CRITICAL
(K)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews, interviews, and policy reviews, the facility failed to provide adequate supervision for residents ident...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews, interviews, and policy reviews, the facility failed to provide adequate supervision for residents identified as high risk for elopement for 2 out of 14 vulnerable residents (Residents #1 and #2) and for one resident identified as physically aggressive towards self, staff, and residents (Resident #4). The facility failed to provide supervision to prevent an unwitnessed exit from the facility for Resident #1 and Resident #2 on 8/30/2025 while Resident #2 was assigned to one-to-one (1:1) supervision and both Residents #1 and #2 were located on a secured, locked unit of the facility. The facility failed to prevent Resident #4 from self-injury while on one-to-one supervision on 9/8/2025 and failed to prevent physical aggression by Resident #4 on 9/9/2025 resulting in Resident #4 punching a nurse in the face and being removed from the facility by law enforcement under an order for involuntary psychiatric examination. The cumulative effect of these events resulted in deficient practice the level of Immediate Jeopardy starting on 8/8/2025.This situation resulted in a finding of Immediate Jeopardy at a scope and severity of Pattern, (K). The facility's Administrator was notified of the Immediate Jeopardy on 9/11/2025 at 2:30 PM. The Immediate Jeopardy was determined to have begun on 8/08/2025. At the time of the survey exit on 9/11/2025, the Immediate Jeopardy was ongoing.Cross reference to F600.The findings include:Resident #1 and #2
A record review for Resident #1 included diagnoses of chronic kidney disease stage 3, hyperlipidemia, generalized anxiety, hypertension, Atrial fibrillation, chronic systolic heart failure, and Traumatic Brain Injury. A minimum data set (MDS) assessment, dated 8/12/2025, included a brief interview for mental status score (BIMS) of 7. A score of 0-7 indicates severe problems with thinking or memory according to Cleveland Clinic, accessed at my.clevelandclinic.org on 09/17/2025. A comprehensive care plan initiated for Resident #1 on 8/5/2025 included a care plan for elopement risk/wanderer related to impaired safety awareness/wanders aimlessly with a goal for safety to be maintained. Interventions included assess for elopement risk, distract from wandering by offering pleasant diversions, electronic monitoring device, and place on secured unit under increased supervision. A psychiatric admission note dated 8/6/2025 documented “patient presents guarded and non-cooperative initially during interview, patient states, I don't ever sleep, and I just want to get out of here.”
A record review for Resident #2 documented admission to the facility occurred on 6/17/2025 with diagnoses of unspecified dementia, type 2 diabetes, difficulty in walking, cognitive deficits, and mood disorder. On 6/17/25, an elopement risk screen was completed which indicated a score of 3.0, indicating at risk for elopement. Review of the care plan for Resident #2 revealed there was a care plan initiated on 6/18/2025 documenting “resident is an elopement risk/wanderer related to disoriented to place, impaired safety awareness, and resident wanders aimlessly. Interventions include assess for elopement risk, distract resident from wandering by offering pleasant diversions and structured activities, electronic monitoring device per MD (doctor) orders, and place on the unit for increased supervision. On 6/20/2025, Resident #2's care plan was updated to “resident being placed on 1:1 supervision due to cutting off his wander guard bracelet and exit seeking.” A progress note dated 6/20/2025 at 11:40 pm stated “at approximately 2225 pm (10:25PM) CNA (certified nursing assistant) assigned as 1:1 stated Resident #2 was missing, the nurse checked patient's room and confirmed Resident #2 was not present, observed patient window inside of room was opened, and no visual of resident outside of room, DON (Director of Nursing) was notified and elopement protocol was initiated.
A psychiatric progress note dated 6/21/2025 documented Resident #2 was able to engage in a rational process of relevant information, able to recognize the importance of medication and treatment compliance, able to recognize his medical condition and consequences of lack of treatment and had the capacity to make decisions related to his need for healthcare or long-term placement. He was documented as able to understand the nature, extent, and probable outcome of not receiving medical care and was alert and oriented to self, place, time, and situation. On 6/21/2025, an elopement risk evaluation was repeated and again indicated a score of 3.0, indicating at risk for elopement. On 6/23/2025, the care plan for Resident #2 was updated for behaviors due to “refusing care and medications, becoming agitated and will curse at staff. He slams the door and tells staff to stop following him, removes his wander guard, and is able to unscrew his window to leave facility. Interventions include administer medications as ordered, anticipate resident's needs, explain all procedures to resident before starting care, if reasonable discuss residents behaviors and why behavior is inappropriate.”
On 6/29/2025, Resident #2 was transferred from the facility for an involuntary psychiatric evaluation due to mood disorder unspecified with documentation stating “patient has become violent towards staff, he is attempting to assault them and commit battery, he has a knife and is trying to break out the windows and exit facility. Due to his current state, he cannot be managed safely at this location and requires a higher level of care. Patient has failed all interventions by staff to help alleviate current symptoms. Due to these impulsive unpredictable and violent behaviors, the patient requires a higher level of care to ensure the safety of others at this time.” Resident #2 was discharged and re-admitted on [DATE] to facility.
An MDS assessment for Resident #2 dated 6/23/2025 documented a BIMS score of 5 (severe problems with thinking or memory). During the 7-day assessment period associated with the MDS, wandering was documented to have occurred on 1-3 days and to place the resident at significant risk of getting to a potentially dangerous place. Diagnoses included: dementia, neurological disorders, diabetes, malnutrition, anxiety, bipolar disorder, encephalopathy, muscle weakness, difficulty walking, cognitive communication deficit, history of alcohol abuse.
A progress note dated 7/13/2025 revealed: “alarm to the back door going off, when checking it out, they said that [Resident #2] was messing with the alarm on the door, they saw him doing it and told him several times to leave the door alone, after the alarm would not shut off, this nurse trouble shooting the problem and noticed that [Resident #2] had pulled the wires and tripping the connections to the alarm. A temporary fix on the door alarm, risk manager and maintenance is aware. [Resident #2] continues on 1:1 supervision.”
Documentation demonstrated Resident #2 continued to refuse medications from the facility except for metformin. On 7/22/2025, Resident #2 refused medications, education was provided. Resident #2 stated he is going home and doesn't need anything from here. A progress note dated 7/23/2025 documented Resident #2 was not sleeping at night, stayed up all night, and was verbally aggressive to staff. Nurse able to re-direct resident.
A 7/26/25 behavior progress note stated that while the nurse was in the lock down unit Resident #2 was witnessed using a butter knife to attempt to take the brackets off the window or pry the window open, the aide that witnessed this got him to give her the knife.
Progress note dated 8/6/25 stated that Resident #2 declined to have a wander guard on his ankle. Resident #2 takes the wander guard off and continues on 1:1 care.
A police report related to an elopement of Residents #1 and #2, which occurred on 8/30/2025, included documentation that a call was received from the facility at 7:13 PM to report a missing person – adult endangered. The description stated a window was broken during the escape attempt. The officer responded to a missing person and stolen vehicle at the facility. During the course of the investigation it was discovered that room [ROOM NUMBER] had a broken window, which was used by Resident #1 and Resident #2 to escape the nursing home. At approximately 8:04 pm, dispatch received a call reporting the potential whereabouts of Resident #2 at a local store approximately 1.8 miles from the facility. At approximately 11:59 pm, dispatch received a call with the whereabouts of Resident #1, who was observed walking on Interstate 10 near the 255 east bound mile marker. The stolen vehicle was located at mile marker 254 on the side of the road. The location where Resident #1 was located was approximately 40 miles from the facility. Resident #1 had an active warrant and was arrested and transported to jail.
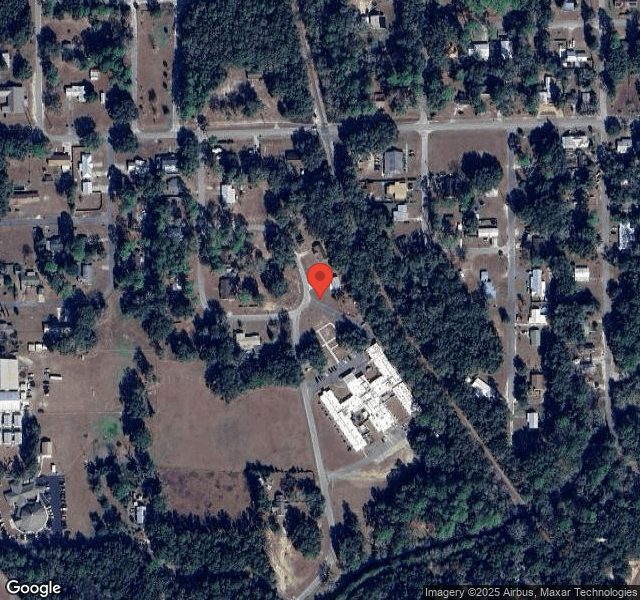
The facility is surrounded by wooded areas on the back and left and right sides, with access to highways in front and on the sides of the building. There is easy access to a creek area with a portion of the creek unfenced near the facility. Both Resident #1 and #2 faced hazards along the paths of the elopement which included the potential of being hit by a vehicle, being involved in a motor vehicle accident, being abducted, falling, and/or drowning which could have resulted in serious physical injury or death. Resident #1, who stole a facility employee's vehicle which was left unsecured with the window open and keys in the vehicle from the parking lot, drove it approximately 40 miles on a busy Interstate and then abandoned the vehicle and was found walking along the interstate near midnight in the dark experienced an increased level of risk based on the distance, method, and location traveled.
A timeline of events of the elopement of Residents #1 and #2 on 8/30/2025 based on witness statements collected by the facility describe the following:
Staff Member F, a certified nursing assistant, was assigned to 1:1 supervision of Resident #2 on 8/30/2025. According to the Administrator, who is also the Risk Manager, based on the facility investigation, Residents #1 and #2 were last seen on 8/30/2025 between 6:30 – 6:50 pm during change of shift. An announcement was made on the overhead page system for elopement at 7:05PM (which was 7 minutes prior to the time Staff Member F reported to ask for help in finding the residents). At approximately 7:00 PM, per witness statement, Resident #1 went to the bathroom and Staff Member F exited the doors of the locked unit where Residents #1 and #2 resided to get someone to sit with Resident #2 while she used the restroom. At 7:10pm, Staff Member F knocked on the door to check on him and there was no answer. Staff Member F entered the room next door and noticed the window was busted out and at approximately 7:12 PM ran to the nurses' station to get help finding the two residents. Staff Member P made a witness statement that the elopement announcement occurred at 7:15pm. The Administrator reported that Resident #2 was spotted in town at 7:44PM.
On 9/11/2025, an interview was conducted with Staff Member H, who found Resident #2 after he eloped from the facility on 8/30/2025. Staff Member H said she was in a vehicle and observed Resident #2 walking across the highway to the store and stopped next to Resident #2 speaking with him. She stated Resident #2 had a mouth full of snuff and asked if she would take him to Lake City. Staff Member H described that three other staff members pulled into the parking lot along with law enforcement and she observed Resident #2 state to law enforcement that he and Resident #1 left the facility through the window, Resident #1 got into a truck in the parking lot, but he did not because he does not steal. She reported Resident #2 said, “I am no thief.” Staff Member H described the facility's procedure for elopement as “Once a page is announced of an elopement, we report to the nurses station of where the elopement occurred and receive a blue card telling us where we are assigned to search for missing resident, once that area is searched, we return it to the nurses' station. If the resident is not located after 10 minutes, law enforcement is to be notified.”
In an interview with the Administrator on 9/8/2025 at 1:18 pm, the administrator confirmed the facility does not have a policy for resident supervision or one-to-one (1:1) supervision. A follow up interview with the Regional [NAME] President of Operations (RVPO) and the Regional Director of Clinical Services (RDCS) on 9/8/2025 at 4:08 pm confirmed there is not a policy for supervision, and this includes no policy for staff expectations for staff observing residents on 1:1 supervision but there was training after the elopements happened. The RDCS was not able to answer what type of training or expectations occurred prior to the elopements. The RVPO brought a set of toenail clippers to the interview and described them as the implement thought to have been used by Resident #2 to cut the wire located in his room which powered the gate alarm to the gate believed to have been used to exit the facility during the elopement on 8/30/2025. The RVPO and RDCS confirmed the wires powering the alarm were located in a resident room on a secured, locked unit and accessible to the resident.
The facility policy Elopement (N-1031 effective date 9/21/2016 revised 8/1/2020) revealed, Patients to be evaluated on admission, re-admission, 7 days post admission, quarterly, with a significant change, and elopement event using the risk tool. Further review of best practice training only reveals that an organized search will be conducted immediately when a resident is determined missing (usually the resident does not go far from the facility unless it is an alert-oriented resident who has planned his leave). During the first 10 minutes of discovering that a resident is missing states time is important, announce all staff to a central location, search facility, search outside grounds, notify the executive director and director of clinical services, notify the police within 10 minutes of discovering the resident is missing.
Staff training information that was given after the 8/30/25 incident reveals, One to one supervision is assigned to a resident based on behaviors that require monitoring. This could be risk of elopement, suicidal ideation, attempts to harm self or others. The staff should always place themselves in a location where they have a clear view to maintain observation of the resident and to be close enough to the resident to intervene should a behavior occur.
Resident #4
A record review for Resident #4 included the following diagnoses: schizoaffective disorder, anxiety, trauma, “brittle” diabetic, anemia, other impulse disorders, restlessness and agitation, major depressive disorder, single episode, personal history of traumatic brain injury, mixed hyperlipidemia, epilepsy, intractable with status epilepticus, abnormal involuntary movements.
A care plan was initiated on 1/11/2022 and most recently revised on 8/6/2025 for behaviors related to agitation, physically aggressive and combative with staff/residents and refusal of care, described that Resident #4 gets on the floor on his hands/knees disrobing and wandering in and out of others room, suffers from impulse disorder (sexual) and banging head/face episodes against wall. Resident #4 refuses to wear his helmet daily. The care plan included documentation under the heading “Interventions” that, on 8/31/2024, Resident #4 was 1:1 supervision and became hostile and overpowered the aide and entered into a fellow resident's room and struck the resident after he exited out the opposite door when using the restroom. Both parties were separated and addressed.
Another care plan was initiated on 1/11/2022 for elopement risk wanderer related to disorientation to place, impaired safety awareness, resident wanders aimlessly, significantly intrudes on the privacy or activities. Interventions included: 1:1 supervision 24/7 for safety due to aggressive behaviors with others. DO NOT sit inside resident's room – sit in the doorway facing him so that he remains in your visual field – If he goes into the restroom, you are to stand by the door with it cracked, to ensure that he does not go through the door on the other side. This care plan was initiated on 3/12/2023 with a most recent revision on 9/8/2025.
The most recent MDS assessment for Resident #4 was completed on 7/1/2025 and documented a BIMS score of 9, which indicated “moderate problems with thinking or memory” according to Cleveland Clinic accessed at https://my.clevelandclinic.org/health/diagnostics/bims-score on 9/17/2025.
A progress note dated 9/4/2025 at 5:40am documented “Resident was observed waking from sleep and immediately began pacing rapidly up and down the halls. Assigned CNA followed for supervision. Resident began attempting to exit through the doors and became agitated. Resident [#4] went out the facility along with 3 other staff members. The other nurse on shift attempted to support the resident to prevent him from falling. During the intervention, the resident forcefully moved his head forward and made contact with nurse. Resident then attempted to leave the premises and fell into the bushes hitting his head. Resident was noted with abrasions to his left forehead and left knee. Due to continued attempts to leave the facility and inability of staff to maintain control, law enforcement was contacted. Resident [#4] was redirected back into the facility prior to their arrival. Police arrived shortly thereafter. Resident [#4] continues to be combative and agitated.”
A psychiatric progress note date 8/18/2025 documented “The patient is seen today at the request of the staff after a report of the patient hitting a staff member. Staff reports that the patient was informed not to exit the building, and he responded aggressively and hit staff. The patient was temporarily restrained by holding his hands/arms in order to prevent him from further hitting the staff and once he was calm, his 1:1 CNA was changed out.”
A psychiatric service note dated 8/17/2025 documented Resident #4 “has consistently demonstrated psychotic symptoms, including fixed delusions, auditory hallucinations, disorganized speech with derailment and incoherence, and grossly disorganized behavior.”
A progress note dated 8/15/2025 noted “Resident attacked PCA (patient care assistant) assigned to 1:1 with him. Resident was informed not to exit building and punched staff in chest. Staff member restrained resident to ensure safety and resident then head-butted him. PCA removed from 1:1 new 1:1 placed with resident.”
A transfer/discharge notice signed by the Administrator on 07/04/2025 documented that a discharge notice was provided to the resident/legal guardian for the reason “Your needs cannot be met in this facility” and “the safety of other individuals in this facility is endangered.” The document also included a brief explanation to support this action as “physical aggression toward staff, safety of staff and others compromised by his impulsive aggressive behaviors. Intervention unsuccessful in managing his behavior and impulsive aggressive behavior resulting in [involuntary psychological examination].
A PASRR (pre-admission screening and resident review) level 2 dated 7/11/2025 documented that any receiving nursing facility should assess the patient to confirm they are able to meet his needs and ensure the patient's safety, as well as the safety of others.
On 9/8/2025 at 3:15 pm at the end of a hallway with patient rooms, a staff member and a younger resident were observed standing. The resident, later identified as Resident #4, had a raised red mark in the center of his forehead. A record review for Resident #4 included a progress note dated 9/8/2025 and described that Resident #4 “hit and head butted his head on the floor, he later hit his head on his bed siderail and then got up to go to the bathroom and hit his head on the door. A later note at 5:14pm documented the medical director was notified and advised “if resident is not complaining then just continue to monitor. Resident has not had any change in condition.”
On 9/9/2025 at 11:30 am, Resident #4 was observed in the tv area sitting in a chair with CNA S near him. CNA S said she was trained to be within arm's reach for 1:1 observation and agreed Resident #4 exhibits aggressive behavior but said she had not received any training in how to deal with these behaviors.
On 9/9/2025 at approximately 3:00 pm several law enforcement vehicles and personnel were observed in front of the facility entrance and, at 3:19 pm, an interview took place with Registered Nurse (RN) I, who explained Resident #4 punched her in the face and then assaulted a law enforcement officer when they were taking him out of the building.
A certificate of Professional Initiating Involuntary Examination dated 9/9/2025 at 11:30am listed that “[Resident #4] has become psychotic, and violent, impulsive and has been physically aggressive towards staff. He has also assaulted the nurses. He is danger to others in his current state and needs a higher level of care to ensure his safety and the safety of others. Pt has failed all interventions by staff to help alleviate his current symptoms, due to these impulsive, unpredictable and violent behaviors, he needs a higher level of care to ensure the safety of others.” The form was signed by a doctor of nursing practice who is a psychiatric advanced practice registered nurse.
On 9/9/2025 at 11:35am, Certified Nursing Assistant (CNA) B said in an interview that she doesn't feel safe working with Resident #4 and has observed aggressive behaviors and is aware Resident #4 tries to leave the building. She expressed that they were trained to back away and let him calm down, try to redirect him, and just stay close to him when he's running and alert the nurse. She said there isn't a specific way for staff to communicate or respond when the events happen.
An interview with the Nurse Unit Manager (Staff Member R) on 9/9/2025 at 4:27 pm revealed that she said she has worked at the facility since May 13, 2025 and Resident #4 has been assigned 1:1 supervision for all the time she has worked at the facility. She described the 1:1 supervision duties for Resident #4 as “to make sure we kept ourselves and him safe, to be close enough to prevent bodily harm, to keep eyes on. We sit in the door[way] because it was very sporadic with his behaviors. He's been here the whole time I've been here and the behaviors are the same since he came. I was trained to keep him in the room as much as possible, to stay in the room, and to keep him at arms distance and to keep him from getting out. The only training we had was abuse and neglect training and told us to redirect him. I try to talk to him; I can't put my hands on him. I can't put my hands on him to restrain him. When he's on the floor I was told not to do anything to him because if I put my hands on him he thinks I'm part of his game.” She confirmed that if staff see him involved in acts of self-harm there is no action other than to watch him and report it.
In an interview on 9/10/2025 at 5:12 pm, the psychiatric nurse practitioner assigned as the psychiatric services provider seeing Resident #4 said she has been seeing Resident #4 for about one month and agreed that the facility is not a safe setting for Resident #4, emphasizing “not at all.” She added, “I reached out today to ask why he isn't in a mental health facility and it's so clear that he can't manage his voices and they said that is a good idea. It takes specialized people to help to take care of them. I was talking to another resident and he said, ‘that guy was standing over me in my bed the other day – is he violent?' And the nurse came and they are all scared of him, I know that's true.”
On 9/11/2025 at approximately 9:50am, an interview took place with the Administrator, the RVPO, and the RDCS regarding the facility's ability to meet the needs for safety for Resident #4 and why the facility continues to readmit Resident #4 after multiple discharges related to aggression and exiting the facility in which an involuntary psychological examination was ordered. The RVPO said that they have discussed it and reached out to the Long-Term Care Ombudsman and other facilities who refuse to accept Resident #4, and they take him back because “we'll be in trouble with the state if we don't.” The Administrator was asked about the discharge notice signed on July 4, 2025, which she signed and documented that Resident #4's needs could not be met at the facility and what had changed in Resident #4's condition or the services offered by the facility that indicated his needs could be met at the facility. The response was that “he's our resident and we have to take him back.” During the interview, copies of documentation of communication with the Ombudsman and requests to other facilities to accept Resident #4 were requested but not provided.
CRITICAL
(L)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected most or all residents
⚠️ Facility-wide issue
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record reviews, interviews, and policy reviews, the facility failed to prevent abuse and neglect resultin...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record reviews, interviews, and policy reviews, the facility failed to prevent abuse and neglect resulting in an elopement for two residents (Residents #1 and #2) while in a secured and locked unit and while Resident #2 was under one-to-one supervision creating a potential for serious injury or death for both residents. The facility failed to prevent neglect for Resident #3, who was immobile and left in her room with the body of her deceased roommate for three hours resulting in serious psychosocial harm. The facility failed to prevent abuse by Resident #4, who suffered injuries from self-harm and was removed from the facility because of physical aggression toward a staff member while under one-to-one supervision. The cumulative effect of the failures resulted in potential for abuse and/or neglect for 85 out of 85 residents. Cross reference to F689 (Residents #1, #2, and #4), F550 (Resident #3), and F656 (Residents #1, # 2, and #4).This situation resulted in a finding of Immediate Jeopardy at a scope and severity of widespread, (L). The facility's Administrator was notified of the Immediate Jeopardy on 9/11/2025 at 2:30 PM. The Immediate Jeopardy was determined to have begun on 8/08/2025. At the time of the survey exit on 9/11/2025, the Immediate Jeopardy was ongoing. Resident #1 and #2
A record review for Resident #1 included diagnoses of chronic kidney disease stage 3, hyperlipidemia, generalized anxiety, hypertension, Atrial fibrillation, chronic systolic heart failure, and Traumatic Brain Injury. A minimum data set (MDS) assessment, dated 8/12/2025, included a brief interview for mental status score (BIMS) of 7. A score of 0-7 indicates severe problems with thinking or memory according to Cleveland Clinic, accessed at my.clevelandclinic.org on 09/17/2025. A comprehensive care plan initiated for Resident #1 on 8/5/2025 included a care plan for elopement risk/wanderer related to impaired safety awareness/wanders aimlessly with a goal for safety to be maintained. Interventions included assess for elopement risk, distract from wandering by offering pleasant diversions, electronic monitoring device, and place on secured unit under increased supervision. A psychiatric admission note dated 8/6/2025 documented “patient presents guarded and non-cooperative initially during interview, patient states, I don't ever sleep, and I just want to get out of here.”
A record review for Resident #2 documented admission to the facility occurred on 6/17/2025 with diagnoses of unspecified dementia, type 2 diabetes, difficulty in walking, cognitive deficits, and mood disorder. On 6/17/25, an elopement risk screen was completed which indicated a score of 3.0, indicating at risk for elopement. Review of the care plan for Resident #2 revealed there was a care plan initiated on 6/18/2025 documenting “resident is an elopement risk/wanderer related to disoriented to place, impaired safety awareness, and resident wanders aimlessly. Interventions include assess for elopement risk, distract resident from wandering by offering pleasant diversions and structured activities, electronic monitoring device per MD (doctor) orders, and place on the unit for increased supervision. On 6/20/2025, Resident #2's care plan was updated to “resident being placed on 1:1 supervision due to cutting off his wander guard bracelet and exit seeking.” A progress note dated 6/20/2025 at 11:40 pm stated “at approximately 2225 pm (10:25PM) CNA (certified nursing assistant) assigned as 1:1 stated Resident #2 was missing, the nurse checked patient's room and confirmed Resident #2 was not present, observed patient window inside of room was opened, and no visual of resident outside of room, DON (Director of Nursing) was notified and elopement protocol was initiated.
A progress note dated 7/13/2025 stated, “ .alarm to the back door going off, when checking it out, they said that [Resident #2] was messing with the alarm on the door, they saw him doing it and told him several times to leave the door alone, after the alarm would not shut off, this nurse trouble shooting the problem and noticed that [Resident #2] had pulled the wires and tripping the connections to the alarm. A temporary fix on the door alarm, risk manager and maintenance is aware. [Resident #2] continues on 1:1 supervision.”
A 7/26/25 behavior progress note stated that. while the nurse was in the lock down unit, Resident #2 was witnessed using a butter knife to attempt to take the brackets off the window or pry the window open, the aide that witnessed this got him to give her the knife.
A police report related to the elopement of Residents #1 and #2, which occurred on 8/30/2025, included documentation that a call was received from the facility at 7:13PM to report a missing person – adult endangered. The description given stated a window was broken during the escape attempt. The officer responded to a missing person and stolen vehicle at the facility. During the course of investigation, it was discovered that room [ROOM NUMBER] had a broken window and was used by Resident #1 and Resident #2 to escape the nursing home. At approximately 8:04 pm, dispatch received a call reporting the potential whereabouts of Resident #2 at a store approximately 1.8 miles from the facility. At approximately 11:59 pm, dispatch received a call with the whereabouts of Resident #1, who was observed walking on Interstate 10 near the 255 east bound mile marker. The stolen vehicle was located at mile marker 254 on the side of the road. The location where Resident #1 was located was approximately 40 miles from the facility. Resident #1 had an active warrant and was arrested and transported to jail.
In an interview with the Facility Administrator on 9/8/2025 at 1:18pm, the Administrator confirmed the facility does not have a policy for resident supervision or one-to-one (1:1) supervision. A follow up interview with the Regional [NAME] President of Operations (RVPO) and the Regional Director of Clinical Services (RDCS) on 9/8/2025 at 4:08 pm confirmed there is not a policy for supervision, and this includes no policy for staff expectations for staff observing residents on 1:1 supervision, but there was training after the previous elopements happened. The RDCS was not able to answer what type of training or expectations occurred prior to the elopements.
Staff training information that was given to the staff reveals: one to one supervision is assigned to a resident based on behaviors that require monitoring. This could be risk of elopement, suicidal ideation, attempts to harm self or others. The staff should always place themselves in a location where they have a clear view to maintain observation of the resident and to be close enough to the resident to intervene should a behavior occur.
Resident #3
On 9/8/25, an interview was conducted with Resident #3 that indicated that she has been very upset lately because of her roommate's death on 8/27/25. She stated, “It was a horrible and upsetting event for me. We became close friends since I got here a year ago. She didn't have any family, so we looked out for one another”. Resident #3 stated “I stayed with her until she took her last breath. I specifically told them that I would, but once she passed, I want to be moved out of the room. I did not want to stay in the room with a dead body”.
With tears in her eyes, she stated “I was told that I had to stay in my room with the door closed so the room could stay cool until the funeral home came “. At this time the resident began crying and was visibly shaking and trembling in her upper body and hands. Her face was red in color and constantly wiping tears from her face as she describes listening to Staff Member D come into the room to bathe and dress her roommate. Afterwards, Staff D left the room and shut the door. Resident #3 stated she was left inside the room with her roommate's dead body in the bed beside her for almost three hours. Resident #3 stated that she asked to be moved into a room across the hall that was empty until the funeral home came. She stated she was told that they did not have time to move her. Resident #3 begins crying again with a trembling voice and visibly shaking when she stated, No one came in to check to see if I was okay, and when someone finally came into my room, it was some man with a gurney. I lost it then, I had to stay in here by myself with all of that going on. I had to listen to everything that man from the funeral home was doing, taking the bag out, lifting the body up, and putting her in the bag. Listening as he zipped up the bag was horrible. All I could do was cry and listen. I had to watch him push her body out of the room, he came right in front of me with her on the gurney. No one from the facility ever came in to help or check on me. That is an image I didn't want to see and now I can't get it out of my mind. I haven't been able to sleep or eat since then. And now I am having to get therapy because of it. It has just added more stress to me and to my anxiety.
A record review for Resident #3 included a diagnosis of generalized anxiety disorder, muscle wasting and atrophy, chronic pain and depression. A minimum data set (MDS) assessment dated [DATE] included a brief interview for mental status score (BIMS) of 15. A score of 13-15 indicates intact cognition according to Cleveland Clinic accessed at my.clevelandclinic.org on 09/17/2025. A comprehensive care plan was initiated on 10/16/2024 for Resident #3 indicating that she is dependent on staff to meet emotional, physical, intellectual, and social needs related to her diagnosis of generalized anxiety and has a mood problem related to anxiety and depression. Interventions include administering medications as ordered and monitoring for side effects, assisting resident to identify strengths and positive coping skills.
A psychiatry progress note dated 8/20/25 revealed Resident #3 discussed recent stressors such as coping with her roommate's terminal diagnosis. On further review, a progress note dated 8/27/25 at 2:20 pm stated that Resident #3 was seen by a therapist indicating she has “increased anxiety related to the death of her roommate early this AM”. On 9/5/25, a progress note from the therapy services was reviewed indicating the need of ongoing psychotherapy for anxiety and grief related to the death of her roommate. Resident #3 discussed ongoing symptoms of not sleeping, particularly around the time of death, and increased anxiety. Psychotherapy services will continue and will address trauma symptoms related to the passing of the roommate.
An Interview with the Medical Director for Resident #3 was conducted on 9/9/25 at 3:35 pm. The Medical Director revealed that she is seen by her physician on a weekly basis most of the time. The Medical Director does not recall if Resident # 3 expressed any emotions related to her roommate's death, but does state, I know she was very close to her roommate, and I do believe there would be some definite emotional stress. I know I wouldn't want to be in a room with a dead body, I would have a problem with it myself”.
An interview with Staff Member R (Nurse Unit Manager) on 9/9/25 at 4:30 pm was conducted. She stated that staff receives ongoing training on abuse and types of abuse. Staff member R was able to explain the definition of abuse and different examples. Staff member R further stated, “the protocol for death of any resident with a roommate would be to move the other resident out of the room before providing postmortem care”. She agreed that “it is undignified to have another resident present I room for postmortem care and the facility should take every possible measure to honor the roommates request to be removed from the room”.
A follow up interview was conducted with Resident #3. She stated the Administrator came to see her on 9/9/25 around 6:20 pm in regard to the event that took place on 8/27/25. She further states the Administrator apologized to her for what she went through on 8/27/25 with her roommate's passing and the events that took place afterwards. Resident #3 stated that she let the Administrator know she was still having difficulty sleeping because every time she closed her eyes all she could see is her roommate being zipped up in the body bag and leaving her room on the gurney. Resident #3 states she asked the housekeeper earlier today to make up the roommate's bed because it was too upsetting to see the empty blue mattress where her roommate once resided. Resident #3 continues to receive counseling services due to issues coping with her roommate's death.
The facility policy for Abuse, Neglect and Exploitation (N-1265 effective date 11/30/2014 revised date 11/16/2022) states, It is inherent in the nature and dignity of each resident at the center that he/she be afforded basic human rights, including the right to be free from abuse, neglect, mistreatment, exploitation and misappropriation of property. One of the examples states that involuntary seclusion is defined as separation of a resident from other residents or from his/her room or confinement to his/her room (with or without roommates) against the resident's will or the will of the resident representative.
Resident #4
On 9/8/2025 at 3:15 pm at the end of a hallway with patient rooms, a staff member and a younger resident were observed standing. The resident, later identified as Resident #4, had a raised red mark in the center of his forehead.
A record review for Resident #4 included a progress note dated 9/8/2025 and described that Resident #4 “hit and head butted his head on the floor, he later hit his head on his bed siderail and then got up to go to the bathroom and hit his head on the door. A later note at 5:14 pm documented the medical director was notified and advised “if resident is not complaining then just continue to monitor. Resident has not had any change in condition.”
During an interview on 9/9/2025 at 11:35am, Certified Nursing Assistant (CNA) B said Resident #4 used to wear a safety helmet, but it had been awhile since she's seen it; no training was provided in regard to the helmet. She said she was aware he tried to leave and was here Saturday when he left but wasn't assigned to him.
On 9/9/2025 at approximately 3:00pm, several law enforcement vehicles and personnel were observed in front of the facility entrance. At 3:19 pm, an interview took place with Registered Nurse (RN) I, who explained Resident #4 punched her in the face and then assaulted a law enforcement officer when they were taking him out of the building.
During an interview with the interim director of nursing (DON) on 9/10/2025 at 12:24 pm, she explained that Resident #4 had been on 1:1 supervision since she came to the facility in January 2025 and said she is involved in his care planning. She described that “after the behaviors started getting more aggressive, we moved staff from sitting in the room to sitting outside the room. We have been trying to get things in place to get him more comfortable. The change to having staff sit outside the room was sometime in June.”
In an interview with the Social Services Assistant (Staff Member L) on 9/10/2025 at 9:55am, she explained that she has performed 1:1 supervision duties for Resident #4 and received training for this which included “talk in soft tones and try to deescalate and talk in a calm voice and keep hands down; if that doesn't work, keep doing the same thing and get out of his way.” She further explained that she was not provided with a form of communication such as a phone or walkie talkie to ask for help and that she would use her personal phone or shout for help if she needed it. She said that, when performing duties with Resident #4, sometimes she felt safe and sometimes she didn't.
In an interview on 9/10/2025 at 5:12pm, the Psychiatric Nurse Practitioner assigned as the psychiatric services provider seeing Resident #4 said she has been seeing Resident #4 for about one month and agreed that the facility is not a safe setting for Resident #4, emphasizing “not at all.” She added, “I reached out today to ask why he isn't in a mental health facility and it's so clear that he can't manage his voices and they said that is a good idea. It takes specialized people to help to take care of them. I was talking to another resident and he said, 'that guy was standing over me in my bed the other day – is he violent?' And the nurse came and they are all scared of him, I know that's true.”
During an interview on 9/11/2025 at 10:46am, the interim director of nursing (DON) provided the task documentation for the one-to-one activities for Resident #4 for August 2025 and there were only 5 days when diversional activities were documented. The DON said that there is a problem with ability to document and agreed that there is no other place in the record where the care plan interventions for diversional activities would be documented.
During the entrance conference on 9/8/2025 at 1:18pm, the Facility Administrator said there was no facility policy for resident supervision or 1:1 supervision.
On 9/8/2025 at 4:08pm, the regional director of clinical services (RDCS) confirmed in an interview that the facility does not have a policy for supervision and this includes no policy for staff expectations for staff observing residents on 1:1 supervision.
A record review for Resident #4 included the following diagnoses: schizoaffective disorder, anxiety, trauma, “brittle” diabetic, anemia, other impulse disorders, restlessness and agitation, major depressive disorder, single episode, personal history of traumatic brain injury, mixed hyperlipidemia, epilepsy, intractable with status epilepticus, abnormal involuntary movements.
A care plan was initiated on 1/11/2022 and most recently revised on 8/6/2025 for behaviors related to agitation, physically aggressive and combative with staff/residents and refusal of care, described that Resident #4 gets on the floor on his hands/knees disrobing and wandering in and out of others room, suffers from impulse disorder (sexual) and banging head/face episodes against wall. Resident #4 refuses to wear his helmet daily. The care plan included documentation under the heading “Interventions” that, on 8/31/2024, Resident #4 was 1:1 supervision and became hostile and overpowered the aide and entered into a fellow resident's room and struck the resident after he exited out the opposite door when using the restroom. Both parties were separated and addressed.
Another care plan was initiated on 1/11/2022 for elopement risk wanderer related to disorientation to place, impaired safety awareness, resident wanders aimlessly, significantly intrudes on the privacy or activities. Interventions included: 1:1 supervision 24/7 for safety due to aggressive behaviors with others. DO NOT sit inside resident's room – sit in the doorway facing him so that he remains in your visual field – If he goes into the restroom, you are to stand by the door with it cracked, to ensure that he does not go through the door on the other side. This care plan was initiated on 3/12/2023 with a most recent revision on 9/8/2025. Other interventions include distract resident from wandering by offering pleasant diversions, structured activities, food, conversation, television, book. Resident prefers: (blank) date initiated 1/11/2022.
A psychiatric progress note dated 8/17/2025 documented that “staff note that he becomes easily bored and that his attention fluctuates during interactions. His presentation remains consistent with chronic psychosis, with ongoing negative symptoms such as blunted affect and reduced motivation. Behavioral interventions have recently been introduced, focusing on structured reward-based strategies to encourage engagement and reduce maladaptive behaviors. Initial staff feedback suggests that he responds intermittently to these supports.” Another psychiatric noted dated 8/29/2025 noted “Staff report that the patient's attention fluctuates during interactions and that he becomes easily bored.”
A task list for one-to-one activities reviewed for past 30 days listed documentation for only the following days: 8/12/2025, 8/13/2025, 8/15/2025, and 8/20/2025. Resident #4 was observed to be on 1:1 observation with staff on 9/8/2025 (date of survey entry) and the date of this review was 9/9/2025 – no documentation identified for 9/9/2025.
The activities/participation (Question 2) documenting for each of the 4 dates that talking was the only activity used out of several listed which included arts and crafts, board games, exercise, games, gardening, meditation/relaxation, music, and others.
A progress note dated 8/15/2025 noted “Resident attacked PCA (patient care assistant) assigned to 1:1 with him. Resident was informed not to exit building and punched staff in chest. Staff member restrained resident to ensure safety and resident then head-butted him. PCA removed from 1:1, new 1:1 placed with resident.”
A psychiatric progress note date 8/18/2025 documented “The patient is seen today at the request of the staff after a report of the patient hitting a staff member. Staff reports that the patient was informed not to exit building, and he responded aggressively and hit staff. The patient was temporarily restrained by holding his hands/arms in order to prevent him from further hitting the staff and once he was calm, his 1:1 CNA was changed out.”
A progress note dated 9/4/2025 at 5:40am documented “Resident was observed waking from sleep and immediately began pacing rapidly up and down the halls. Assigned CNA followed for supervision. Resident began attempting to exit through the doors and became agitated. Resident [#4] went out the facility along with 3 other staff members. The other nurse on shift attempted to support the resident to prevent him from falling. During the intervention, the resident forcefully moved his head forward and made contact with nurse. Resident then attempted to leave the premises and fell into the bushes hitting his head. Resident was noted with abrasions to his left forehead and left knee. Due to continued attempts to leave the facility and inability of staff to maintain control, law enforcement was contacted. Resident [#4] was redirected back into the facility prior to their arrival. Police arrived shortly thereafter. Resident[#4] continues to be combative and agitated.”
CRITICAL
(L)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0865
(Tag F0865)
Someone could have died · This affected most or all residents
⚠️ Facility-wide issue
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, records reviews, a review of the facility QAPI (quality assurance and performance improvement) plan, facili...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, records reviews, a review of the facility QAPI (quality assurance and performance improvement) plan, facility assessment, and event investigation documents, the facility failed to maintain an effective QAPI program to ensure the supervision of residents at risk for elopement, self-harm, and aggressive behaviors (Residents #1, #2, and #4). Cross reference F600, F689.These failures resulted in substandard quality of care at the Immediate Jeopardy level beginning on 8/8/2025.The facility's QAPI committee failed to perform and/or document analysis of events following the elopement while under one-to-one supervision for Resident #2. The facility failed to investigate and/or develop an improvement plan to meet the needs for Resident #4 who had multiple discharges and readmissions to the facility, including after the Administrator issued a transfer discharge notice on July 4, 2025, which identified that Resident #4's needs could not be met at the facility.This situation resulted in a finding of Immediate Jeopardy at a scope and severity of widespread, (L). The facility's Administrator was notified of the Immediate Jeopardy on 9/11/2025 at 2:30 PM. The Immediate Jeopardy was determined to have begun on 8/08/2025. At the time of the survey exit on 9/11/2025, the Immediate Jeopardy was ongoing.The findings include:Resident #4A record review for Resident #4 included the following diagnoses: schizoaffective disorder, anxiety, trauma, brittle diabetic, anemia, other impulse disorders, restlessness and agitation, major depressive disorder, single episode, personal history of traumatic brain injury, mixed hyperlipidemia, epilepsy, intractable with status epilepticus, abnormal involuntary movements.A care plan was initiated on 1/11/2022 and most recently revised on 8/6/2025 for behaviors related to agitation, physically aggressive and combative with staff/residents and refusal of care, described that Resident #4 gets on the floor on his hands/knees disrobing and wandering in and out of others room, suffers from impulse disorder (sexual) and banging head/face episodes against wall. Resident #4 refuses to wear his helmet daily. The care plan included documentation under the heading Interventions that, on 8/31/2024, Resident #4 was 1:1 supervision and became hostile and overpowered the aide and entered into a fellow resident's room and struck the resident after he exited out the opposite door when using the restroom. Both parties were separated and addressed.Another care plan was initiated on 1/11/2022 for elopement risk wanderer related to disorientation to place, impaired safety awareness, resident wanders aimlessly, significantly intrudes on the privacy or activities. Interventions included: 1:1 supervision 24/7 for safety due to aggressive behaviors with others. DO NOT sit inside resident's room - sit in the doorway facing him so that he remains in your visual field - If he goes into the restroom, you are to stand by the door with it cracked, to ensure that he does not go through the door on the other side. This care plan was initiated on 3/12/2023 with a most recent revision on 9/8/2025.Other interventions include distract resident from wandering by offering pleasant diversions, structured activities, food, conversation, television, book. Resident prefers: (blank) date initiated 1/11/2022.Progress notes describe events of exiting the facility, self-harm, and/or physical aggression towards others. These included an event on 8/15/2025 when Resident #4 attempted to exit the building and punched a staff member in the chest. The record documented that the staff member restrained resident to ensure safety and resident then head-butted him. A psychiatric progress note dated 8/18/2025 documented The patient is seen today at the request of the staff after a report of the patient hitting a staff member. Staff reports that the patient was informed not to exit building, and he responded aggressively and hit staff. The patient was temporarily restrained by holding his hands/arms in order to prevent him from further hitting the staff and once he was calm, his 1:1 CNA was changed out.Another event occurred on 9/4/2025 when Resident #4 began attempting to exit through the doors and became agitated. Resident #4 exited the building and 3 staff members followed. The resident attempted to leave the premises and fell into the bushes hitting his head and was noted with abrasions to his left forehead and left knee. Law enforcement was called to respond and Resident #4 continued to be combative and agitated. A psychiatric progress note dated 9/6/2025 documented Resident #4 remains psychiatrically unstable in the context of worsening psychotic symptoms and concurrent medical decompensation. Resident #4 was transferred to the emergency room for medical clearance and stabilization of hyperglycemia; resume psychiatric management following clearance.On 9/8/2025 at approximately 3:15pm, Resident #4 was observed with a red, raised area to his forehead. The medical record documented on 9/8/2025 that a CNA reported Resident #4 hit and head butted his head on the floor, on his bed siderail, and then got up to go to the bathroom and hit his head on the door.On 9/9/2025, Resident #4 punched a nurse in the face and was removed from the facility by law enforcement. A certificate of Professional Initiating Involuntary Examination dated 9/9/2025 at 11:30am listed that [Resident #4] has become psychotic, and violent, impulsive and has been physically aggressive towards staff. He has also assaulted the nurses. He is danger to others in his current state and needs a higher level of care to ensure his safety and the safety of others. Pt has failed all interventions by staff to help alleviate his current symptoms, due to these impulsive, unpredictable and violent behaviors, he needs a higher level of care to ensure the safety of others.In an interview on 9/10/2025 at 5:12pm, the psychiatric nurse practitioner assigned as the psychiatric services provider seeing Resident #4 said she has been seeing Resident #4 for about one month and agreed that the facility is not a safe setting for Resident #4, emphasizing not at all. She added, I reached out today to ask why he isn't in a mental health facility and it's so clear that he can't manage his voices and they said that is a good idea. It takes specialized people to help to take care of them. I was talking to another resident and he said, ‘that guy was standing over me in my bed the other day - is he violent?' And the nurse came and they are all scared of him, I know that's true.On 9/11/2025 at approximately 9:50am, an interview took place with the facility administrator, the RVPO, and the RDCS regarding the facility's ability to meet the needs for safety for Resident #4 and why the facility continues to readmit Resident #4 after multiple discharges related to aggression and exiting the facility in which an involuntary psychological examination was ordered. The RVPO said that they have discussed it and reached out to the Long-Term Care Ombudsman and other facilities, who refuse to accept Resident #4, and they take him back because we'll be in trouble with the state if we don't. The Administrator was asked about the discharge notice signed on July 4, 2025, which she signed and documented that Resident #4's needs could not be met at the facility and what had changed in Resident #4's condition or the services offered by the facility that indicated his needs could be met at the facility. The response was that he's our resident and we have to take him back. During the interview, copies of documentation of communication with the Ombudsman and requests to other facilities to accept Resident #4 were requested but not provided.Resident #1 and #2A police report related to the elopement of Residents #1 and #2, which occurred on 8/30/2025, included documentation that a call was received from the facility at 7:13PM to report a missing person - adult endangered. The description given stated a window was broken during the escape attempt. The officer responded to a missing person and stolen vehicle at the facility. During the course of investigation, it was discovered that room [ROOM NUMBER] had a broken window and was used by Resident #1 and Resident #2 to escape the nursing home. At approximately 8:04 pm, dispatch received a call reporting the potential whereabouts of Resident #2 at a store approximately 1.8 miles from the facility. At approximately 11:59 pm, dispatch received a call with the whereabouts of Resident #1, who was observed walking on the interstate. The stolen vehicle was located a mile back on the side of the road. The location where Resident #1 was located was approximately 40 miles from the facility. Resident #1 had an active warrant and was arrested and transported to jail.The facility is surrounded by wooded areas on the back and left and right sides, with access to highways in front and on the sides of the building. There is easy access to a creek area with a portion of the creek unfenced near the facility. Both Resident #1 and #2 faced hazards along the paths of the elopement which included the potential of being hit by a vehicle, being involved in a motor vehicle accident, being abducted, falling, and/or drowning which could have resulted in serious physical injury or death. Resident #1, who stole a facility employee's vehicle which was left unsecured with the window open and keys in the vehicle from the parking lot and drove it approximately 40 miles on a busy Interstate and then abandoned the vehicle and was found walking along the interstate near midnight in the dark experienced an increased level of risk based on the distance, method, and location traveled. A timeline of events of the elopement of Residents #1 and #2 on 8/30/2025 based on witness statements collected by the facility describe the following:Staff Member F, a certified nursing assistant, was assigned to 1:1 supervision of Resident #2 on 8/30/2025. According to the Administrator, who is also the Risk Manager, based on the facility investigation, Residents #1 and #2 were last seen on 8/30/2025 between 6:30 - 6:50 pm during change of shift. An announcement was made on the overhead page system for elopement at 7:05PM (which was 7 minutes prior to the time Staff Member F reported to ask for help in finding the residents). At approximately 7:00 PM, per witness statement, Resident #1 went to the bathroom and Staff Member F exited the doors of the locked unit where Residents #1 and #2 resided to get someone to sit with Resident #2 while she used the restroom. At 7:10pm, Staff Member F knocked on the door to check on him and there was no answer. Staff Member F entered the room next door and noticed the window was busted out and at approximately 7:12 PM ran to the nurses' station to get help finding the two residents. Staff Member P made a witness statement that the elopement announcement occurred at 7:15pm. The Administrator reported that Resident #2 was spotted in town at 7:44PM.On 9/11/2025, an interview was conducted with Staff Member H, who found Resident #2 after he eloped from the facility on 8/30/2025. Staff Member H said she was in a vehicle and observed Resident #2 walking across the highway to the store and stopped next to Resident #2 speaking with him. She stated Resident #2 had a mouth full of snuff and asked if she would take him to Lake City. Staff Member H described that three other staff members pulled into the parking lot along with law enforcement and she observed Resident #2 state to law enforcement that he and Resident #1 left the facility through the window, Resident #1 got into a truck in the parking lot, but he did not because he does not steal. She reported Resident #2 said, I am no thief. Staff Member H described the facility's procedure for elopement as Once a page is announced of an elopement, we report to the nurses station of where the elopement occurred and receive a blue card telling us where we are assigned to search for missing resident, once that area is searched, we return it to the nurses' station. If the resident is not located after 10 minutes, law enforcement is to be notified.During an interview with the administrator on 9/9/2025 at 11:40am, the Administrator identified herself as the Risk Manager.The QAPI minutes reviewed and dated 8/19/2025 included a review of reports that listed reports concerning neglect/abuse and misappropriation which were submitted in July 2025. Despite the inclusion of five reports of neglect, three of which were documented as substantiated, 2 reports of abuse documented as substantiated, and one report of misappropriation documented as substantiated, there is no indication in any of the documentation provided that the facility recognized abuse/neglect/misappropriation as a concern which required a response, action plan, or further investigation through the QAPI program.In an interview with the administrator on 9/10/2025 at 6:16pm, she said they had not considered QAPI review of Resident #4's behavioral needs because the behaviors just started escalating over the past month.In an interview on 9/11/2025 at 9:50am with the Regional [NAME] President of Operations (RVPO), the Regional Director of Clinical Services (RDCS), the Administrator, and the Regional Social Services Director, the Administrator was asked about a transfer discharge notice from his record dated July 4, 2025 which documented that the facility cannot meet his needs. A discussion ensued with the facility leaders present as to why the facility continued to admit Resident #4 with the documented history of aggressive behaviors and the Administrator said she has only been here for 8 months. The RVPO said they have discussed it and reached out to the Ombudsman and other facilities who refuse to take Resident #4 and they take him back because they will be in trouble with the state if they don't. A request was made to provide any documentation they have of refusals to admit and who they have reached out to for assistance in determining their options for accepting or refusing a re-admission for Resident #4. At the time of exit from the survey on 9/11/2025 at approximately 3:00pm, the facility had not provided the documentation.The question was posed to the group to explain what had changed in the resident's condition or with the services offered by the facility between the times when Resident #4 was discharged and the facility documented an inability to meet the needs for Resident #4 and when they readmitted him and they said again that he's our resident and we have to take him back.A review of an ad hoc QAPI meeting dated 5/16/2025 documented the reason was for an elopement event. Under the heading Opportunity for Improvement the facility documented to ensure that residents who exhibited exit seeking behaviors and/or are at risk of elopement receive adequate supervision and behavioral observance by staff in order to prevent elopements and that care is received in accordance with the person-centered plan of care created to address the unique factors that contribute to wandering or elopement risks. The columns on the form labeled data and analysis were blank. There was no evidence provided that data to determine the root cause of the elopement was gathered or analyzed. The facility assessment dated [DATE] was reviewed and documented that staff training/education and competencies included abuse, neglect, and exploitation, care management for persons with dementia and resident abuse prevention. Trauma informed care, mental health/substance use disorders, behavior, dementia, activities of daily living, caring for residents with mental and psychosocial disorders, as well as residents with a history of trauma and/or post-traumatic stress disorder, substance use disorder and implementing nonpharmacological interventions.A review of the facility's 2025 QAPI plan included a plan for systematic analysis as follows: the facility uses a systematic approach to determine when in-depth analysis is needed to fully understand the problem, its cause, and implications of a change. The QAPI team will review data, prioritize opportunities for improvement based on risk, frequency, relevance, cost and feasibility and determine which opportunities will require a performance improvement project. The PIP [performance improvement projects] Team will analyze the problem area by conducting a root cause analysis, identify solutions and develop a performance improvement plan to be implemented. The Plan Do Study Act quality improvement cycle and Root Cause Analysis will be used to address problems and drive performance improvement. Examples of root cause analysis tools include the 5 Whys and the fishbone diagram. QAPI Committees and PIP Teams will review targeted outcomes and will also monitor for potential unintended outcomes created from systematic or process changes. A review of an ad hoc QAPI meeting dated 8/31/2025 consisted of a one-page document identified under the heading of Opportunity for Improvement the facility documented 1:1 supervision procedure and elopement. Under the heading data (assess current situation - what were the results/trend), the facility documented 1:1 supervision requirements not being followed adequately to ensure resident safety and prevent elopement. Under the heading analysis (root cause analysis) the facility documented staff not ensuring resident was correctly supervised while on 1:1 observation allowing an elopement. There was no evidence of an analysis of the data to include the examples listed in the facility QAPI plan such as the 5 Whys and the fishbone diagram.
SERIOUS
(H)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Comprehensive Care Plan
(Tag F0656)
A resident was harmed · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, observation, record, and policy reviews, the facility failed to implement care plan interventions for 4 resi...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, observation, record, and policy reviews, the facility failed to implement care plan interventions for 4 residents (#1, #2, #5, and #11). Resident #11 was negatively impacted by the failure to implement the care plan to assist the resident in communicating his emotional, intellectual, physical, and social needs. The facility's failure to implement care plans related to adequate supervision for residents #1, #2, and #4 resulted in their ability to exit the facility for residents #1, #2, and #4 and for Resident #4 to cause physical injury to himself and others.Cross reference F600, F689.The findings include:Resident #1 and #2
A record review for Resident #1 included diagnoses of chronic kidney disease stage 3, hyperlipidemia, generalized anxiety, hypertension, Atrial Fibralation, chronic systolic heart failure, and TBI. A minimum data set (MDS) assessment dated [DATE] included a brief interview for mental status score (BIMS) of 7. A score of 0-7 indicates severe problems with thinking or memory according to Cleveland Clinic accessed at my.clevelandclinic.org on 09/17/2025. A comprehensive care plan initiated for Resident #1 on 8/5/2025 included a care plan for elopement risk/wanderer related to impaired safety awareness, wanders aimlessly with a goal for safety to be maintained. Interventions included: assess for elopement risk, distract from wandering by offering pleasant diversions, electronic monitoring device and place on secured unit for increased supervision. A psychiatric admission note dated 8/6/2025 documented “patient presents guarded and non-cooperative initially during interview, patient states I don't ever sleep, and I just want to get out of here.”
A record review for Resident #2 documented admission to the facility occurred on 6/17/2025 with diagnoses of unspecified dementia, type 2 diabetes, difficulty in walking, cognitive deficits, and mood disorder. On 6/17/25 an elopement risk screen was completed which indicated a score of 3.0, indicating at risk for elopement. Review of the care plan for Resident #2 revealed there was a care plan initiated on 6/18/2025 documenting “resident is an elopement risk/wanderer related to disoriented to place, impaired safety awareness, and resident wanders aimlessly. Interventions included: assess for elopement risk, distract resident from wandering by offering pleasant diversions and structured activities, electronic monitoring device per MD (doctor) orders and place on the unit for increased supervision. On 6/20/2025 Resident #2's care plan was updated to “resident being placed on 1:1 supervision due to cutting off his wander guard bracelet and exit seeking.” Review of physician orders indicates an order for 1:1 supervision was initiated on 8/29/25 for elopement at 1900.
A progress note dated 6/20/2025 at 23:40 pm stated “at approximately 2225 pm (10:25PM) CNA (certified nursing assistant) assigned as 1:1 with Resident #2 was missing, the nurse checked patients room and confirmed Resident #2 was not present, observed patient window inside of room was opened, and no visual of resident outside of room, DON (director of nursing) was notified elopement protocol was initiated. A psychiatric progress note dated 6/21/2025 documented Resident #2 was able to engage in a rational process of relevant information, able to recognize the importance of medication and treatment compliance, able to recognize his medical condition and consequences of lack of treatment and had the capacity to make decisions related to his need for healthcare or long-term placement. He was documented as able to understand the nature, extent, and probable outcome of not receiving medical care and was alert and oriented to self, place, time, and situation. On 6/21/2025, an elopement risk evaluation was repeated and again indicated a score of 3.0, indicating at risk for elopement. On 6/23/2025, the care plan for Resident #2 was updated for behaviors due to “refusing care and medications, becoming agitated and will curse at staff. He slams the door and tells staff to stop following him, removes his wander guard, and is able to unscrew his window to leave facility. Interventions include administer medications as ordered, anticipate resident's needs, explain all procedures to resident before starting care, if reasonable discuss residents' behaviors and why behavior is inappropriate.”
A progress note dated 7/13/2025 stated, “ .alarm to the back door going off, when checking it out, they said that [Resident #2] was messing with the alarm on the door, they saw him doing it and told him several times to leave the door alone, after the alarm would not shut off, this nurse trouble shooting the problem and noticed that [Resident #2] had pulled the wires and tripping the connections to the alarm. A temporary fix on the door alarm, risk manager and maintenance is aware. [Resident #2] continues on 1:1 supervision.”
A 7/26/25 behavior progress note stated that while the nurse was in the lock down unit, Resident #2 was witnessed using a butter knife to attempt to take the brackets off the window or pry the window open, the aide that witnessed this got him to give her the knife.
A police report related to the elopement of Residents #1 and #2, which occurred on 8/30/2025, included documentation that a call was received from the facility at 7:13PM to report a missing person – adult endangered. The description given stated a window was broken during the escape attempt. The officer responded to a missing person and stolen vehicle at the facility. During the course of investigation, it was discovered that room [ROOM NUMBER] had a broken window and was used by Resident #1 and Resident #2 to escape the nursing home. At approximately 8:04 pm, dispatch received a call reporting the potential whereabouts of Resident #2 at a store approximately 1.8 miles. At approximately 11:59 pm, dispatch received a call with the whereabouts of Resident #1, who was observed walking on Interstate 10. The stolen vehicle was located a mile back on the side of the road. The location where Resident #1 was located was approximately 40 miles from the facility. Resident #1 had an active warrant and was arrested and transported to jail.
In an interview with the facility administrator on 9/8/2025 at 1:18pm, the administrator confirmed the facility does not have a policy for resident supervision or one-to-one (1:1) supervision. A follow up interview with the Regional [NAME] President of Operations (RVPO) and the Regional Director of Clinical Services (RDCS) on 9/8/2025 at 4:08pm confirmed there is not a policy for supervision, and this includes no policy for staff expectations for staff observing residents on 1:1 supervision but there was training after the elopements happened. The RDCS was not able to answer what type of training or expectations occurred prior to the elopements
Resident #4
A record review for Resident #4 included the following diagnoses: schizoaffective disorder, anxiety, trauma, “brittle” diabetic, anemia, other impulse disorders, restlessness and agitation, major depressive disorder, single episode, personal history of traumatic brain injury, mixed hyperlipidemia, epilepsy, intractable with status epilepticus, abnormal involuntary movements.
A care plan was initiated on 1/11/2022 and most recently revised on 8/6/2025 for behaviors related to agitation, physically aggressive and combative with staff/residents and refusal of care, described that Resident #4 gets on the floor on his hands/knees disrobing and wandering in and out of others room, suffers from impulse disorder (sexual) and banging head/face episodes against wall. Resident #4 refuses to wear his helmet daily. The care plan included documentation under the heading “Interventions” that, on 8/31/2024, Resident #4 was 1:1 supervision and became hostile and overpowered the aide and entered into a fellow resident's room and struck the resident after he exited out the opposite door when using the restroom. Both parties were separated and addressed.
Another care plan was initiated on 1/11/2022 for elopement risk wanderer related to disorientation to place, impaired safety awareness, resident wanders aimlessly, significantly intrudes on the privacy or activities. Interventions included: 1:1 supervision 24/7 for safety due to aggressive behaviors with others. DO NOT sit inside resident's room – sit in the doorway facing him so that he remains in your visual field – If he goes into the restroom, you are to stand by the door with it cracked, to ensure that he does not go through the door on the other side. This care plan was initiated on 3/12/2023 with a most recent revision on 9/8/2025. Other interventions include distract resident from wandering by offering pleasant diversions, structured activities, food, conversation, television, book. Resident prefers: (blank) date initiated 1/11/2022.
A psychiatric progress note dated 8/17/2025 documented that “staff note that he becomes easily bored and that his attention fluctuates during interactions. His presentation remains consistent with chronic psychosis, with ongoing negative symptoms such as blunted affect and reduced motivation. Behavioral interventions have recently been introduced, focusing on structured reward-based strategies to encourage engagement and reduce maladaptive behaviors. Initial staff feedback suggests that he responds intermittently to these supports.” Another psychiatric noted dated 8/29/2025 noted “Staff report that the patient's attention fluctuates during interactions and that he becomes easily bored.”
A task list for one-to-one activities reviewed for past 30 days listed documentation for only the following days: 8/12/2025, 8/13/2025, 8/15/2025, and 8/20/2025. Resident #4 was observed to be on 1:1 observation with staff on 9/8/2025 (date of survey entry) and the date of this review was 9/9/2025 – no documentation identified for 9/9/2025.
The activities/participation (Question 2) documenting for each of the 4 dates that talking was the only activity used out of several listed which included arts and crafts, board games, exercise, games, gardening, meditation/relaxation, music, and others.
A progress note dated 8/15/2025 noted “Resident attacked PCA (patient care assistant) assigned to 1:1 with him. Resident was informed not to exit building and punched staff in chest. Staff member restrained resident to ensure safety and resident then head-butted him. PCA removed from 1:1, new 1:1 placed with resident.”
A psychiatric progress note date 8/18/2025 documented “The patient is seen today at the request of the staff after a report of the patient hitting a staff member. Staff reports that the patient was informed not to exit building, and he responded aggressively and hit staff. The patient was temporarily restrained by holding his hands/arms in order to prevent him from further hitting the staff and once he was calm, his 1:1 CNA was changed out.”
A progress note dated 9/4/2025 at 5:40am documented “Resident was observed waking from sleep and immediately began pacing rapidly up and down the halls. Assigned CNA followed for supervision. Resident began attempting to exit through the doors and became agitated. Resident [#4] went out the facility along with 3 other staff members. The other nurse on shift attempted to support the resident to prevent him from falling. During the intervention, the resident forcefully moved his head forward and made contact with nurse. Resident then attempted to leave the premises and fell into the bushes hitting his head. Resident was noted with abrasions to his left forehead and left knee. Due to continued attempts to leave the facility and inability of staff to maintain control, law enforcement was contacted. Resident [#4] was redirected back into the facility prior to their arrival. Police arrived shortly thereafter. Resident[#4] continues to be combative and agitated.”
Resident #11
On September 8, 2025 at 3:15 PM, Resident #11 shared that he has difficulty communicating. His roommate offered that he has asked the staff to get Resident #11 a communication board several times, but they have not. Resident #11 confirmed that he has never received one. When asked how it would assist, he stated that because of his communication difficulties, it would help him to let the staff know what he needs. No communication board was seen in the resident's room.
On September 9, 2025 at 10:25 AM, a review of the care plan for Resident #11 (last reviewed 6/23/25) shows a focus area of the resident being dependent on staff for meeting emotional, intellectual, physical, and social needs. The goal of the resident was maintaining involvement in cognitive stimulation and social activities as desired. Interventions included, All staff to converse with resident while providing care; Assist with arranging community activities; Arrange transportation; Ensure that the activities the resident is attending are: Compatible with physical and mental capabilities; Compatible with known interests and preferences; Adapted as needed (such as large print, holders if resident lacks hand strength, task segmentation), Compatible with individual needs and abilities; and age appropriate; Invite the resident to scheduled activities; providing a Community Life calendar; notifying resident of any changes to the calendar of activities; thanking resident for attendance at Community Life functions; assisting/escorting to Community Life functions; providing bedside/in-room visits and activities if unable to attend out of room events. Also included in interventions in a note stating Resident #11 has a communication board but can communicate without it if given time. Another focus area is communication problems related to aphasia. One of the interventions is to evaluate the resident for dexterity/ability to use communication board, writing, use of computer, or use of sign language as alternate communication to speech. Also included is to refer to speech therapy for evaluation and treatment as ordered. The date of initiation is 01/21/2022.
On September 9, 2025 at 12:10 PM, a review of the resident's orders since admission reveal no order for speech, occupational therapy, physical therapy, or evaluation.
On 9/9/25 at 12:18 PM, the MDS Coordinator was asked for evidence of referral to speech therapy as documented in the care plan. The MDS Coordinator was unable to locate the referral. She called the Therapy Director for the facility's contracted speech therapy, and the director was unable to locate a referral or any visit notes. The MDS Coordinator was asked if the referral or communication board was followed up on, and she stated that it doesn't look like it was.