RESERVOIR CENTER FOR HEALTH & REHABILITATION, THE




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
The Reservoir Center for Health & Rehabilitation has a Trust Grade of C, which means it is average and falls in the middle of the pack for nursing homes. It ranks #175 out of 338 facilities in Massachusetts, placing it in the bottom half, and #38 out of 72 in Middlesex County, indicating that there are better local options. Unfortunately, the facility's trend is worsening, with issues increasing from 7 in 2023 to 17 in 2024. Staffing is average with a rating of 3 out of 5 stars and a turnover rate of 42%, which is consistent with the state average, suggesting that staff stability is not a strong point. The facility has incurred $12,895 in fines, which is concerning, and they have average RN coverage that may not be sufficient to catch all potential problems. Specific incidents from inspections reveal that the facility failed to ensure adequate supervision for residents at risk of falls, leading to serious injuries, and there were issues with food safety, including unlabeled and expired items in the kitchen. Additionally, a staff member was observed not wearing the required eye protection while providing care to a resident, which could pose a risk of infection. While the facility does have some strengths, such as a decent quality measure rating of 4 out of 5 stars, the combination of increasing issues and specific safety concerns is something families should carefully consider.
- Trust Score
- C
- In Massachusetts
- #175/338
- Safety Record
- Moderate
- Inspections
- Getting Worse
- Staff Stability ○ Average
- 42% turnover. Near Massachusetts's 48% average. Typical for the industry.
- Penalties ✓ Good
- $12,895 in fines. Lower than most Massachusetts facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 34 minutes of Registered Nurse (RN) attention daily — about average for Massachusetts. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 40 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (42%)
6 points below Massachusetts average of 48%
Facility shows strength in quality measures, fire safety.
The Bad
Near Massachusetts average (2.9)
Meets federal standards, typical of most facilities
Near Massachusetts avg (46%)
Typical for the industry
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 40 deficiencies on record
Oct 2024
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews, for one of three sampled residents (Resident #1), who required hemodialysis (a life-saving treatment that filters waste products and excess fluid when the kid...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews, for two of three sampled residents, (Resident #1 and #2), the facility failed to ensur...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews, for one of three sampled residents (Resident #1), who required hemodialysis (a life-sa...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interviews for one of three sampled residents (Resident #1), who upon admission and then re-admissio...
Read full inspector narrative →
Oct 2024
13 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, interview, and policy review, the facility failed to provide a dignified dining experience for one Resident (#79), out of a total sample of 27 residents.
Specifically, the facili...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
2. Resident #79 was admitted to the facility in April of 2024 with diagnoses including Urinary Retention (difficulty urinating and completely emptying the bladder), and Obstructive and Reflux Uropathy...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on interview, record and policy review, the facility failed to ensure its staff implement the plan of care for one Resident (#75) relative to weight measurements, out of a total sample of 27 res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident #9 was admitted to the facility in July 2024, with diagnoses including Schizoaffective Disorder (chronic mental heal...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, policy and record review, the facility failed to develop and implement an effective discharge planning proce...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide care and services according to professional s...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide appropriate pain management for one Resident ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to provide services consistent with professional standards of practice relative to hemodialysis (a procedure where a machine wit...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0742
(Tag F0742)
Could have caused harm · This affected 1 resident
Based on interview, policy and record review, the facility failed to provide appropriate treatment and services to attain the highest practicable mental and psychosocial well-being for one Resident (#...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, policy and record review, the facility failed to ensure that one Resident (#84), out of a total sample of 27...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview, and policy review, the facility failed to remove expired medications from one medication cart, out of a sample of four medication carts.
Specifically, the facility fai...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. On 9/26/24 at 8:26 A.M., the surveyor observed CNA #2 enter a room with Droplet Precautions sign at the door, outlining the r...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0646
(Tag F0646)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy and record review, and interview, the facility failed to notify the state mental health authority for a resident...
Read full inspector narrative →
Jul 2023
3 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on record review, policy review and interview, the facility failed to provide care and services consistent with professional standards for one Resident (#51) who required renal dialysis (a life ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, policy review and interview, the facility failed to ensure that all medications were properly stored and labeled in accordance with currently accepted professional principles and...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on inspection and interview, the facility failed to label, date and maintain food products that were not expired, in four out of four Unit Nourishment kitchenettes.
Findings include:
Review of t...
Read full inspector narrative →
Jan 2023
4 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on document review and interview, the facility failed to ensure that its staff assessed signs and symptoms of COVID-19 for one out of 3 sampled Residents at the appropriate frequency, when the f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, record review, and interview, the facility failed to ensure that its staff offered the appropriate pneum...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0886
(Tag F0886)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure its staff conducted COVID-19 testing for residents and staff as required. Specifically, the facility failed to ensure that its staff...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0885
(Tag F0885)
Could have caused harm · This affected multiple residents
Based on document review, and interview, the facility failed to ensure that its staff notified Residents, families, or Resident Representatives of COVID-19 positive staff and resident cases in the fac...
Read full inspector narrative →
Oct 2021
16 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on observation, record review, and interview, the facility failed to provide adequate supervision and develop or implement effective fall prevention interventions for two Residents (#116 and #35...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure the interdisciplinary team determined one Resident (#86) was safe and clinically appropriate to self-administer medica...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
Based on record review, observation, and interview, the facility failed to document ongoing re-evaluation for the need of restraints for one Resident (#67), out of a total of 24 sampled residents.
Fi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to provide the adequate assistance related to eating for two Residents (#105 and #120), out of 24 sampled residents.
Findings i...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
2. For Resident #81 the facility failed to provide an activity program based on the Resident's preference.
Resident #81 was admitted to the facility in June 2021.
Review of the MDS assessment, dated...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to assess and provide appropriate services related to urinary incontinence for one Resident (#35) and failed to provide appropri...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, record review, observation, and interview, the facility failed to provide an ongoing evaluation of risks...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
2. Resident #67 was admitted to the facility in October 2019 with diagnoses including vascular dementia with behavioral disturbance and anxiety disorder.
Review of a Physician's Order, dated 2/26/21,...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure a psychotropic medication (chemical that changes brain function and results in alteration in perception, mood, consciousness, cognit...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0882
(Tag F0882)
Could have caused harm · This affected 1 resident
Based on the Quality Assurance and Performance Improvement (QAPI) quarterly attendance records and interview, the facility failed to ensure the Infection Preventionist (IP) was present at the QAPI mee...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
Based on smoking schedule review, observation, and interview, the facility
1) Failed to ensure two Residents (#35 and #57) were able to exercise their right to smoke regularly, and
2) Failed to provi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
3. For Resident #107, the facility failed to follow a physician's order related to a behavioral intervention.
Resident #107 was admitted to the facility in July 2019 with diagnoses including Alzheimer...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility
1) Failed to ensure all staff were vaccinated against COVID-19 per the facility's policy;
2) Failed to ensure staff wore appropriate P...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
2. Resident #116 was admitted to the facility in October 2020.
Review of an immunization consent form, dated 10/6/20, indicated Resident #116's representative consented to administration of the pneumo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0886
(Tag F0886)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to ensure that all unvaccinated staff were BinaxNOW (a rapid test) tested for COVID-19 prior to every shift as required for 6 out of 8 sampled...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0909
(Tag F0909)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to ensure regular inspection of all bed frames, mattresses and bed rails to identify any areas of possible entrapment on 2 out of 2 units.
Fi...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 42% turnover. Below Massachusetts's 48% average. Good staff retention means consistent care.
- • 40 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • $12,895 in fines. Above average for Massachusetts. Some compliance problems on record.
- • Grade C (53/100). Below average facility with significant concerns.
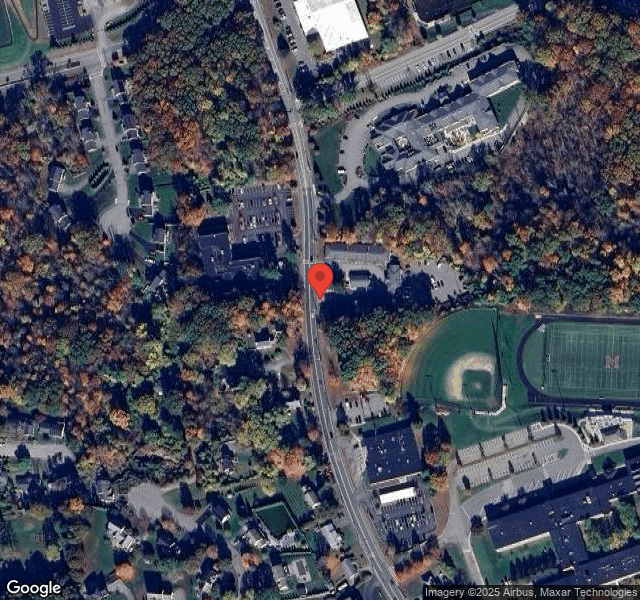
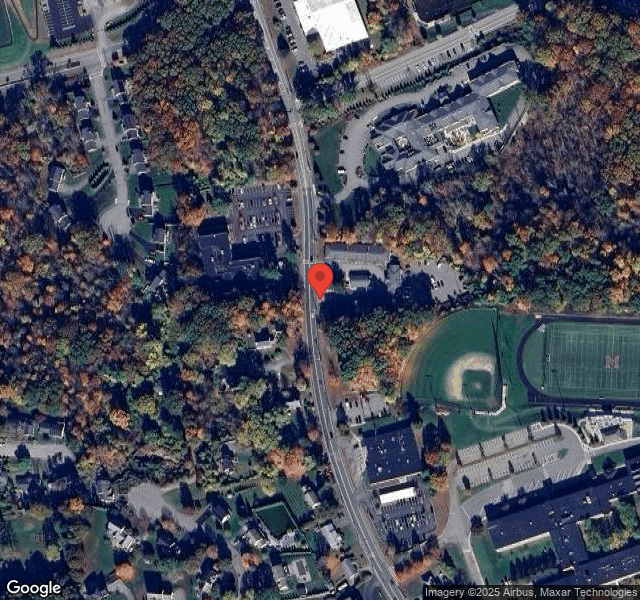
About This Facility
What is Reservoir Center For Health & Rehabilitation, The's CMS Rating?
CMS assigns RESERVOIR CENTER FOR HEALTH & REHABILITATION, THE an overall rating of 3 out of 5 stars, which is considered average nationally. Within Massachusetts, this rating places the facility higher than 99% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Reservoir Center For Health & Rehabilitation, The Staffed?
CMS rates RESERVOIR CENTER FOR HEALTH & REHABILITATION, THE's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 42%, compared to the Massachusetts average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Reservoir Center For Health & Rehabilitation, The?
State health inspectors documented 40 deficiencies at RESERVOIR CENTER FOR HEALTH & REHABILITATION, THE during 2021 to 2024. These included: 1 that caused actual resident harm, 38 with potential for harm, and 1 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Reservoir Center For Health & Rehabilitation, The?
RESERVOIR CENTER FOR HEALTH & REHABILITATION, THE is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by NATIONAL HEALTH CARE ASSOCIATES, a chain that manages multiple nursing homes. With 144 certified beds and approximately 133 residents (about 92% occupancy), it is a mid-sized facility located in MARLBOROUGH, Massachusetts.
How Does Reservoir Center For Health & Rehabilitation, The Compare to Other Massachusetts Nursing Homes?
Compared to the 100 nursing homes in Massachusetts, RESERVOIR CENTER FOR HEALTH & REHABILITATION, THE's overall rating (3 stars) is above the state average of 2.9, staff turnover (42%) is near the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Reservoir Center For Health & Rehabilitation, The?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Reservoir Center For Health & Rehabilitation, The Safe?
Based on CMS inspection data, RESERVOIR CENTER FOR HEALTH & REHABILITATION, THE has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #1 of 100 nursing homes in Massachusetts. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Reservoir Center For Health & Rehabilitation, The Stick Around?
RESERVOIR CENTER FOR HEALTH & REHABILITATION, THE has a staff turnover rate of 42%, which is about average for Massachusetts nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Reservoir Center For Health & Rehabilitation, The Ever Fined?
RESERVOIR CENTER FOR HEALTH & REHABILITATION, THE has been fined $12,895 across 2 penalty actions. This is below the Massachusetts average of $33,208. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Reservoir Center For Health & Rehabilitation, The on Any Federal Watch List?
RESERVOIR CENTER FOR HEALTH & REHABILITATION, THE is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.