Country Lane Manor




Inspected within the last 6 months. Data reflects current conditions.
Country Lane Manor has received a Trust Grade of F, indicating significant concerns about its quality of care. It ranks #339 out of 392 nursing homes in Iowa, placing it in the bottom half of facilities statewide, although it is the only option in Van Buren County. The facility is showing improvement, reducing issues from 37 in 2024 to 12 in 2025, but it still has a concerning track record with fines totaling $59,150, which is higher than 89% of Iowa facilities. Staffing, rated 2 out of 5 stars, shows a 54% turnover rate, which is average, but the facility has less RN coverage than 80% of Iowa facilities, meaning fewer registered nurses are available to catch potential problems. Specific incidents of concern include failing to conduct necessary assessments for a resident with low blood sugar and not implementing interventions for another resident who hadn’t had a bowel movement for several days. Additionally, one resident was noted to have multiple pressure ulcers upon admission, which raises alarms about the adequacy of care provided. Overall, while there are some signs of improvement, families should be cautious and weigh both the strengths and weaknesses of Country Lane Manor.
- Trust Score
- F
- In Iowa
- #339/392
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 54% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $59,150 in fines. Lower than most Iowa facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 29 minutes of Registered Nurse (RN) attention daily — below average for Iowa. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 56 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Iowa average (3.0)
Significant quality concerns identified by CMS
Near Iowa avg (46%)
Higher turnover may affect care consistency
Above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 56 deficiencies on record
Aug 2025
10 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
Based on staff interview, clinical record review, and facility policy review, the facility failed to attempt to designate resident representation for 1 of 1 residents (Resident #23) with a moderate co...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation, clinical record review, facility policy review and staff interview, the facility failed to complete a self-medication assessment for 1 of 1 residents (Resident #9) who self-admin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
Based on clinical record review, facility policy review, resident and staff interviews, the facility failed to allow 1 of 1 residents (Resident #28) reviewed for smoking, to choose to continue smoking...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, clinical record review, facility policy review, and staff interview, the facility failed to notify the phy...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, clinical record review and staff interviews the facility failed to include the use of an indwelling catheter prior to admission on the care plan for 1 of 1 residents (Resident #4...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, clinical record review, facility policy review and staff interview, the facility failed to clarify orders ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0868
(Tag F0868)
Could have caused harm · This affected 1 resident
Based on attendance record review and interview, the facility failed to have the minimum required members in attendance at their Quality Assurance and Performance Improvement (QAPI) meetings. The faci...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and staff interview, the facility failed to follow infection prevention protocols for 2 of 3...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation and staff interview, the facility failed to follows safe sanitation and food handling practices to prevent cross contamination and foodborne illness. The facility reported a censu...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected multiple residents
Based on staff interview, review of CMS-2567 reports, and facility policy review, the facility failed to ensure an effective QAPI (Quality Assurance Performance Improvement) process to prevent three d...
Read full inspector narrative →
May 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on clinical record review and staff interview, the facility failed to initiate treatment for an eye infection timely and in accordance with professional standards of practice for 1 of 5 resident...
Read full inspector narrative →
Feb 2025
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, food temperatures during food services, and resident interview, the facility failed to serve food in an a...
Read full inspector narrative →
Nov 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on clinical record review, policy review, provider and staff interviews the facility failed to implement a physician order to change a type of wound dressing for 1 of 3 residents (Resident #6) w...
Read full inspector narrative →
Sept 2024
11 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident and staff interview, and clinical record review, the facility failed to ensure resident choice of...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident and staff interview, clinical record review, and facility policy review, the facility failed to e...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure basic nursing principles were followed for 2...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on interview, clinical record review, and facility policy review, the facility failed to follow Provider's orders for indwelling catheter balloon size for 1 of 2 resident (Resident #43) reviewed...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure a Gradual Dose Reduction (GDR) was trialed f...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, clinical record review, and staff interviews the facility failed to have a consistent plan and procedure ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on record review, facility provided documents, and interviews the facility failed to provide sufficient qualified nursing staff to provide nursing services that meet the residents' needs safely ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
Based on interviews, record review, and policy review, the facility failed to provide Monthly Drug Regimen Reviews for the month of July. The facility reported a census of 56 residents.
Findings incl...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and facility policy review, the facility failed to prevent potential for contamination when gloves were not changed at appropriate times during meal service for 1 of 1...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected multiple residents
Based on staff interview, review of CMS-2567 reports, and facility policy review, the facility failed to ensure an effective QAPI (Quality Assurance Performance Improvement) process to address previou...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
PASARR Coordination
(Tag F0644)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, clinical record review, and Pre-admission Screening Resident Review (PASRR) level 2 review, the facili...
Read full inspector narrative →
May 2024
22 deficiencies
4 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, policy review, resident interview and staff interviews, the facility failed to carry out assess...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. The MDS assessment dated [DATE] revealed Resident #208 scored a 15 out of 15 on the BIMS exam, which indicated cognition inta...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. The MDS assessment dated [DATE] revealed Resident #19 scored a 11 out of 15 on the BIMS exam, which indicated moderately impa...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0692
(Tag F0692)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. The MDS assessment dated [DATE] revealed Resident #13 scored a 6 out of 15 on the BIMS exam, which indicated moderately impai...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, staff interview, and clinical record review, the facility failed to ensure a dignified dining experience ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, clinical record review, policy review, resident interview and staff interview, the facility failed to individualize the physical space of a resident's bathroom in order to ensure...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on resident interview, staff interviews, clinical record review, and the facility policy, the facility failed to supply th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on clinical record review, staff interview, and policy review, the facility failed to notify 1 of 3 Medicare Part A beneficiaries of coverage ending (Resident#8). The facility reported a census ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on personnel record review, staff interview, and facility policy review the facility failed to ensure staff's background checks completed prior to hire date for 1 of 5 staff; and failed to ensur...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Review of the MDS assessment for Resident #11 dated 3/21/24 revealed the resident scored 6 out of 15 on a Brief Interview for...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. The MDS assessment dated [DATE] revealed Resident #50 scored a 14 out of 15 on the BIMS exam, which indicated cognition intac...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, staff interviews, resident interviews, clinical record review, and facility policy review the facility fa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. The MDS assessment dated [DATE] revealed Resident #19 scored a 12 out of 15 on the BIMS exam, which indicated moderately impa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interviews, clinical record review, and the facility policy, the facility failed to ensure the resident didn't ha...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. The MDS assessment dated [DATE] revealed Resident #13 scored a 6 out of 15 on the BIMS exam, which indicated cognition severe...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0809
(Tag F0809)
Could have caused harm · This affected 1 resident
Based on clinical record review, policy review, resident interviews and staff interviews, the facility failed to offer bedtime snacks to 2 of 2 residents who desired bedtime snacks (Residents #28 and ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0567
(Tag F0567)
Could have caused harm · This affected multiple residents
Based on facility document review, staff interview and facility policy review, the facility failed to ensure a process in place to allow consistent access to resident funds outside of business hours f...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, resident interviews, staff interviews, clinical record review, and the facility policy, the facility fail...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on observations, menu review, policy review, and staff interviews, the facility failed to ensure 18 of 18 residents receiving a mechanical soft diet received the correct meal portion and failed ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observations, facility document review, policy review, and staff interviews, the facility failed to maintain adequate kitchen sanitation and failed to follow infection control measures to pre...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0570
(Tag F0570)
Minor procedural issue · This affected multiple residents
Based on facility document review, staff interview and facility policy review, the facility failed to ensure a surety bond in place to cover the total amount of personal funds in the resident trust ac...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0865
(Tag F0865)
Minor procedural issue · This affected most or all residents
Based on staff interview, review of CMS-2567 reports, and facility QAPI (Quality Assurance and Performance Improvement) Plan, the facility failed to ensure an effective QAPI (Quality Assurance Perform...
Read full inspector narrative →
Mar 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected 1 resident
Based on observations, food temperatures during food services, and resident interviews, the facility failed to serve food within appropriate temperature ranges, with consistently adequate flavoring an...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Administration
(Tag F0835)
Could have caused harm · This affected multiple residents
Based on observations and provider interview, the facility failed to pay it's waste management providers resulting in delayed and absent pick up. The facility reported census was 50 residents.
Finding...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on record review, staff interviews, facility policy review, and Centers for Disease Control information the facility failed to follow proper infection control practices to mitigate the risk for ...
Read full inspector narrative →
Oct 2023
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, record review, and facility policy review, the facility failed to ensure residents treated in a dignified m...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, record review, and facility policy review, the facility failed to update the Care Plan and fall intervention...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, record review, and the facility policy review, the facility failed to adequately supervise a resident in a s...
Read full inspector narrative →
MINOR
(C)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Minor Issue - procedural, no safety impact
Deficiency F0865
(Tag F0865)
Minor procedural issue · This affected most or all residents
Based on interview, the plan of correction and review of CMS-2567 reports, the facility failed to ensure an effective QAPI (Quality Assurance Performance Improvement) process to address previously ide...
Read full inspector narrative →
Aug 2023
3 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, clinical record review and staff interviews, the facility failed to safely provide cares when turning a re...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, clinical record review and staff interviews, the facility failed to provide incontinence cares for 1 of 4 residents reviewed who were unable to carry out the activity independent...
Read full inspector narrative →
MINOR
(B)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Minor Issue - procedural, no safety impact
Deficiency F0573
(Tag F0573)
Minor procedural issue · This affected multiple residents
Based on clinical record review, family and staff interviews, the facility failed to ensure requests for medical records are provided within two working days of the request for 2 of 2 records reviewed...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 5 harm violation(s), $59,150 in fines, Payment denial on record. Review inspection reports carefully.
- • 56 deficiencies on record, including 5 serious (caused harm) violations. Ask about corrective actions taken.
- • $59,150 in fines. Extremely high, among the most fined facilities in Iowa. Major compliance failures.
- • Grade F (5/100). Below average facility with significant concerns.
About This Facility
What is Country Lane Manor's CMS Rating?
CMS assigns Country Lane Manor an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Iowa, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Country Lane Manor Staffed?
CMS rates Country Lane Manor's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 54%, compared to the Iowa average of 46%.
What Have Inspectors Found at Country Lane Manor?
State health inspectors documented 56 deficiencies at Country Lane Manor during 2023 to 2025. These included: 5 that caused actual resident harm, 46 with potential for harm, and 5 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
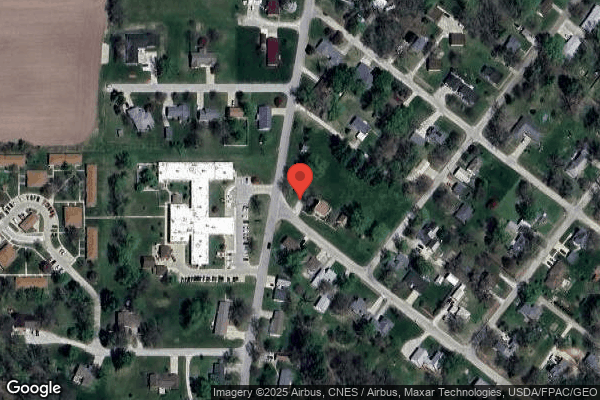
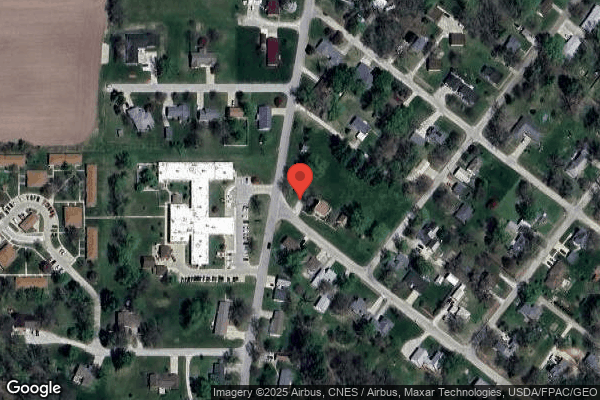
Who Owns and Operates Country Lane Manor?
Country Lane Manor is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by CAMPBELL STREET SERVICES, a chain that manages multiple nursing homes. With 60 certified beds and approximately 53 residents (about 88% occupancy), it is a smaller facility located in Keosauqua, Iowa.
How Does Country Lane Manor Compare to Other Iowa Nursing Homes?
Compared to the 100 nursing homes in Iowa, Country Lane Manor's overall rating (1 stars) is below the state average of 3.0, staff turnover (54%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Country Lane Manor?
Based on this facility's data, families visiting should ask: "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the below-average staffing rating.
Is Country Lane Manor Safe?
Based on CMS inspection data, Country Lane Manor has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Iowa. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Country Lane Manor Stick Around?
Country Lane Manor has a staff turnover rate of 54%, which is 8 percentage points above the Iowa average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Country Lane Manor Ever Fined?
Country Lane Manor has been fined $59,150 across 1 penalty action. This is above the Iowa average of $33,670. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Country Lane Manor on Any Federal Watch List?
Country Lane Manor is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.