ST ELIZABETH HEALTHCARE CENTER




Inspected within the last 6 months. Data reflects current conditions.
St. Elizabeth Healthcare Center has a Trust Grade of C+, indicating it is slightly above average but not exceptional. It ranks #191 out of 505 facilities in Indiana, placing it in the top half, and it is the only option in Carroll County. The facility is improving, with issues decreasing from 8 in 2024 to 4 in 2025. Staffing is a concern, with a turnover rate of 57%, higher than the state average, which may affect continuity of care. There have been no fines, which is a positive sign, and the center has more RN coverage than 98% of Indiana facilities, allowing for better oversight of resident care. However, there have been serious incidents, such as a resident having two pain patches improperly monitored, and concerns about staffing levels affecting timely responses to resident needs, indicating areas for improvement in their operations.
- Trust Score
- C+
- In Indiana
- #191/505
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 57% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Indiana facilities.
- Skilled Nurses ✓ Good
- Each resident gets 67 minutes of Registered Nurse (RN) attention daily — more than 97% of Indiana nursing homes. RNs are the most trained staff who catch health problems before they become serious.
- Violations ⚠ Watch
- 28 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
11pts above Indiana avg (46%)
Frequent staff changes - ask about care continuity
Part of a multi-facility chain
Ask about local staffing decisions and management
9 points above Indiana average of 48%
The Ugly 28 deficiencies on record
May 2025
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure resident council concerns and grievances were resolved for 3 of 5 residents reviewed for resident council concerns. (Resident 28, 37...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure staff obtained a follow-up weight to determine if a significant weight loss or gain had occurred and to document if a resident refus...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0628
(Tag F0628)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. The clinical record for Resident 27 was reviewed on 5/6/25 at 11:03 a.m. The diagnoses included, but were not limited to, dis...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure staff had documented training prior to administering 2 step Mantoux skin tests for tuberculosis (TB) and all parts of the procedure ...
Read full inspector narrative →
Apr 2024
8 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure resident council concerns and grievances were addressed and the resolutions to the concerns/grievances were documented in the meetin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure the Notice of Medicare Non-Coverage was given 48 hours prior to the Medicare benefits ending date for 2 of 3 residents reviewed for ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a revised Preadmission Screen and Resident Review (PASARR) level I was completed after psychotropic medications were prescribed for ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure expired medications were removed from the medication cart and medications were labeled for 1 of 3 medication carts revi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure resident rooms and hallways were in good repair...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3a. The clinical record for Resident 31 was reviewed on 4/18/24 at 12:22 p.m. The diagnoses included, but were not limited to, p...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
2. During an observation, on 4/15/24 at 12:45 p.m., Resident 31 was wearing oxygen tubing connected to an empty portable oxygen tank.
During an interview, on 4/15/24 at 12:49 p.m., CNA 10 indicated t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure staff followed infection control standards rela...
Read full inspector narrative →
Jul 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a resident with a diagnosis of dementia, who was at risk for elopement, was supervised when the resident left the facility through a...
Read full inspector narrative →
Jan 2023
15 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0760
(Tag F0760)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure pain patches were monitored for placement and to change an o...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to resolve resident council concerns and grievances for 3 of 3 residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to submit a revised Preadmission Screen and Resident Review (PASARR) Level I after psychotropic medications were prescribed for 1 of 3 residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview, the facility failed to ensure a cognitively impaired resident was provided a preferred activity for 1 of 3 residents reviewed for activities. (Reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to continue to provide a recommended hand splint for a resident with a contracture to the right hand for 1 of 4 residents reviewe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure medications were not left unattended for 1 of 3 residents observed for medication administration. (Resident H)
Finding ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a resident was started on the bowel protocol and to ensure an incontinent resident was changed for 2 of 2 residents observed for bow...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and interview, the facility failed to obtain a physician's order for the use of oxygen (02) ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to dispose of loose pills, refrigerate an unopened insulin pen and to dispose of a compromised controlled substance for 2 of 6 carts reviewed fo...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on record review, interview and observation, the facility failed to serve food at appropriate temperatures for 4 of 4 residents reviewed for food at appropriate temperatures. (Residents Q, R, S ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview, the facility failed to accurately document whether a splint was utilized for a resident's right-hand contracture for 1 of 4 residents reviewed for ra...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 7. During an observation, on 1/6/23 at 2:55 p.m., room [ROOM NUMBER] had a horrible urine odor, and the odor went out into the h...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to ensure a resident needing assistance with ADLs (activity of daily living) were provided the scheduled daily showers for 6 of 6...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the facility failed to ensure enough staff were available to check on call light response times, to staff CNAs according to the Facility Assessment p...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected most or all residents
Based on observation, interview and record review, the facility failed to have nurse staffing posted where it could easily be viewed and failed to have the staffing posted correctly for 5 of the 7 day...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most Indiana facilities.
- • 28 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • 57% turnover. Above average. Higher turnover means staff may not know residents' routines.
About This Facility
What is St Elizabeth Healthcare Center's CMS Rating?
CMS assigns ST ELIZABETH HEALTHCARE CENTER an overall rating of 4 out of 5 stars, which is considered above average nationally. Within Indiana, this rating places the facility higher than 99% of the state's 100 nursing homes. This rating reflects solid performance across the metrics CMS uses to evaluate nursing home quality.
How is St Elizabeth Healthcare Center Staffed?
CMS rates ST ELIZABETH HEALTHCARE CENTER's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 57%, which is 11 percentage points above the Indiana average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs.
What Have Inspectors Found at St Elizabeth Healthcare Center?
State health inspectors documented 28 deficiencies at ST ELIZABETH HEALTHCARE CENTER during 2023 to 2025. These included: 1 that caused actual resident harm, 26 with potential for harm, and 1 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates St Elizabeth Healthcare Center?
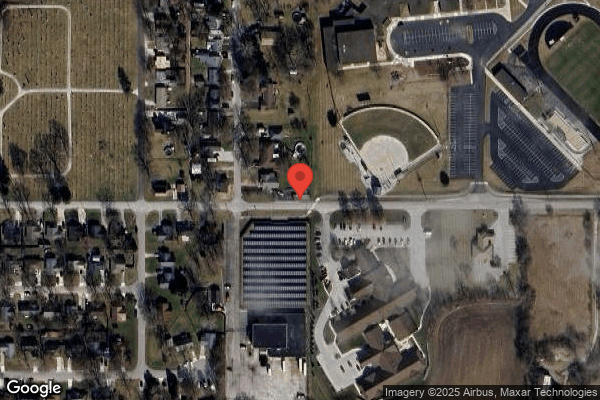
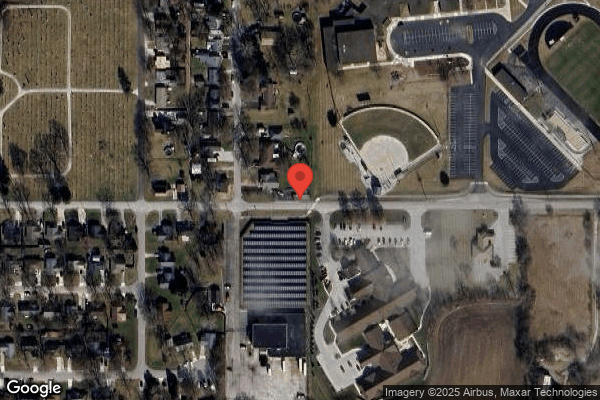
ST ELIZABETH HEALTHCARE CENTER is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility is operated by TRILOGY HEALTH SERVICES, a chain that manages multiple nursing homes. With 64 certified beds and approximately 52 residents (about 81% occupancy), it is a smaller facility located in DELPHI, Indiana.
How Does St Elizabeth Healthcare Center Compare to Other Indiana Nursing Homes?
Compared to the 100 nursing homes in Indiana, ST ELIZABETH HEALTHCARE CENTER's overall rating (4 stars) is above the state average of 3.1, staff turnover (57%) is significantly higher than the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting St Elizabeth Healthcare Center?
Based on this facility's data, families visiting should ask: "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's high staff turnover rate.
Is St Elizabeth Healthcare Center Safe?
Based on CMS inspection data, ST ELIZABETH HEALTHCARE CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 4-star overall rating and ranks #1 of 100 nursing homes in Indiana. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at St Elizabeth Healthcare Center Stick Around?
Staff turnover at ST ELIZABETH HEALTHCARE CENTER is high. At 57%, the facility is 11 percentage points above the Indiana average of 46%. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was St Elizabeth Healthcare Center Ever Fined?
ST ELIZABETH HEALTHCARE CENTER has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is St Elizabeth Healthcare Center on Any Federal Watch List?
ST ELIZABETH HEALTHCARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.