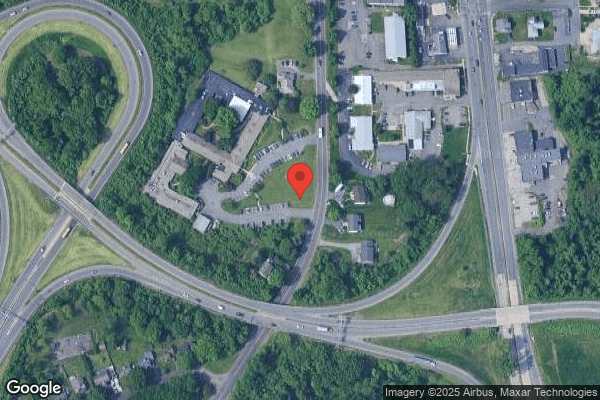
BEAR MOUNTAIN AT WEST SPRINGFIELD
Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Bear Mountain at West Springfield has a Trust Grade of F, indicating poor performance and significant concerns about the quality of care provided. It ranks #201 out of 338 facilities in Massachusetts, placing it in the bottom half of all state nursing homes, and #17 out of 25 in Hampden County, meaning there are only a few better options locally. While the facility is reportedly improving, as issues decreased from 30 in 2023 to 9 in 2024, it still has substantial problems, including $219,716 in fines, which is concerning and higher than 90% of Massachusetts facilities. Staffing is average with a 3/5 rating, but RN coverage is below average, being less than 90% of state facilities, which could impact resident care. Notable incidents include residents with gastrostomy tubes experiencing serious complications due to inadequate monitoring and care, as well as a resident falling during care because staff did not follow their care plan, highlighting both the strengths and weaknesses of this facility.
- Trust Score
- F
- In Massachusetts
- #201/338
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 46% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $219,716 in fines. Lower than most Massachusetts facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 23 minutes of Registered Nurse (RN) attention daily — below average for Massachusetts. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 55 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Massachusetts average (2.9)
Below average - review inspection findings carefully
Near Massachusetts avg (46%)
Higher turnover may affect care consistency
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 55 deficiencies on record
Oct 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on interviews and records reviewed, for one of three sampled residents (Resident #1), who was cognitively intact and had the potential to be verbally aggressive, the Facility failed to ensure he...
Read full inspector narrative →
Aug 2024
8 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure a care plan was developed to address the medical needs for one Resident (#52) out of a total sample of 26 residents.
Specifically, ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on interview, record review, and policy review the facility failed to maintain professional standards of practice to prevent the development and promote healing of pressure ulcers/skin injuries ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview, record and policy review, the facility failed to provide care and services for the administration of supplemental Oxygen (O2), consistent with professional standards o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on interview, record and policy review, the facility failed to ensure that recommendations made by the Consultant Pharmacist during a monthly Medication Regimen Review (MRR) were acted upon as r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0773
(Tag F0773)
Could have caused harm · This affected 1 resident
Based on record review, and interview, the facility failed to ensure that Physician orders were in place prior to laboratory testing being conducted for two Residents (#52 and #59), out of a total app...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident #1 was admitted to the facility in April 2018, with diagnoses including Chronic Obstructive Pulmonary Disease (COPD:...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, interview, and policy review, the facility failed to adhere to infection control standards to prevent the potential transmission of communicable diseases and infections within th...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Assessment Accuracy
(Tag F0641)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident #54 was admitted to the facility in May 2024, with diagnoses including Anxiety Disorder (mental health disorder char...
Read full inspector narrative →
Dec 2023
6 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews, for one of four sampled residents (Resident #3), who's physician orders included the a...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews, for one of four sampled residents (Resident #1), the Facility failed to ensure that staff implemented and followed their Abuse Policy related to the need to i...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews, for one of four sampled residents (Resident #1), the Facility failed to ensure that after being made aware of an allegation of neglect on 10/22/23, that they ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0694
(Tag F0694)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews, for one of four sampled residents (Resident #3) who had a peripherally inserted centra...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews, for one of four sampled residents (Resident #3), who had a recent partial hip replacement and was at risk for the development of a blood clot, and had physici...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interview, for one out of four sampled residents (Resident #3) who was admitted to the Facility wi...
Read full inspector narrative →
Oct 2023
2 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Comprehensive Care Plan
(Tag F0656)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews, for one of three sampled residents (Resident #1), whose Plan of Care indicated that he...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews, for one of three sampled residents (Resident #1), who was assessed by nursing to be at...
Read full inspector narrative →
May 2023
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to ensure its staff completed a Significant Change in St...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, policy review and interview, the facility failed to provide discharge planning services with respect for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, and interviews the facility failed to provide Activities of Daily Living (ADLs - basic sel...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0687
(Tag F0687)
Could have caused harm · This affected 1 resident
Based on policy review, record review, and interview, the facility failed to ensure routine diabetic foot care was provided for one Resident (#68) out of a total sample of 24 residents, to maintain go...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure its staff provided care and services consistent...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation, interview, and policy review, the facility failed to ensure that its staff maintained a clean and sanitary environment in the main kitchen, and adhered to safe food practices rel...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident #24 was admitted to the facility in July 2020 with diagnoses including Dementia (A group of symptoms that affects me...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. For Resident #1, the facility failed to ensure its staff reviewed and acted upon pharmacy recommendations for Abnormal Involu...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** b) On 5/30/23 at 12:40 P.M., on Unit One, the surveyor observed the side one medication cart in the hallway unlocked and unatten...
Read full inspector narrative →
May 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews, for one of three sampled residents (Resident #1), the Facility failed to ensure that a...
Read full inspector narrative →
Mar 2023
6 deficiencies
3 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews, for one of three sampled residents (Resident #1), who upon admission to the Facility i...
Read full inspector narrative →
SERIOUS
(H)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0692
(Tag F0692)
A resident was harmed · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews, for two of three sampled residents (Resident #1 and Resident #2), who had gastrostomy ...
Read full inspector narrative →
SERIOUS
(H)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Tube Feeding
(Tag F0693)
A resident was harmed · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews, for two of three sampled residents (Resident #1 and Resident #2), who had gastrostomy ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews, for two of three sampled residents (Resident #1, and Resident #2), who had gastrostomy tubes (tube placed through the abdomen into the stomach, for feedings, ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews, for three of three sampled employee personnel files, (Nurse #4, Nurse #5 and Nurse #6 ), who consistently worked the 11:00 P.M. to 7:00 A.M., and were assigne...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews, for two of three sampled residents (Resident #1 and Resident #2), the Facility failed to ensure they maintained a complete and accurate medical record that in...
Read full inspector narrative →
Jan 2023
4 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure that its staff maintained medical records that included documentation indicating that the Resident or Resident's Representative was ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
During an observation and interview on 1/18/23 at 8:53 A.M., the surveyor observed Nurse #1 exit a resident room that indicated droplet precautions were in effect as evidenced by a sign outside the do...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0886
(Tag F0886)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to ensure its staff tested for COVID-19 in accordance with current Ce...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0885
(Tag F0885)
Could have caused harm · This affected most or all residents
Based on record review and interviews, the facility failed to ensure that its staff informed/ notified all Residents, their Representatives, and families by 5 P.M. the next calendar day following an o...
Read full inspector narrative →
Jan 2023
2 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Comprehensive Care Plan
(Tag F0656)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, records reviewed and interviews for one of three sampled residents (Resident #1), who was assessed by nurs...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, records reviewed and interviews for one of three sampled residents (Resident #1), who required hands on as...
Read full inspector narrative →
Sept 2021
16 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure one Resident (#13) was provided reasonable accommodations relative to providing him/her with a hand bell within reach ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to notify the Physician of a change in condition for one...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Employment Screening
(Tag F0606)
Could have caused harm · This affected 1 resident
Based on interview, review of staff personnel files and policy review, the facility failed to perform State Nurse Aide Registry checks, as required, prior to hiring of one out of five sampled staff me...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide adequate supervision to prevent accidents for one Resident (#61) out of a total sample of 19 residents.
Findings incl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to adhere to requirements related to 1) Foley catheter (tube inserted into the bladder to drain urine) care and services for one...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Review of the facility's policy titled Consultant Pharmacist Reports, revised January 2018, indicated:
.C. Recommendations are acted upon and documented by the facility staff and/or the prescriber .
...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to limit the timeframe for a PRN (as needed) psychotropic medication (a medication that alters mood/behavior) to 14 days for one Resident (#48)...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one Resident (#72) was free of significant medication errors, relative to the administration of an anticoagulant (blood thinner medi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview, and policy review, the facility failed to ensure medications and biologicals were properly stored in one out of three medication carts.
Findings include:
Review of fac...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0772
(Tag F0772)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure laboratory services were provided timely for one sampled Resident (#13), out of a total sample of 19 residents.
Findings include:
R...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to maintain a clinical record that was complete and accurate for one Residents (#13), out of a a total sample of 19 residents.
Findings includ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure the plan of care was developed and/or implemen...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected multiple residents
Based on interview, the facility failed to designate a person, who met regulatory requirements, to serve as the Director of Food and Nutrition Services when a full-time dietician was not employed.
Fin...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
2. On Unit 3, the facility failed to ensure staff members used eye protection before entering a resident's room, as required.
On 9/27/21 at 10:07 A.M., the surveyor observed Laundry Personnel #1 enter...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, that facility failed to ensure that A.) food items for resident consumption were labeled and dated, B.) food items that indicated a use by date were...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0868
(Tag F0868)
Minor procedural issue · This affected multiple residents
Based on interview the facility failed to provide documented evidence that quarterly Quality Assurance and Performance Improvement (QAPI: a committee that identifies problems within the facility and i...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 7 harm violation(s), $219,716 in fines. Review inspection reports carefully.
- • 55 deficiencies on record, including 7 serious (caused harm) violations. Ask about corrective actions taken.
- • $219,716 in fines. Extremely high, among the most fined facilities in Massachusetts. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Bear Mountain At West Springfield's CMS Rating?
CMS assigns BEAR MOUNTAIN AT WEST SPRINGFIELD an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Massachusetts, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Bear Mountain At West Springfield Staffed?
CMS rates BEAR MOUNTAIN AT WEST SPRINGFIELD's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 46%, compared to the Massachusetts average of 46%.
What Have Inspectors Found at Bear Mountain At West Springfield?
State health inspectors documented 55 deficiencies at BEAR MOUNTAIN AT WEST SPRINGFIELD during 2021 to 2024. These included: 7 that caused actual resident harm, 46 with potential for harm, and 2 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Bear Mountain At West Springfield?
BEAR MOUNTAIN AT WEST SPRINGFIELD is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by BEAR MOUNTAIN HEALTHCARE, a chain that manages multiple nursing homes. With 168 certified beds and approximately 113 residents (about 67% occupancy), it is a mid-sized facility located in WEST SPRINGFIELD, Massachusetts.
How Does Bear Mountain At West Springfield Compare to Other Massachusetts Nursing Homes?
Compared to the 100 nursing homes in Massachusetts, BEAR MOUNTAIN AT WEST SPRINGFIELD's overall rating (2 stars) is below the state average of 2.9, staff turnover (46%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Bear Mountain At West Springfield?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Bear Mountain At West Springfield Safe?
Based on CMS inspection data, BEAR MOUNTAIN AT WEST SPRINGFIELD has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Massachusetts. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Bear Mountain At West Springfield Stick Around?
BEAR MOUNTAIN AT WEST SPRINGFIELD has a staff turnover rate of 46%, which is about average for Massachusetts nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Bear Mountain At West Springfield Ever Fined?
BEAR MOUNTAIN AT WEST SPRINGFIELD has been fined $219,716 across 4 penalty actions. This is 6.2x the Massachusetts average of $35,276. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Bear Mountain At West Springfield on Any Federal Watch List?
BEAR MOUNTAIN AT WEST SPRINGFIELD is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.