MARISTHILL NURSING & REHABILITATION CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Maristhill Nursing & Rehabilitation Center has a Trust Grade of D, indicating below-average performance with some significant concerns. The facility ranks #225 out of 338 in Massachusetts, placing it in the bottom half of nursing homes in the state, and #44 out of 72 in Middlesex County, which means there are only a few local options that are better. While the staffing situation is a strength, with a 4 out of 5-star rating and a turnover rate of 34% that is below the state average, the overall quality of care is troubling, as shown by the 45 total issues found during inspections, including serious concerns where a resident suffered a second-degree burn from an electric curling iron. Additionally, there have been concerns regarding sanitation practices, such as improper food handling that could lead to illness. Despite these weaknesses, the facility shows a trend of improvement, reducing serious issues from 13 in 2024 to just 1 in 2025, and they have more registered nurse coverage than 96% of Massachusetts facilities, which is a positive aspect for resident safety and care.
- Trust Score
- D
- In Massachusetts
- #225/338
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ○ Average
- 34% turnover. Near Massachusetts's 48% average. Typical for the industry.
- Penalties ✓ Good
- $9,110 in fines. Lower than most Massachusetts facilities. Relatively clean record.
- Skilled Nurses ✓ Good
- Each resident gets 61 minutes of Registered Nurse (RN) attention daily — more than 97% of Massachusetts nursing homes. RNs are the most trained staff who catch health problems before they become serious.
- Violations ⚠ Watch
- 45 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (34%)
14 points below Massachusetts average of 48%
Facility shows strength in staffing levels, fire safety.
The Bad
Below Massachusetts average (2.9)
Below average - review inspection findings carefully
12pts below Massachusetts avg (46%)
Typical for the industry
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 45 deficiencies on record
Feb 2025
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews, for one of three sampled residents, (Resident #1), who required assistance from staff ...
Read full inspector narrative →
Oct 2024
13 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, policy review and interviews, the facility failed to report allegations of abuse to the state agency wit...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, policy review and interview, the facility failed to accurately complete a Level 1 Preadmission Screening...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observations, record review and interviews, the facility failed to ensure a comprehensive resident centered care plan was developed for one Resident (#63) out of a total sample of 22 Resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and interview, the facility failed to provide services that met professional standards of pr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observations, record review and interviews, the facility failed to provide assistance with Activities of Daily Living (ADLs) for dependent residents for one Resident (#1) out of a total sampl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and interview the facility failed to ensure standards of quality of care were implemented fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
Based on observation, interview, record review, the facility failed to ensure a resident received proper treatment to maintain hearing and ensure assistive devices to maintain hearing and enhance comm...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review and interviews the facility failed to ensure a resident who required respiratory care (cont...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0699
(Tag F0699)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure a plan of care was developed for Trauma-Informed Care for on...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and interview the facility failed to maintain an accurate medical record for two Residents (...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, the facility failed to assess for eligibility, and offer pneumococcal vaccinations per th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Resident #55 was admitted to the facility in July 2024 with diagnoses including dementia, pressure ulcer of the buttock.
Revi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to ensure staff followed proper sanitation and food handling practices to prevent the outbreak of foodborne illness.
Review of the facility pol...
Read full inspector narrative →
Oct 2023
17 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation and interview the facility failed to provide a dignified dining experience for one Resident (#19) out of a total sample of 21 residents.
Findings include:
Resident #19 was admitte...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
Based on observations, record review and interview the facility failed to ensure, for one Resident (#77), was free from the use of a restraint, out of a total sample of 21 residents.
Findings include...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to complete a Significant Change in Status Minimum Data Set (MDS) asse...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on record review, and interview, the facility failed to meet professional standards of quality for three Residents (#18, #1 and #55), out of a total sample of 21 residents. Specifically:
1. For ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, record review and policy review the facility failed to ensure quality care was provided for two...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3.) For Resident #19, a Resident at high risk for developing pressure ulcers, the facility failed to:
a.) apply bunny boots as o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview, the facility failed to follow the plan of care for an indwelling urinary catheter/Foley (a flexible tube that passes through the urethra and into the...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview the facility failed to develop and implement a plan of care and maintain oxyg...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, interview and observation, the facility failed to: assess for the use of an installed bed rail, obtain i...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview, the facility failed to ensure a licensed Registered Nurse (RN) had the appropriate competency and skill set to provide the necessary care and treatme...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to ensure that the pharmacy recommendations were addressed by the attending physician for one Resident (#53), out of 21 sampled resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on records reviewed, policy review, and interviews, the facility failed to ensure that as needed (PRN) orders for psychotropic medications are limited to 14 days unless the prescribing practitio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
2. On 9/29/23 at 9:40 A.M., the surveyor observed two plastic storage containers, containing 5 vials of insulin, 4 flex pen insulin, and one plastic storage container, containing lancets (a small, sha...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on observations, record reviews and interviews, the facility failed to maintain accurate medical records for three Residents (#84, #19 and #44) out of a total sample of 21 Residents. Specificall...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview the facility failed to adhere to standards of practice to prevent the spread of potential infection on two of three resident care units. Specifically,...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on record review, policy review, and interview the facility failed to ensure that residents were provided education on the pneumococcal vaccine, were assessed for the eligibility for the adminis...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
2) During an observation of the meal service on the C unit the following was observed:
-On 10/2/23 at 12:45 P.M., Diet Aide (DA) #1 had gloved hands and used utensils for serving food from the steam ...
Read full inspector narrative →
Sept 2022
14 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and policy review, the facility failed to report an abuse allegation within 2 hours as required ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. For Resident #78 the facility failed to investigate a skin tear of unknown origin.
Findings include:
Review of facility polic...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to provide one Resident (#46), out of a total sample of 19 residents, ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to provide written notification of the bed hold policy for 1 Resident ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to follow physician orders for 3 Residents (#4, #74, and #...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview the facility failed to ensure professional standards of practice were adhered to, for two Residents (#44 and #50.). Specifically, the facility failed ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview the facility failed to ensure the necessary services to carry out activities of daily living, specifically, removal of facial hair, was provided to tw...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to thoroughly investigate bruising for 1 Resident (#19) ou...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. For Resident #74 the facility failed to store nebulizer equipment in a dated/labeled bag.
Resident # 74 was admitted on [DATE...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on record review and interview the facility failed to ensure recommendations made by the consulting pharmacist from the monthly medication regimen reviews were acknowledged and addressed for two...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2.) For Resident #78 the facility failed to accurately document the presence a pressure ulcer.
Review of the facility policy ti...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview the facility failed to adhere to standards of infection control on one of three resident units. Specifically, Nurse #3 used shared resident equipment ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident # 66 was admitted to the facility in August 2022 with diagnoses including disruption of wound, malignant neoplasm of...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview and policy review, the facility 1) failed to ensure food items were dated and labeled in accordance with facility policy in the main kitchen and on 2 of 3 kitchenettes ...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 34% turnover. Below Massachusetts's 48% average. Good staff retention means consistent care.
- • 45 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • Grade D (43/100). Below average facility with significant concerns.
About This Facility
What is Maristhill Nursing & Rehabilitation Center's CMS Rating?
CMS assigns MARISTHILL NURSING & REHABILITATION CENTER an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Massachusetts, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Maristhill Nursing & Rehabilitation Center Staffed?
CMS rates MARISTHILL NURSING & REHABILITATION CENTER's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 34%, compared to the Massachusetts average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Maristhill Nursing & Rehabilitation Center?
State health inspectors documented 45 deficiencies at MARISTHILL NURSING & REHABILITATION CENTER during 2022 to 2025. These included: 1 that caused actual resident harm and 44 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Maristhill Nursing & Rehabilitation Center?
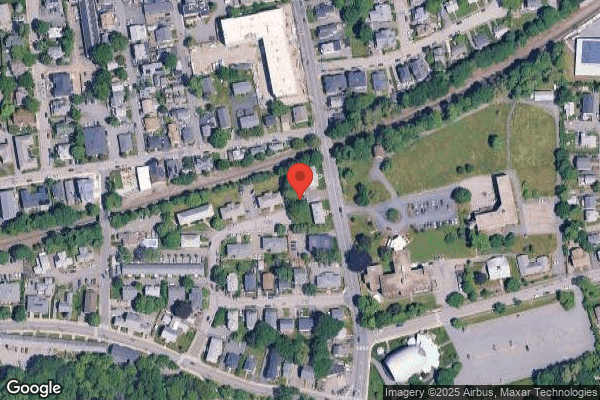
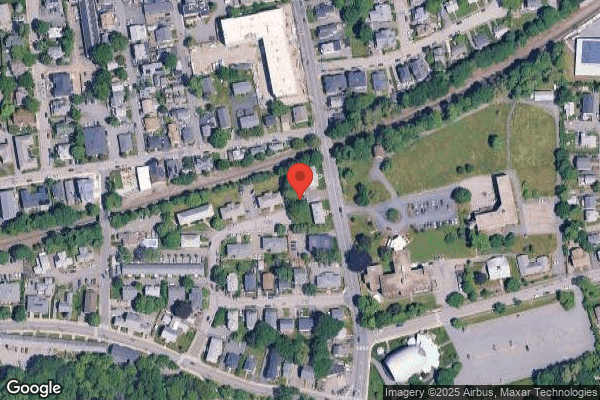
MARISTHILL NURSING & REHABILITATION CENTER is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility is operated by COVENANT HEALTH, a chain that manages multiple nursing homes. With 123 certified beds and approximately 91 residents (about 74% occupancy), it is a mid-sized facility located in WALTHAM, Massachusetts.
How Does Maristhill Nursing & Rehabilitation Center Compare to Other Massachusetts Nursing Homes?
Compared to the 100 nursing homes in Massachusetts, MARISTHILL NURSING & REHABILITATION CENTER's overall rating (2 stars) is below the state average of 2.9, staff turnover (34%) is significantly lower than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Maristhill Nursing & Rehabilitation Center?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Maristhill Nursing & Rehabilitation Center Safe?
Based on CMS inspection data, MARISTHILL NURSING & REHABILITATION CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Massachusetts. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Maristhill Nursing & Rehabilitation Center Stick Around?
MARISTHILL NURSING & REHABILITATION CENTER has a staff turnover rate of 34%, which is about average for Massachusetts nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Maristhill Nursing & Rehabilitation Center Ever Fined?
MARISTHILL NURSING & REHABILITATION CENTER has been fined $9,110 across 1 penalty action. This is below the Massachusetts average of $33,170. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Maristhill Nursing & Rehabilitation Center on Any Federal Watch List?
MARISTHILL NURSING & REHABILITATION CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.