WEST NEWTON HEALTHCARE




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
West Newton Healthcare has received a Trust Grade of F, indicating significant concerns and poor quality care. It ranks #334 out of 338 facilities in Massachusetts, placing it in the bottom half of nursing homes in the state, and #71 out of 72 in Middlesex County, meaning there is only one local option that performs worse. Despite an improving trend in issues reported, dropping from 43 in 2024 to 24 in 2025, the facility still faces serious challenges, including a concerning staffing turnover rate of 70%, which is well above the state average. Additionally, the facility has incurred fines totaling $227,924, which is higher than 94% of Massachusetts facilities, suggesting ongoing compliance issues. Specific incidents include failing to follow physician orders for pressure ulcer prevention, resulting in serious injuries for a resident, and not alerting a physician in time about a resident's serious health changes, leading to hospitalization. Overall, while there is some improvement in the number of issues, the facility has significant weaknesses that families should consider carefully.
- Trust Score
- F
- In Massachusetts
- #334/338
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 70% turnover. Very high, 22 points above average. Constant new faces learning your loved one's needs.
- Penalties ✓ Good
- $227,924 in fines. Lower than most Massachusetts facilities. Relatively clean record.
- Skilled Nurses ✓ Good
- Each resident gets 48 minutes of Registered Nurse (RN) attention daily — more than average for Massachusetts. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 91 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Massachusetts average (2.9)
Significant quality concerns identified by CMS
24pts above Massachusetts avg (46%)
Frequent staff changes - ask about care continuity
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
22 points above Massachusetts average of 48%
The Ugly 91 deficiencies on record
Jan 2025
24 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview, the facility failed file a grievance for one Resident (#7), out of a total sample of 24 residents.
Specifically, the facility staff failed to ensure...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record review, the facility failed to identify and assess the use of an abdominal binder as a potential restraint for one Resident (#74) out of a total sample of...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure that Minimum Data Set (MDS) assessments were coded accurately for one Resident (#26) out of a total sample of 24 Residents. Specific...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
3. For Resident #24 the facility failed to develop a care plan for the use of antidepressant and anti-anxiety medication.
Resident #24 was admitted to the facility in November 2023 with diagnoses incl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record review the facility failed to ensure care plans were reviewed with the interdisciplinary team (IDT) as required for two Residents (#35 and #61) out of a t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview the facility failed to ensure vision services were provided for one Resident (#6) out of a total sample of 24 residents. Specifically, the facility fa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure nursing implemented interventions for pressure ulcer care for one Resident (#61) out of a total sample of 24 Residents...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to consistently provide range of motion (ROM) care and t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to maintain acceptable parameters of nutritional status for one Resident (#88) out of a total sample of 24 residents. Specifically, for Reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observations, interview, and record review, the facility failed to ensure that respiratory care and services consistent with professional standards of practice, were provided for one Resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0699
(Tag F0699)
Could have caused harm · This affected 1 resident
3. Resident #78 was admitted to the facility in December 2024 with diagnoses that include assault by unspecified means, post traumatic stress disorder (PTSD) and anxiety disorder.
Review of the most r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview the facility failed to ensure that bilateral side rails were implemented in accordance with the care plan, for one Resident (#74) out of a total sampl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observations, record review, and interviews, the facility failed to ensure it was free from a medication error rate of greater than 5% when one out of four nurses observed made 10 errors out ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation and interview the facility failed to ensure drugs and biologicals were stored in accordance with accepted professional standards of practice. Specifically:
1. A medication nurse g...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
Based on observations, interviews and record reviews, the facility failed to provide dental services for one Resident (#85) out of a total sample of 24 residents.
Findings include:
Review of the poli...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview the facility failed to ensure accuracy of the medical record for two Residents (#90 and #88) out of a total sample of 24 residents. Specifically:
1. F...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
3b. On 1/7/25 at 12:22 P.M., the surveyor observed a Certified Nursing Assistant (CNA) sitting on the arm of a chair while assisting a resident to eat in the second floor dining room.
During an interv...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
Based on observation, record review and interview, the facility failed to meet professional standards of practice for three Residents (#14, #35 and #74) out of a total of sample of 24 residents. Speci...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
Based on observation, record review and interview the facility failed to ensure assistance with Activities of Daily Living (ADLs) were provided to three Residents (#23, #5, and #7) out of a total samp...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Laboratory Services
(Tag F0770)
Could have caused harm · This affected multiple residents
Based on record review and interviews, the facility failed to ensure laboratory services were provided for one Resident (#7) out of a sample of 24 Residents. Specifically, the facility failed to ensur...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observations and interviews, the facility failed to adhere to safe food practices to prevent contamination of food and beverage items intended for resident consumption in the facility's main ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, record review and interview the facility failed to establish and maintain an infection prevention and control program designed to provide a safe, sanitary and comfortable environ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0909
(Tag F0909)
Could have caused harm · This affected multiple residents
Based on observation, record review and interview, the facility failed identify and minimize areas of possible entrapment in resident beds. Specifically for Resident #74, out of a total of 24 sampled ...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected multiple residents
Based on observations and interviews, the facility failed to post nursing staff data daily, at the start of each shift, as required.
Findings include:
On 1/6/25 at 6:47 A.M., and at 5:00 P.M., and on...
Read full inspector narrative →
Feb 2024
43 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record reviews and interviews, the facility failed to ensure physician's orders were followed for prevent...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Resident #35 was admitted in June 2014 with diagnoses including hypertension and cognitive impairment.
Review of the Minimum...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to 1. complete admission consents and 2. invoke the health care proxy ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation, record review and interviews, the facility failed to ensure one Resident (#2C) had a physician order in place and was assessed for the ability to self-administer medications inde...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and interview the facility failed to 1. Ensure resident wheelchairs were maintained in a saf...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to file a grievance for one Resident (#72) out of a total sample of 40...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to ensure podiatry services were offered and toenails we...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, policy review, and interview, the facility failed to complete a Level I Preadmission Screening and Resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record record review and interview the facility failed to create a baseline plan of care within the required 48 hours o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to update the falls care plan with appropriate interventions to preven...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and interview, the facility failed to identify and address a significant weight loss timely ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview, the facility failed to ensure staff provided appropriate care and services for one Resident (#42) with a Gastrostomy tube (G-tube: a tube that is pla...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on record review, policy review and interview, the facility failed to provide care and services consistent with professional standards for one Resident (#404) who required renal dialysis (a life...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0699
(Tag F0699)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation record review and interview, the facility failed to ensure a plan of care was developed for Trauma-Informed...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0740
(Tag F0740)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to provide behavioral health services for 1 Resident (#255) out of a t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0745
(Tag F0745)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to provide medically related social services to attain t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to provide dental services to replace missing dentures for 1 Resident ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation and policy review the facility failed to maintain proper sanitation practices in the kitchen, specifically related to glove use when serving the tray line.
Findings include:
Rev...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Administration
(Tag F0835)
Could have caused harm · This affected 1 resident
Based on observations and interviews the facility failed to ensure it was administered in a manner that enabled the facility to use its resources effectively to attain the highest practicable physical...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0837
(Tag F0837)
Could have caused harm · This affected 1 resident
Based on interview and record review, including review of the Quality Assurance and Performance Improvement program (QAPI) facility policy, the facility failed to ensure that the governing body provid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0841
(Tag F0841)
Could have caused harm · This affected 1 resident
Based on record review and interview the facility failed to ensure that the medical director attended the Quality Assurance and Performance Improvement (QAPI) meetings at least quarterly.
Findings inc...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected 1 resident
Based on interview and review of the Quality Assurance Performance Improvement (QAPI) meeting minutes for 2023, the facility staff failed to ensure an effective QAPI plan was in place.
Findings inclu...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0868
(Tag F0868)
Could have caused harm · This affected 1 resident
Based on observation and interview the facility failed to ensure that the Medical Director or an appropriate designee attended Quality Assurance and Performance Improvement Plan (QAPI) Committee meeti...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to offer and provide influenza immunization for one Resident (#64) out of five residents reviewed.
Findings include:
Resident #64 was admitt...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to offer and provide Covid-19 immunization for one Resident (#64) out of five residents reviewed.
Findings include:
Resident #64 was admitte...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility staff failed to provide a choice of smoking was honored for two Resident's (#15) and (#79), out of a total sample of 40 residents.
Fin...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident #70 was admitted to the facility in June, 2023 with diagnoses including fracture of right leg and orthostatic hypote...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. Resident #90 was admitted to the facility in May 2023 with diagnoses including diabetes mellitus due to underlying condition ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and interview, the facility failed to: 1. assess and treat one Resident (#68) after a declin...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident #48 was admitted to the facility in November 2023 with diagnoses including chronic obstructive pulmonary disease, in...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, facility assessment review, and in-service documentation review, the facility failed to ensure that the nurs...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to complete annual Certified Nurse Aide (CNA) performance reviews for six of six sampled Certified Nurses Assistants (CNAs).
Findings include:...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and interviews, the facility failed to ensure it provided a physician ordered medication for...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observations, record reviews, policy reviews and interviews, the facility failed to ensure it was free from a medication error rate of greater than 5 percent. Three out of four nurses observe...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected multiple residents
Based on observations, record reviews and interviews, the facility failed to ensure that a resident was free from significant medication error. Specifically, the facility failed to ensure blood pressu...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observations, policy review and interviews, the facility failed to ensure medications with short expiration dates were dated when opened, failed to ensure medication carts were securely locke...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and review of the facility assessment, the facility failed to accurately evaluate their resident population ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Resident #91 was admitted to the facility in September 2023 with diagnoses including, adult failure to thrive and weakness.
R...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
2. Review of facility policy titled 'Medication Administration' date 2/2023 indicated the following but not limited to:
*Staff follow established facility infection control procedures (e.g., hand wash...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected multiple residents
Based on record review, policy review, and interview the facility failed to ensure that at least 12 hours of in-service training was completed for six of six Certified Nurse Aides (CNAs).
Findings inc...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected most or all residents
Based on observation and interview, the facility failed to provide an ongoing program of individual and group activities designed to meet the interests of and support the physical, mental and psychoso...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Transfer Notice
(Tag F0623)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Resident #42 was admitted to the facility in November 2022 with diagnoses including anoxic brain damage.
Review of Resident #...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0625
(Tag F0625)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Resident #42 was admitted to the facility in November 2022 with diagnoses including anoxic brain damage.
Review of Resident #...
Read full inspector narrative →
Sept 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews for one of four sampled residents (Resident #1) the Facility failed to ensure they main...
Read full inspector narrative →
Dec 2022
23 deficiencies
3 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Notification of Changes
(Tag F0580)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews, policy review and interviews, the facility failed to alert the physician in a timely manner of a change...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews, policy review and interviews, the facility 1) failed to ensure treatment and services were provided in ...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, record review and policy review, the facility failed to provide the necessary treatment and services to prev...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview the facility failed to obtain a doctor's order for the self administration of medication fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure adaptive equipment for meals, specifically buil...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview the facility failed to ensure a bruise of unknown origin was reported to the State Agency for 1 resident (#27) out of a total sample of 29 residents. ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and interview the facility failed to 1. ensure standards of quality nursing practice for fou...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, record review and policy review, the facility failed to investigate an unwitnessed fall for 1 Resident (#48)...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure Oxygen was administered in accordance with phy...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview, the facility failed to ensure sufficient staff was in place on 1 of 3 resident care units to implement the plan of care for 1 Resident (#19) out of a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to act on the monthly medication reviews conducted by the consulting pharmacist, for 1 Resident (#98) out of 5 residents reviewed for medicati...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure for one resident (#98) out of a total sample of 29 residents, that an as needed (PRN) psychotropic medication did not exceed 14 days...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure it was free from a medication error rate of greater than 5 percent. 1 of 2 nurses observed made 2 errors in 28 opportun...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to provide dental services for 1 Resident (#57) out of a total sample of 29 residents.
Findings include:
Review of the facility'...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. For Resident #40, the facility failed to accurately transcribe provider orders and failed to document a medication administer...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure an on-going effective, comprehensive quality assurance and improvement plan was in place with good faith effort to identify deficien...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview the facility failed to ensure infection control measures were implemented to prevent the spread of infection on 2 of 3 units.
Findings include:
Review...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
Based on policy review and interview , the facility failed to implement an antibiotic stewardship program to determine if antibiotics were prescribed for the correct amount of time, at the correct dos...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and interview the facility failed to ensure investigations were conducted for 2 residents (#...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. For Resident #9, the facility failed to obtain weekly weights as ordered.
Review of facility policy titled 'Weight Measuremen...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Resident #84 was admitted to the facility in October 2022 with diagnoses including muscular dystrophy, heart failure, type 2 ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. For Resident #51, the facility failed to provide continuous supervision while eating during meal times.
Resident #51 was admi...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0582
(Tag F0582)
Minor procedural issue · This affected most or all residents
Based on record review and interview, the facility failed to meet the obligation to issue residents who received services under Medicare Part A, a Skilled Nursing Facility Advanced Beneficiary Notice ...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 4 harm violation(s), $227,924 in fines. Review inspection reports carefully.
- • 91 deficiencies on record, including 4 serious (caused harm) violations. Ask about corrective actions taken.
- • $227,924 in fines. Extremely high, among the most fined facilities in Massachusetts. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is West Newton Healthcare's CMS Rating?
CMS assigns WEST NEWTON HEALTHCARE an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Massachusetts, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is West Newton Healthcare Staffed?
CMS rates WEST NEWTON HEALTHCARE's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 70%, which is 24 percentage points above the Massachusetts average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs. RN turnover specifically is 86%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at West Newton Healthcare?
State health inspectors documented 91 deficiencies at WEST NEWTON HEALTHCARE during 2022 to 2025. These included: 4 that caused actual resident harm, 83 with potential for harm, and 4 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates West Newton Healthcare?
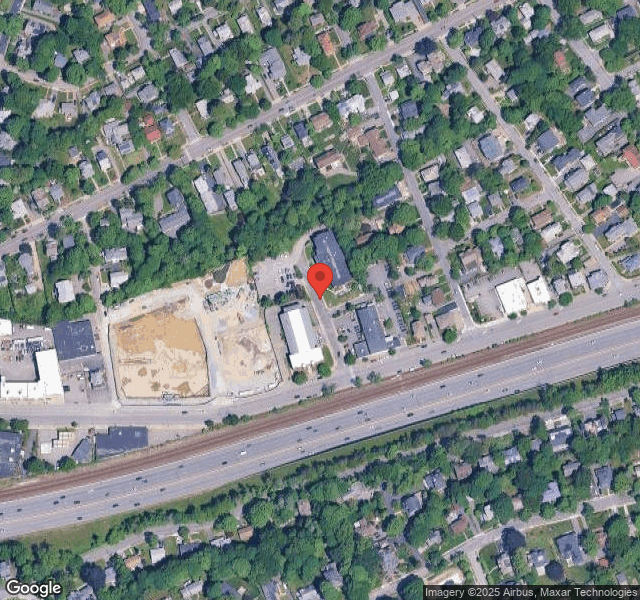
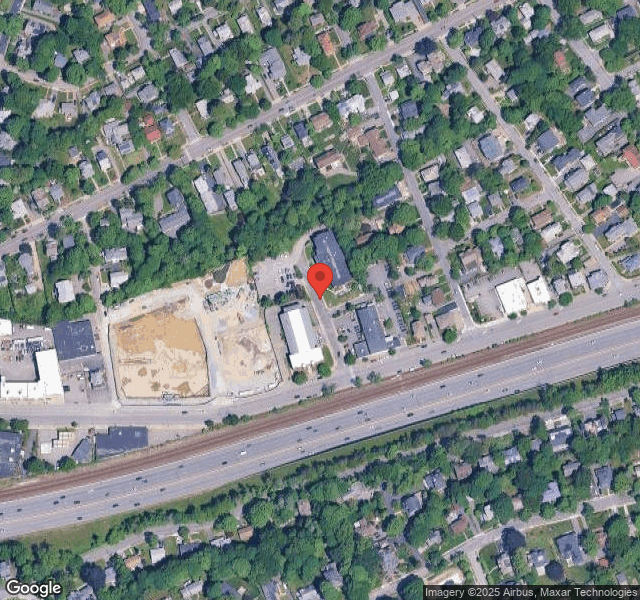
WEST NEWTON HEALTHCARE is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by NEXT STEP HEALTHCARE, a chain that manages multiple nursing homes. With 123 certified beds and approximately 102 residents (about 83% occupancy), it is a mid-sized facility located in WEST NEWTON, Massachusetts.
How Does West Newton Healthcare Compare to Other Massachusetts Nursing Homes?
Compared to the 100 nursing homes in Massachusetts, WEST NEWTON HEALTHCARE's overall rating (1 stars) is below the state average of 2.9, staff turnover (70%) is significantly higher than the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting West Newton Healthcare?
Based on this facility's data, families visiting should ask: "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's high staff turnover rate and the below-average staffing rating.
Is West Newton Healthcare Safe?
Based on CMS inspection data, WEST NEWTON HEALTHCARE has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Massachusetts. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at West Newton Healthcare Stick Around?
Staff turnover at WEST NEWTON HEALTHCARE is high. At 70%, the facility is 24 percentage points above the Massachusetts average of 46%. Registered Nurse turnover is particularly concerning at 86%. RNs handle complex medical decisions and coordinate care — frequent RN changes can directly impact care quality. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was West Newton Healthcare Ever Fined?
WEST NEWTON HEALTHCARE has been fined $227,924 across 2 penalty actions. This is 6.4x the Massachusetts average of $35,358. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is West Newton Healthcare on Any Federal Watch List?
WEST NEWTON HEALTHCARE is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.