BRICKYARD HEALTHCARE - MUNCIE CARE CENTER




Inspected within the last 6 months. Data reflects current conditions.
Brickyard Healthcare - Muncie Care Center has received a Trust Grade of F, indicating poor quality and significant concerns about the facility's operations. It ranks #431 out of 505 nursing homes in Indiana, placing it in the bottom half of facilities statewide, and #11 out of 13 in Delaware County, meaning there are only two better local options available. The trend is worsening, with issues increasing from 8 in 2024 to 14 in 2025. Staffing is average with a rating of 3 out of 5 stars and a turnover rate of 50%, which is on par with the state average. However, the facility has concerning fines totaling $22,360, higher than 89% of Indiana facilities, and less RN coverage than 80% of state homes, which could impact patient care. Specific incidents reported include a failure to protect a resident from physical abuse by a staff member, which could cause ongoing fear and anxiety. Additionally, there was a serious incident where an allegation of abuse was not reported promptly, leading to further harm to a cognitively impaired resident. While staffing levels are average, the presence of significant quality and safety issues raises concerns for families considering this facility for their loved ones.
- Trust Score
- F
- In Indiana
- #431/505
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 50% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ○ Average
- $22,360 in fines. Higher than 71% of Indiana facilities. Some compliance issues.
- Skilled Nurses ⚠ Watch
- Each resident gets only 27 minutes of Registered Nurse (RN) attention daily — below average for Indiana. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 38 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Indiana average (3.1)
Significant quality concerns identified by CMS
Near Indiana avg (46%)
Higher turnover may affect care consistency
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 38 deficiencies on record
May 2025
13 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0551
(Tag F0551)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure the designated resident health care representative signed medical consent forms for 1 of 1 resident reviewed for health care represe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to notify the physician of elevated blood pressures for 1 of 5 residents reviewed for unnecessary medications. (Resident 39)
Finding includes:...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to provide notifications of hospitalization to the Long-Term Care Ombu...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure bed hold policies were provided to the resident and/or responsible parties at the time of the hospital transfer for 2 of 3 residents...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide catheter care in a manner to reduce the risk of contamination for 1 of 1 resident reviewed for catheter services (Res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to follow Registered Dietician recommendations and notify the physician for a resident experiencing significant weight loss for 1 of 4 residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to check placement and prevent contamination during site care for 1 of 2 residents reviewed for feeding tubes. (Resident 36)
Fin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to follow physician orders regarding oxygen flow rate and humidity for 1 of 2 residents reviewed for oxygen. (Resident 48)
Findi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0744
(Tag F0744)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide individualized interventions for dementia services to reduce or eliminate the need for psychoactive medications for 1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure shift to shift narcotic reconciliation was completed for 5 of 6 carts reviewed for medication storage. (C Unit 2 hall cart, C Unit 1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to ensure insulin was dated after opening and discarded when expired for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to offer and educate residents regarding Pneumococcal vaccines per the Center for Disease and Control (CDC) guidance for 1 of 5 residents revi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to provide education regarding and failed to offer COVID-19 vaccines per the Center for Disease and Control (CDC) guidance for 1 of 5 resident...
Read full inspector narrative →
Feb 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to follow physician ordered parameters for medication administration related to a blood pressure medication for 1 of 3 residents reviewed for ...
Read full inspector narrative →
Jul 2024
8 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure completion of a Significant Change Minimum Set (MDS) assessment within 14 days of a determined status change for 2 of 5 residents re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0638
(Tag F0638)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure timely completion of Quarterly Minimum Data Set (MDS) assessments every three months for 1 of 5 reviewed for timely assessment. (Res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
MDS Data Transmission
(Tag F0640)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure timely submission of Minimum Data Set (MDS) assessments for 1 of 5 resident reviewed for assessment submission. (Resident 65)
Findin...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide consistent interventions to maintain urinary drainage devices for 2 of 3 residents reviewed for urinary catheters. (R...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to monitor the amount of fluids consumed by 1 or 2 residents on fluid restrictions reviewed for dialysis. (Residents 30)
Findings...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to implement and utilize infection prevention and control practices related to contact isolation, enhanced barrier precautions (...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to implement an antibiotic stewardship program per facility policy. This had the potential to affect 98 or 98 residents residing in the facili...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0882
(Tag F0882)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to designate one or more individual(s) as the Infection Preventionist with qualifying training or certification. The facility did not have a c...
Read full inspector narrative →
Aug 2023
3 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to protect the resident's right to be free from physical...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Abuse Prevention Policies
(Tag F0607)
A resident was harmed · This affected 1 resident
Based on interviews and record review, the facility failed to report to the Administrator or designee allegations of abuse for 1 of 3 allegations of abuse reviewed (CNA 6 to Resident D). This failure ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to report timely to the State Agency allegations of abuse for 3 of 3 allegations of abuse (CNA 6 and Resident B, CNA 6 and Resident D, and Re...
Read full inspector narrative →
Jun 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to provide supervision and implement person-centered interventions to ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0659
(Tag F0659)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure QMAs who were not insulin-certified did not administer insulin for 6 of 23 residents receiving insulin or other injectable anti-diab...
Read full inspector narrative →
May 2023
6 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to protect the resident's right to be free from sexual abuse when a resident with severe cognitive impairment (Resident 22) was groped and kis...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to following physician's orders regarding medication administration pa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure staff promptly obtained urinary catheter orders and utilized proper urinary catheter assessment and management techniq...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0740
(Tag F0740)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to develop and implement behavioral programming regarding sexually inappropriate behaviors for 1 of 3 residents reviewed for mood and behavior...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to prime insulin pens to ensure accurate dose administration for 2 of 14 residents observed for medication administration. There...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to resolve resident council concerns related to long call light wait times.
Findings include:
During record review on 5/18/23 at 10:29 a.m., ...
Read full inspector narrative →
Mar 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure the resident representative was notified when a new psychotr...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a new psychotropic medication had an appropriate indication ...
Read full inspector narrative →
Feb 2023
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to prevent the physical abuse of a cognitively impaired resident (Resi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure staff reported allegations of abuse to the Administrator in a timely manner for 1 of 4 residents reviewed for abuse (Resident G). Th...
Read full inspector narrative →
Dec 2022
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to ensure adequate supervision was provided and individualized interventions were initiated to prevent falls for 1 of 3 resident...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 3 harm violation(s). Review inspection reports carefully.
- • 38 deficiencies on record, including 3 serious (caused harm) violations. Ask about corrective actions taken.
- • $22,360 in fines. Higher than 94% of Indiana facilities, suggesting repeated compliance issues.
- • Grade F (23/100). Below average facility with significant concerns.
About This Facility
What is Brickyard Healthcare - Muncie's CMS Rating?
CMS assigns BRICKYARD HEALTHCARE - MUNCIE CARE CENTER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Indiana, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Brickyard Healthcare - Muncie Staffed?
CMS rates BRICKYARD HEALTHCARE - MUNCIE CARE CENTER's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 50%, compared to the Indiana average of 46%.
What Have Inspectors Found at Brickyard Healthcare - Muncie?
State health inspectors documented 38 deficiencies at BRICKYARD HEALTHCARE - MUNCIE CARE CENTER during 2022 to 2025. These included: 3 that caused actual resident harm and 35 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
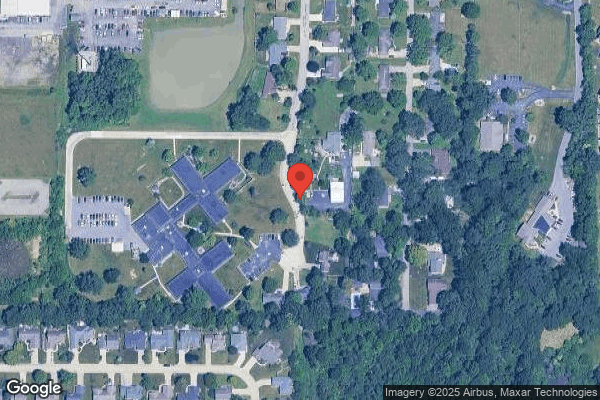
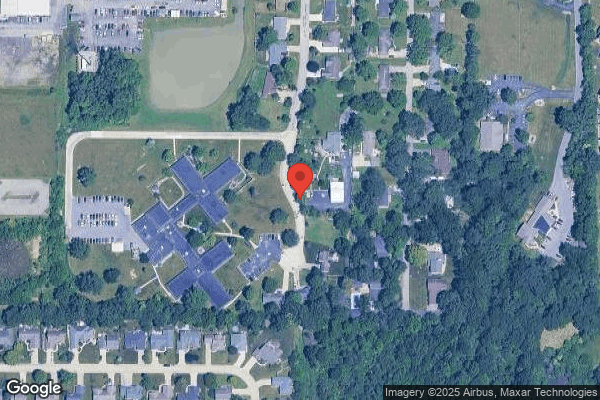
Who Owns and Operates Brickyard Healthcare - Muncie?
BRICKYARD HEALTHCARE - MUNCIE CARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by BRICKYARD HEALTHCARE, a chain that manages multiple nursing homes. With 117 certified beds and approximately 99 residents (about 85% occupancy), it is a mid-sized facility located in MUNCIE, Indiana.
How Does Brickyard Healthcare - Muncie Compare to Other Indiana Nursing Homes?
Compared to the 100 nursing homes in Indiana, BRICKYARD HEALTHCARE - MUNCIE CARE CENTER's overall rating (1 stars) is below the state average of 3.1, staff turnover (50%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Brickyard Healthcare - Muncie?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Brickyard Healthcare - Muncie Safe?
Based on CMS inspection data, BRICKYARD HEALTHCARE - MUNCIE CARE CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Indiana. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Brickyard Healthcare - Muncie Stick Around?
BRICKYARD HEALTHCARE - MUNCIE CARE CENTER has a staff turnover rate of 50%, which is about average for Indiana nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Brickyard Healthcare - Muncie Ever Fined?
BRICKYARD HEALTHCARE - MUNCIE CARE CENTER has been fined $22,360 across 2 penalty actions. This is below the Indiana average of $33,302. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Brickyard Healthcare - Muncie on Any Federal Watch List?
BRICKYARD HEALTHCARE - MUNCIE CARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.