WICOMICO NURSING HOME




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Wicomico Nursing Home has a Trust Grade of F, indicating significant concerns about its quality of care. With a state rank of #132 out of 219, they fall in the bottom half of facilities in Maryland, though they rank #2 out of 4 locally in Wicomico County, meaning only one nearby option is better. The facility is showing improvement, with issues decreasing from 9 in 2024 to 3 in 2025. Staffing is a relative strength, rated 4 out of 5 stars, but with a turnover rate of 43%, it is about average. However, the facility has incurred $28,343 in fines, which is higher than 77% of Maryland facilities, suggesting ongoing compliance issues. Additionally, there have been serious incidents, such as a failure to provide timely dental care for a resident, leading to significant weight loss, and allegations of abuse where a staff member mishandled a resident during care. While there are strengths in staffing and RN coverage, families should weigh these against the facility's poor trust grade and concerning history of fines and incidents.
- Trust Score
- F
- In Maryland
- #132/219
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- 43% turnover. Near Maryland's 48% average. Typical for the industry.
- Penalties ✓ Good
- $28,343 in fines. Lower than most Maryland facilities. Relatively clean record.
- Skilled Nurses ✓ Good
- Each resident gets 59 minutes of Registered Nurse (RN) attention daily — more than average for Maryland. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 39 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (43%)
5 points below Maryland average of 48%
Facility shows strength in staffing levels, fire safety.
The Bad
Near Maryland average (3.0)
Meets federal standards, typical of most facilities
Near Maryland avg (46%)
Typical for the industry
Below median ($33,413)
Moderate penalties - review what triggered them
The Ugly 39 deficiencies on record
Mar 2025
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on surveyor reviews of a facility reported incident and facility staff interview, it was determined that the facility failed to report the final investigation of an incident of alleged abuse rep...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on reviews of a complaint, interviews with staff, and reviews of a closed record, it was determined that the facility failed to ensure that a resident's medications were administered as ordered....
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined the facility staff failed to maintain a medical record in the most accurate form. This was evident for 1 of (Resident #1) of 4 res...
Read full inspector narrative →
Aug 2024
9 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Deficiency Text Not Available
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Dental Services
(Tag F0791)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, resident and staff interviews, and record review, the facility failed to ensure routine and 24-hour emerg...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and policy review, the facility failed to provide visual privacy during a bed bath for one of one resident (Resident (R) 56) reviewed for privacy of 30 sample reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, record review, and policy review, the facility failed to maintain a restraint free environmen...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Deficiency Text Not Available
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Deficiency Text Not Available
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Deficiency Text Not Available
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and policy review, CPAP (continues positive airway pressure)/ nebulizer masks were not properly...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
Deficiency Text Not Available
Read full inspector narrative →
Jun 2019
24 deficiencies
2 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
Based on resident interview, staff interview, clinical record review, and a review of the facility abuse investigation it was determined that the facility staff failed to ensure residents were free fr...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on a facility reported incident, review of a medical record, and staff interview, it was
determined that a facility staff member failed to follow a resident's care plan to prevent the
resident f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on record review, observation and interview, it was determined the facility staff failed to provide residents (#42, #53 and #164) with the most dignified existence. This was evident for 3 of 34 ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, it was determined the facility staff failed to void an older MOLST form located in a resident's ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on medical record review and interviews with facility staff, it was determined the facility staff failed to notify the responsible party in a timely manner of a resident's fall ( Resident #212) ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations it was determined the facility failed to 1) provide housekeeping and maintenance services to keep the resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on clinical record review, staff interview, and a review of the facility investigation it was determined that the facility staff failed to conduct a thorough investigation. This was evident for ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with staff it was determined the facility staff failed to provide a written notice for emergency transfers to the resident /or the resident representative....
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, it was determined the facility staff failed to provide the resident and thei...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, it was determined the facility staff failed to initiate, provide and implement comprehensive care plans for residents. This was evident for 1 (Resident #1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, it was determined the facility staff failed to ensure Resident #26 was free from constipation. This was evident for 1 of 3 residents selected for review o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical review and interview, it was determined the facility staff failed to thoroughly address pain complaints for Res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0729
(Tag F0729)
Could have caused harm · This affected 1 resident
Based on medical record review, observation and interview, it was determined the facility staff failed to verify a privately hired sitter's training and competency to perform tasks as a Geriatric Nurs...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, it was determined the facility staff failed to hold a blood pressure medication when the documented blood pressure was below the set parameter as ordered ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Laboratory Services
(Tag F0770)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, it was determined the facility staff failed to obtain laboratory test as ordered for Resident (#31). This was evident for 1 of 34 residents selected for r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0790
(Tag F0790)
Could have caused harm · This affected 1 resident
Based on clinical record review, resident observation, resident interview and staff interview it was determined that facility staff failed to obtain a dental examination for its residents (#53). This ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined the facility staff failed to thorough review during the QA meetings the continued use of antibiotics for Resident (#31). This was evident for 1 ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
2. A review of employee's health records was conducted on 6/12/2019. Employee's #17's, 18's, 19's and #20's Health Records lacked documentation of the employee's Tuberculosis screening prior to being ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on record review and staff interview it was determined the facility staff failed to address the pneumococcal vaccine with a Resident (#63). This was evident for 1 of 34 residents selected for re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0943
(Tag F0943)
Could have caused harm · This affected 1 resident
Based on a review of employee records it was determined that a staff member was allowed to work prior to receiving abuse training. This was true for 1 out 1 employee reviewed for allegations of abuse....
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected multiple residents
Based on medical record review and interview it was determined the facility staff failed to provide showers to Residents (#26 and #31). This was evident for 2 of 2 resident reviewed for choices during...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
2. On 6/12/19 at 9:04 AM, the care plan for Resident #8 was reviewed. The care plan is a document that outlines specific risks for a resident and provides information to staff to tailor care to the re...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected most or all residents
Based on surveyor observation and interview with staff it was determined that the facility failed to post the total number and the actual hours worked for Registered Nurses, Licensed Practical Nurses ...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0838
(Tag F0838)
Minor procedural issue · This affected most or all residents
Based on staff interview, it was determined that facility failed to conduct and document a facility-wide assessment to determine what resources are necessary to care for its residents competently duri...
Read full inspector narrative →
Mar 2018
3 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. A review of Resident #68's clinical record revealed that on 1/3/18 Resident #68 received a cut letter (The Notice of Medicare...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Resident #12
Based on staff interview and review of the medical record, it was determined the facility staff failed to accurately document a resident's functional status for Range of Motion (ROM) in t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with staff it was determined that the facility staff failed to have a policies and procedures in place for the medication regimen review (MRR). This was fo...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 43% turnover. Below Maryland's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: 4 harm violation(s), $28,343 in fines. Review inspection reports carefully.
- • 39 deficiencies on record, including 4 serious (caused harm) violations. Ask about corrective actions taken.
- • $28,343 in fines. Higher than 94% of Maryland facilities, suggesting repeated compliance issues.
- • Grade F (35/100). Below average facility with significant concerns.
About This Facility
What is Wicomico's CMS Rating?
CMS assigns WICOMICO NURSING HOME an overall rating of 3 out of 5 stars, which is considered average nationally. Within Maryland, this rating places the facility higher than 0% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Wicomico Staffed?
CMS rates WICOMICO NURSING HOME's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 43%, compared to the Maryland average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Wicomico?
State health inspectors documented 39 deficiencies at WICOMICO NURSING HOME during 2018 to 2025. These included: 4 that caused actual resident harm, 33 with potential for harm, and 2 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
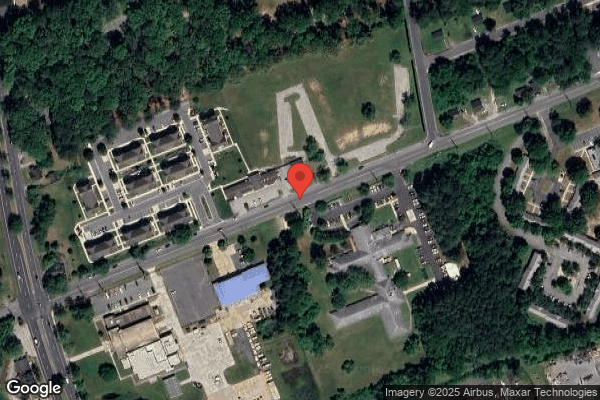
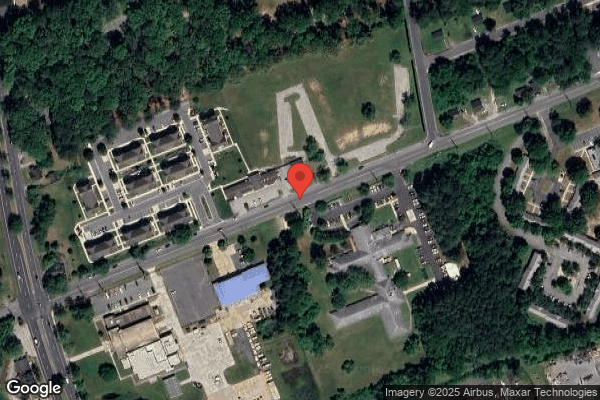
Who Owns and Operates Wicomico?
WICOMICO NURSING HOME is owned by a government entity. Government-operated facilities are typically run by state, county, or municipal agencies. The facility operates independently rather than as part of a larger chain. With 102 certified beds and approximately 63 residents (about 62% occupancy), it is a mid-sized facility located in SALISBURY, Maryland.
How Does Wicomico Compare to Other Maryland Nursing Homes?
Compared to the 100 nursing homes in Maryland, WICOMICO NURSING HOME's overall rating (3 stars) is below the state average of 3.0, staff turnover (43%) is near the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Wicomico?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Wicomico Safe?
Based on CMS inspection data, WICOMICO NURSING HOME has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #100 of 100 nursing homes in Maryland. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Wicomico Stick Around?
WICOMICO NURSING HOME has a staff turnover rate of 43%, which is about average for Maryland nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Wicomico Ever Fined?
WICOMICO NURSING HOME has been fined $28,343 across 1 penalty action. This is below the Maryland average of $33,362. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Wicomico on Any Federal Watch List?
WICOMICO NURSING HOME is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.