ACADIA ST LANDRY NURSING & REHABILITATION CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Acadia St Landry Nursing & Rehabilitation Center has received a Trust Grade of F, indicating significant concerns about the facility's quality of care. It ranks #174 out of 264 nursing homes in Louisiana, placing it in the bottom half of facilities in the state, and #4 out of 5 in Acadia County, meaning only one local option is better. While the facility has shown improvement in its trend, reducing issues from 18 in 2024 to 13 in 2025, it still faces serious challenges, including $268,528 in fines, which is concerning and higher than 94% of Louisiana facilities. Staffing is a mixed bag; although the turnover rate of 36% is better than the state average of 47%, the facility has less RN coverage than 79% of state facilities, which impacts the quality of care. Specific incidents of concern include a resident falling and getting injured due to improper transfer methods, and another resident not receiving appropriate diabetic foot care, leading to serious skin issues. Overall, families should weigh these strengths and weaknesses carefully when considering this facility.
- Trust Score
- F
- In Louisiana
- #174/264
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- 36% turnover. Near Louisiana's 48% average. Typical for the industry.
- Penalties ⚠ Watch
- $268,528 in fines. Higher than 76% of Louisiana facilities, suggesting repeated compliance issues.
- Skilled Nurses ⚠ Watch
- Each resident gets only 9 minutes of Registered Nurse (RN) attention daily — below average for Louisiana. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 46 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (36%)
12 points below Louisiana average of 48%
Facility shows strength in fire safety.
The Bad
Below Louisiana average (2.4)
Significant quality concerns identified by CMS
Near Louisiana avg (46%)
Typical for the industry
Well above median ($33,413)
Significant penalties indicating serious issues
The Ugly 46 deficiencies on record
Feb 2025
13 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to protect the resident's right to be free from neglect for 1 (#105)...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide form CMS (Centers for Medicare and Medicaid Services) 10123- Notice of Medicare Non Coverage (NOMNC) as required for 1 Resident (#9...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to provide the necessary care and services to provide ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interviews, the facility failed to ensure ongoing communication and collaboration with the dialysis ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to ensure that residents who were capable of using call bells were able ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observation, and interviews, the facility failed to ensure a resident's change in condition was immediat...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to refer residents with newly diagnosed mental disorders or had a sign...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, the facility failed to ensure a resident's plan of care was implemented for 1 (#107) out ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0576
(Tag F0576)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interviews, the facility failed to ensure the residents received mail on Saturdays. The deficient pr...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected most or all residents
Based on observations and interviews, the facility failed to ensure drugs were stored in accordance with currently accepted professional principles by:
1. having loose pills in 2 (Cart A and Cart B) o...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations and interviews, the facility failed to maintain a clean and sanitary kitchen to prevent the likelihood of foodborne illnesses and store and serve meals in accordance with profess...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Administration
(Tag F0835)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to be administered in a manner that enabled it to use its resources effectively and efficiently to ensure the well-being of resi...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to establish and maintain an infection prevention and co...
Read full inspector narrative →
Dec 2024
4 deficiencies
3 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Comprehensive Care Plan
(Tag F0656)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, the facility failed to develop a comprehensive person-centered care plan for foot care an...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0658
(Tag F0658)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, record review,and observation the facility failed to ensure services provided met professional standards of...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0687
(Tag F0687)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to ensure that residents received preventative foot care to avoid co...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to notify the resident's Responsible Party (RP) of a change in skin condition for 1 (Resident #3) of 6 (Resident #1,#2, #3, #R1, #R2, and #R3...
Read full inspector narrative →
May 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews the facility failed to ensure physician orders/plan of care were implemented as ordered fo...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on observations, interview, and menu review, the facility's kitchen staff failed to follow the menu to ensure residents were served the appropriate portion/serving size of food during meals in o...
Read full inspector narrative →
Jan 2024
12 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0568
(Tag F0568)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to maintain a system of accounting of each resident's personal funds e...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on observations and interviews, the facility failed to maintain privacy and confidentiality of residents' medical records for 2 out of 6 residents observed during medication pass. The facility h...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview the facility failed to provide residents with a safe, clean and homelike environment for 2 (#...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0642
(Tag F0642)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident #54:
A review of Resident #54's Discharge MDS (Minimum Data Set) with an ARD (Assessment Reference Date) of 12/15/2023,...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and record reviews, the facility failed to ensure residents who need respiratory care were pro...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review and interviews, the facility failed to ensure its medication error rate was not 5 percent o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to ensure medications were stored properly and not left unattended on top of the medication cart while administering medicati...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure the facility-wide assessment included any ethnic, cultural, ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
MDS Data Transmission
(Tag F0640)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to electronically transmit a completed Minimum Data Set (MDS) to the C...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and record reviews, the facility failed to implement the residents' plan of care by not follow...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on observations, record review, and interview, the facility failed to ensure recipes for pureed meals were available for staff. This failure had the potential to contribute to an unpleasant dini...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observations, record review and interviews, the facility failed to serve food in a sanitary manner as evidenced by:
1.
staff failing to wear gloves while handling raw meat; and
2.
staff fai...
Read full inspector narrative →
Nov 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure 1 (#3) of 3 (#1, #2, #3) residents were free from abuse as e...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to make efforts to demonstrate diligence and a genuine attempt to develop and implement appropriate plans of action to ensure residents were f...
Read full inspector narrative →
Aug 2023
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility's nursing staff failed to revise the resident's care plan upon return from th...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility's nursing staff failed to implement the residents' plan of care for obtaining...
Read full inspector narrative →
MINOR
(C)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected most or all residents
Based on observations, interviews and record reviews, the facility failed to ensure the posted nurse staffing information was current with the actual hours worked and posted on a daily basis at the be...
Read full inspector narrative →
Jun 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident #5
Resident #5 was admitted to the facility on [DATE] with diagnoses in part: Hemiplegia and Hemiparesis following Cere...
Read full inspector narrative →
Dec 2022
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, the facility failed to ensure a resident's dialysis status was accurately coded on the MD...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observations, record review, and interviews the facility failed to ensure 1 (#22) of 32 sampled residents' slippers were clean and sanitary out of a census of 106 Residents.
Findings:
Record...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and record review, the facility's nursing services failed to demonstrate appropriate competenci...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observation, and interview, the facility failed to ensure the resident received a mechanically soft chop...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
Based on observations, record review and interviews the facility failed ensure 1 (#22) of a 32 sampled residents observed for call lights were working at bedside in a facility with a census of 106 Res...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observations, record review and interviews the facility failed to ensure 6 (#21,#22, #43, #49, #64, and #68) of 62 residents that utilized wheelchairs in the facility were clean and sanitary ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0646
(Tag F0646)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to refer a resident who demonstrated increased behavioral, psychiatric...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, record review and interviews, the facility failed to accurately monitor the temperature of cold food and hot foods. This deficient practice had the potential to affect 101 reside...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0868
(Tag F0868)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to maintain an Infection Preventionist as part of the quality assessment and assurance committee. This had the potential to affect the 106 res...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What safeguards are in place to prevent abuse and neglect?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 36% turnover. Below Louisiana's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: Federal abuse finding, 4 harm violation(s), $268,528 in fines. Review inspection reports carefully.
- • 46 deficiencies on record, including 4 serious (caused harm) violations. Ask about corrective actions taken.
- • $268,528 in fines. Extremely high, among the most fined facilities in Louisiana. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Acadia St Landry Nursing & Rehabilitation Center's CMS Rating?
CMS assigns ACADIA ST LANDRY NURSING & REHABILITATION CENTER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Louisiana, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Acadia St Landry Nursing & Rehabilitation Center Staffed?
CMS rates ACADIA ST LANDRY NURSING & REHABILITATION CENTER's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 36%, compared to the Louisiana average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Acadia St Landry Nursing & Rehabilitation Center?
State health inspectors documented 46 deficiencies at ACADIA ST LANDRY NURSING & REHABILITATION CENTER during 2022 to 2025. These included: 4 that caused actual resident harm, 41 with potential for harm, and 1 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
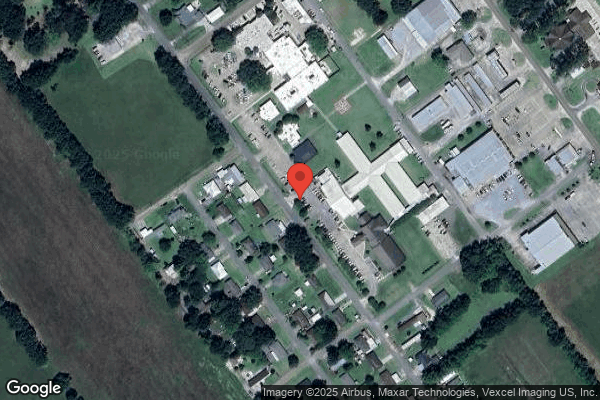
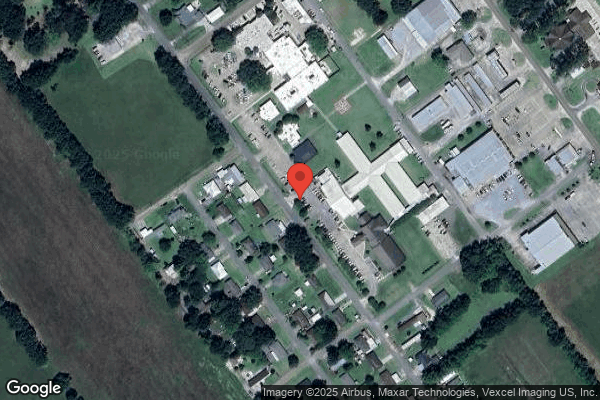
Who Owns and Operates Acadia St Landry Nursing & Rehabilitation Center?
ACADIA ST LANDRY NURSING & REHABILITATION CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 134 certified beds and approximately 120 residents (about 90% occupancy), it is a mid-sized facility located in CHURCH POINT, Louisiana.
How Does Acadia St Landry Nursing & Rehabilitation Center Compare to Other Louisiana Nursing Homes?
Compared to the 100 nursing homes in Louisiana, ACADIA ST LANDRY NURSING & REHABILITATION CENTER's overall rating (1 stars) is below the state average of 2.4, staff turnover (36%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Acadia St Landry Nursing & Rehabilitation Center?
Based on this facility's data, families visiting should ask: "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the substantiated abuse finding on record and the below-average staffing rating.
Is Acadia St Landry Nursing & Rehabilitation Center Safe?
Based on CMS inspection data, ACADIA ST LANDRY NURSING & REHABILITATION CENTER has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Louisiana. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Acadia St Landry Nursing & Rehabilitation Center Stick Around?
ACADIA ST LANDRY NURSING & REHABILITATION CENTER has a staff turnover rate of 36%, which is about average for Louisiana nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Acadia St Landry Nursing & Rehabilitation Center Ever Fined?
ACADIA ST LANDRY NURSING & REHABILITATION CENTER has been fined $268,528 across 2 penalty actions. This is 7.5x the Louisiana average of $35,764. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Acadia St Landry Nursing & Rehabilitation Center on Any Federal Watch List?
ACADIA ST LANDRY NURSING & REHABILITATION CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.