BUFFALO PRAIRIE CENTER FOR REHAB AND HEALTHCARE




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Buffalo Prairie Center for Rehab and Healthcare has received a Trust Grade of F, indicating significant concerns and a poor reputation among nursing homes. Ranking #354 out of 479 facilities in Missouri places it in the bottom half, and it is the second-worst option in Dallas County. Although the facility is improving, with issues decreasing from 17 in 2024 to 13 in 2025, it still faces serious deficiencies, including a critical incident where a staff member inappropriately restricted a resident's freedom. Staffing is a positive aspect, as the facility has a 0% turnover rate, well below the state average, and offers good RN coverage, exceeding 87% of other Missouri facilities. However, it has incurred $8,731 in fines and has a troubling history of managing basic operations, such as failing to pay bills on time, which led to the removal of necessary equipment like a generator.
- Trust Score
- F
- In Missouri
- #354/479
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- Turnover data not reported for this facility.
- Penalties ✓ Good
- $8,731 in fines. Lower than most Missouri facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 28 minutes of Registered Nurse (RN) attention daily — below average for Missouri. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 56 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Missouri average (2.5)
Significant quality concerns identified by CMS
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 56 deficiencies on record
Jun 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure all allegations of possible abuse were reported immediately to facility management and within two hours to the state licensing agenc...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to document a timely and thorough investigation, to include interviews with multiple staff and other residents, and immediate steps taken to p...
Read full inspector narrative →
May 2025
7 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to complete an admission Minimum Data Set (MDS - a federally mandated comprehensive assessment instrument completed by facility staff) in a ti...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to complete significant change Minimum Data Sets (MDS - a federally mandated assessment instrument completed by facility staff) one resident (...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
MDS Data Transmission
(Tag F0640)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to complete a discharge with return anticipated Minimum Data Set (MDS ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to develop a baseline care plan for all residents when staff failed to complete a baseline care plan within 48 hours of admission of one resid...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to develop and implement accurate comprehensive care plans for all residents when staff failed to complete a comprehensive care plan for one r...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide pharmacy services that included procedures for accurate adm...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure food was served at temperatures that were pala...
Read full inspector narrative →
Apr 2025
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure appropriate incontinent care (support and management strategies needed to assist individuals who experience the involu...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0728
(Tag F0728)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure nurse aides (NA) completed their training, competencies, and testing in a timely manner when two NA's failed to complete a state app...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Administration
(Tag F0835)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure the facility was administered in an effective ...
Read full inspector narrative →
Jan 2025
1 deficiency
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Administration
(Tag F0835)
Could have caused harm · This affected most or all residents
Deficiency Text Not Available
Read full inspector narrative →
Nov 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure all residents maintained acceptable parameters of nutrition...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to maintain a functional environment for all residents, staff, and the public when staff failed to maintian the front entrance door power Americ...
Read full inspector narrative →
Oct 2024
15 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide reasonable accommodation of resident needs and preferences when they failed to have hydration accessible for one resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to administer the required Preadmission Screening and Resident Review (PASARR) Screening (Level 1) to identify residents with a mental disabil...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide pharmaceutical services to meet the needs of each resident when facility staff documented ordered medication could not be administe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure all residents were free of significant medication errors when staff failed to administer warfarin sodium (blood thinne...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to maintain complete medical records for all residents w...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Review of Resident #6's face sheet showed the following information:
-admission date of 07/02/24;
-Diagnoses included type tw...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide respiratory care per standards of practice wh...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to provide effective pain management for all residents when staff failed to administer pain medications as ordered for two resid...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Review of the National Library of Medicine document Preventing Errors When Drugs Are Given Via Enteral Feeding Tubes, dated 2...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure all medications were stored and labeled in accordance with standards of practice when staff failed to store controlled...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to ensure consistent and sufficient Registered Nurse (RN) and Director of Nursing (DON) hours to allow the DON to complete the duties of DON w...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility staff failed to employ a qualified dietary manager for food and nutrition services with accredited education in food service management. The facility...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Administration
(Tag F0835)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure the facility was administered in an effective and efficient manner to ensure the highest practical well-being of all r...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
2. Review of facility records showed the facility did not provide a policy or procedure regarding hand hygiene and/or the use of alcohol-based hand rubs.
Review of the CDC Clinical Safety: Hand Hygie...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to implement an effective and complete antibiotic stewardship program when staff failed to track residents on antibiotics for various infectio...
Read full inspector narrative →
Dec 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure residents were free from significant medication errors when the facility failed to document transcribe physician's orders accurately...
Read full inspector narrative →
Feb 2023
4 deficiencies
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0603
(Tag F0603)
Someone could have died · This affected 1 resident
Based on observation, record review, and interview, the facility failed to protect the resident's right to be free from involuntary seclusion by staff when one staff member Registered Nurse (RN) A hel...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review, facility staff failed to notify one resident's (Resident #1) family and physician, in a timely manner, of a change in behaviors that resulted in seclusion of the ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility staff failed to report an allegation of abuse immediately to the facility management and within two hours to the State Survey Agency (Department of H...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility staff failed to complete a timely investigation of abuse when staff observed one resident (Resident #1) involuntarily secluded to his/her room by a s...
Read full inspector narrative →
Dec 2022
16 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to promote and facilitate self-determination when staff ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to provide clean bed linens that were in good condition for four residents (Residents #15 and #18). The facility census was 49. ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
MDS Data Transmission
(Tag F0640)
Could have caused harm · This affected 1 resident
Based on record review and interviews, the facility failed to complete and electronically transmit a discharge Minimum Data Set (MDS - a federally mandated assessment tool completed by facility staff)...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to complete a baseline care plan within 48 hours of admission for one resident (Resident #203) and failed to document reviewing or providing a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to complete a criminal background check (CBC) and Employee Disqualification List (EDL - a state listing of individuals who have been determine...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 1. Record review of Resident #44's face sheet showed an admission date of 9/26/2022.
Record review of resident's nurses' notes ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Record review of Resident #44's face sheet showed the following information and admission date of 9/26/2022.
Record review of...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0638
(Tag F0638)
Could have caused harm · This affected multiple residents
Based on record review and interview, facility staff failed to complete a quarterly Minimum Data Set (MDS - a federally mandated assessment instrument completed by facility staff) assessment for eight...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to develop and implement a care plan related to Resident...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0678
(Tag F0678)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Record review of Resident #10's face sheet showed the following:
-admitted to the facility on [DATE];
-Full Code.
Record revi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility staff failed to store refrigerated medications at the manufacture's recommended temperatures and failed to have a system in place to mo...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to have sufficient nursing staff to meet the needs of al...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected most or all residents
Based on interview, observation, and record review, the facility failed to provide palatable and appeasing food to all residents. The facility had a census of 49.
Record review of the facility policy,...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on interview, observation, and record review, the facility failed to protect food while stored per professional standards food contact surfaces (dishes) were stacked wet instead of air dried, de...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
1. Record review of the CDC (Centers for Disease Control and Prevention) Toolkit for Legionella (also titled Developing a Water Management Program to Reduce Legionella Growth & Spread in Buildings), d...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected most or all residents
Based on observation and interview, facility staff failed to post required nurse staffing information daily. The facility census was 49.
1. Observation on 12/06/22, at 10:52 A.M., showed the nurse sta...
Read full inspector narrative →
Nov 2019
5 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to provide a Skilled Nursing Facility Advance Beneficiary Notice (SNFABN, form CMS-10055) or a denial letter at the initiation, reduction, or ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide restorative nursing services to maintain or im...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one resident (Resident #35), with a history of...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0570
(Tag F0570)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to maintain a surety bond sufficient to ensure protection of resident funds. The facility's census was 46.
1. Record review of the facility's ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected most or all residents
Based on observation and interview, facility staff failed to ensure every hose that extended below the flood plain had a backflow preventer (an anti-siphon device used to keep toxins from backing up i...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 1 life-threatening violation(s), Payment denial on record. Review inspection reports carefully.
- • 56 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • Grade F (26/100). Below average facility with significant concerns.
About This Facility
What is Buffalo Prairie Center For Rehab And Healthcare's CMS Rating?
CMS assigns BUFFALO PRAIRIE CENTER FOR REHAB AND HEALTHCARE an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Missouri, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Buffalo Prairie Center For Rehab And Healthcare Staffed?
CMS rates BUFFALO PRAIRIE CENTER FOR REHAB AND HEALTHCARE's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes.
What Have Inspectors Found at Buffalo Prairie Center For Rehab And Healthcare?
State health inspectors documented 56 deficiencies at BUFFALO PRAIRIE CENTER FOR REHAB AND HEALTHCARE during 2019 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 54 with potential for harm, and 1 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
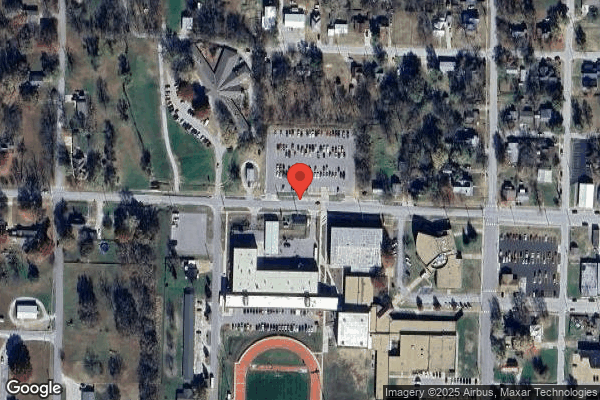
Who Owns and Operates Buffalo Prairie Center For Rehab And Healthcare?
BUFFALO PRAIRIE CENTER FOR REHAB AND HEALTHCARE is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by PRIME HEALTHCARE MANAGEMENT, a chain that manages multiple nursing homes. With 60 certified beds and approximately 49 residents (about 82% occupancy), it is a smaller facility located in BUFFALO, Missouri.
How Does Buffalo Prairie Center For Rehab And Healthcare Compare to Other Missouri Nursing Homes?
Compared to the 100 nursing homes in Missouri, BUFFALO PRAIRIE CENTER FOR REHAB AND HEALTHCARE's overall rating (1 stars) is below the state average of 2.5 and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Buffalo Prairie Center For Rehab And Healthcare?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's Immediate Jeopardy citations and the below-average staffing rating.
Is Buffalo Prairie Center For Rehab And Healthcare Safe?
Based on CMS inspection data, BUFFALO PRAIRIE CENTER FOR REHAB AND HEALTHCARE has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Missouri. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Buffalo Prairie Center For Rehab And Healthcare Stick Around?
BUFFALO PRAIRIE CENTER FOR REHAB AND HEALTHCARE has not reported staff turnover data to CMS. Staff turnover matters because consistent caregivers learn residents' individual needs, medications, and preferences. When staff frequently change, this institutional knowledge is lost. Families should ask the facility directly about their staff retention rates and average employee tenure.
Was Buffalo Prairie Center For Rehab And Healthcare Ever Fined?
BUFFALO PRAIRIE CENTER FOR REHAB AND HEALTHCARE has been fined $8,731 across 1 penalty action. This is below the Missouri average of $33,166. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Buffalo Prairie Center For Rehab And Healthcare on Any Federal Watch List?
BUFFALO PRAIRIE CENTER FOR REHAB AND HEALTHCARE is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.