GREENE COUNTY HEALTH AND REHABILITATION
Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Greene County Health and Rehabilitation holds a Trust Grade of C+, indicating a decent performance that's slightly above average among nursing homes. In Mississippi, it ranks #69 out of 200, placing it in the top half of facilities, and it is the best option in Greene County, where it ranks #1 of 2. The facility is improving, with the number of issues decreasing from three in 2024 to two in 2025. Staffing is a strength, with a turnover rate of 0%, meaning staff members are likely to stay long-term and build relationships with residents. However, there have been serious incidents, including a medication error where a resident received another's medication, leading to hospitalization, and a failure to document the use of a restraint on another resident. Overall, while there are positive aspects, families should be aware of these significant weaknesses.
- Trust Score
- C+
- In Mississippi
- #69/200
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ○ Average
- Turnover data not reported for this facility.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Mississippi facilities.
- Skilled Nurses ○ Average
- Each resident gets 36 minutes of Registered Nurse (RN) attention daily — about average for Mississippi. RNs are the most trained staff who monitor for health changes.
- Violations ✓ Good
- Only 5 deficiencies on record. Cleaner than most facilities. Minor issues only.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Near Mississippi average (2.6)
Meets federal standards, typical of most facilities
The Ugly 5 deficiencies on record
Jul 2025
2 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0658
(Tag F0658)
A resident was harmed · This affected 1 resident
Based on interviews, record review, and facility policy review, the facility failed to ensure that medications were administered in accordance with accepted standards of nursing practice and professio...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0760
(Tag F0760)
A resident was harmed · This affected 1 resident
Based on interview, record review, and facility policy review, the facility failed to ensure that a resident was free from a significant medication error for one (1) of four (4) sampled residents, as ...
Read full inspector narrative →
Oct 2024
3 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
Based on observation, interviews, record review, and facility policy review, the facility failed to ensure a resident's right to be free from physical restraints by not identifying and documenting the...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, staff interview, record review, and facility policy review, the facility failed to develop and implement a comprehensive, person-centered care plan to reflect the use of a restra...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation, staff interview, record review, and facility policy review, the facility failed to follow proper sanitation and food handling practices to prevent the possible outbreak of foodbo...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most Mississippi facilities.
- • 5 deficiencies on record, including 2 serious (caused harm) violations. Ask about corrective actions taken.
About This Facility
What is Greene County's CMS Rating?
CMS assigns GREENE COUNTY HEALTH AND REHABILITATION an overall rating of 3 out of 5 stars, which is considered average nationally. Within Mississippi, this rating places the facility higher than 99% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Greene County Staffed?
CMS rates GREENE COUNTY HEALTH AND REHABILITATION's staffing level at 3 out of 5 stars, which is average compared to other nursing homes.
What Have Inspectors Found at Greene County?
State health inspectors documented 5 deficiencies at GREENE COUNTY HEALTH AND REHABILITATION during 2024 to 2025. These included: 2 that caused actual resident harm and 3 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
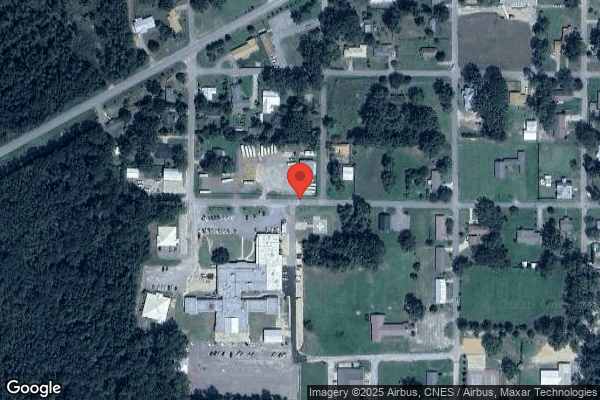
Who Owns and Operates Greene County?
GREENE COUNTY HEALTH AND REHABILITATION is owned by a government entity. Government-operated facilities are typically run by state, county, or municipal agencies. The facility operates independently rather than as part of a larger chain. With 60 certified beds and approximately 50 residents (about 83% occupancy), it is a smaller facility located in LEAKESVILLE, Mississippi.
How Does Greene County Compare to Other Mississippi Nursing Homes?
Compared to the 100 nursing homes in Mississippi, GREENE COUNTY HEALTH AND REHABILITATION's overall rating (3 stars) is above the state average of 2.6 and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Greene County?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Greene County Safe?
Based on CMS inspection data, GREENE COUNTY HEALTH AND REHABILITATION has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #1 of 100 nursing homes in Mississippi. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Greene County Stick Around?
GREENE COUNTY HEALTH AND REHABILITATION has not reported staff turnover data to CMS. Staff turnover matters because consistent caregivers learn residents' individual needs, medications, and preferences. When staff frequently change, this institutional knowledge is lost. Families should ask the facility directly about their staff retention rates and average employee tenure.
Was Greene County Ever Fined?
GREENE COUNTY HEALTH AND REHABILITATION has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Greene County on Any Federal Watch List?
GREENE COUNTY HEALTH AND REHABILITATION is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.