WILLOWBROOKE CT SKILLED CARE CTR AT BAYLEIGH CHASE




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Willowbrooke Court Skilled Care Center at Bayleigh Chase has received a Trust Grade of F, indicating significant concerns about the quality of care provided. Ranking #180 out of 219 nursing homes in Maryland places it in the bottom half of facilities in the state, although it is ranked #1 out of 2 in Talbot County, meaning there is only one other local option. The facility's trend is worsening, with issues increasing from 11 in 2019 to 12 in 2025, raising red flags for potential future problems. Staffing is a relative strength, with a rating of 4 out of 5 stars and a turnover rate of 20%, which is well below the state average. However, the facility has accumulated $109,968 in fines, which is concerning because it is higher than 95% of Maryland facilities, suggesting ongoing compliance issues. Several specific incidents highlight weaknesses at this facility. It was found that staff failed to protect residents from incidents of abuse and did not adequately investigate when one resident had 11 falls, resulting in a serious injury. Additionally, the facility did not conduct annual performance reviews for Geriatric Nursing Assistants, potentially affecting the quality of care across the board. While there are strengths in staffing and RN coverage, the overall picture raises serious concerns that families should consider carefully.
- Trust Score
- F
- In Maryland
- #180/219
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ✓ Good
- 20% annual turnover. Excellent stability, 28 points below Maryland's 48% average. Staff who stay learn residents' needs.
- Penalties ✓ Good
- $109,968 in fines. Lower than most Maryland facilities. Relatively clean record.
- Skilled Nurses ✓ Good
- Each resident gets 62 minutes of Registered Nurse (RN) attention daily — more than 97% of Maryland nursing homes. RNs are the most trained staff who catch health problems before they become serious.
- Violations ⚠ Watch
- 38 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
Low Staff Turnover (20%) · Staff stability means consistent care
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover is low (20%)
28 points below Maryland average of 48%
Facility shows strength in staffing levels, staff retention, fire safety.
The Bad
Below Maryland average (3.0)
Below average - review inspection findings carefully
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 38 deficiencies on record
Jan 2025
12 deficiencies
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility reported incidents, record review and interview with facility staff it was determined that the facility staff ...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, record review, and policy review, the facility failed to ensure one resident (Resident (R)52) of two residen...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, review of facility reported incidents and interview with facility staff, it was determined that ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview with facility staff, it was determined that the facility staff failed to thoroughly...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, record review, and policy review, the facility failed to ensure one of six observed residents (...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with facility staff, and after the review of multiple facility reported incidents, it was determined that the facility failed to administer and document pa...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on review of the medical record and interview with staff it was determined the facility staff failed to maintain complete and accurate medical records. This was evident for 1 (#901) of 9 residen...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Administration
(Tag F0835)
Could have caused harm · This affected multiple residents
Based on staff interview and medical record review, it was determined that the facility administration failed to provide effective oversight activities for the facility to ensure that resources were u...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0943
(Tag F0943)
Could have caused harm · This affected multiple residents
Based on record review and staff interview it was determined the facility failed to ensure that all nursing staff received training on abuse which included procedures for reporting incidents of abuse,...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected most or all residents
Based on review of staff records and interview with facility staff, it was determined that the facility failed to ensure Geriatric Nursing Assistants (GNAs) received a performance review at least once...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, record review, interview, and policy review, the facility failed to ensure staff were taking meal temperatures to ensure they were served at safe temperatures before each meal wa...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected most or all residents
Based on interview and review of facility documentation, the Quality Assurance (QA) committee failed to complete a thorough Performance Improvement Project (PIP) that was a continuous improvement of p...
Read full inspector narrative →
Jul 2019
11 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on medical record review and interview it was determined that the facility failed to include the required statement of the resident's appeal rights and Ombudsman contact information in the writt...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
MDS Data Transmission
(Tag F0640)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with facility staff, it was determined that Resident #1's Minimum Data Set assessment was not submitted regarding the resident's discharge. This was eviden...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, medical record review and interview with the facility staff it was determined that the facility failed to ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
Based on interview with resident, staff and observation it was determined that the facility failed to provide activities to all residents equally that were admitted to the facility.
The findings incl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview it was determined that facility staff failed to: 1) maintain observation of a cognitively impaired resident who was later found outside of the facili...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation and medical record review it was determined that the facility failed to administer medications and maintain an error rate of less than 5% by following physician orders. This was e...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on tour and observation it was determined that the facility failed to maintain a secure store room. This was evident during a random tour of the facility.
The findings include:
During tour of t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview it was determined that facility staff failed to document a resident's wandering behaviors in the medical record. This was evident for 1 of 23 residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0923
(Tag F0923)
Could have caused harm · This affected 1 resident
Based on observation and staff interview it was determined that the facility failed to provide proper ventilation for residents. This was true for 1 of 2 bathing spas (Chop Tank) that were in the faci...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
3) Review of the Care Plan signature sheets on 7/11/19 revealed there were no signatures of attendance for a nutrition service staff or a Geriatric Nursing Assistant (GNA) for Resident #23 and Residen...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected multiple residents
Based on review of posted staffing and interview with the Director of Nursing (DON) it was determined that the facility failed to identify a charge nurse other than the DON.
The findings include:
Revi...
Read full inspector narrative →
Feb 2018
15 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with the facility staff, it was determined that the facility failed to document timely notification to a resident or representative (RP) regarding notifica...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with staff it was determined that the facility failed to have a system in place to ensure that residents or resident representatives were notified in writi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with staff it was determined that the facility failed to have a system in place to ensure that residents or resident responsible party (RP) were given writ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview it was determined that the facility staff failed to provide an accurate assessment of Resident #17's transfer status. This was true in 1 (Resident #1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on medical record review, interview with facility staff it was determined that the facility failed to obtain an Occupational Therapy evaluation prior to giving the resident a walker and to asses...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations it was determined the facility staff failed to adhere to infection control practices and policies when pro...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. On 02/13/18 at 3:24 PM an interview with Resident #43 was conducted. The resident stated that staff would hold various conver...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected multiple residents
Based upon resident interviews, record review and staff interviews it was determined that facility staff failed to consider or act upon Resident Council's grievances regarding food and staff interacti...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. On 2/16/18 Resident #29's medical records were reviewed. It revealed that the resident was admitted to Hospice Care on 12/21/...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
3. On 2/15/18 at 4:45 PM a review of Resident #82's medical records was conducted. The resident was receiving the medication Coumadin a blood thinner. Review of the electronic version of the care plan...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
2. On 02/14/18 at 3:31 PM a medical record review for Resident #33 was conducted. The Minimum Data Set (MDS) conducted on 9/28/17 noted a significant change in the Functional Status for transfers, toi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
Based on observation, medical record review, resident and staff interviews it was determined that the facility staff failed to put a system into place to ensure that delegation of duties regarding med...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
2. During observation on the Wye unit on 2/15/18 at 6:30 PM surveyor noted GNA (Staff #5) approached Resident #17 to escort him/her down hallway to the activity room. Surveyor noted that although the ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on medication administration observation it was determined the facility staff failed to ensure a medication error rate of less than 5 percent (7.89%) for 5 Residents (Resident #59, #79, #70, #13...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
Based on interviews and review of dietary temperature logs it was determined that the facility staff failed to ensure meals were palatable. This failure had the potential to affect all residents recei...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "What safeguards are in place to prevent abuse and neglect?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 20% annual turnover. Excellent stability, 28 points below Maryland's 48% average. Staff who stay learn residents' needs.
- • Multiple safety concerns identified: Federal abuse finding, 1 life-threatening violation(s), 1 harm violation(s), $109,968 in fines. Review inspection reports carefully.
- • 38 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $109,968 in fines. Extremely high, among the most fined facilities in Maryland. Major compliance failures.
- • Grade F (8/100). Below average facility with significant concerns.
About This Facility
What is Willowbrooke Ct Skilled Care Ctr At Bayleigh Chase's CMS Rating?
CMS assigns WILLOWBROOKE CT SKILLED CARE CTR AT BAYLEIGH CHASE an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Maryland, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Willowbrooke Ct Skilled Care Ctr At Bayleigh Chase Staffed?
CMS rates WILLOWBROOKE CT SKILLED CARE CTR AT BAYLEIGH CHASE's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 20%, compared to the Maryland average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Willowbrooke Ct Skilled Care Ctr At Bayleigh Chase?
State health inspectors documented 38 deficiencies at WILLOWBROOKE CT SKILLED CARE CTR AT BAYLEIGH CHASE during 2018 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 1 that caused actual resident harm, and 36 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Willowbrooke Ct Skilled Care Ctr At Bayleigh Chase?
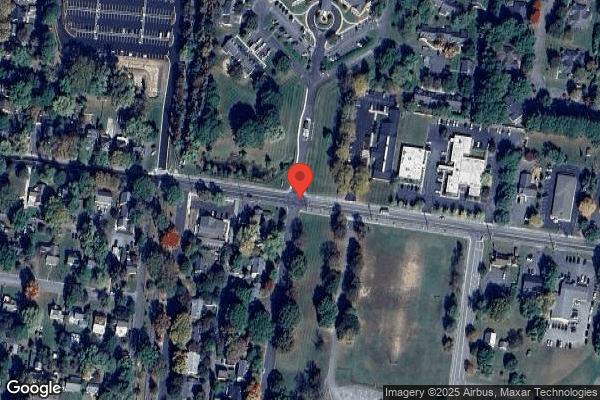
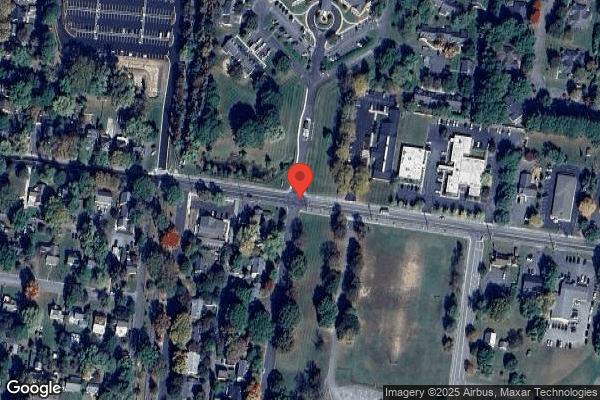
WILLOWBROOKE CT SKILLED CARE CTR AT BAYLEIGH CHASE is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility is operated by ACTS RETIREMENT-LIFE COMMUNITIES, a chain that manages multiple nursing homes. With 99 certified beds and approximately 59 residents (about 60% occupancy), it is a smaller facility located in EASTON, Maryland.
How Does Willowbrooke Ct Skilled Care Ctr At Bayleigh Chase Compare to Other Maryland Nursing Homes?
Compared to the 100 nursing homes in Maryland, WILLOWBROOKE CT SKILLED CARE CTR AT BAYLEIGH CHASE's overall rating (2 stars) is below the state average of 3.0, staff turnover (20%) is significantly lower than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Willowbrooke Ct Skilled Care Ctr At Bayleigh Chase?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's Immediate Jeopardy citations and the substantiated abuse finding on record.
Is Willowbrooke Ct Skilled Care Ctr At Bayleigh Chase Safe?
Based on CMS inspection data, WILLOWBROOKE CT SKILLED CARE CTR AT BAYLEIGH CHASE has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Maryland. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Willowbrooke Ct Skilled Care Ctr At Bayleigh Chase Stick Around?
Staff at WILLOWBROOKE CT SKILLED CARE CTR AT BAYLEIGH CHASE tend to stick around. With a turnover rate of 20%, the facility is 25 percentage points below the Maryland average of 46%. Low turnover is a positive sign. It means caregivers have time to learn each resident's needs, medications, and personal preferences. Consistent staff also notice subtle changes in a resident's condition more quickly. Registered Nurse turnover is also low at 17%, meaning experienced RNs are available to handle complex medical needs.
Was Willowbrooke Ct Skilled Care Ctr At Bayleigh Chase Ever Fined?
WILLOWBROOKE CT SKILLED CARE CTR AT BAYLEIGH CHASE has been fined $109,968 across 1 penalty action. This is 3.2x the Maryland average of $34,179. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Willowbrooke Ct Skilled Care Ctr At Bayleigh Chase on Any Federal Watch List?
WILLOWBROOKE CT SKILLED CARE CTR AT BAYLEIGH CHASE is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.