WINDSOR NURSING & RETIREMENT HOME
Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Windsor Nursing & Retirement Home has received a Trust Grade of F, indicating significant concerns about its quality of care. It ranks #337 out of 338 facilities in Massachusetts, placing it in the bottom tier of nursing homes in the state, and #15 out of 15 in Barnstable County, meaning there are no better local options. While the facility's trend shows improvement, moving from 13 issues in 2023 to 8 in 2025, it still struggles with serious staffing challenges, having a high turnover rate of 56%, which is above the state average of 39%. Additionally, the home has faced some concerning incidents, such as a resident developing pressure ulcers due to inadequate care and two residents being hospitalized for infected wounds with maggots. On a positive note, the nursing home has average RN coverage, which can help catch potential issues early. However, the combination of weaknesses and serious incidents makes it crucial for families to consider other options carefully.
- Trust Score
- F
- In Massachusetts
- #337/338
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 56% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $15,636 in fines. Lower than most Massachusetts facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 38 minutes of Registered Nurse (RN) attention daily — about average for Massachusetts. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 42 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Massachusetts average (2.9)
Significant quality concerns identified by CMS
Near Massachusetts avg (46%)
Frequent staff changes - ask about care continuity
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
8 points above Massachusetts average of 48%
The Ugly 42 deficiencies on record
Jan 2025
8 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to initiate the grievance process on behalf of one Resident (#76), out of a total sample of 19 residents. Specifically, for Resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on record review, interview, and observation, the facility failed to follow professional standards of practice for one Resident (#197), out of a total sample of 19 residents. Specifically, the f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, and interview, the facility failed to ensure post-fall interventions were developed and im...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to ensure residents in two of three dining rooms had a comfortable and homelike dining experience.
Findings include:
During dining observations...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure audiology services were offered to ensure the highest practicable level of care for one Resident (#76), out of a total...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview, and document review, the facility failed to ensure all medications used in the facility were stored and labeled in accordance with currently accepted professional stan...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to follow professional standards of practice for food safety and sanitation to prevent the potential spread of foodborne illness to residents wh...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to ensure an accurate medical record for one Resident (#84), out of a total sample of 19 residents. Specifically, the facility failed to ensur...
Read full inspector narrative →
Oct 2023
10 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, policy review, observation, and interview, the facility failed for one Resident (#88), out of a total sa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure that individualized, resident-centered, comprehensive care plans were developed and consistently implemented for one Resident (#32),...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview, and policy review, the facility failed for two Residents (#82 and #302) to ensure respiratory equipment and tubing was managed and stored in a sanitary way to prevent ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on policy review, interview, and record review, the facility failed to ensure for one Resident (#17), of one resident receiving hemodialysis, that treatment, care and services were consistent wi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0849
(Tag F0849)
Could have caused harm · This affected 1 resident
Based on record review, hospice contract review, and staff interview, the facility failed to ensure for one Resident (#44), out of a total sample of 19 residents, that hospice services were provided i...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected multiple residents
Based on interviews, policy review, and review of Resident Council Minutes, the facility failed to ensure that grievances brought forward through Resident Council from 4/27/23 through 9/26/23 were add...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected multiple residents
2. Resident #88 was admitted to the facility in September 2023 with diagnoses including: COVID-19, urinary tract infection, and hypertension (high blood pressure).
During an interview on 10/5/23 at 11...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected multiple residents
Based on record review, observations, policy review, and interviews, the facility failed to assist one Resident (#43) and their family, out of a total sample of 19 residents, in sourcing a replacement...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Transfer Notice
(Tag F0623)
Minor procedural issue · This affected multiple residents
Based on record review, policy review, and interview, the facility failed to ensure written notice for transfer and discharge was provided to Residents and/or Resident Representatives prior to hospita...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0625
(Tag F0625)
Minor procedural issue · This affected multiple residents
Based on policy review, record review, and interview, the facility failed to provide written notification of the bed hold policy to the Resident or Resident Representative prior to discharge to the ho...
Read full inspector narrative →
Jun 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews for two of three sampled Employee Personnel Records (Nurse #1 and Certified Nurse Aide # 2), the Facility failed to ensure they implemented and followed their ...
Read full inspector narrative →
Mar 2023
2 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview, and policy review, the facility failed to establish and maintain an infection prevention and control program designed to provide a safe, sanitary, and comfortable envi...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0886
(Tag F0886)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to ensure staff conducted testing and specimen collect...
Read full inspector narrative →
Apr 2021
21 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0658
(Tag F0658)
A resident was harmed · This affected 1 resident
Based on record review and staff interview, the facility failed to ensure that for two Residents (#16, #45), from a total sample of 31 residents, that staff provided care and treatment in accordance w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure that residents and/or their representatives were fully informed in advance, and given information necessary to make health care deci...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on policy review, observation, record review, and resident and staff interviews, the facility failed to ensure that the interdisciplinary team assessed residents for safe self-administration of ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on policy review, grievance log review, employee record review, and resident and staff interviews, the facility failed to ensure that staff:
1) implemented written policies and procedures for al...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on policy review, grievance review, and interviews, the facility failed to ensure that staff reported to the Department of Public Health (DPH) immediately, but not later than 24 hours, allegatio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on policy review, grievance documentation review, and staff interview, the facility failed to ensure that staff thoroughly investigated and reported to the Department of Public Health (DPH) alle...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
2) Resident #185 was admitted to the facility in March 2021 with diagnoses including diabetes mellitus type II, epilepsy with recurrent seizures, muscle contractures, and dysphagia (difficulty swallow...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on policy review, observation, resident and staff interview, and record review, the facility failed to ensure that staff developed and implemented a comprehensive person-centered care plan for t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0687
(Tag F0687)
Could have caused harm · This affected 1 resident
Based on policy review, record review, observation, and resident and staff interview, the facility failed to ensure that for one Resident (#47), of a total sample of 31 residents, that foot care and a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, record review, resident and staff interview, the facility failed to ensure staff provided the necessary respiratory care and services for one Resident (#47), out of a total sampl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure staff adhered to standards of practice for a Resident receiving dialysis services, including physician's orders for the provision of...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
2. Resident #69 was admitted to the facility in November 2019 with medical diagnoses including Bipolar disorder, post-traumatic stress disorder, anxiety disorder unspecified, restlessness, and agitati...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Laboratory Services
(Tag F0770)
Could have caused harm · This affected 1 resident
Based on record review and observation, the facility failed to ensure that staff ordered a laboratory draw for a Valproic Acid level for Resident #69 as ordered. Valproic Acid levels are taken to meas...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected multiple residents
Based on policy review, grievance book review, and resident and staff interview, the facility failed to ensure that:
a) staff addressed and promptly resolved 13 of 15 resident grievances, and
b) staf...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
Based on observation and interviews, the facility failed to ensure that residents were provided an environment that was free from accident hazards on two of two units, and for two Residents (#10, #16)...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on observation, policy review, and staff interview, the facility failed to provide pharmaceutical services to meets the needs of its residents by ensuring emergency insulin (regulates the amount...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on policy review, observation, and staff interview, the facility failed to ensure staff properly stored and secured medications, including a Schedule II drug (high potential for abuse) for one R...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected most or all residents
Based on resident and staff interviews, policy review, and review of Resident Council Minutes and the grievance book, the facility failed to ensure that grievances brought forward through Resident Cou...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected most or all residents
Based on documentation review and staff interview, the facility failed to ensure staff accurately assessed the facility resources needed to provide competent support and care for their resident popula...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. The facility failed to ensure staff implemented a system of surveillance that included a dated facility risk assessment, test...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected most or all residents
Based on record review and staff interview, the facility failed to develop an antibiotic stewardship program that promoted the appropriate use of antibiotics and included a system of monitoring to imp...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • 42 deficiencies on record, including 2 serious (caused harm) violations. Ask about corrective actions taken.
- • $15,636 in fines. Above average for Massachusetts. Some compliance problems on record.
- • Grade F (23/100). Below average facility with significant concerns.
- • 56% turnover. Above average. Higher turnover means staff may not know residents' routines.
About This Facility
What is Windsor Nursing & Retirement Home's CMS Rating?
CMS assigns WINDSOR NURSING & RETIREMENT HOME an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Massachusetts, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Windsor Nursing & Retirement Home Staffed?
CMS rates WINDSOR NURSING & RETIREMENT HOME's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 56%, which is 10 percentage points above the Massachusetts average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs. RN turnover specifically is 57%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Windsor Nursing & Retirement Home?
State health inspectors documented 42 deficiencies at WINDSOR NURSING & RETIREMENT HOME during 2021 to 2025. These included: 2 that caused actual resident harm, 38 with potential for harm, and 2 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Windsor Nursing & Retirement Home?
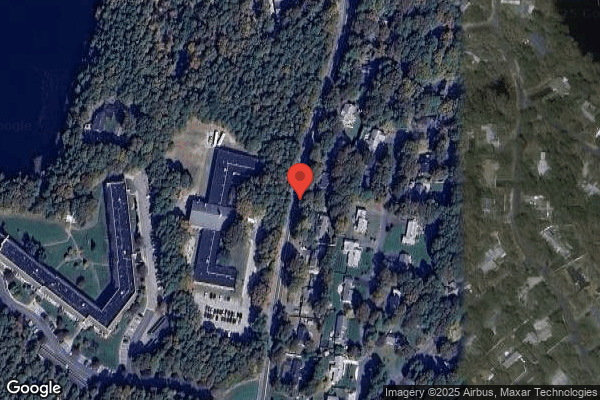
WINDSOR NURSING & RETIREMENT HOME is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility is operated by INTEGRITUS HEALTHCARE, a chain that manages multiple nursing homes. With 120 certified beds and approximately 92 residents (about 77% occupancy), it is a mid-sized facility located in SOUTH YARMOUTH, Massachusetts.
How Does Windsor Nursing & Retirement Home Compare to Other Massachusetts Nursing Homes?
Compared to the 100 nursing homes in Massachusetts, WINDSOR NURSING & RETIREMENT HOME's overall rating (1 stars) is below the state average of 2.9, staff turnover (56%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Windsor Nursing & Retirement Home?
Based on this facility's data, families visiting should ask: "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's high staff turnover rate and the below-average staffing rating.
Is Windsor Nursing & Retirement Home Safe?
Based on CMS inspection data, WINDSOR NURSING & RETIREMENT HOME has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Massachusetts. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Windsor Nursing & Retirement Home Stick Around?
Staff turnover at WINDSOR NURSING & RETIREMENT HOME is high. At 56%, the facility is 10 percentage points above the Massachusetts average of 46%. Registered Nurse turnover is particularly concerning at 57%. RNs handle complex medical decisions and coordinate care — frequent RN changes can directly impact care quality. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Windsor Nursing & Retirement Home Ever Fined?
WINDSOR NURSING & RETIREMENT HOME has been fined $15,636 across 2 penalty actions. This is below the Massachusetts average of $33,235. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Windsor Nursing & Retirement Home on Any Federal Watch List?
WINDSOR NURSING & RETIREMENT HOME is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.