CUMBERLAND REHAB & HEALTH CC




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Cumberland Rehab & Health Center has a Trust Grade of D, which means it is below average with some concerning issues. It ranks #499 out of 665 nursing homes in Illinois, placing it in the bottom half of all facilities, and #2 out of 2 in Cumberland County, indicating that only one local option is better. Unfortunately, the facility is worsening, with the number of issues increasing from 8 in 2023 to 18 in 2024. Although staffing is a relative strength with a turnover rate of 26%, well below the state average, there are significant concerns regarding RN coverage, as there were days without RN presence, which can potentially affect all residents. Additionally, the facility has faced issues related to food service management, including the lack of qualified dietary staff, which raises concerns about the quality of care provided.
- Trust Score
- D
- In Illinois
- #499/665
- Safety Record
- Low Risk
- Inspections
- Getting Worse
- Staff Stability ✓ Good
- 26% annual turnover. Excellent stability, 22 points below Illinois's 48% average. Staff who stay learn residents' needs.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Illinois facilities.
- Skilled Nurses ⚠ Watch
- Each resident gets only 29 minutes of Registered Nurse (RN) attention daily — below average for Illinois. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 29 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Low Staff Turnover (26%) · Staff stability means consistent care
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover is low (26%)
22 points below Illinois average of 48%
Facility shows strength in staff retention, fire safety.
The Bad
Below Illinois average (2.5)
Significant quality concerns identified by CMS
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 29 deficiencies on record
Sept 2024
17 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide a resident with an Advance Beneficiary Notice (ABN), at the termination of a Medicare Part A covered stay, thereby nullifying the r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to issue a written bed hold notice to a resident's family member when the resident was transferred to the hospital. This failure affects one o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to closely monitor a resident's weight loss, notify the physician of si...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to label and document expiration dates for medications for two residents (R7, R25) and failed to lock the convenience box after ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to appropriately assess, evaluate, and document a resident's behaviors after administering medications for behaviors for one resident (R29) of...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2.) R27's Medical Diagnoses List dated September 2024 documents R27 is diagnosed with Cerebral Palsy, Cerebral Infarction, Convu...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed repeatedly to change oxygen tubing and nasal cannula, sto...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. On 9/22/24 at 8:30 AM, R9 stated the food at the facility is terrible, it's cold. R9 also stated when they had beef and noodl...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to use the services of a Registered Nurse (RN) for at lea...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to employ a qualified Director of Food and Nutrition Services. This failure has the potential to affect all 36 residents residing in the facil...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0802
(Tag F0802)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to employ dietary support/staff with the appropriate com...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected most or all residents
4.) On 9/23/24 at 9:28 AM, during the Resident Council Meeting, R9 and R30 stated condiments are not being served with the meals and not coming on trays (R9) in rooms, the residents have to ask for it...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0809
(Tag F0809)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review the facility failed to provide residents breakfast meal in a timely manner. This failure affected all 36 residents residing in the facility.
Findings...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to prevent the potential for cross-contamination and food-borne illness, by failing to maintain sanitization of a commercial tab...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on interview and record review the facility failed to establish a water management program, failed to develop a risk assessment ensuring that interventions to monitor control limits are met, dev...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interview, and record review the facility failed to maintain kitchen equipment in a safe operable and fun...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review the facility failed to honor residents' right to a clean and comfortable homelike environment by failing to repair and maintain the cleanliness of th...
Read full inspector narrative →
May 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure complete and accurate controlled medication records. This failure has the potential to affect one resident (R1) of three reviewed fo...
Read full inspector narrative →
Dec 2023
8 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to notify the Physician of missed medication for one of one resident (R38) reviewed for Physician notification in the sample list of 26.
Findi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to complete a restraint/enabler assessment for two residents (R12, R21) and failed to release a restraint during lunch for one re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3.) The facility provided Psychotropic Medication Policy revised date November 2001 documents that any resident receiving psycho...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to administer an anticoagulant medication as ordered for one resident. This failure resulted in a significant medication error for one of one r...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on interview and record review the facility failed to ensure that controlled substances were accounted and reconciled for seven (R2, R3, R4, R10, R15, R16, and R23) of seven residents reviewed f...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review the facility failed to store and secure controlled medications behind a separately locked compartment for four (R10, R22, R36 and R193) of four reside...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to have RN (Registered Nurse) coverage for 8 hours/day, 7 days/week for one day, 12/3/23 of 15 days reviewed for nursing coverage. This failur...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to prevent the potential for cross-contamination of disposable plates and failed to maintain sanitary kitchen and pantry floor a...
Read full inspector narrative →
Oct 2022
3 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0661
(Tag F0661)
Could have caused harm · This affected 1 resident
Based on record review and interview the facility failed complete the recapitulation of stay, discharge summary and failed to implement a discharge plan of care for one (R37) resident out of one resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review facility staff failed to prevent cross contamination during urinary catheter care for 1 (R6) of 1 resident reviewed for urinary catheter care in a sam...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to prevent the potential for chemical cross-contamination in the kitchen dishwashing sinks. This failure has the potential to af...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most Illinois facilities.
- • 26% annual turnover. Excellent stability, 22 points below Illinois's 48% average. Staff who stay learn residents' needs.
- • 29 deficiencies on record. Higher than average. Multiple issues found across inspections.
- • Grade D (43/100). Below average facility with significant concerns.
About This Facility
What is Cumberland Rehab & Health Cc's CMS Rating?
CMS assigns CUMBERLAND REHAB & HEALTH CC an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Illinois, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Cumberland Rehab & Health Cc Staffed?
CMS rates CUMBERLAND REHAB & HEALTH CC's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 26%, compared to the Illinois average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Cumberland Rehab & Health Cc?
State health inspectors documented 29 deficiencies at CUMBERLAND REHAB & HEALTH CC during 2022 to 2024. These included: 29 with potential for harm.
Who Owns and Operates Cumberland Rehab & Health Cc?
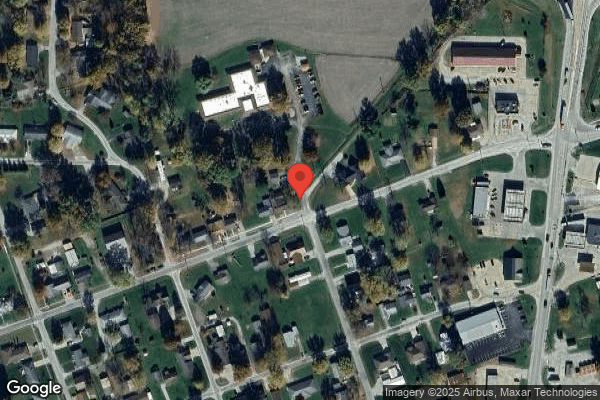
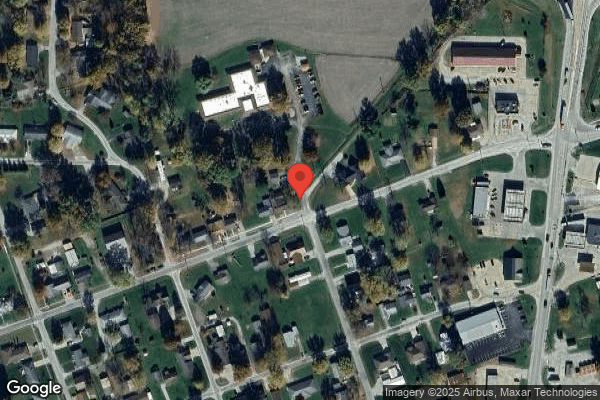
CUMBERLAND REHAB & HEALTH CC is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by PETERSEN HEALTH CARE, a chain that manages multiple nursing homes. With 54 certified beds and approximately 32 residents (about 59% occupancy), it is a smaller facility located in GREENUP, Illinois.
How Does Cumberland Rehab & Health Cc Compare to Other Illinois Nursing Homes?
Compared to the 100 nursing homes in Illinois, CUMBERLAND REHAB & HEALTH CC's overall rating (1 stars) is below the state average of 2.5, staff turnover (26%) is significantly lower than the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Cumberland Rehab & Health Cc?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Cumberland Rehab & Health Cc Safe?
Based on CMS inspection data, CUMBERLAND REHAB & HEALTH CC has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Illinois. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Cumberland Rehab & Health Cc Stick Around?
Staff at CUMBERLAND REHAB & HEALTH CC tend to stick around. With a turnover rate of 26%, the facility is 20 percentage points below the Illinois average of 46%. Low turnover is a positive sign. It means caregivers have time to learn each resident's needs, medications, and personal preferences. Consistent staff also notice subtle changes in a resident's condition more quickly.
Was Cumberland Rehab & Health Cc Ever Fined?
CUMBERLAND REHAB & HEALTH CC has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Cumberland Rehab & Health Cc on Any Federal Watch List?
CUMBERLAND REHAB & HEALTH CC is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.