Minimum Data Set (MDS) assessment revealed a Brief Interview for Mental Status (BIMS) score of 00 out of 15 possible points, indicating severe cognitive impairment. On 3/29/24, at 12:50 a.m., the resident pushed open the fire exit door on the East Wing, sounding the alarm. No care plan interventions were reviewed or revised after this incident. On 4/25/24 at 2:30 p.m., Resident #1 was observed walking outside of the facility in the grass adjacent to the road. She was returned to the facility at 2:32 p.m. Her walker was discovered at the East Wing fire exit door, the same door she pushed open on 3/29/24. The door's alarm was disarmed. Keys to disarm the fire door were at the nursing station, and the door alarmed properly once armed correctly with the key. There was no investigation into why the fire exit door's alarm was disarmed. The Administrator speculated that families or staff were using the door to go outside. The key remained at the nursing station. There was no wander monitoring device sensor alarm on this door. Two of seven exits were fitted with wander monitoring device sensor alarms. Both were near the front entrance. The facility had no policy and procedure for wander monitoring devices. New orders were written for 15-minute safety checks of Resident #1 for three days. They began on 4/25 at 11:00 p.m., 8.5 hours after the event. Between 4/25 and 4/28, documentation of 15-minute checks over large blocks of time was missing. It is unknown whether safety checks were completed as ordered. No elopement drills were documented during the year preceding this event, and the only drill completed after the event was conducted almost three weeks later, on 5/15/24. Twenty-seven of 131 staff members participated. There were no additional drills between 5/15/24 and the date of survey commencement on 6/12/24. Staff orientation and annual training did not include information on elopement/wandering. After the event, 57 of 131 staff received elopement training, and 21 of 131 staff were trained in the proper use of the key for arming/disarming the fire door alarms.
Immediate Jeopardy (IJ) at a scope and severity of L (widespread) was identified at 11:10 a.m. on June 13, 2024.
On March 29, 2024 at 12:05 a.m., Immediate Jeopardy began.
On June 13, 2024 at 5:20 p.m., the Administrator was notified of the IJ determination, and Immediate Jeopardy was ongoing as of the survey exit on June 13, 2024.
The findings include:
Cross reference F600, F689, F867
During a tour of the facility on 6/12/24 at 10:30 a.m. on the South hallway just off the front lobby, there were wander monitoring device sensors installed on both doors and protecting approximately 50 feet of the southernmost end of the hall. A glass fire exit door was located halfway up the hall on the west side. The door was a magnetic lock fire door and alarmed by use of a key. This door had no wander monitoring device alarm sensor. A red sticker on the door's press bar instructed, Push to open. Alarm will sound. This exit opened to an interior courtyard with an unlocked but latched gate which led to a parking lot. The hall dead-ended to the North in the restorative dining/activity room, which had two exits. One was a magnetic employee badge lock (not a fire exit) which led to a small outdoor patio with an approximately 3 1/2 foot high (unlocked but latched) gate. The second door was a magnetic lock fire door with a key-activated alarm and the same red sign instructing to press the press bar to open. Neither door was equipped with a wander monitoring device sensor. At this intersection, the east hall branched to the right, and the west hall branched to the left. Each hall ended at a glass fire door with the same key-operated magnetic lock and red sign. Neither was equipped with a wander monitoring device alarm sensor. The east door exited to a grassy area and sidewalk which went around the building to Ohio Avenue. The west door opened to a parking lot.
A record review for Resident #1 found she was admitted on [DATE] with diagnoses including, but not limited to, Alzheimer's disease, disorder of bone density and structure, hypertension, a history of falls, delusional disorder and sick sinus syndrome (a heart rhythm disorder resulting from the heart's natural pacemaker malfunctions).
A quarterly MDS assessment, dated 3/25/24, assessed Resident #1 with a brief interview for mental status (BIMS) score of 00 out of a possible 15 points, indicating severely impaired cognitive functioning for daily decision making. She had highly impaired hearing and used a hearing aid. She could walk 150 feet independently and had two falls since admission/most recent assessment. Antipsychotic medication was received routinely. A wander/elopement alarm was marked as not used, and no discharge planning to return to the community was occurring.
Resident #1 had a care plan dated 5/22/23, last revised on 3/28/24 for
Focus: Elopement Risk/Wanderer as evidenced by impaired safety awareness. The focus was revised on 4/29/24 for: Elopement on 4/25/24, returned safely to facility. The goal was to maintain her safety through the next review date of 9/11/24. Interventions included assessing for fall risk, distracting the resident from wandering by offering pleasant diversions, structured activities, food, and conversation, to identify patterns, monitor location frequently and use of a wander alert bracelet. A new intervention was added on 4/29/24 for the wander monitoring device function to be verified weekly by nursing staff. (Photographic evidence obtained)
Resident #1 had a physician's order dated 2/11/23, for Wanderguard system for safety, which was revised on 11/8/23 to include a system function test every Wednesday. Resident #1 routinely received Quetiapine Fumarate (an antipsychotic medication) 25 milligrams (mg) twice daily for paranoia and agitation (started on 11/28/23), and Zoloft (antidepressant) 25 mg every morning for depression (started 11/29/23). She also had a past order for Ativan (antianxiety) 0.5 mg every 6 hours as needed for anxiety, start on 4/5/24 and continue for 14 days (end 4/19/24). (Photographic evidence obtained)
On 4/25/24 at 11:00 p.m., the physician ordered every 15-minute visual checks for Resident #1 for three days (end 4/28/24).
Resident #1 was assessed for wandering risk on 2/9/23, 5/9/23, 8/9/23, 11/3/23, and most recently on 3/23/24 (moderate risk), 4/27/24 (high risk) and 6/9/24 (high risk). (Photographic evidence obtained)
A review of nursing progress notes for Resident #1 found the following:
On 12/9/23, Resident #1 tried to leave with another visitor, stating she had to go get her Cadillac.
On 12/4/23, Resident #1 wanted to go home, walking up and down the hall trying to find the girl who stole her radio.
On 1/2/2024, Resident #1 was yelling at staff and visitors that she wanted to leave with them and would pay them. She even asked another resident to leave with her and go to the bank. Another entry this day noted she was yelling about her Cadillac, she needed to pick her car up, she wasn't going to kill herself, but she would.
On 3/29/24, Resident #1 was attempting to get into another resident's room and was combative with staff and other residents when being redirected. She was noted as unsteady and attempted to elope out the east hall emergency exit, setting off the alarm. The physician was notified and there were pending PRN (as needed) orders. (There was no indication in the note of what those orders were.) (Photographic evidence obtained) There were no revisions to the care plan after the occurrence, and there was no further mention of the event in the electronic medical record (EMR).
On 4/18/24, Resident #1 was noted to be found sitting on the floor in the hallway with her walker in front of her. No injuries were sustained.
On 4/30/24 at 9:01 a.m., it was noted that the Interdisciplinary Team (IDT) reviewed Resident #1 having been found outside of the facility on 4/25/24. Per the review, staff observed the resident ambulating independently outside adjacent to the property on the road. The resident was returned to an activity of her choice without difficulty. Interventions included body audit, physician and family notification, verification of door alarm system, verification of wander monitoring device placement, staff education on wander monitoring devices and door checks, increased visual safety checks every 15 minutes as ordered, and door monitoring for alarm engagement as indicated.
(Photographic evidence of all nursing progress notes obtained)
Resident #1's medical record included a monitoring log which was utilized to document the 15-minute visual checks ordered by the physician on 4/25/24. Documentation commenced this day at 11:00 p.m. (The incident occurred at 2:30 p.m. this same day.) and continued until 4/26/24 at 9:00 p.m. then stopped. Checks resumed on 4/27/24 at 7:00 a.m. through 1:00 p.m., then stopped again. Documentation resumed on 4/28/24 at 7:00 a.m. then stopped at 1:30 p.m. In conjunction with the log, facility nurses were signing Resident #1's medication administration log/treatment administration log (MAR/TAR) on each of the two shifts daily that 15-minute checks were being completed despite no documentation on the monitoring log over large periods of time. (Photographic evidence obtained)
A review of a facility report, generated on 5/1/24 by the Nursing Home Administrator (NHA) alleging neglect, revealed that on 4/25/24, Resident #1 was seen ambulating outside the facility at 2:30 p.m. by Certified Nursing Assistant (CNA) A. She was on the facility grass and slightly on the road. CNA A asked CNA B for help and they retrieved and returned Resident #1 to the facility without difficulty. A body assessment was completed with no injuries identified, and the resident was returned to a preferred activity. The physician and family were notified. Wander monitoring device placement was verified on her left ankle, and frequent visual checks were put into place.
The facility's analysis and investigation of the incident determined that Resident #1 walked out the East wing exit door, leaving her walker inside beside the door. The east wing exit fire door alarm system required arming by key function. At the time of the resident's exit, the door alarm was found to be disengaged, therefore, it did not sound when the exit bar was pushed, and the door opened. Education was initiated for the management team and facility nurses on 4/26/24 about monitoring exit doors for alarm function. Resident #1 had a history of wandering behaviors and was already listed in the facility's elopement book. The facility verified the incident, although they included a disclaimer that they had to classify the incident as Neglect since elopement was not an option on the form. The summary of corrective actions taken included:
1. Frequent visual checks to monitor for increased wandering behaviors.
2. Education initiated for door monitoring and wander monitoring device use and function.
3. Ongoing education for elopement will be provided upon hire and annually.
4. All residents were re-evaluated for wandering risk.
(Photographic evidence obtained)
In a follow-up report generated by the NHA on 5/9/24, the incident was reclassified to Resident Elopement. It included new orders received by the physician for a 15-minute safety check for three days to monitor the resident's location and activity. It added that Resident #1 had a BIMS score of 00/15 on 3/25/24. The door was evaluated and found to be in proper working order once it was armed correctly with the key. All facility doors with alarms that required a key to alarm were also checked and found to be in proper functioning order. Education was provided to the management team and nursing staff on engaging the door alarm with the key to ensure proper functioning.
The corrective actions implemented by the facility post-incident (4/25/24) were as follows:
1. Facility reviews of the elopement policy and procedure.
2. Quotes obtained, and a project was initiated for providing upgraded wander guard (wander monitoring device) systems to the east wing, west wing, restorative dining room (doors), and south hall exit doors.
3. Verification of wander guard placement and use for all residents.
4. Review of monitoring tools for door checks, wander guard device checks.
5. Staff education on the arming of the door system with the key.
6. Continue with wander guard device checks and placement as ordered for those residents at wandering risk.
7. Staff education upon hire and quarterly of the Elopement policy and procedures.
8. Performance Improvement Plan (PIP) to assess and monitor progress of the initiatives put into place to avoid further occurrence. Review of PIP with QA&A committee for the next three-month period or until substantial compliance.
9. Review of Interdisciplinary Team (IDT) assessment upon resident admission for residents deemed to be at risk for wandering behaviors, and continuation of wandering resident assessments quarterly with updates to elopement book as required.
10. All residents re-evaluated for wandering resident risk assessment.
In response to the facility's alleged corrective actions, the facility's staff education plan and training was reviewed. Per the facility's annual in-service training calendar, abuse and neglect training were required every year in July. Elopement training was not a requirement at any time during the year. (Photographic evidence obtained)
The facility's All Staff New Hire Orientation training program/syllabus was reviewed and revealed that although it was three pages long, the facility's policies and procedures for elopement prevention and response were not included. Elder Abuse and Resident Rights training was reviewed during orientation.
A review of the facility's employee roster found there were a total of 84 staff dedicated to working in the facility, but a total of 131 shared staff between the hospital and the nursing facility. A review of employee training transcripts found that after the 4/25/24 elopement by Resident #1, only 57 of 84 facility staff and 131 combined staff had received any training in the facility's elopement prevention and response policies and procedures. (Photographic evidence obtained)
An elopement drill was conducted on 5/15/24. Only 27 of the facility's 84 staff members participated. No elopement drills were conducted in the year leading up to the incident. (Photographic evidence obtained)
Training titled Monitoring Exit Door for Alarm Function was provided between 4/26/24 and 5/15/24. Only 21 of 84 facility staff received the training. (Photographic evidence obtained)
Maintenance records were reviewed, revealing no fire door or wander monitoring device alarm system checks had been documented leading up to the incident on 4/25/24. A review of the fire door surveillance logs, which covered both the hospital and the nursing home fire doors, revealed that the fire doors were checked annually, most recently on 10/13/23.
An interview was conducted with CNA A on 6/12/24 at 11:00 a.m. She was sitting with several residents on the small, gated patio off the restorative dining room. CNA A explained that she was assigned to sit outside with the residents. The door from the dining room to the patio was locked when no one was outside; she let the residents in and out using her (magnetic) badge. The doors on the east and west residential halls sounded an alarm, then released, if you pushed them. She explained that residents must sign out and back in on the leave of absence (LOA) book at the nurse's station if they wanted to go out. She had never had to participate in an actual search for a missing resident, but stated there were approximately ten residents at risk for elopement. Elopement books were kept in the activity room, the nurses' stations, up at the front of the facility, and the social services director had one. The facility used wander monitoring devices; however, the only wander monitoring device sensor was up front on the south hall. There was a second one closer to the front lobby. The east, west and restorative dining room doors were locked but none had wander monitoring device sensors. In a second interview at 4:00 p.m., CNA A confirmed that she was the staff member who saw Resident #1 outside on 4/25/24. CNA A was sitting in the restorative/activity room when she saw Resident #1 walking along the sidewalk that went around the building. She got CNA B and they went out the patio gate and retrieved the resident. Resident #1 said she was going home. CNA A never heard an alarm sound. The nurses had the key to the exit doors at the nurses' station. She did not know why someone used it. The unit clerk checked those doors daily and always had. Resident #1 was exit-seeking and always said she wanted to go home. CNA A reported that she only recently received training in elopement and participated in one elopement drill since the 4/25/24 incident. Prior to that, she had not participated in an elopement drill in a long, long time. CNA A explained that the facility was trying to get things back up and running after changes in administration.
On 6/12/24 at 12:15 p.m., during an interview with the NHA, he explained that the east and west wing doors were alarmed fire exits that sounded when the doors were opened. The restorative dining room had two doors with the same alarm. If the door was pushed, it opened immediately and sounded the alarm. Staff did not use those doors; they only used the front door, even after hours. A new wander monitoring device system was being installed next month (July) on the east, west and south halls and on the restorative dining room doors. The current wander monitoring device system was for the main dining room and was located at the end of the south hall close to the front entrance. The NHA said his understanding was that there had been an elopement a long time ago. In response, a wander monitoring device system was installed in the front, but not the back, of the facility. There had been no other elopements since he had been employed by the facility. The maintenance department checked all fire doors and administration checked the wander monitoring device system sensors. He said the unit clerk checked the doors daily, Monday through Friday, to ensure they were armed. Before the elopement, no one was documenting those inspections. He thought the charge nurse checked the doors on the weekends. Now, wander zones and all exit door alarms were inspected daily and documented. The nurses kept the key to the fire doors at the east and west wing nurses' stations and maintenance had a key. When the fire exit door opened, the alarm sounded, and the door closed behind the person exiting. A key was required to deactivate the alarm. It made a beeping sound. The door must also be re-armed using the key. No one should go out those doors for any reason, and as far as he was aware, no one was. The NHA then admitted seeing a chair outside of the east wing door for some time, but he didn't really think anything about it. He never saw anyone out there and thought maybe family members liked to sit out there and watch the ducks. Now, in hindsight, he could only assume someone was going out that door to smoke. No one admitted using that door before the incident. He reviewed the facility's camera footage of the day before the event, but it did not reveal anyone using the door. The cameras at the end of the hall did not have a time stamp on the footage and he was not sure how much memory they had. When asked if he only reviewed one day of footage, the NHA confirmed that he had not reviewed prior days to see when the door may have been utilized. Upon suggestion, the NHA acknowledged the likelihood that the door was disarmed for longer than a day.
An interview was attempted with Resident #1 on 6/12/24 at 2:00 p.m. When asked what her name was and how she was doing, she was unable to answer. She spoke at length as though she could not hear, despite efforts to speak as loudly as possible. Resident #1 then asked, Where is the other one? She was advised, In the conference room. Resident #1 laughed, then asked if this surveyor had ever been upstairs (building is single story). She explained that it was beautiful up there. As the conversation continued, it was evident that Resident #1 had trouble understanding what was being said to her as well as disorganized thinking. As her confusion increased, the interview was concluded. Resident #1 then said, Tell your sister I love her. I hope you come back.
In an interview with the NHA on 6/12/24 at 2:55 p.m., he was asked if any additional elopement drills had been conducted, aside from the drill dated 5/15/24. He replied no but was asked to double-check over the last year to verify. He confirmed that there were no drills conducted in the last year; he had none to share.
CNA B was interviewed on 6/12/24 at 4:03 p.m. She confirmed that she assisted CNA A with retrieving Resident #1 from the sidewalk on 4/25/24. She had been on the south hall and never heard an alarm sound. CNA B stated she had not participated in an elopement drill until after the 4/25/24 incident. The key for the fire exit doors was kept at the nurses' station. Those doors would only be used in the event of a fire. The facility was admitting more and more residents who wandered compared to past admissions. Resident #1 wandered and wanted to go home or get her car. The wander monitoring device alarm was at the end of the south hall but there were none on the east or west halls.
During an interview with the NHA on 6/13/24 at 9:38 a.m., he was asked about his investigation into Resident #1's 4/25/24 elopement. He returned at 9:50 a.m. and explained that CNA A saw Resident #1 hovering by the road in the grass outside of the activities/restorative dining room. She called for CNA B, told her the resident was outside, and they got her safely back inside. In response, a body check was performed. The door function was checked, and it (the alarm) didn't sound. He said, Resident #1's wander guard bracelet was checked, although that bracelet means nothing for those doors; only for the front. The NHA stated that prompted him to inquire about the door checks, which there was no documentation for up to the event. Staff just reported they were conducting them. The NHA implemented daily fire and exit door checks that same day. He then began training staff on the Wandering Resident policy, which he had reviewed and updated on 4/26/24. He made it more user and reader-friendly and included a major change, which was that the search for a missing resident could not exceed 10 minutes prior to notification. That gave staff an opportunity to search for the resident prior to calling him. This change shortened the time from the previous 15-minute search. Staff should also check the LOA (leave of absence) book to see if the resident signed out with family. The NHA put this policy in the electronic staff training database and set a deadline for all staff to complete the training by 5/31/24. When he printed the transcripts for the survey team's review on 6/13/24, he realized not all staff had completed the required training. There was a total of 131 staff shared between the hospital and nursing home; shared staff included the dietary department, physical therapy, housekeeping and maintenance departments. Those were split departments and staff came over from the hospital to work at the nursing home. New staff orientation training was provided by Human Resources (HR). The NHA was asked if he noticed there was no elopement training included in the new hire orientation packet. He said yes and had already spoken with HR and planned to change that. The NHA said he reviewed the elopement policy with staff during the May elopement drill. When asked how he was keeping the residents at risk safe, he replied that a new wander monitoring device system would be installed, and he was making sure the doors were being checked and documented every morning. The Risk Manager (RM) received the log, checked it, and brought it to the Friday meeting for review. The Social Services Director (SSD) reviewed and updated the elopement books weekly, upon significant change or new admission, and reviewed those at the meeting. When asked how the facility identified residents at risk, the NHA stated risk was usually identified by family or hospital admission papers. He was not sure if nurses used a wandering or elopement assessment. He called the Director of Nursing (DON), who reported that residents were assessed on admission and quarterly. The NHA added as part of his investigation that he obtained a written statement from CNA A, the only direct witness to Resident #1's elopement. When asked about his investigation into how or why the door was unlocked, he said he was still trying to figure out when the nurse last locked it. He wondered if they waited for the beep, beep, beep sound that indicated it was armed, or if someone forgot to lock it altogether. They hadn't figured that out. He again asserted that doors should not be disarmed for any reason, and staff did not use those doors. When asked if he retrained nurses in situations where the fire doors should be used, he said no; just to check the doors, properly arm them and wait for the three beeps when turning the alarm back on. The nurses had the key to turn off the alarm if a resident exited through those doors. When asked if CNAs could use the key, he said yes, but usually a nurse did. The NHA was asked if he was made aware that Resident #1 successfully opened that door a month prior to the incident (on 3/29/24). He said he had not been told that, but she was a wanderer, so he believed that happened. The NHA said the day after the 4/25/24 incident, they happened to have a QAPI (Quality Assurance and Performance Improvement) meeting. They reviewed the incident and developed a Performance Improvement Plan (PIP). When asked if the facility had identified a root cause analysis (RCA), he did not know but said he would provide that information.
The Risk Manager (RM) was interviewed on 6/13/24 at 10:30 a.m. and shared the QAPI meeting information at that time. She explained that the committee, including the Medical Director, met on 4/26/24 and reviewed the 4/25/24 incident. They covered the facts of the situation and did a drill down for the time the resident was seen inside versus outside. The committee looked at recent changes in medications and increased behaviors. Resident #1 did experience anxiety, wanted to go home, and was functionally able to move around. They spoke with the activities staff about continuing to redirect Resident #1 (to activities) and spoke with her family to encourage their visits. Residents' locations were verified immediately following the event, and every door was inspected and armed, including the badge-in, badge-out doors. The committee also reviewed processes moving forward with the wander monitoring device system and door checks daily, as well as wander monitoring device checks. Those devices were checked for function weekly and for placement every shift. The RCA focused on the door that had been disarmed with the key, but facility management could not determine who disarmed the door alarm. It had not been re-armed correctly. We did all-staff education that day with the staff on duty. The RM was asked about staff not on duty and said she would have to look at the training records. Upon review of the training logs, the RM realized that only 21 staff had been trained in the use of the door alarm key. The RM was asked if the QAPI committee identified a lack of staff training on elopement prevention and response. She did not answer. The NHA interjected and implied that they had not. He said that outside of QAPI, they had reviewed and recognized the lack of elopement orientation and training for staff. They had nursing home-specific training in the works. The RM said the committee did look at education during the drill down. Since they were part of the hospital, there was a standardized orientation training program. Moving forward, they would provide elopement training during the new hire orientation. When asked if the committee considered training current staff and having them participate in elopement drills, she deferred to the NHA who did not respond. Instead, the DON (also present in the room) answered. She stated nursing home staff training was now being separated from the hospital and infection control training. The Staff Development nurse would train new hires and conduct quarterly training on elopement procedures. She admitted that was not part of the QAPI discovery or plan. Recent elopement training was provided and those would pick up quarterly. Quarterly elopement drills would be conducted with all staff on all shifts. When asked why there was a lack of urgency in training current staff and having them participate in an elopement drill, the DON replied that there were about 75 - 80 employees who were employed solely by the nursing home. When asked if that might be a core sample to target for training and drills, the DON said yes. The RM also confirmed that was not identified during the QAPI meeting. She explained what was decided on, referencing the following evidence: 1) A post-incident census tracking sheet to verify placement of all residents in the facility; 2) Daily door check logs for all doors; 3) Verification of physician's orders for wander monitoring devices for the eight residents at risk for elopement; and 4) Door alarm monitoring training (21 staff trained).
An interview was conducted with the Chief Nursing Officer (CNO) on 6/13/24 at 2:15 p.m. She stated she was a member of the Governing Body and provided clinical oversight to the nursing home and the NHA. This past week a new Clinical Educator was hired, who would be separating the infection control and nursing education for facility staff. Education needed to take a priority and be increased. The CNO confirmed that elopement prevention and response was included in the orientation or required training. She then insisted that the current wander monitoring device system had successfully prevented residents who got too close to the exits from exiting in the past. When she was reminded that there were no wander monitoring device sensors on the exit doors on the nursing units, she said she wondered whether they had become complacent with the wander monitoring device system. She was advised that staff reported the admission of more residents now who wandered than it had admitted in[TRUNCATED]
CRITICAL
(L)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
QAPI Program
(Tag F0867)
Someone could have died · This affected most or all residents
⚠️ Facility-wide issue
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, staff interviews, resident, facility, and staff record reviews, the facility's policy for Resident Elopem...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, staff interviews, resident, facility, and staff record reviews, the facility's policy for Resident Elopement, the Facility Assessment, and a review of the Quality Assurance and Performance Improvement (QAPI) Program, the facility failed to have an effective Quality Assurance and Performance Improvement (QAPI) process to monitor/audit facility practices involving resident elopements, assessment of elopements, staff education and competencies, and development of effective safety and preventative measures for Resident #1, who was identified as an elopement risk, as well as seven other residents identified as at risk for elopement. The QAPI committee failed to address 1) An incomplete facility investigation following Resident #1's elopement on 4/25/24, 2) All-staff training related to elopement and fire exit doors, 3) Staff participation in elopement drills, and 4) A wander monitoring system that only protected two of seven facility doors that opened to the outside. Instead, the committee identified a root cause analysis (RCA) focused on a key that was not used to re-arm a fire door alarm after it had been disarmed, and the fact that only 21 of 131 staff were trained in the proper use if the key. As of 6/13/24, the majority of the plan moving forward was still being discussed by the QAPI committee, seven weeks after the event. This failure contributed to a likelihood of suffering serious injury, serious harm or death to the facility's eight residents identified as at risk for wandering and/or exit-seeking.
On 2/9/23, Resident #1 was admitted to the facility and was assessed as at risk for elopement. On 2/11/23, a wander monitoring device was placed on the resident's left ankle. A 3/25/24 Minimum Data Set (MDS) assessment revealed a Brief Interview for Mental Status (BIMS) score of 00 out of 15 possible points, indicating severe cognitive impairment. On 3/29/24, at 12:50 a.m., the resident pushed open the fire exit door on the East Wing, sounding the alarm. No care plan interventions were reviewed or revised after this incident. On 4/25/24 at 2:30 p.m., Resident #1 was observed walking outside of the facility in the grass adjacent to the road. She was returned to the facility at 2:32 p.m. Her walker was discovered at the East Wing fire exit door, the same door she pushed open on 3/29/24. The door's alarm was disarmed. Keys to disarm the fire door were at the nursing station, and the door alarmed properly once armed correctly with the key. There was no investigation into why the fire exit door's alarm was disarmed. The Administrator speculated that families or staff were using the door to go outside. The key remained at the nursing station. There was no wander monitoring device sensor alarm on this door. Two of seven exits were fitted with wander monitoring device sensor alarms. Both were near the front entrance. The facility had no policy and procedure for wander monitoring devices. New orders were written for 15-minute safety checks of Resident #1 for three days. They began on 4/25 at 11:00 p.m., 8.5 hours after the event. Between 4/25 and 4/28, documentation of 15-minute checks over large blocks of time was missing. It is unknown whether safety checks were completed as ordered. No elopement drills were documented during the year preceding this event, and the only drill completed after the event was conducted almost three weeks later, on 5/15/24. Twenty-seven of 131 staff members participated. There were no additional drills between 5/15/24 and the date of survey commencement on 6/12/24. Staff orientation and annual training did not include information on elopement/wandering. After the event, 57 of 131 staff received elopement training, and 21 of 131 staff were trained in the proper use of the key for arming/disarming the fire door alarms.
Immediate Jeopardy (IJ) at a scope and severity of L (widespread) was identified at 11:10 a.m. on June 13, 2024.
On March 29, 2024 at 12:05 a.m., Immediate Jeopardy began.
On June 13, 2024 at 5:20 p.m., the Administrator was notified of the IJ determination, and Immediate Jeopardy was ongoing as of the survey exit on June 13, 2024.
The findings include:
Cross reference F600, F689, F835
During a tour of the facility on 6/12/24 at 10:30 a.m. on the South hallway just off the front lobby, there were wander monitoring device sensors installed on both doors and protecting approximately 50 feet of the southernmost end of the hall. A glass fire exit door was located halfway up the hall on the west side. The door was a magnetic lock fire door and alarmed by use of a key. This door had no wander monitoring device alarm sensor. A red sticker on the door's press bar instructed, Push to open. Alarm will sound. This exit opened to an interior courtyard with an unlocked but latched gate which led to a parking lot. The hall dead-ended to the North in the restorative dining/activity room, which had two exits. One was a magnetic employee badge lock (not a fire exit) which led to a small outdoor patio with an approximately 3 1/2 foot high (unlocked but latched) gate. The second door was a magnetic lock fire door with a key-activated alarm and the same red sign instructing to press the press bar to open. Neither door was equipped with a wander monitoring device sensor. At this intersection, the east hall branched to the right, and the west hall branched to the left. Each hall ended at a glass fire door with the same key-operated magnetic lock and red sign. Neither was equipped with a wander monitoring device alarm sensor. The east door exited to a grassy area and sidewalk which went around the building to Ohio Avenue. The west door opened to a parking lot.
A record review for Resident #1 found she was admitted on [DATE] with diagnoses including, but not limited to, Alzheimer's disease, disorder of bone density and structure, hypertension, a history of falls, delusional disorder and sick sinus syndrome (a heart rhythm disorder resulting from the heart's natural pacemaker malfunctions).
A quarterly MDS assessment, dated 3/25/24, assessed Resident #1 with a brief interview for mental status (BIMS) score of 00 out of a possible 15 points, indicating severely impaired cognitive functioning for daily decision making. She had highly impaired hearing and used a hearing aid. She could walk 150 feet independently and had two falls since admission/most recent assessment. Antipsychotic medication was received routinely. A wander/elopement alarm was marked as not used, and no discharge planning to return to the community was occurring.
Resident #1 had a care plan dated 5/22/23, last revised on 3/28/24 for
Focus: Elopement Risk/Wanderer as evidenced by impaired safety awareness. The focus was revised on 4/29/24 for: Elopement on 4/25/24, returned safely to facility. The goal was to maintain her safety through the next review date of 9/11/24. Interventions included assessing for fall risk, distracting the resident from wandering by offering pleasant diversions, structured activities, food, and conversation, to identify patterns, monitor location frequently and use of a wander alert bracelet. A new intervention was added on 4/29/24 for the wander monitoring device function to be verified weekly by nursing staff. (Photographic evidence obtained)
Resident #1 had a physician's order dated 2/11/23, for Wanderguard system for safety, which was revised on 11/8/23 to include a system function test every Wednesday. Resident #1 routinely received Quetiapine Fumarate (an antipsychotic medication) 25 milligrams (mg) twice daily for paranoia and agitation (started on 11/28/23), and Zoloft (antidepressant) 25 mg every morning for depression (started 11/29/23). She also had a past order for Ativan (antianxiety) 0.5 mg every 6 hours as needed for anxiety, start on 4/5/24 and continue for 14 days (end 4/19/24). (Photographic evidence obtained)
On 4/25/24 at 11:00 p.m., the physician ordered every 15-minute visual checks for Resident #1 for three days (end 4/28/24).
Resident #1 was assessed for wandering risk on 2/9/23, 5/9/23, 8/9/23, 11/3/23, and most recently on 3/23/24 (moderate risk), 4/27/24 (high risk) and 6/9/24 (high risk). (Photographic evidence obtained)
A review of nursing progress notes for Resident #1 found the following:
On 12/9/23, Resident #1 tried to leave with another visitor, stating she had to go get her Cadillac.
On 12/4/23, Resident #1 wanted to go home, walking up and down the hall trying to find the girl who stole her radio.
On 1/2/2024, Resident #1 was yelling at staff and visitors that she wanted to leave with them and would pay them. She even asked another resident to leave with her and go to the bank. Another entry this day noted she was yelling about her Cadillac, she needed to pick her car up, she wasn't going to kill herself, but she would.
On 3/29/24, Resident #1 was attempting to get into another resident's room and was combative with staff and other residents when being redirected. She was noted as unsteady and attempted to elope out the east hall emergency exit, setting off the alarm. The physician was notified and there were pending PRN (as needed) orders. (There was no indication in the note of what those orders were.) (Photographic evidence obtained) There were no revisions to the care plan after the occurrence, and there was no further mention of the event in the electronic medical record (EMR).
On 4/18/24, Resident #1 was noted to be found sitting on the floor in the hallway with her walker in front of her. No injuries were sustained.
On 4/30/24 at 9:01 a.m., it was noted that the Interdisciplinary Team (IDT) reviewed Resident #1 having been found outside of the facility on 4/25/24. Per the review, staff observed the resident ambulating independently outside adjacent to the property on the road. The resident was returned to an activity of her choice without difficulty. Interventions included body audit, physician and family notification, verification of door alarm system, verification of wander monitoring device placement, staff education on wander monitoring devices and door checks, increased visual safety checks every 15 minutes as ordered, and door monitoring for alarm engagement as indicated.
(Photographic evidence of all nursing progress notes obtained)
Resident #1's medical record included a monitoring log which was utilized to document the 15-minute visual checks ordered by the physician on 4/25/24. Documentation commenced this day at 11:00 p.m. (The incident occurred at 2:30 p.m. this same day.) and continued until 4/26/24 at 9:00 p.m. then stopped. Checks resumed on 4/27/24 at 7:00 a.m. through 1:00 p.m., then stopped again. Documentation resumed on 4/28/24 at 7:00 a.m. then stopped at 1:30 p.m. In conjunction with the log, facility nurses were signing Resident #1's medication administration log/treatment administration log (MAR/TAR) on each of the two shifts daily that 15-minute checks were being completed despite no documentation on the monitoring log over large periods of time. (Photographic evidence obtained)
A review of a facility report, generated on 5/1/24 by the Nursing Home Administrator (NHA), who was a member of the QAA committee, alleging neglect, revealed that on 4/25/24, Resident #1 was seen ambulating outside the facility at 2:30 p.m. by Certified Nursing Assistant (CNA) A. She was on the facility grass and slightly on the road. CNA A asked CNA B for help and they retrieved and returned Resident #1 to the facility without difficulty. A body assessment was completed with no injuries identified, and the resident was returned to a preferred activity. The physician and family were notified. Wander monitoring device placement was verified on her left ankle, and frequent visual checks were put into place.
The facility's analysis and investigation of the incident determined that Resident #1 walked out the East wing exit door, leaving her walker inside beside the door. The east wing exit fire door alarm system required arming by key function. At the time of the resident's exit, the door alarm was found to be disengaged, therefore, it did not sound when the exit bar was pushed, and the door opened. Education was initiated for the management team and facility nurses on 4/26/24 about monitoring exit doors for alarm function. Resident #1 had a history of wandering behaviors and was already listed in the facility's elopement book. The facility verified the incident, although they included a disclaimer that they had to classify the incident as Neglect since elopement was not an option on the form. The summary of corrective actions taken included:
1. Frequent visual checks to monitor for increased wandering behaviors.
2. Education initiated for door monitoring and wander monitoring device use and function.
3. Ongoing education for elopement will be provided upon hire and annually.
4. All residents were re-evaluated for wandering risk.
(Photographic evidence obtained)
In a follow-up report generated by the NHA on 5/9/24, the incident was reclassified to Resident Elopement. It included new orders received by the physician for a 15-minute safety check for three days to monitor the resident's location and activity. It added that Resident #1 had a BIMS score of 00/15 on 3/25/24. The door was evaluated and found to be in proper working order once it was armed correctly with the key. All facility doors with alarms that required a key to alarm were also checked and found to be in proper functioning order. Education was provided to the management team and nursing staff on engaging the door alarm with the key to ensure proper functioning.
The corrective actions implemented by the facility post-incident (4/25/24) were as follows:
1. Facility reviews of the elopement policy and procedure.
2. Quotes obtained, and a project was initiated for providing upgraded wander guard (wander monitoring device) systems to the east wing, west wing, restorative dining room (doors), and south hall exit doors.
3. Verification of wander guard placement and use for all residents.
4. Review of monitoring tools for door checks, wander guard device checks.
5. Staff education on the arming of the door system with the key.
6. Continue with wander guard device checks and placement as ordered for those residents at wandering risk.
7. Staff education upon hire and quarterly of the Elopement policy and procedures.
8. Performance Improvement Plan (PIP) to assess and monitor progress of the initiatives put into place to avoid further occurrence. Review of PIP with QA&A committee for the next three-month period or until substantial compliance.
9. Review of Interdisciplinary Team (IDT) assessment upon resident admission for residents deemed to be at risk for wandering behaviors, and continuation of wandering resident assessments quarterly with updates to elopement book as required.
10. All residents re-evaluated for wandering resident risk assessment.
In response to the facility's alleged corrective actions, the facility's staff education plan and training was reviewed. Per the facility's annual in-service training calendar, abuse and neglect training were required every year in July. Elopement training was not a requirement at any time during the year. (Photographic evidence obtained)
The facility's All Staff New Hire Orientation training program/syllabus was reviewed and revealed that although it was three pages long, the facility's policies and procedures for elopement prevention and response were not included. Elder Abuse and Resident Rights training was reviewed during orientation.
A review of the facility's employee roster found there were a total of 84 staff dedicated to working in the facility, but a total of 131 shared staff between the hospital and the nursing facility. A review of employee training transcripts found that after the 4/25/24 elopement by Resident #1, only 57 of 84 facility staff and 131 combined staff had received any training in the facility's elopement prevention and response policies and procedures. (Photographic evidence obtained)
An elopement drill was conducted on 5/15/24. Only 27 of the facility's 84 staff members participated. No elopement drills were conducted in the year leading up to the incident. (Photographic evidence obtained)
Training titled Monitoring Exit Door for Alarm Function was provided between 4/26/24 and 5/15/24. Only 21 of 84 facility staff received the training. (Photographic evidence obtained)
Maintenance records were reviewed, revealing no fire door or wander monitoring device alarm system checks had been documented leading up to the incident on 4/25/24. A review of the fire door surveillance logs, which covered both the hospital and the nursing home fire doors, revealed that the fire doors were checked annually, most recently on 10/13/23.
An interview was conducted with CNA A on 6/12/24 at 11:00 a.m. She was sitting with several residents on the small, gated patio off the restorative dining room. CNA A explained that she was assigned to sit outside with the residents. The door from the dining room to the patio was locked when no one was outside; she let the residents in and out using her (magnetic) badge. The doors on the east and west residential halls sounded an alarm, then released, if you pushed them. She explained that residents must sign out and back in on the leave of absence (LOA) book at the nurse's station if they wanted to go out. She had never had to participate in an actual search for a missing resident, but stated there were approximately ten residents at risk for elopement. Elopement books were kept in the activity room, the nurses' stations, up at the front of the facility, and the social services director had one. The facility used wander monitoring devices; however, the only wander monitoring device sensor was up front on the south hall. There was a second one closer to the front lobby. The east, west and restorative dining room doors were locked but none had wander monitoring device sensors. In a second interview at 4:00 p.m., CNA A confirmed that she was the staff member who saw Resident #1 outside on 4/25/24. CNA A was sitting in the restorative/activity room when she saw Resident #1 walking along the sidewalk that went around the building. She got CNA B and they went out the patio gate and retrieved the resident. Resident #1 said she was going home. CNA A never heard an alarm sound. The nurses had the key to the exit doors at the nurses' station. She did not know why someone used it. The unit clerk checked those doors daily and always had. Resident #1 was exit-seeking and always said she wanted to go home. CNA A reported that she only recently received training in elopement and participated in one elopement drill since the 4/25/24 incident. Prior to that, she had not participated in an elopement drill in a long, long time. CNA A explained that the facility was trying to get things back up and running after changes in administration.
On 6/12/24 at 12:15 p.m., during an interview with the NHA, he explained that the east and west wing doors were alarmed fire exits that sounded when the doors were opened. The restorative dining room had two doors with the same alarm. If the door was pushed, it opened immediately and sounded the alarm. Staff did not use those doors; they only used the front door, even after hours. A new wander monitoring device system was being installed next month (July) on the east, west and south halls and on the restorative dining room doors. The current wander monitoring device system was for the main dining room and was located at the end of the south hall close to the front entrance. The NHA said his understanding was that there had been an elopement a long time ago. In response, a wander monitoring device system was installed in the front, but not the back, of the facility. There had been no other elopements since he had been employed by the facility. The maintenance department checked all fire doors and administration checked the wander monitoring device system sensors. He said the unit clerk checked the doors daily, Monday through Friday, to ensure they were armed. Before the elopement, no one was documenting those inspections. He thought the charge nurse checked the doors on the weekends. Now, wander zones and all exit door alarms were inspected daily and documented. The nurses kept the key to the fire doors at the east and west wing nurses' stations and maintenance had a key. When the fire exit door opened, the alarm sounded, and the door closed behind the person exiting. A key was required to deactivate the alarm. It made a beeping sound. The door must also be re-armed using the key. No one should go out those doors for any reason, and as far as he was aware, no one was. The NHA then admitted seeing a chair outside of the east wing door for some time, but he didn't really think anything about it. He never saw anyone out there and thought maybe family members liked to sit out there and watch the ducks. Now, in hindsight, he could only assume someone was going out that door to smoke. No one admitted using that door before the incident. He reviewed the facility's camera footage of the day before the event, but it did not reveal anyone using the door. The cameras at the end of the hall did not have a time stamp on the footage and he was not sure how much memory they had. When asked if he only reviewed one day of footage, the NHA confirmed that he had not reviewed prior days to see when the door may have been utilized. Upon suggestion, the NHA acknowledged the likelihood that the door was disarmed for longer than a day.
An interview was attempted with Resident #1 on 6/12/24 at 2:00 p.m. When asked what her name was and how she was doing, she was unable to answer. She spoke at length as though she could not hear, despite efforts to speak as loudly as possible. Resident #1 then asked, Where is the other one? She was advised, In the conference room. Resident #1 laughed, then asked if this surveyor had ever been upstairs (building is single story). She explained that it was beautiful up there. As the conversation continued, it was evident that Resident #1 had trouble understanding what was being said to her as well as disorganized thinking. As her confusion increased, the interview was concluded. Resident #1 then said, Tell your sister I love her. I hope you come back.
In an interview with the NHA on 6/12/24 at 2:55 p.m., he was asked if any additional elopement drills had been conducted, aside from the drill dated 5/15/24. He replied no but was asked to double-check over the last year to verify. He confirmed that there were no drills conducted in the last year; he had none to share.
CNA B was interviewed on 6/12/24 at 4:03 p.m. She confirmed that she assisted CNA A with retrieving Resident #1 from the sidewalk on 4/25/24. She had been on the south hall and never heard an alarm sound. CNA B stated she had not participated in an elopement drill until after the 4/25/24 incident. The key for the fire exit doors was kept at the nurses' station. Those doors would only be used in the event of a fire. The facility was admitting more and more residents who wandered compared to past admissions. Resident #1 wandered and wanted to go home or get her car. The wander monitoring device alarm was at the end of the south hall but there were none on the east or west halls.
During an interview with the NHA on 6/13/24 at 9:38 a.m., he was asked about his investigation into Resident #1's 4/25/24 elopement. He returned at 9:50 a.m. and explained that CNA A saw Resident #1 hovering by the road in the grass outside of the activities/restorative dining room. She called for CNA B, told her the resident was outside, and they got her safely back inside. In response, a body check was performed. The door function was checked, and it (the alarm) didn't sound. He said, Resident #1's wander guard bracelet was checked, although that bracelet means nothing for those doors; only for the front. The NHA stated that prompted him to inquire about the door checks, which there was no documentation for up to the event. Staff just reported they were conducting them. The NHA implemented daily fire and exit door checks that same day. He then began training staff on the Wandering Resident policy, which he had reviewed and updated on 4/26/24. He made it more user and reader-friendly and included a major change, which was that the search for a missing resident could not exceed 10 minutes prior to notification. That gave staff an opportunity to search for the resident prior to calling him. This change shortened the time from the previous 15-minute search. Staff should also check the LOA (leave of absence) book to see if the resident signed out with family. The NHA put this policy in the electronic staff training database and set a deadline for all staff to complete the training by 5/31/24. When he printed the transcripts for the survey team's review on 6/13/24, he realized not all staff had completed the required training. There was a total of 131 staff shared between the hospital and nursing home; shared staff included the dietary department, physical therapy, housekeeping and maintenance departments. Those were split departments and staff came over from the hospital to work at the nursing home. New staff orientation training was provided by Human Resources (HR). The NHA was asked if he noticed there was no elopement training included in the new hire orientation packet. He said yes and had already spoken with HR and planned to change that. The NHA said he reviewed the elopement policy with staff during the May elopement drill. When asked how he was keeping the residents at risk safe, he replied that a new wander monitoring device system would be installed, and he was making sure the doors were being checked and documented every morning. The Risk Manager (RM) received the log, checked it, and brought it to the Friday meeting for review. The Social Services Director (SSD) reviewed and updated the elopement books weekly, upon significant change or new admission, and reviewed those at the meeting. When asked how the facility identified residents at risk, the NHA stated risk was usually identified by family or hospital admission papers. He was not sure if nurses used a wandering or elopement assessment. He called the Director of Nursing (DON), who reported that residents were assessed on admission and quarterly. The NHA added as part of his investigation that he obtained a written statement from CNA A, the only direct witness to Resident #1's elopement. When asked about his investigation into how or why the door was unlocked, he said he was still trying to figure out when the nurse last locked it. He wondered if they waited for the beep, beep, beep sound that indicated it was armed, or if someone forgot to lock it altogether. They hadn't figured that out. He again asserted that doors should not be disarmed for any reason, and staff did not use those doors. When asked if he retrained nurses in situations where the fire doors should be used, he said no; just to check the doors, properly arm them and wait for the three beeps when turning the alarm back on. The nurses had the key to turn off the alarm if a resident exited through those doors. When asked if CNAs could use the key, he said yes, but usually a nurse did. The NHA was asked if he was made aware that Resident #1 successfully opened that door a month prior to the incident (on 3/29/24). He said he had not been told that, but she was a wanderer, so he believed that happened. The NHA said the day after the 4/25/24 incident, they happened to have a QAPI (Quality Assurance and Performance Improvement) meeting. They reviewed the incident and developed a Performance Improvement Plan (PIP). When asked if the facility had identified a root cause analysis (RCA), he did not know but said he would provide that information.
The Risk Manager (RM), who was a member of the QAA committee, was interviewed on 6/13/24 at 10:30 a.m. and shared the QAPI meeting information at that time. She explained that the committee, including the Medical Director, met on 4/26/24 and reviewed the 4/25/24 incident. They covered the facts of the situation and did a drill down for the time the resident was seen inside versus outside. The committee looked at recent changes in medications and increased behaviors. Resident #1 did experience anxiety, wanted to go home, and was functionally able to move around. They spoke with the activities staff about continuing to redirect Resident #1 (to activities) and spoke with her family to encourage their visits. Residents' locations were verified immediately following the event, and every door was inspected and armed, including the badge-in, badge-out doors. The committee also reviewed processes moving forward with the wander monitoring device system and door checks daily, as well as wander monitoring device checks. Those devices were checked for function weekly and for placement every shift. The RCA focused on the door that had been disarmed with the key, but facility management could not determine who disarmed the door alarm. It had not been re-armed correctly. We did all-staff education that day with the staff on duty. The RM was asked about staff not on duty and said she would have to look at the training records. Upon review of the training logs, the RM realized that only 21 staff had been trained in the use of the door alarm key. The RM was asked if the QAPI committee identified a lack of staff training on elopement prevention and response. She did not answer. The NHA interjected and implied that they had not. He said that outside of QAPI, they had reviewed and recognized the lack of elopement orientation and training for staff. They had nursing home-specific training in the works. The RM said the committee did look at education during the drill down. Since they were part of the hospital, there was a standardized orientation training program. Moving forward, they would provide elopement training during the new hire orientation. When asked if the committee considered training current staff and having them participate in elopement drills, she deferred to the NHA who did not respond. Instead, the DON (also present in the room and a QAA committee member) answered. She stated nursing home staff training was now being separated from the hospital and infection control training. The Staff Development nurse would train new hires and conduct quarterly training on elopement procedures. She admitted that was not part of the QAPI discovery or plan. Recent elopement training was provided and those would pick up quarterly. Quarterly elopement drills would be conducted with all staff on all shifts. When asked why there was a lack of urgency in training current staff and having them participate in an elopement drill, the DON replied that there were about 75 - 80 employees who were employed solely by the nursing home. When asked if that might be a core sample to target for training and drills, the DON said yes. The RM also confirmed that was not identified during the QAPI meeting. She explained what was decided on, referencing the following evidence: 1) A post-incident census tracking sheet to verify placement of all residents in the facility; 2) Daily door check logs for all doors; 3) Verification of physician's orders for wander monitoring devices for the eight residents at risk for elopement; and 4) Door alarm monitoring training (21 staff trained).
An interview was conducted with the Chief Nursing Officer (CNO) on 6/13/24 at 2:15 p.m. She stated she was a member of the Governing Body and provided clinical oversight to the nursing home and the NHA. This past week a new Clinical Educator was hired, who would be separating the infection control and nursing education for facility staff. Educa[TRUNCATED]