AYER VALLEY REHAB AND NURSING




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Ayer Valley Rehab and Nursing has received a Trust Grade of F, indicating significant concerns about the facility's quality of care. They rank #267 out of 338 facilities in Massachusetts, placing them in the bottom half, and #55 out of 72 in Middlesex County, meaning only a few local options are worse. Although the facility is reportedly improving, with the number of issues decreasing from 25 to 21, it still faces serious challenges, including a concerning staff turnover rate of 64%, which is much higher than the state average. The facility has also incurred $82,554 in fines, a figure that is higher than 81% of Massachusetts facilities, suggesting ongoing compliance problems. Specific incidents have raised alarm, such as the failure to notify medical staff about a resident's deteriorating pressure wound and an incident of staff abuse that left a resident visibly upset. While there is some RN coverage, it is only at an average level, which may not sufficiently protect residents from potential issues.
- Trust Score
- F
- In Massachusetts
- #267/338
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 64% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $82,554 in fines. Lower than most Massachusetts facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 40 minutes of Registered Nurse (RN) attention daily — about average for Massachusetts. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 84 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Massachusetts average (2.9)
Significant quality concerns identified by CMS
18pts above Massachusetts avg (46%)
Frequent staff changes - ask about care continuity
Well above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
16 points above Massachusetts average of 48%
The Ugly 84 deficiencies on record
Mar 2025
18 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, and interview, the facility failed to notify the Physician of a change in condition for one Resident (#1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, and interview, the facility failed to resolve a grievance timely for one Resident (#66), out of a total ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0694
(Tag F0694)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, and interview, the facility failed to provide care and services in accordance with professional standard...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0699
(Tag F0699)
Could have caused harm · This affected 1 resident
Based on interview, and record review, the facility failed to develop a comprehensive Trauma Informed Care Plan for one Resident (#2), out of a total sample of 23 residents.
Specifically, for Residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure that three Licensed Nurses (Nurse #3, ADON [As...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected 1 resident
Based on record review, and interview, the facility failed to complete a performance review at least once every 12 months for one Certified Nurses Aide (CNA) #2 out of a sample of five CNAs reviewed. ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on interview, and record review, the facility failed to ensure that one Resident (#104) out of a total sample of 23 residents, was free from a significant medication error when an anticoagulatio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide food and drink at a safe and appetizing temperature to residents on the North One Unit and for two Residents (#77 and...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide food that was designed to meet the individual...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0825
(Tag F0825)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, and interview, the facility failed to ensure that specialized rehabilitation services were provided to o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to maintain accurate medical records relative to the app...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to adhere to infection control standards of practice for two Residents (#44 and #75) out of a total sample of 23 residents, incr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to offer pneumococcal immunizations in accordance with Centers for Di...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to offer updated COVID-19 immunizations for three Residents (#45, #51...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Resident #12 was admitted to the facility in May 2022 with diagnoses including Dementia and COPD.
Review of Resident #12's Mi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0712
(Tag F0712)
Could have caused harm · This affected multiple residents
Based on interview, and record review, the facility failed to provide Physician visits at the required frequency for five Residents (#10, #28, #45, #51 and #68) for an applicable sample of six residen...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure that recommendations made by the Consultant Pharmacist duri...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0843
(Tag F0843)
Could have caused harm · This affected most or all residents
Based on record review, and interview, the facility failed to have in effect a written transfer agreement with one or more hospitals approved for participation under the Medicare and Medicaid programs...
Read full inspector narrative →
Jan 2025
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews, for three of three sampled residents (Resident #1, #2, and #3), the facility failed to ensure nursing notified the Physician, per facility policy, when all th...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews, for one of three sampled residents (Resident #3), the Facility failed to ensure nursing services provided met professional standards of quality related to obt...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on record reviewed and interviews, for three of three sampled residents (Resident #1, #2 and #3), who were assessed by nursing to be at risk for altered nutritional status which included the pot...
Read full inspector narrative →
Jun 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and records reviewed, for one of three sampled residents (Resident #3) who's comprehensive care...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on observations, interviews and records reviewed, for one of three nursing units (North 2), the Facility failed to ensure they provided and maintained a sufficient number of Certified Nurse Aide...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected multiple residents
Based on records reviewed and interviews, the Facility failed to ensure they implemented their Quality Assurance Performance Improvement (QAPI) plan of action to monitor, assess, and document the data...
Read full inspector narrative →
Mar 2024
22 deficiencies
2 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Notification of Changes
(Tag F0580)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, record and policy review, the facility failed to notify the Physician/Non Physician Practitione...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
Based on record and policy review, and interview, the facility failed to provide necessary pressure ulcer (PU: localized damage to the skin and/or underlying soft tissue usually over a bony prominence...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview the facility failed to respect the rights and ensure the dignified treatment of one Resident (#89) out of a total sample of 26 residents.
Specifical...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. Resident #46 was admitted to the facility in March 2022, with diagnoses of Dementia, Psychosis (a collection of symptoms that...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
Based on interview, policy and record review, the facility failed to re-submit a Level I Preadmission Screening and Resident Review (PASRR- is a federal requirement to help ensure that individuals are...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to develop a discharge plan for one Resident (#304) out of a sample of...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, record and policy review, the facility failed to ensure that activities of daily living (ADL's-...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, policy and record review, the facility failed to implement weight monitoring to maintain the nutritional sta...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0699
(Tag F0699)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, policy and record review, the facility failed to ensure that residents who are trauma survivors receive cult...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure that two Licensed Nurses (Nurse #2 and Unit Ma...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on record and policy review, and interview, the facility failed to ensure that recommendations made by the Consultant Pharmacist during a monthly Medication Regime Review (MRR) were reviewed by ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to monitor for side effects and adverse reactions to medications for one Resident (#25) out of a total sample of 26 residents.
Specifically, ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to schedule a follow-up dental appointment for one Resid...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0638
(Tag F0638)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to ensure timely completion as required of the Minimum Data Set (MDS) Assessments for 14 Residents (#93, #15, #56, #70, #73, #32, #55, #5, #47...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 9. Resident #46 was admitted to the facility in March 2022 with diagnoses of Dementia, Psychosis (a collection of symptoms that ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to maintain an environment that is free of accidents and...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on observation, record review and interview, the facility failed to provide sufficient staffing to coordinate and carry out resident care required on the North Two Unit.
Specifically, the facil...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to provide food and drink that was palatable, at a safe and appetizing temperature to residents on the North Two Unit.
Specific...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0868
(Tag F0868)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure the Quality Assessment and Performance Improvement (QAPI) committee meets at least quarterly and as needed to coordinate and evaluat...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on review of the facility's Licensed Nurse staff schedule and interviews, the facility failed to provide the services of a Registered Nurse (RN) for at least eight consecutive hours a day, seven...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on interview, record and policy review, the facility failed to implement an infection control and prevention program to provide a sanitary environment and help prevent the development and transm...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0625
(Tag F0625)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. Resident #46 was admitted to the facility in March 2022 with diagnoses including Dementia, Psychosis (a collection of symptom...
Read full inspector narrative →
Dec 2023
13 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
Based on observations, records reviewed, and interviews, for one of three sampled residents (Resident #3), who was cognitively impaired and wandered, the Facility failed to ensure they implemented a m...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews, for one of three sampled residents (Resident #1), the Facility failed to ensure nursing care met professional standards or practice, when on 12/25/23, Nurse #...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected 1 resident
Based on records reviewed, interviews, and observations, the Facility failed to ensure that meals prepared for and delivered to each resident, were served at an appropriate temperature.
Findings inclu...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, records reviewed, and interviews, for one of three resident care units (North 2 Unit), the facility faile...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
Based on records reviewed and interviews, for two of three sampled residents (Resident #1 and Resident #3) and 11 non-sampled residents (Non-Sampled Residents (NS-RT) #4, #5, #6, #7, #8, #9, #10, #11,...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
Based on observations, records reviewed, and interviews, for one of three sampled residents (Resident #1), who required extensive physical assistance to total dependence on staff to meet his/her care ...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected most or all residents
Based on observations, records reviewed, and interviews for one of three sampled residents (Resident #1) and one non-sampled resident (Non-Sampled Resident (NS-RT) #11, the facility failed to treat th...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected most or all residents
Based on observations, records reviewed, and interviews, for three of three nursing units (North 1 Unit, North 2 Unit, and South 2 Unit), the Facility failed to provide sufficient staffing to ensure t...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected most or all residents
Based on records reviewed and interviews, for three of three sampled residents (Resident #1, Resident #2, and Resident #3), the Facility failed to ensure they maintained complete and accurate medical ...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observations, records reviewed and interviews, the Facility failed to ensure it provided a sanitary environment in an effort to prevent contamination and transmission of infections.
Findings...
Read full inspector narrative →
MINOR
(C)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Minor Issue - procedural, no safety impact
Deficiency F0837
(Tag F0837)
Minor procedural issue · This affected most or all residents
Based on interview and license review, the facility failed to ensure the Administrator was licensed in Massachusetts, as required.
Findings include:
In an email to the Surveyor, dated 01/02/24, the R...
Read full inspector narrative →
MINOR
(C)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Minor Issue - procedural, no safety impact
Safe Environment
(Tag F0921)
Minor procedural issue · This affected most or all residents
Based on observations, records reviewed, and interviews, the Facility failed to ensure it provided a safe, functional, and sanitary environment, in the basement level of the Facility where laundry ser...
Read full inspector narrative →
MINOR
(C)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Minor Issue - procedural, no safety impact
Deficiency F0925
(Tag F0925)
Minor procedural issue · This affected most or all residents
Based on observations, records reviewed, and interviews, the Facility failed to ensure they maintained an effective pest control program, when from October 2023 to the end of December 2023, the baseme...
Read full inspector narrative →
Sept 2023
3 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
Based on records reviewed, review of facility surveillance camera video footage, and interviews, for one of three sampled residents (Resident #1), who had severe cognitive impairment and was dependent...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews, for one of three sampled residents (Resident #1), who had severe cognitive impairment,...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on records reviewed, review of surveillance camera video footage, and interviews. for one of three sampled residents (Resident #1), the Facility failed ensure medications were stored properly, w...
Read full inspector narrative →
Jul 2023
3 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0557
(Tag F0557)
A resident was harmed · This affected 1 resident
Based on records reviewed and interviews, for one of three sampled residents (Resident #1) who was cognitively intact, made his/her own decisions, who resided in a room where he/she occupied and enjoy...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0559
(Tag F0559)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews for one of three sampled residents (Resident #1), who was cognitively intact and made his/her own decisions, the Facility staff failed to ensure he/she was pro...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews, for one of three sampled residents (Resident #1) who was cognitively intact, made his/her own decisions and had allegedly been verbally abused by a staff memb...
Read full inspector narrative →
Apr 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews, for one of three sampled residents (Resident #1) who requested staff assistance with toileting care needs, the Facility failed to ensure he/she was treated in...
Read full inspector narrative →
Feb 2023
3 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on record review, policy review, and interview, the facility failed to ensure that its staff consistently assessed signs and symptoms of COVID-19 each shift per facility policy, during an outbre...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on record review, policy review, and interview, the facility failed to ensure that its staff implemented its policy to offer education and an updated Pneumococcal Conjugate Vaccine (PCV) to one ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
Based on record review, document review, and interview, the facility failed to ensure that its staff implemented the facility policy to obtain a Physician's order to administer a COVID-19 vaccine for ...
Read full inspector narrative →
Jun 2022
15 deficiencies
3 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Notification of Changes
(Tag F0580)
A resident was harmed · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure staff notified the physician of: (1) A change in the treatment plan, specifically a missed hemodialysis (procedure used...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
2. For Resident #69 the facility failed to ensure staff: (a) measured two pressure ulcers weekly, (b) provided the physician ordered wound care and (c) obtain wound care orders for a pressure ulcer on...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0698
(Tag F0698)
A resident was harmed · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure staff provided dialysis services; specifically, failed to (1) provide transportation to a dialysis treatment appointmen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility staff failed to obtain a physician's order for the treatment of an open wound for one Resident (#69) out of 23 sampled residents.
Findin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure the resident environment remained free of accident hazards, specifically related to storage of smoking materials, for o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview, the facility failed to ensure one Resident (#88) was assessed for risk of entrapment from bed rails, failed to ensure the risks and benefits of bed r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0740
(Tag F0740)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to provide individualized meaningful approaches relative to behavioral health care for one Resident (#13) out of 23 total sam...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview the facility failed to maintain an accurate medical record relative to the application of thrombo-embolic deterrent (TED; compression stockings used t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected 1 resident
Based on interview and review of facility audits and reports, the facility failed to develop a Quality Assurance Performance Improvement (QAPI) plan in a good faith effort to address the deficient pra...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to a offer one Resident (#91) a Covid-19 booster when eligible, out of a total of five sampled residents.
Findings include:
Review of the poli...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. For Resident #31 the facility staff failed to implement an individualized person-centered mood and psychotropic medication ca...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on observations, interviews, and record reviews, the facility failed to provide sufficient nurse staffing for two out of three days (7:00 A.M. - 3:00 P.M.) shifts, during the survey period, on t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to offer a pneumococcal immunization to two Residents (#55 and #93) and the influenza (flu) immunization (during the October 1, 2021 to March ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0886
(Tag F0886)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview the facility staff failed to: 1) perform COVID-19 outbreak testing for three Residents (#18...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observation, interview and document review the facility staff failed to maintain infection control standards to prevent the further spread of COVID-19 in the facility by ensuring all visitors...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 7 harm violation(s), $82,554 in fines. Review inspection reports carefully.
- • 84 deficiencies on record, including 7 serious (caused harm) violations. Ask about corrective actions taken.
- • $82,554 in fines. Extremely high, among the most fined facilities in Massachusetts. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Ayer Valley Rehab And Nursing's CMS Rating?
CMS assigns AYER VALLEY REHAB AND NURSING an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Massachusetts, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Ayer Valley Rehab And Nursing Staffed?
CMS rates AYER VALLEY REHAB AND NURSING's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 64%, which is 18 percentage points above the Massachusetts average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs. RN turnover specifically is 81%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Ayer Valley Rehab And Nursing?
State health inspectors documented 84 deficiencies at AYER VALLEY REHAB AND NURSING during 2022 to 2025. These included: 7 that caused actual resident harm, 73 with potential for harm, and 4 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
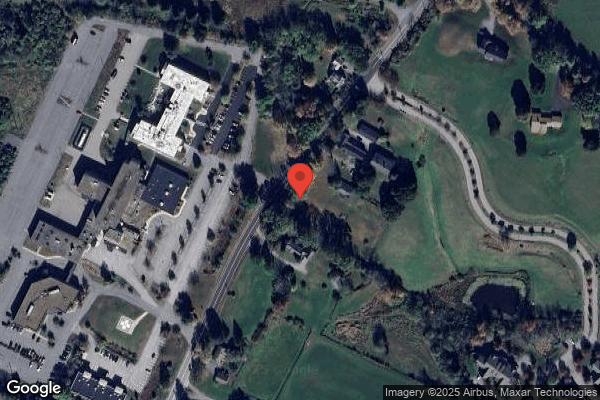
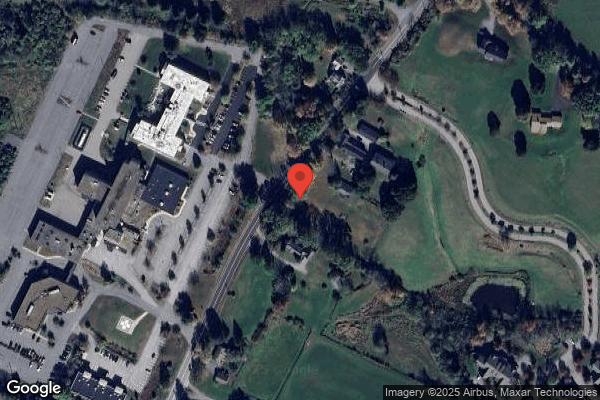
Who Owns and Operates Ayer Valley Rehab And Nursing?
AYER VALLEY REHAB AND NURSING is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by STERN CONSULTANTS, a chain that manages multiple nursing homes. With 123 certified beds and approximately 109 residents (about 89% occupancy), it is a mid-sized facility located in AYER, Massachusetts.
How Does Ayer Valley Rehab And Nursing Compare to Other Massachusetts Nursing Homes?
Compared to the 100 nursing homes in Massachusetts, AYER VALLEY REHAB AND NURSING's overall rating (1 stars) is below the state average of 2.9, staff turnover (64%) is significantly higher than the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Ayer Valley Rehab And Nursing?
Based on this facility's data, families visiting should ask: "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's high staff turnover rate and the below-average staffing rating.
Is Ayer Valley Rehab And Nursing Safe?
Based on CMS inspection data, AYER VALLEY REHAB AND NURSING has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Massachusetts. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Ayer Valley Rehab And Nursing Stick Around?
Staff turnover at AYER VALLEY REHAB AND NURSING is high. At 64%, the facility is 18 percentage points above the Massachusetts average of 46%. Registered Nurse turnover is particularly concerning at 81%. RNs handle complex medical decisions and coordinate care — frequent RN changes can directly impact care quality. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Ayer Valley Rehab And Nursing Ever Fined?
AYER VALLEY REHAB AND NURSING has been fined $82,554 across 4 penalty actions. This is above the Massachusetts average of $33,904. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Ayer Valley Rehab And Nursing on Any Federal Watch List?
AYER VALLEY REHAB AND NURSING is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.