CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide adequate supervision, a secure environment an...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide adequate supervision, a secure environment and failed to respond appropriately to door alarms to prevent a vulnerable, physically and cognitively impaired resident from exiting the facility unsupervised for 1 of 8 residents reviewed for risk of elopement (#1). This failure contributed to the elopement of resident #1 and placed him at risk for serious injury/impairment/death. While resident #1 was out of the facility unsupervised, he sustained a fall with minor injuries. There was likelihood he could have been hit by a car, become lost, or sustained more severe injuries from the fall.
On [DATE] at approximately 1:40 PM, resident #1 left his room in his wheelchair, proceeded to the end of the hallway and pushed the fire egress door for 30 seconds until it opened and he exited the building, unsupervised. The door alarm sounded at the nurse's station but staff failed to respond appropriately to determine if the door had been opened and if a resident had exited. Resident #1 wheeled himself out the door to the landing and down a 20-foot ramp onto the sidewalk below. The resident's wheelchair went over the curb of the sidewalk and he fell out of his wheelchair onto the road. A Good Samaritan stopped his car, assisted the resident into his wheelchair and brought the resident to the facility. The facility was unaware the resident had exited the facility and had fallen on the road until the Good Samaritan advised the weekend Nursing Supervisor and the Activities Director the resident fell off the sidewalk. The resident sustained abrasions to his left forearm. While resident #1 was out of the facility, he could have been hit by a car and sustained major injuries or died.
The facility's failure to provide adequate supervision, secure environment and failure to respond appropriately to door alarms contributed to resident #1's elopement and placed all residents who wandered at risk for serious injury/impairment/death. This failure resulted in Immediate Jeopardy, that began on [DATE] and was removed on [DATE].
Findings:
Review of the medical record revealed resident #1 was admitted to the facility on [DATE] from an acute care hospital with diagnoses of Parkinson's disease, spinal stenosis, cognitive communication deficit, cognitive impairment, history of falls, and need for continuous supervision.
The Florida Agency for Health Care Administration 5000-3008 Medical Certification for Medicaid Long Term Care Services and Patient Transfer Form dated [DATE], revealed resident #1 was a fall risk, used a walker, could self-transfer and ambulated with assistance.
The Minimum Data Set (MDS) quarterly assessment with assessment reference date [DATE] showed resident #1 had moderately impaired cognition, had no behaviors to himself or others and did not wander during the lookback period. The assessment showed he required extensive assistance with bed mobility, transfers and locomotion and used a wheelchair and walker for mobility. The assessment indicated resident #1 had two or more falls with no injury since admission or the prior assessment and received anti-anxiety and anti-depressant medications during the 7-day lookback period. The assessment noted resident #1 did not have any alarms placed, including for wandering.
Resident #1's care plan for risk of injury from falls related to poor safety awareness, history of falls, psychotropic drug use noted he fell five times in the past 5 months, on [DATE], [DATE], [DATE], [DATE] and [DATE]. The interventions directed staff to keep the resident in the common area, and encourage the resident to use his hands to propel his wheelchair instead of using his feet.
There were no care plans or interventions for elopement risk, or to address his cognition deficits before his elopement on [DATE].
Review of the medical record revealed a physician's order dated [DATE] that indicated resident #1 could take leave from the facility only with a responsible party. The medical record revealed additional orders for multiple medications required to treat resident #1's Parkinson's disease, Carbidopa/Levodopa 25-100 milligrams (mg) ordered four times a day, Rivastigmine Tartrate 6 mg twice a day and Carbidopa/Levodopa extended release 25-100 mg at bedtime.
Review of a physician progress note dated [DATE] revealed resident #1 was alert and oriented to self. A physician progress note dated [DATE], noted resident #1 was assessed as alert, with increased confusion and acute disorganized behavior with a plan to monitor due to recent infection. The note documented a fall 3 weeks prior. Review of another physician progress note dated [DATE], showed resident #1 was again assessed as alert only, with a history of falls.
Review of the admission Accident Risk Evaluation dated [DATE] indicated the resident had difficulty maintaining standing position, impaired balance during transitions and gait problems. Review of the Exit Seeking Evaluation portion of the document revealed that resident #1 was not ambulatory and was unable to walk alone without assistive device. The nurse incorrectly documented resident #1 was unable to use a wheelchair independently, had no diagnosis of cognitive impairment, nor could he be mobile via wheelchair without the assistance of someone else. Finally, the documentation that resident #1 was unable to physically leave the facility without assistance was incorrect on the evaluation. The Action/Interventions portion of the evaluation showed an electronic wander device was determined not to be placed because the resident was not an elopement risk.
Review of the Accident Risk Evaluation dated [DATE] revealed a quarterly evaluation for accident risk. The falls risk portion of the document indicated resident #1 had three or more falls with minor injury since the last assessment. The evaluation incorrectly documented resident #1 was unable to use a wheelchair independently but noted he was mobile with the wheelchair without assistance. The evaluation also incorrectly documented resident #1 as having no diagnosis of cognitive impairment and that he was unable to physically leave the facility unassisted.
Review of a psychiatric consult progress noted dated [DATE] revealed resident #1 was alert and oriented to person and place. The assessment showed he was deficient in long term memory and mildly deficient in short term memory. Resident #1's fund of knowledge and insight was assessed as fair, and his judgement was assessed as diminished.
Review of the Occupational Therapy (OT) Discharge summary dated [DATE] showed resident #1 was on therapy caseload to improve his posture and stability in his wheelchair among other tasks. The document indicated he attained his wheelchair mobility goals on [DATE] and required supervision for safety and technique cues.
On [DATE] at 4:43 PM, Physical Therapy Assistant (PTA) G stated resident #1 had been on therapy caseload several times due to multiple falls and diagnosis of Parkinson's disease. PTA G explained the resident was fully able to ambulate with his wheelchair independently throughout the facility using his feet and arms to propel. PTA G recalled resident #1 often tried to show he was able to do things on his own and at various times indicated he wanted to go home. He stated the resident had poor judgement of his abilities and would often do things he knew he shouldn't do, whether they were risky or not. PTA G said the resident had mental fatigue and mental fog and would not be safe on his own outside the facility.
Review of a progress note by Licensed Practical Nurse (LPN) A dated [DATE] at 6:09 PM showed resident #1 went outside unnoticed and unsupervised through the 200-hallway door. LPN A indicated neither she nor other staff heard the alarm sound when he exited the building. She documented the resident fell while he was outside and sustained an abrasion to the left forearm. She noted the physician, and the resident's wife were notified.
In interviews in person and by telephone on [DATE] at 12:35 PM and on [DATE] at 11:15 AM, resident #1's wife stated she visited her husband at the facility almost daily. She recalled she had visited her husband just before lunch on Sunday [DATE] and left at about 1:30 PM, after lunch. She remembered he was more confused and not as fresh that day when she visited. She explained he had not taken his afternoon medications before she left the facility that day and explained his mentation usually improved about an hour after taking his medications. She said she saw resident #1's assigned LPN A at the 200-unit nurse's station on her way to his room and encountered Certified Nursing Assistant (CNA) B in the hall near his room. Resident #1's wife recalled CNA B was going to assist her husband to use the restroom and she left him in her care. Resident #1's wife stated she told LPN A as she again passed by the 200-hall nurse's station that she brought her boyfriend back to his room. Resident #1's wife then recalled it was not long after she had left the facility, that she received a telephone call from the weekend supervisor that her husband had exited the facility.
On [DATE] at 10:01 AM, the weekend Nursing Supervisor stated he was working on Sunday [DATE] and had come out of a room on the 100 unit when he heard a faint alarm sound. He recalled he went to the door alarm panel at the nurse's station to see which door was activated. He showed the panel at the 100-unit nurse's station which indicated through a row of lights when one of the door alarms was activated. He said he saw it was the 200-unit west emergency exit door that was lit and headed towards the door. He recalled he observed resident #2, a known elopement risk resident who had a wander alarm device on her wheelchair near the door. He remembered there were no other staff in the area at that time and he assumed resident #2 had activated the door alarm with her wander device. He said he took the resident back to her room and spent a few minutes speaking to her. He indicated he then returned to the exit door to turn the alarm off. He stated he attempted to turn off the alarm using the code on the keypad, but it didn't work, so he pushed the door open and looked outside briefly but did did not go outside to check for any resident that may have exited. The Nursing Supervisor explained he then closed the door, but the alarm continued to sound. He repeated opening and closing the door, again without success then made his way to the 200-unit nurse's station door panel. He said he heard an overhead page requesting him to come to the front desk as he turned off the alarm. He recalled he saw resident #1 in his wheelchair with a stranger when he arrived at the front desk and thought the man was possibly a relative. He stated he was surprised and had no idea resident #1 had left the facility unsupervised when he was told the man found resident #1 outside the facility. The weekend Nursing Supervisor stated the man, a Good Samaritan told him and the Activity Director he stopped his car to help resident #1 after he had fallen on the road. He said they walked outside and around the corner of the building to where the Good Samaritan's vehicle was parked on the street near the facility. He explained the Good Samaritan said he and two other drivers stopped their vehicles in the middle of the street when they witnessed resident #1 on the road. He said he did not get the Good Samaritan's name or his telephone number and the other people who had stopped their cars were no longer present. He acknowledged facility staff were unaware the resident had exited the building until the Good Samaritan brought the resident back. The weekend Nursing Supervisor said, If he didn't fall down, I don't know how far he would've gone.
On [DATE] at approximately 10:20 AM, the weekend Nursing Supervisor stated he knew resident #1 from a previous facility he worked at, and he had progressively declined through the years. He noted resident #1 did not have good judgement and had a history of frequent falls. He said after resident #1 was returned to his room, he assessed him and found abrasions to his left forearm.
In a telephone interview on [DATE] at 4:11 PM, the Activities Director stated she was filling in for the receptionist on [DATE]. She stated resident #1's wife had left a short time earlier when the Good Samaritan wheeled resident #1 into the facility through the front door. She said she wondered how the resident got outside because she didn't remember him going out through the front door. She said the Good Samaritan told her he was driving down the street when he and other drivers saw resident #1 go off the curb and stopped to assist. The Activities Director stated resident #1 then said, I fell. She stated she paged for the weekend Nursing Supervisor to come to the front desk and when he arrived, resident #1 again stated he fell and that he left through the back door. She recalled she did not get the Good Samaritan's name, nor his contact information.
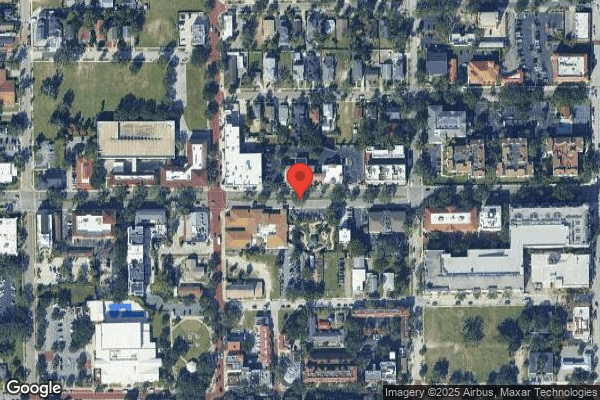
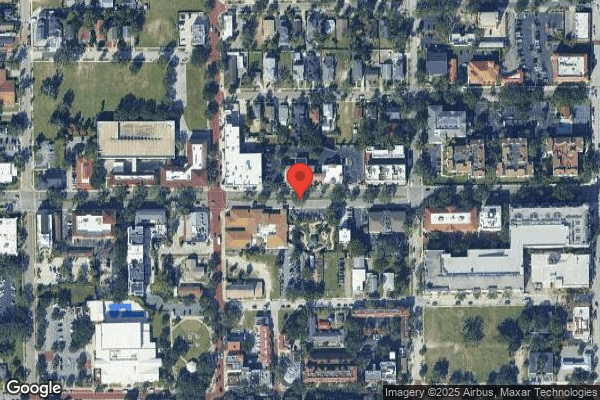
On [DATE] at 10:35 AM, resident #1's probable elopement route was retraced. Resident #1 wheeled himself approximately 75 feet from his room to the 200-unit west emergency exit door. He pushed on the door for approximately 30 seconds and the door opened. From there he exited the recessed doorway on to the landing platform and rolled down a sloped ramp approximately 20 feet to the sidewalk below. From the end of the ramp to the cobblestone street measured approximately 13 feet to the raised curb. The sidewalk had numerous decorative contraction joints which posed a hazard for walking or for wheelchairs. The facility was located on the corner of two moderately trafficked streets with a busy restaurant across the street. It is unknown exactly how far resident #1 traveled before he fell out of his wheelchair onto the road and the Good Samaritan stopped his car to assist and return him to the facility. From inside the doorway of the exit, the view out to the street was mostly obstructed, that indicated the Nursing Supervisor would not have been able to see the resident unless he came out to the landing.
In a telephone interview on [DATE] at 5:44 PM, CNA B stated she cared for resident #1 on the day he eloped, [DATE]. She said he had memory problems, was head strong and described resident #1 as often trying to do things he shouldn't do. She recalled she spoke to the resident's wife before she left that day, and then took resident #1 to the restroom. She noted she left resident #1 at his door in his wheelchair then went to the room across the hall to provide care for another resident. CNA B said she did not hear the door alarm in the room and was surprised to learn the resident had exited through the fire door.
On [DATE] at 10:05 AM, CNA F said she usually worked on the 200-unit where resident #1's room was located and knew the resident well. She noted resident #1 could wheel himself around the facility independently but explained resident #1 had intermittent confusion which was often worse when his wife left after visits. She stated she was on her lunch break when resident #1 left the facility and did not hear any door alarm. She was told about the resident's elopement when she returned from break.
On [DATE] at 10:22 AM, CNA E stated she was assigned to work on the 200-unit on [DATE]. She stated after lunch, she went between the dining room, activity room and the unit assisting residents to return to their rooms or go to activities. CNA E stated she did not hear the door alarm when it sounded but later observed the weekend Nursing Supervisor at the back door pushing the door back and forth in an attempt to turn the alarm off. She stated she did not speak with the weekend Nursing Supervisor at that time to determine if a resident had eloped and instead returned to her duties in a resident's room. She stated later everyone was shocked when they learned resident #1 had left the facility unsupervised.
On [DATE] at 10:39 AM, CNA D stated she often cared for resident #1 when he previously resided on the 100 unit. She stated he could wheel himself around the facility in his wheelchair independently and noted he was more confused and upset after his wife left from visits. She said she was on lunch break when resident #1 left the facility unsupervised and did not hear the alarm.
In a telephone interview on [DATE] at 2:55 PM, LPN A stated resident #1 was on her assignment on [DATE]. She recalled she was at the desk at the 200-unit nurse's station around 1:30 PM or 1:40 PM when resident #1's wife told her she was leaving. She explained she went for lunch shortly after in the break room. She indicated she did not hear the alarm from the break room but received a call from the weekend Nursing Supervisor later that resident #1 had exited but was now back in the facility. LPN A stated she assessed resident #1 and he had an abrasion to his arm, but he denied any pain. She stated resident #1 had never done anything like this before, but he was a bit confused especially since his wife had just left him to go home. She noted he was a high fall risk and did not have good judgement about what he could and couldn't do so the staff tried to check on him frequently.
On [DATE] at 11:49 AM, the Maintenance Director reported he checked the exit doors weekly on Fridays before resident #1's elopement. He stated the door check on Friday, [DATE] did not show any variances and all the doors and alarms were in working order. He stated he was notified of the elopement on the afternoon of [DATE] and came to work afterwards to inspect the doors and alarms. He found the 200-unit west door which was opened by resident #1 in proper working order. He explained resident #1 did not have an electronic wander alarm device at that time, so only the emergency exit door alarm sounded when he pushed on the door, and after 30 seconds it opened as it was supposed to. The Maintenance Director demonstrated the function of the 200-unit west emergency exit door. He stated it had an electronic wander device alarm installed and a magnetic lock. He explained there was no screamer type alarm installed at the time of resident #1's elopement, so the only alarm that sounded was a low buzzing that sounded at the 100-unit nurse's station approximately 100 feet away from the door.
On [DATE] at 1:26 PM, resident #1 recalled the day he left the facility and said his wheelchair tipped over because the ramp was, too fast. He said he remembered he saw the cobblestones of the road and that two men picked him up. Resident #1 then remembered he heard a lady say she thought he belonged to the facility and one of the men helped him back to the facility. He explained he wasn't trying to leave the facility, but was going down the sidewalk to the game.
On [DATE] at 11:45 AM, resident #1's elopement was reviewed with the Social Service Director (SSD), the Director of Nursing (DON) and the Administrator. The Administrator confirmed the weekend Nursing Supervisor telephoned the DON on [DATE] sometime before 2:00 PM to inform her resident #1 had eloped from the building and was brought back by a Good Samaritan. The DON verified she called to notify the Administrator and the SSD and they all came to the facility immediately. The SSD provided statements they collected from staff that worked that day. The SSD read the statements collected from LPN A, CNA B and the Activities Director. The DON stated the weekend Nursing Supervisor told them he was in a room helping a resident, when he came out and heard a faint alarm and went to the board at the nurse's station to see which door alarmed. They said he went to the door, pushed on it and opened it and stuck his head out to see if anyone was there. She continued that he stated he was called to come to the front lobby and was then told the Good Samaritan had helped resident #1 back into the building. The facility was asked to provide the statement from the weekend Nursing Supervisor and they stated they could not find it. The SSD stated she interviewed resident #1 on the evening of [DATE] and assessed his cognition as intact. She said the resident told her he was going to a scrimmage game across from the facility, across the grassy fields. She indicted resident #1 told her he did not fall and that a man who was a friend of his helped him down the ramp and brought him back inside. She stated he could not recall who the friend was but said he had, seen him around the neighborhood. She stated resident #1 told her he hurt his arm because of the door. The SSD did not reply to how resident #1's cognition could be assessed as intact when he thought he was going to a scrimmage at a field across from the facility when the facility was in the downtown part of the city with no field nearby. The DON confirmed the elopement risk evaluation performed on [DATE] was inaccurate. She acknowledged the elopement evaluation dated [DATE], after resident #1's elopement had different answers to the questions of the resident's physical ability than how they were answered on the previous quarterly assessment. She acknowledged resident #1's physical ability nor his cognition had changed since the previous assessment, but the facility decided to apply an electronic wander device to resident #1 now. The Administrator stated the investigation found the root cause of the incident was the resident had a change in his mentation as he was not an elopement risk previously. She said they felt if he had an electronic wander device, the door would have locked, and he would not have been able to exit the facility. The DON stated now they realized resident #1's mentation comes and goes and he had poor safety awareness before the incident that had not changed. The DON stated her expectation was for staff to stop what they were doing if they heard an alarm, find which door was breached and walk out of the door to survey the area in order to determine if any resident got out. She clarified staff must walk around outside and determine if a resident exited the building and not just stand in the doorway and peep outside. The SSD stated they had determined in their investigation that resident #1 did not fall when he eloped based on the minor injuries he sustained and his statement later that day. The SSD, DON and Administrator did not provide an answer when informed that several staff interviewed and documented the Good Samaritan who found resident #1 said that he was found on the road and he and other Good Samaritans helped him into his wheelchair and back to the facility. They stated since the resident had only minor injuries, they decided he must not have fallen, and they disregarded the statements from the Good Samaritan who said he witnessed him on the ground and helped him up off the street. The Administrator acknowledged that while the resident was outside the building, unsupervised he was at risk of being hit by a car and may have sustained major injuries from his fall including death.
In a telephone interview on [DATE] at 12:08 PM, the Medical Director stated she was resident #1's attending physician and was at the facility a few times a week. She said she was surprised and concerned for resident #1's welfare when she was alerted by phone the day the resident eloped from the facility. The Medical Director explained the resident was usually confused although he could communicate. She elaborated resident #1 was not alert and oriented to place and time. She confirmed resident #1 was at risk for injuries from falls, getting hit by cars or getting lost when he was outside the facility unsupervised. The Medical Director acknowledged door and electronic wander alarms were not a substitute for adequate supervision, only a backup. She acknowledged staff needed to act appropriately to respond to alarms and to look outside for residents if an alarm sounded.
Review of the Facility Assessment dated [DATE], revealed common diagnoses of residents which may be present on admission or may develop included impaired cognition and Parkinson's disease. The assessment documented services and care that was offered included, Identifying hazards and risks for residents, by getting to know the resident, incorporating this information into the care planning process and making sure the staff caring for the resident had this information.
Review of the undated Policy/Procedure- Elopement revealed the intent of the facility to be aware of the resident's usual habits and locations as reasonably practicable to identify possible elopement. The definition of elopement was given as a, Situation in which a resident leaves the premises or a safe area without the facility's knowledge and supervision . The document noted the situation represented a risk to the resident's health and safety and placed them at risk of environmental exposure, dehydration, other medical complication, drowning or being struck by a motor vehicle.
Review of the Policy/Procedure, The Gardens at [NAME] Wandering and Elopements dated 08/22, revealed the facility did not have a secure unit and did not admit residents with high risk wandering or elopement behaviors, however, if a resident declined and developed these behaviors staff would identify those at risk and strive to prevent harm while maintaining the least restrictive environment. The policy described if residents were identified as at risk for wandering, elopement or other safety issues, the resident's care plan would include strategies and interventions to maintain the resident's safety.
Review of immediate actions implemented by the facility to remove the Immediate Jeopardy revealed the following, which were verified by the survey team:
*On [DATE], a facility resident head count was completed and confirmed.
*On [DATE], an Accident/Elopement Evaluation was done on resident #1. An electronic wander device was placed on resident #1, and he was started on 1 to 1 supervision for safety until doors/alarms could be professionally inspected/addressed. Resident #1's care plan was revised as indicated.
*On [DATE], a head-to-toe assessment and neurological check was initiated on resident #1. The resident sustained a left forearm abrasion, which was treated. Resident #1 reported no pain, and his baseline range of motion was intact.
*On [DATE], all residents were re-evaluated and verified by DON for Accident/Elopement Risk Evaluations. The MDS Coordinator was re-educated by the DON for assessment procedure.
*On [DATE], the DON initiated mandatory online and in person education for all staff on elopement and response to alarms with a 68.6% (46 of 67) staff trained. Agency Staff to be first educated through the Agency in service book and new hires to be educated during orientation. Maintenance Supervisor to walk all new staff around the facility during the Life Safety training and Agency staff to be oriented by the Supervisor, DON or Assistant DON.
* On [DATE], all staff present, and working were re-educated in person, in writing, electronically and with demonstration by managers on response to alarms, types of alarms, and exit doors (27 staff per attendance sheet). This education to continue in orientation, with new agency staff, and through drills.
*On [DATE], all doors were immediately checked for proper function by the Maintenance Supervisor.
*On [DATE], the Medical Director, on call physician, and wife of resident #1 were notified. The non-profit Board Chairman was notified by Administrator of the event.
* On [DATE], a risk/incident report was completed on resident #1. The RN Supervisor, Social Service Director and Assistant DON began collecting staff statements. Social Services Director filed the AHCA 1-day immediate report and notified the Department of Children and Families.
*On [DATE], all managers were notified to attend a mandatory emergency Ad Hoc Quality Assurance Performance Improvement (QAPI) meeting at the facility. The Elopement Policy and Procedure was reviewed.
*On [DATE], the Maintenance Director installed a screamer alarm at the 200 Hall exit from which the resident eloped. The Maintenance Director ordered additional Stop Sign screamer alarms to install on other exits with spares on hand. The Maintenance Director contacted door and alarm vendors on an emergency call for a stat appointment to assess all doors, alarms and equipment related to exits. Maintenance researching end gates that will open only in rather than out (with magnetic locks) as appropriate to fire and life safety codes.
* On [DATE], the Elopement Books were checked for accuracy, and resident #1 was added.
*On [DATE], the Board was contacted for financial authorization to add alarms and vendors to check doors/alarms.
*On [DATE], the elopement was reviewed and discussed in clinical morning meeting to review any additional items that needed to be addressed and additional education needed to be performed.
*On [DATE], elopement drill and in-service education were performed and to continue toward 100% compliance.
*On [DATE], 1 to 1 monitoring of resident until doors were verified functioning.
*On [DATE] the elopement was again reviewed and discussed in clinical morning meeting to review additional items that needed to be addressed and education that needed to be performed.
* On [DATE] a Behavior Management meeting was held, and no changes were made to resident #1's medications.
* On [DATE] a QAPI meeting was held with all managers and the Medical Director to discuss the elopement and the steps taken to mitigate the recurrence and any negative outcomes going forward. A written action plan was begun by Risk Manager regarding F689.
*On [DATE] elopement drill and in-service education were performed to continue toward 100% compliance (17 staff participated per attendance sheet).
*On [DATE] the elopement was again reviewed and discussed in clinical morning meeting to review items that still needed to be addressed and education that needed to be performed.
*On [DATE] an All staff meeting was held. The elopement event was reviewed, education continued, and an elopement drill with demonstration was performed by the Maintenance Supervisor.
Review of in-service and drill attendance sheets and reconciliation with staff roster validated education was completed according to facility's plan.
From [DATE] to [DATE], interviews conducted with 20 staff representing both day and evening shifts including 6 nurses, 7 CNAs, 4 dietary staff, 3 housekeeping staff, 2 therapy staff, and the receptionist revealed staff participated in elopement drills, and were knowledgeable of the facility's elopement standards and guidelines. Staff verbalized the importance of responding to door alarms by going outside and looking all around for possible eloped residents. Nursing staff was knowledgeable of the importance of correctly performing risk assessments and the need to re-assess if there is a change in mentation or physical condition.
The sample was expanded to include 7 additional residents at risk for elopement and wandering. Observations, interviews and record reviews revealed residents #2, #3, #4, #5, #6, #7 and #8 had elopement risk assessments, appropriate care plans and demographic information placed in the elopement binder on each unit and front desk.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0563
(Tag F0563)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, and interview, the facility failed to provide visitors immediate access to residents in the facility for 2...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, and interview, the facility failed to provide visitors immediate access to residents in the facility for 2 of 2 residents, 2 family members and State Survey Agency, (#1, #9).
Findings:
On Sunday, 11/20/22 at 8:55 AM, surveyors attempted to enter the facility through the front door but the doors were locked and there were no staff visible in the lobby. The doorbell was rung but no staff responded. A sign posted near the door directed visitors to ring the bell at the garden gate entrance if staff did not respond at the front door. At 9:02 AM, the facility phone number was called and the phone rang for 4 minutes with no response. Another phone call was made at 9:06 AM with no response and no voice mail. The garden gate entrance bell was pressed several times with no response. A phone call was placed to the facility again at 9:10 AM and the phone rang for 3 minutes with no answer. The back of the facility was accessed through a church parking lot and dietary staff were observed through one of the windows in the kitchen. Surveyors knocked on a service door and at 9:17 AM, a dietary staff member opened the service door. The dietary staff member stated she was not allowed to let anyone into the kitchen but would get someone to let the surveyors in through the facility back door. At approximately 9:22 AM, Registered Nurse (RN) C came to the back door of the facility. She indicated she was in charge and the Weekend Supervisor would be in later.
On 11/20/22 at 10:01 AM, the Weekend Supervisor stated the receptionist started work late on the weekends. He explained the garden gate bell rang at the nurse's station but staff were busy in resident rooms this morning providing care. He indicated visitors could call on the phone if no one answered the gate but did not say what visitors should do if the telephone was unanswered.
On 11/20/22 at 12:35 PM, resident #1's wife reported she had to use the garden gate bell after hours but added the bell only worked half the time. She explained, if you can get the nurse to answer it. She stated a nurse would either buzz her in or come out with a key fob to open the gate. Resident #1's wife stated the nurses have said they were too busy to answer the bell. She explained she had spoken to other residents' family members who had the same issue of not being able to enter the facility if no one was at the front desk to let them in. She explained if she wanted to come at 7:00 AM to see her husband, she would have to call and wait for the nurse to answer which sometimes took half hour to an hour. Resident #1's wife recalled she attempted to reach the facility and the telephone rang 20 times before she hung up and called again. She stated she could not visit anytime she wanted because of the difficulty of getting in the building. She added she was afraid to stand out in the dark waiting for someone to let her inside.
On 11/21/22 at 3:24 PM and on 11/22/22 at 10:50 AM, two family members were interviewed regarding visitation. Both family member #1 and family member #2 confirmed it was difficult to enter the facility when no one was at the front desk. Both stated they sometimes had to telephone when they were outside to get someone to let them in. Family member #1 stated she used to visit whenever she wanted, but now she does not feel like she can visit after hours. She explained it was inconvenient not knowing if the bell would work or if staff were available to answer the door. Family member #1 said she felt the facility did not want visitors in the building other than particular hours. She stated, Family members should be able to come and go without all the hassle. Both family members requested their family member in the facility not be identified.
On 11/21/22 at 11:55 AM, the Administrator verified the nurses were to answer the bell from the garden gate to allow visitors inside. She said the facility was struck by lightning 7/19/22 which affected the facility's door bell system. The Administrator acknowledged the facility had not made any changes to accommodate for the malfunctioning doorbell at the garden gate.
On 11/22/22 at 2:07 PM, the Social Services Director (SSD) confirmed she received a grievance regarding the doorbell not working. She stated the wife of resident #9 complained the doorbell was not working when her husband was admitted on [DATE]. She reported it was raining heavily outside when the resident arrived and it took 30-45 minutes before someone let the wife inside. The SSD stated the investigation showed the doorbell was not working due to being hit by lightning. The SSD explained the wife chose to discharge her husband on 9/17/22 and there was no further contact with her. She recalled the facility was waiting for the insurance company to approve repairs to the system and thought the system was fixed.
On 11/22/22 at 3:49 PM, the Maintenance Director explained the garden gate doorbell had a camera to view the visitor and when pressed, it rang at the reception desk, nurse station and activities room. The Maintenance Director recalled the doorbell started malfunctioning in July 2022 after the facility was struck by lightning. He stated he rebooted the system and the system would work for a few days and then stop again. He stated the vendor serviced the doorbell which worked and then stopped working. The Maintenance Director reported the system was currently working intermittently and acknowledged the key pad was finicky. At 4:00 PM, the Maintenance Director went outside and demonstrated the operation of the garden gate bell by pushing on the top left corner of the pad. He explained the user had to press gently on the pad but not in the center. He clarified the sensors in the middle of the pad were probably worn out and did not work. The pad had no indication of where to press in order to activate the bell. When the outside pad was pushed, the receiving panel was activated at the 100-hall nurse station. The panel was noted to have 3 positions and the volume was in the lowest position and was not audible half way down the hallway.
Review of the Facility assessment dated [DATE], revealed the facility would maintain the building, grounds and physical equipment utilizing a scheduled preventative maintenance program and capital expenditure process to ensure they were maintained to protect and promote the health and safety of the residents.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure Minimum Data Set (MDS) assessments were accurate related to ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure Minimum Data Set (MDS) assessments were accurate related to wander/elopement alarms for 6 of 8 residents reviewed for elopement risk, (#2, #3, #4, #5, #6 and #7).
Findings:
1. Resident #2 was admitted to the facility on [DATE] with diagnoses including cognitive communication deficit, adjustment disorder with mixed anxiety and depressed mood.
Review of the Minimum Data Set (MDS) quarterly assessment with Assessment Reference Date (ARD) 10/10/22 revealed resident #2 had a Brief Interview for Mental Status (BIMS) score of 5 that indicated the resident was severely cognitively impaired. The assessment noted the resident did not use a wander or elopement alarm.
Review of resident #2's medical record revealed a physician order dated 10/07/22 for wander guard applied to left ankle.
2. Resident #3 was admitted to the facility on [DATE] with diagnoses including dementia, major depressive disorder, Alzheimer's disease, anxiety and cognitive communication deficit
Review of the MDS quarterly assessment with ARD 10/14/22 revealed resident #3 had long-term and short-term memory problems and severely impaired cognitive skills for daily decision making. The assessment indicated the resident did not use a wander or elopement alarm.
Review of resident #3's medical record revealed a current physician order dated 7/20/21 for wander guard to right ankle.
3. Resident #4 was admitted to the facility on [DATE] with diagnoses including unspecified psychosis, dementia, traumatic subdural hemorrhage, and traumatic brain injury.
Review of the MDS quarterly assessment with ARD 9/02/22 revealed resident #4 had a BIMS score of 5 indicating the resident was severely cognitively impaired. The assessment indicated the resident did not use a wander or elopement alarm.
Review of resident #4's medical record revealed a current physician order dated 11/25/20 for wander guard, placement on left ankle.
4. Resident #5 was admitted to the facility on [DATE] with diagnoses including unspecified dementia, unspecified psychosis, and major depressive disorder.
Review of the MDS annual assessment with ARD 10/24/22 revealed resident #5 had a BIMS score of 6 indicating the resident was severely cognitively impaired. The assessment indicated the resident did not use a wander or elopement alarm.
Review of resident #5's medical record revealed a physician order dated 6/16/22 for wander guard to back of wheelchair on left side.
5. Resident #6 was admitted to the facility on [DATE] with diagnoses including traumatic brain injury, traumatic brain hemorrhage, dementia and cognitive communication deficit.
Review of the MDS annual assessment with ARD 9/01/22 revealed resident #6 had a BIMS score of 7 indicating the resident was severely cognitively impaired. The assessment indicated the resident did not use a wander or elopement alarm.
Review of resident #6's medical record revealed a current physician order dated 1/27/21 for wander guard to right ankle
6. Resident #7 was admitted to the facility on [DATE] with diagnoses including Alzheimer's disease, unspecified dementia, major depressive disorder, hypertension and history of falling.
Review of the MDS quarterly assessment with ARD 8/12/22 revealed resident #7 had a BIMS score of 6 indicating resident was severely cognitively impaired. The assessment indicated the resident did not use a wander or elopement alarm.
Review of resident #7's medical record revealed a current physician order dated 11/05/21 for wander guard to right ankle.
On 11/22/22 at 10:12 AM, the MDS Coordinator reviewed Section P - Restraints and Alarms for resident #2's MDS quarterly assessment with ARD 10/10/22 and confirmed the assessment did not reflect the resident had a wander guard. She acknowledged an error was made and the assessment was inaccurate. She explained she had not considered the wander guard as an alarm and acknowledged residents' #3, #4, #5, #6 and #7 assessments were also inaccurate.
The Centers for Medicare and Medicaid Services (CMS) Long Term Care Resident Assessment Instrument (RAI) 3.0 Users Manual, Version 1.17.1, dated October 2019 defined a wander or elopement alarm as a device such as bracelets, pins/buttons worn on the resident's clothing, sensors in shoes, or building/unit exit sensors worn by/attached to the resident that activate an alarm and/or alert the staff when the resident nears or exits a specific area or the building. This includes devices that are attached to the resident's assistive device (e.g., walker, wheelchair, cane) or other belongings.