THE HAVEN OF BEMENT.




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
The Haven of Bement has received an F grade for its trust score, indicating significant concerns about the quality of care provided. Ranking #647 out of 665 facilities in Illinois places it in the bottom half of the state, and it is the second of only two facilities in Piatt County, suggesting limited options in the area. While the facility is improving-reducing issues from 33 in 2024 to only 1 in 2025-there are still major weaknesses, including a high staff turnover rate of 71%, which is concerning compared to the state average of 46%. There has been no record of fines, which is a positive sign, but RN coverage is only average, meaning there could be gaps in critical care. Specific incidents include a failure to report a resident's urinary tract infection in a timely manner, leading to hospitalization, and inadequate staffing of certified nursing assistants, resulting in delayed responses to residents' needs and missed scheduled showers. Overall, while there are signs of improvement, families should weigh these serious concerns carefully.
- Trust Score
- F
- In Illinois
- #647/665
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 71% turnover. Very high, 23 points above average. Constant new faces learning your loved one's needs.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Illinois facilities.
- Skilled Nurses ✓ Good
- Each resident gets 43 minutes of Registered Nurse (RN) attention daily — more than average for Illinois. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 47 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Illinois average (2.5)
Significant quality concerns identified by CMS
25pts above Illinois avg (46%)
Frequent staff changes - ask about care continuity
Part of a multi-facility chain
Ask about local staffing decisions and management
23 points above Illinois average of 48%
The Ugly 47 deficiencies on record
Sept 2025
1 deficiency
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to provide the services of a registered nurse for eight consecutive hours seven days per week. This failure has the potential to affect all 39...
Read full inspector narrative →
Dec 2024
15 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Incontinence Care
(Tag F0690)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to monitor urine characteristics, timely report changes in urine and ur...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3.) On 12/09/24 at 9:52 AM R8 was in R8's room and had approximately 1/4 inch long facial hair to chin and upper lip. On 12/9/24...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to perform a mechanical lift transfer safely for one (R8)...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to replace an oxygen mask weekly, failed to store respiratory equipment in a manner to prevent cross contamination, failed to fol...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to ensure medications were available and administered as ordered resulting in significant medication errors for two (R8, R18) of 10 residents r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to offer pneumococcal vaccinations and maintain vaccination documentati...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected multiple residents
Based on interview and record review the facility failed to document and follow up on grievances for five (R4, R14, R18, R22, R31) of five residents reviewed for grievances in the sample list of 30.
...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to serve pureed diets as planned on the menu. This failure affects three residents (R2, R7, R13) of four reviewed for pureed die...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to sufficiently staff certified nursing assistants (CNAs)...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review the facility failed to staff a full time Director of Nursing (DON). This failure has the potential to affect all 32 residents in the facility.
Findi...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0729
(Tag F0729)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to document registry verifications of nurse aide competency for five newly hired nurse aides prior to beginning employment in the facility. Th...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to employ a clinically qualified Director of Food and Nutrition Services. This failure has the potential to affect all 32 reside...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to maintain sanitary food storage areas. This failure has the potential to affect all 32 residents residing in the facility.
Fin...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on interview and record review the facility failed to implement surveillance monitoring of resident infections and implement corrective measures, and failed to develop a water management plan th...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected most or all residents
Based on interview and record review the facility failed to implement its antibiotic stewardship policy by failing to evaluate clinical data to ensure infection criteria and appropriate use of antibio...
Read full inspector narrative →
Nov 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to report an allegation of misappropriation of medication for one resident (R1) of three residents reviewed for medications in the sample list...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to investigate a report of misappropriation of resident medication for one resident (R1) of three residents reviewed for medications in the sa...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to administer seizure medications to a resident with a seizure disorder requiring scheduled therapeutic medication monitoring. This failure af...
Read full inspector narrative →
Sept 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to notify the physician of a resident's physical change of condition. T...
Read full inspector narrative →
Mar 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on record review and interview the facility failed to provide a written Notice of Medicare Non-Coverage notice, (NOMNC) for two (R4 and R5) of three residents reviewed for Medicare Non-Coverage ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0825
(Tag F0825)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review the facility failed to ensure therapy services were provided for five (R1, R2, R3, R4 and R5) of five residents reviewed for therapy services from a s...
Read full inspector narrative →
Jan 2024
12 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to follow Physician orders to obtain daily weights for two residents wi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide Passive Range of Motion (PROM) to one resident (R28) admitted with contractures of one resident reviewed for Restorative Nursing in...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to properly manage a tracheostomy tube for one (R22) of on...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0712
(Tag F0712)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to provide required physician's visits for one resident (R28) of one re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to administer medications as ordered to keep the medication error rate below five percent (5%). There were two medication errors ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to prevent a significant medication error for one resident (R28) of seven residents reviewed for medication in a sample list of 24.
Findings i...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to ensure the dignity of five (R11, R5, R6, R12, R17 and R...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected multiple residents
Based on interview and record review the facility failed to document the organisms being treated prior to initiating and/or continuing antibiotic therapy for four of four residents (R26, R85, R86, R29...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to use the services of an RN eight consecutive hours Seven days a week ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the facility failed to ensure proper food storage and labeling to prevent potential food spoilage and resident illness. This failure has the potentia...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0882
(Tag F0882)
Could have caused harm · This affected most or all residents
Based on interview and record review the facility failed to have an Infection Preventionist working at the facility and overseeing the infection control program This failure has the potential to affec...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0577
(Tag F0577)
Minor procedural issue · This affected most or all residents
Based on observation, interview, and record review the facility failed to post the most up to date survey inspection results for residents and families review. This failure has the potential to affect...
Read full inspector narrative →
Mar 2023
13 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to maintain a resident's (R23) dignity by failing to provide timely ass...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. R35's Nurse's Notes dated 2/26/23 document R35 was discharged from the facility to (hospital) due to behavioral issues, suici...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to provide oral care multiple times for one (R6) resident ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to follow Speech Therapy recommendations and Physician or...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on Observation, Interview and Record Review the facility failed to maintain safe power supply of medical equipment by plug...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to clarify physician orders, and failed to administer a physician ordered amount of water flushes, for a resident receiving hydration by a gas...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to change Oxygen tubing and Nebulizer tubing and failed to...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to administer medications per physician order and facility...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to obtain consent for a psychotropic medication for two (R...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to provide the services of a Registered Nurse to serve as a full time Director of Nursing, and failed to provide the services of...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to employ a qualified Director of Food and Nutrition Services. This failure has the potential to affect all 37 residents residin...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to prevent the potential for cross-contamination and forborne illness by failing to maintain sanitary food preparation and food ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0868
(Tag F0868)
Could have caused harm · This affected most or all residents
Based on record review and interview, the facility failed to maintain their Quality Assessment and Assurance Committee to consist of the required members including the Director of Nursing. This failur...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most Illinois facilities.
- • 47 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • Grade F (25/100). Below average facility with significant concerns.
- • 71% turnover. Very high, 23 points above average. Constant new faces learning your loved one's needs.
About This Facility
What is The Haven Of Bement.'s CMS Rating?
CMS assigns THE HAVEN OF BEMENT. an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Illinois, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is The Haven Of Bement. Staffed?
CMS rates THE HAVEN OF BEMENT.'s staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 71%, which is 25 percentage points above the Illinois average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs.
What Have Inspectors Found at The Haven Of Bement.?
State health inspectors documented 47 deficiencies at THE HAVEN OF BEMENT. during 2023 to 2025. These included: 1 that caused actual resident harm, 45 with potential for harm, and 1 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
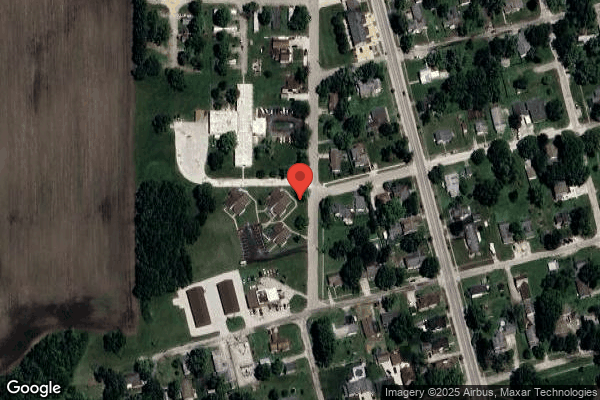
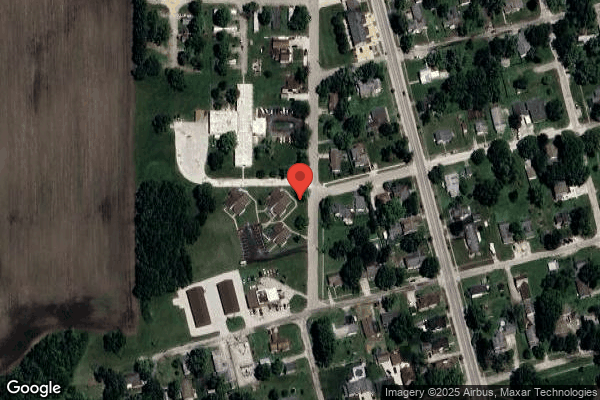
Who Owns and Operates The Haven Of Bement.?
THE HAVEN OF BEMENT. is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by HAVEN HEALTHCARE, a chain that manages multiple nursing homes. With 60 certified beds and approximately 33 residents (about 55% occupancy), it is a smaller facility located in BEMENT, Illinois.
How Does The Haven Of Bement. Compare to Other Illinois Nursing Homes?
Compared to the 100 nursing homes in Illinois, THE HAVEN OF BEMENT.'s overall rating (1 stars) is below the state average of 2.5, staff turnover (71%) is significantly higher than the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting The Haven Of Bement.?
Based on this facility's data, families visiting should ask: "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's high staff turnover rate and the below-average staffing rating.
Is The Haven Of Bement. Safe?
Based on CMS inspection data, THE HAVEN OF BEMENT. has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Illinois. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at The Haven Of Bement. Stick Around?
Staff turnover at THE HAVEN OF BEMENT. is high. At 71%, the facility is 25 percentage points above the Illinois average of 46%. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was The Haven Of Bement. Ever Fined?
THE HAVEN OF BEMENT. has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is The Haven Of Bement. on Any Federal Watch List?
THE HAVEN OF BEMENT. is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.