CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure resident dignity by not providing a dignity ba...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure resident dignity by not providing a dignity bag to cover a resident's Foley catheter (a tube with retaining balloon passed through the urethra into the bladder to drain urine) while the resident was in his/her room for two sampled residents (Resident #40 and #197) and to ensure the resident's privacy curtain and window blinds were pulled closed during incontinent and wound care for one sampled resident (Resident #40) out of 16 sampled residents. The facility census was 55 residents.
Record review of the facility Indwelling Urinary Catheter Policy revised date of November 2017 showed:
-Cover the urine bag to provide privacy.
-Drainage bag and tubing are to be kept off the floor.
1. Record review of Resident #40's Face Sheet showed he/she was admitted to the facility on [DATE] and readmitted on [DATE] with the following diagnoses:
-Anxiety disorder.
-Pressure ulcer (localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear and/or friction) of sacral region (tailbone), unstageable (Full thickness tissue loss in which the base of the ulcer is covered by slough [necrotic/avascular tissue in the process of separating from the viable portions of the body & is usually light colored, soft, moist, & stringy] and/or eschar (tan, brown or black) in the wound bed).
-Bipolar disorder (mood disorders characterized usually by alternating episodes of depression and mania).
-Major Depressive Disorder.
Record review of the resident's annual Minimum Data Set (MDS - a federally mandated assessment instrument completed by facility staff for care planning) dated 10/20/19 showed the resident:
-Was cognitively intact with a Brief Interview for Mental Status (BIMS) of 15 out of 15.
-Required extensive staff assistance with bed mobility, transfers, dressing, toileting, and personal hygiene.
-Had a urinary catheter and colostomy (an alternative exit from the colon created to divert waste through a hole in the colon and through the wall of the abdomen).
-Had no pressure ulcers or skin issues.
Observation on 11/19/19 at 8:19 A.M., 11/20/19 at 8:40 A.M. and 9:01 A.M., showed:
-The resident was in his/her room in bed.
-His/her Foley catheter bag was hanging from the side of the bed without a dignity bag.
-The resident's uncovered Foley catheter bag was visible from the hallway.
Observation on 11/20/19 at 10:46 A.M. showed:
-The resident's Foley catheter bag was hanging from the side of the bed, uncovered and visible from the hallway.
-Certified Nursing Assistant (CNA) C and Licensed Practical Nurse (LPN) D performed catheter care for the resident.
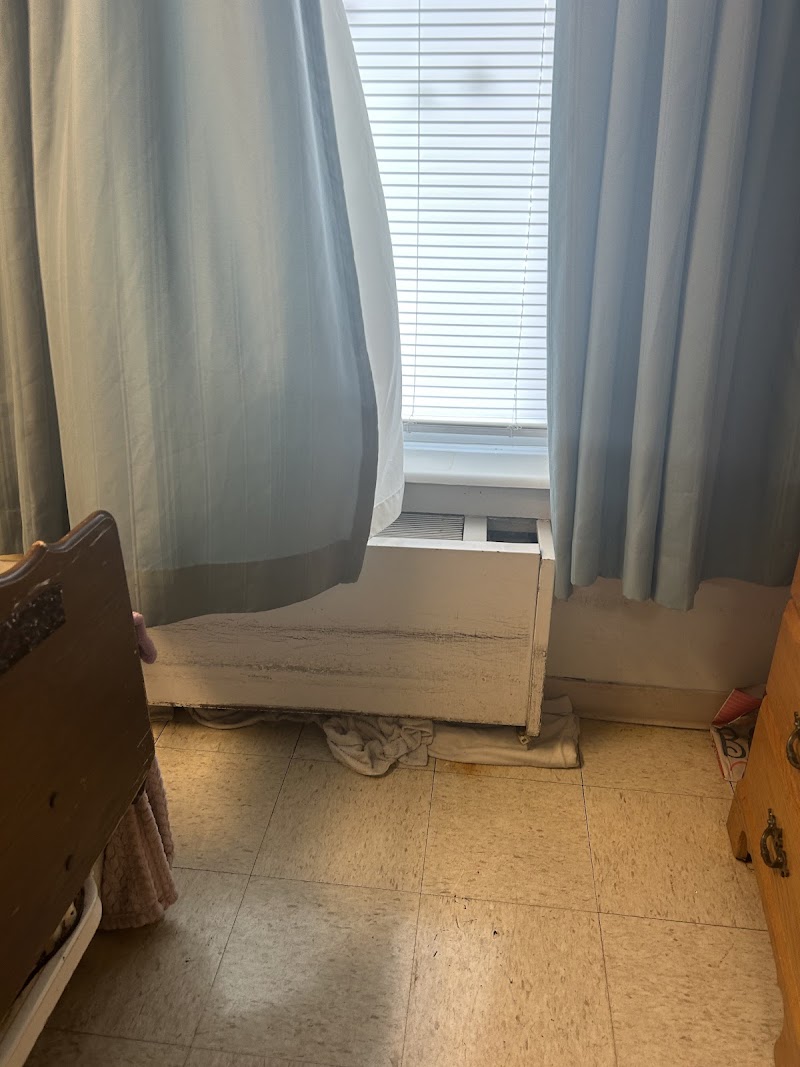
-CNA C and LPN D closed the resident's door, and without pulling the privacy curtain closed or closing the open window blind, uncovered the resident so his/her genitalia were visible, and assisted the resident with opening his/her legs to access the area between his/her legs.
-CNA C and LPN D assisted the resident to turn to his/her side, exposing his/her buttocks so LPN D could perform wound care with the resident's privacy curtain not pulled closed and the window blinds open.
-CNA C and LPN D assisted the resident to turn to lay on his/her back, and with the resident's bed linens pulled to the end of the bed and the resident's genitalia exposed, LPN D opened the door to exit the room, the resident was fully visible from the hallway.
During an interview on 11/20/19 at 11:10 A.M., LPN D said:
-The resident's blinds should have been closed before starting personal cares, exposing the resident, who could have been seen by anyone who was outside at the smokers patio.
-He/She had not noticed the resident did not have a privacy curtain since the resident's bed was by the door and the door was closed.
-The room had a privacy curtain that could be pulled to separate the resident from the resident who lived by the window.
-He/She did not think the resident's catheter bag needed to be covered when he/she was in his/her room.
-The resident's catheter was covered in a dignity bag when he/she was in his/her wheelchair out in the facility.
During an interview on 11/20/19 at 11:23 A.M., CNA C said:
-The resident's blinds should have been closed to prevent anyone at the smokers patio from seeing the resident exposed during cares.
-He/She could have pulled the privacy curtain that separated the resident from the resident that lives on the side by the window, but he/she could not reach the chain that needed to be pulled to switch the tract the privacy curtain was on.
-The resident should have been covered up before the door was opened since there was not a privacy curtain to prevent the resident from being exposed to anyone in the hallway.
-He/She did not think the resident's catheter bag needed to be covered when he/she was in his/her room.
-The resident's catheter was covered in a dignity bag when he/she was in his/her wheelchair out in the facility.
Observation on 11/21/19 at 9:53 A.M. and 12:45 P.M. showed:
-The resident was in his/her room in bed.
-His/Her Foley catheter bag was hanging from the side of the bed without a dignity bag.
-The resident's uncovered Foley catheter bag was visible from the hallway.
2. Record review of Resident #197's Face Sheet showed he/she was admitted to the facility on [DATE] and readmitted on [DATE] with the following diagnoses:
-Urinary Tract Infection (UTI - an infection of one or more structures in the urinary system).
-Pressure ulcer, unspecified stage.
-Right below the knee amputation.
-Left below the knee amputation.
-Colostomy.
-Major Depressive disorder.
-Anxiety.
-Paraplegia (loss of movement of both legs and generally the lower trunk).
Record review of the resident's quarterly MDS dated [DATE] showed he/she:
-Was cognitively intact with a BIMS of 15 out of 15.
-Required total staff dependence for bed mobility, transfers, dressing, toileting, and personal hygiene.
-Had a urinary catheter and colostomy.
-Had Stage III pressure ulcer (a full thickness tissue loss. Subcutaneous fat may be visible but bone, tendon or muscle is not exposed. Slough may be present but does not obscure the depth of tissue loss. May include undermining or tunneling) and Stage IV pressure ulcer (Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present on some parts of the wound bed. Often includes undermining and tunneling).
Observation on 11/19/19 at 8:33 A.M., 11/20/19 at 1:26 P.M., 11/21/19 at 9:52 A.M. showed:
-The resident was in his/her room in bed.
-His/her Foley catheter bag was hanging from the side of the bed without a dignity bag.
-The resident's uncovered Foley catheter bag was visible from the hallway.
3. During an interview on 11/21/19 at 2:55 P.M., the Director of Nursing (DON) and Administrator said:
-A resident's Foley catheter bag should be in a dignity bag, even if the resident is in his/her room.
-He/she expected staff to pull the privacy curtain closed and closed the window blinds before exposing the resident during personal cares and wound care.
-He/she expected the residents who resided on the side of the room by the door to have a privacy curtain, and that privacy curtain should have been pulled closed to ensure the resident was not accidentally exposed if someone entered the resident's room.
-He/she was not aware staff had to pull a cord to change the tract for the privacy curtain or that staff could not reach the cord in order to pull he curtain closed for resident's residing by the door.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0567
(Tag F0567)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to obtain an authorization to manage Resident #35's funds from his/her...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to obtain an authorization to manage Resident #35's funds from his/her legal guardian after that resident became a ward (a person who by reason of incapacity is under the protection of a court either directly or through a guardian appointed by the court-called also ward of court) of the public administrator and to obtain written authorization for Resident #3's hair styling. This practice potentially affected two out of four residents selected for the resident fund review process. The facility census was 55 residents.
1. Record review of the authorization forms (a form signed by the resident or the resident's responsible party to authorize the facility to manage the resident's money), for four selected residents, showed the absence of an authorization for Resident #35.
During an interview on 11/20/19 at 9:10 A.M., the Social Service Designee (SSD) said:
- There was not an authorization form for Resident #35.
- The resident was admitted on [DATE], and
- The resident signed up for funds shortly after that.
2. Record review of Resident #3's records, showed the resident spent $10 on each of the following dates, 8/29/19, 9/8/19, and 9/12/19 for a total of $30.00, and the absence of any signatures by the resident or the resident's designee for hair styling.
During an interview on 11/20/19 at 937 A.M, the Business Office Manager (BOM) and the SSD agreed there were not signatures to authorize those expenses.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0569
(Tag F0569)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to complete and send a Third Party Liability (TPL) form (a form which ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to complete and send a Third Party Liability (TPL) form (a form which is sent to MO Healthnet which gives an accounting of the remaining balance of that resident's funds in the resident trust account), which is required to be sent 30 days after the death of one deceased resident (Resident #1002) who died on [DATE]. This practice affected one resident (Resident #1002) of two deceased residents whose resident fund records were reviewed for the purpose of conducting the resident fund investigation for the completion of the TPL forms. The facility census was 55 residents.
1. Record review of Resident #1002's records showed:
- The resident expired on [DATE]; and
- The Resident had $10.00 in the system at the time of the review.
During interviews on [DATE] at 11:18 A.M., the Social Service Designee (SSD) said:
- The resident received Medicaid; and
- He/she did not know what the TPL form was at that time.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a resident's current code status (whether the resident wante...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a resident's current code status (whether the resident wanted life saving measures taken in the event of his/her heart stopped beating or he/she stopped breathing) was accurate and clear on the resident's Physician's Order Sheet (POS) for two sampled residents (Resident #13 and #198) out of 16 sampled residents. The facility census was 55 residents.
1. Record review of Resident #13's Face Sheet showed he/she was admitted to the facility on [DATE] and readmitted on [DATE] with the following diagnoses:
-Major Depressive disorder.
-Anxiety.
-Hepatitis C (a viral infection that attacks the liver).
-Chronic kidney disease (CKD - gradual loss of kidney function over time).
-Chronic Obstructive Pulmonary Disease (COPD - a disease process that decreases the ability of the lungs to perform ventilation).
-The resident had a Do Not Resuscitate (DNR - do not perform chest compressions or artificial breathing in the case of an emergency; allow natural death).
-The resident had a guardian.
Record review of the resident's care plan dated [DATE] showed:
-The resident was a full code status (all life saving measures are to be taken in the case of an emergency [Cardiopulmonary Resuscitation - CPR - an emergency life saving measure when the heart stops beating and breathing has stopped]).
-A paper was placed on the resident's chart to reflect the resident's wish for a full code status.
Record review of the resident's quarterly Minimum Data Set (MDS - a federally mandated assessment instrument completed by facility staff for care planning) dated [DATE] showed the resident:
-Was cognitively intact with a BIMS of 13 out of 15.
-Was independent with bed mobility.
-Required staff supervision for dressing, eating, toileting, and personal hygiene,
-Required limited staff assistance for transfers.
Record review of the resident's paper chart showed:
-A sheet of paper that had Full Code in all capital, bold letters.
-If he/she should stop breathing for any reason, it was his/her wish that the facility begin CPR and transport him/her to the hospital.
-The form was dated [DATE].
-An Outside the Hospital Do Not Resuscitate Order (a standardized order form explaining the meaning of a DNR order signed by the resident and/or the resident's representative and the resident's physician) was not located on the resident's chart as of [DATE].
Record review of the resident's hospital discharge orders dated [DATE] showed the resident had a DNR/Do not intubate (DNI - no artificial breathing) status.
Record review of the resident's Telephone Order Sheet (TOS) dated [DATE] showed:
-The resident was readmitted to the facility.
-The resident had a DNR/DNI status.
-The order was signed by one nurse.
-The order was not signed by the resident's physician as of [DATE].
Record review of the resident's [DATE] Physician's Order Sheet (POS) showed:
-The resident had a Full Code status.
-The resident's TOS dated [DATE] did not have the resident's desire for DNR/DNI transcribed to the POS.
Record review of the resident's electronic medical record on [DATE] showed the resident had a DNR code status on the resident's profile screen.
During an interview on [DATE] at 10:56 A.M., the resident said he/she wanted to be a full code status.
During an interview on [DATE] at 11:05 A.M. Certified Nursing Assistant (CNA) D said:
-According to the resident's electronic medical record, he/she had a DNR status.
-According to the resident's paper medical record, he/she had a Full Code paper on his/her chart, meaning the resident was Full Code status.
-He/She thought the resident may have had a recent change in code status, but with the conflicting papers, he/she was not sure what the resident's code status was.
During an interview on [DATE] at 11:07 A.M., the Assistant Director of Nursing (ADON) said:
-The resident had a TOS with an order for DNR dated [DATE].
-The order was not signed by the resident's physician, so it was not a valid order.
-If the resident had a DNR order, it should have been signed before 14 days had passed.
During an interview on [DATE] at 11:11 A.M., the Administrator and Social Service Designee said:
-Per the resident's guardian, the resident was a DNR status due to being non-compliant at the hospital.
-The resident's paper chart showed he/she had a Full Code status, but had a DNR order on his/her TOS dated [DATE] when he/she was readmitted to the facility.
-They will search to see if a signed DNR form was received by the facility in the signed order forms from the physician received by the facility that day.
2. Record review of Resident #198's Face Sheet showed he/she was admitted to the facility on [DATE] with diagnoses of peripheral neuropathy (damage to the nerves resulting in sensory loss in the extremities).
Record review of the resident's Care Plan dated [DATE] showed no care plan for the resident's desired code status.
Record review of the resident's [DATE] POS showed no documentation related to the resident's desired code status.
Record review of the resident's electronic medical record showed he/she had a DNR status.
Record review of the resident's paper medical records chart showed:
-An Outside the Hospital Do Not Resuscitate Order signed by the resident on [DATE].
-The order was not signed by the resident's physician as of [DATE].
During an interview on [DATE] at 11:00 A.M. the resident said he wanted to have a DNR status.
During an interview on [DATE] at 11:02 A.M., CNA D said:
-The resident had a DNR order on his/her electronic medical record.
-He/she also had an Outside the Hospital DNR order on his/her paper chart.
-The resident's Outside the Hospital DNR was not signed by his/her physician.
During an interview on [DATE] at 11:08 A.M., the Social Service Designee said:
-A resident's code status is in both the electronic medical record and the paper medical record.
-The resident had a DNR order.
-The resident's DNR order was not signed by his/her physician, so the order was not valid at that time.
-The resident had signed his/her DNR order form on [DATE].
3. During an interview on [DATE] at 11:02 A.M., CNA D said:
-In the case of an emergency, he/she would look either in the resident's electronic medical record on the resident's profile section, or in the resident's paper medical record to find the resident's desired code status.
-The resident's electronic medical record and his/her paper medical record should show the same thing related to the resident's code status.
During an interview on [DATE] at 11:11 A.M., the Administrator and Social Service Designee said:
-A resident's current and accurate code status should be on the resident's POS.
-A resident's TOS orders should be accurately transcribed to the resident's POS.
-A resident's DNR order should be signed by his/her physician within 24 hours.
During an interview on [DATE] at 11:15 A.M., the MDS Coordinator said:
-The resident's care plan should accurately reflect the resident's code status.
-In the past, it was the medical records person's responsibility to ensure TOS orders were signed by the physician and returned to the facility timely.
During an interview on [DATE] tat 3:17 P.M., the Administrator and Director of Nursing (DON) said:
-A resident's DNR order should be signed by his/her physician within 24 hours.
-If the resident's physician was not able to sign the order within 24 hours, two nurses could take a telephone order for the DNR order, or the order could be faxed to the resident's physician for an immediate signature until he/she was able to come in to sign the form.
-Staff could also take the DNR order to the physician to have the physician sign the order.
-The resident's electronic medical record, TOS, POS, and paper medical record should all accurately reflect the resident's DNR status and should match.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure the Pre admission Screen and Resident Review (PASARR) Level ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure the Pre admission Screen and Resident Review (PASARR) Level II screening was obtained for one sampled resident (Resident #28), after the Level I screening identified the resident as having a mental condition requiring additional screening out of 16 sampled residents. The facility census was 55 residents.
1. Record review of Resident #28's Face Sheet showed he/she was admitted on [DATE] with diagnoses including schizoaffective disorder (a chronic mental health condition characterized primarily by symptoms of schizophrenia, such as hallucinations or delusions, and symptoms of a mood disorder, such as mania and depression), anxiety and psychosis (a severe mental disorder in which thought and emotions are so impaired that contact is lost with external reality).
Record review of the resident's quarterly Minimum Data Set (MDS a federally mandated assessment tool to be completed by facility staff for care planning) dated 9/19/19, showed the resident:
-Had severe cognitive incapacity and had no behaviors or mood disturbance.
-Needed supervision with transfers, but was independent with walking, bathing, dressing, grooming eating and toileting.
-Received anti-psychotic and anti-depressant medication.
Record review of the resident's PASARR Level I screening dated 9/25/19, showed the resident had:
-A major mental health disorder (diagnoses of schizoaffective disorder, psychotic disorder and anxiety disorder).
-Has had serious problems with level of functioning in the last six months.
-A level II screening was recommended to be completed.
Record review of the resident's Physician's Telephone Orders showed the following physician's orders:
-7/31/19 Risperdal (used to treat schizophrenia and bipolar disorder) 1 milligram (mg) twice daily for bipolar disorder (a mental health diagnoses for behavior that is characterized by periods of elevated or irritable mood (mania), alternating with periods of depression).
-8/7/19 increase Lexapro (used to treat depression) to 10 mg daily for schizophrenia (a severe mental disorder that can result in hallucinations, delusions, and extremely disordered thinking and behavior).
-8/13/19 discontinue Lexapro-start Cymbalta 30 mg daily for depression per psychiatric review
Record review of the resident's Care Plan dated 9/2019, showed the resident exhibits behavior symptoms such as socially inappropriate/verbally aggressive/abusive and physically aggressive/abusive behaviors related to Schizoaffective Disorder. Interventions showed staff would:
- On 6/20/2019 when placing a roommate, match with the same likes and dislikes to avoid conflict.
-Administer psychotropic meds as ordered.
-Determine cause of behavior and remove resident.
-Distract resident with activities of interest.
-Document all behaviors. Attempt to identify pattern to target interventions.
-Evaluate side effects of medications.
-Initiate psychiatric evaluation as needed.
-The resident prefers to stay in his room in bed with the blanket over his/her head.
-Modify the environment to reduce episodes of negative behavior and risk for fall or injury.
-Notify the physician of inappropriate behavior.
-Notify the physician of negative behavior or activity.
-Provide the resident an opportunity to express him/herself.
-Redirect negative behavior as needed.
-When aggressive behaviors start, place immediately on one to one, attempt to redirect, give medication as needed and allow time to work, when the resident is no longer aggressive you can discontinue one to one (monitoring). If unable to redirect send the resident to the hospital for evaluation and treatment.
-When the resident becomes agitated, remove him/her from the situation and offer one on one activities of choice.
During interview on 11/20/19 at 9:55 A.M., the MDS Coordinator said:
-The resident had been homeless and after he/her received the Public Administrator as Guardian, he/she was placed at the facility.
-The former Social Service Director was employed at the facility when the resident was admitted and was in charge of ensuring the PASARRs were obtained.
-The resident had the PASARR Level I screening completed but he/she was unable to locate a Level II screening and did not know if one had ever been completed on the resident.
-He/she did not know if the facility had contacted the Missouri Central Office Medical Review Unit (COMRU) to see if the resident had ever had a Level II screening completed or to have a Level II screening completed on the resident.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Record review of Resident #197's Face Sheet showed he/she was admitted to the facility on [DATE] and readmitted on [DATE] wit...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Record review of Resident #197's Face Sheet showed he/she was admitted to the facility on [DATE] and readmitted on [DATE] with the following diagnoses:
-Urinary Tract Infection (UTI - an infection of one or more structures in the urinary system).
-Pressure ulcer, unspecified stage.
-Right below the knee amputation.
-Left below the knee amputation.
-Colostomy.
-Major Depressive disorder.
-Anxiety.
-Paraplegia (loss of movement of both legs and generally the lower trunk).
Record review of the resident's Nursing Notes dated 8/25/19 showed:
-Staff attempted to access the resident's Port-a-cath with a 1 1/2 inch Huber needed (a special needle used to access port-a-cath) but was unsuccessful.
-The resident was sent to the hospital to access his/her port-a-cath.
-The resident returned to the facility, reporting the hospital used a smaller needed to access his/her port-a-cath.
Record review of the resident's Telephone Order Sheet (TOS) dated 9/27/19 showed an order for the resident to go the hospital to access his/her port-a-cath.
Record review of the resident's quarterly MDS dated [DATE] showed he/she:
-Was cognitively intact with a BIMS of 15 out of 15.
-Required total staff dependence for bed mobility, transfers, dressing, toileting, and personal hygiene.
-Had a urinary catheter and colostomy.
-Had Stage III pressure ulcer (a full thickness tissue loss. Subcutaneous fat may be visible but bone, tendon or muscle is not exposed. Slough may be present but does not obscure the depth of tissue loss. May include undermining or tunneling) and Stage IV pressure ulcer (Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present on some parts of the wound bed. Often includes undermining and tunneling).
Record review of the resident's October 2019 and November 2019 POS showed:
-Huber needle 20 gauge (g - the diameter size of the needle), 1 1/2 inches in length, use as directed.
--The 1 1/2 inches in length was crossed out and 1 inch in length was handwritten on the POS.
--No physician's order on the resident's TOS or POS to reflect the change from a 1 1/2 inch needle to a 1 inch needle.
-No documentation of a physician's order directing staff to change the dressing on the resident's accessed port-a-cath site or how often to change the dressing.
Record review of the resident's October 2019 and November 2019 Medication Administration Record (MAR) and Treatment Administration Record (TAR) showed:
-No orders to change the dressing on the resident's accessed Port-a-cath.
-No documentation by the facility staff the resident's accessed Port-a-cath dressing was changed.
Record review of the resident's Nursing Notes from 10/1/19-11/21/19 showed:
-No documentation by the facility staff the resident's accessed Port-a-cath site was assessed for signs and symptoms of infection.
-No documentation by the facility staff the resident's accessed Port-a-cath dressing was changed.
Observation on 11/20/19 at 1:28 P.M. showed the resident's transparent dressing covering his/her Port-a-cath was loose and dated 11/12/19.
During an interview on 11/20/19 at 1:30 P.M., LPN D said:
-The resident's Port-a-cath dressing was loose with the edges coming off and no longer adhering to the resident's skin.
-He/she had reported the resident's dressing not adhering to the resident's skin to the Registered Nurse (RN) so it could be changed since it was outside his/her scope of practice.
-The resident's Port-a-cath dressing had not been changed or reinforced yet.
-He/she thought it was supposed to be changed every three days and documented by the nurse on the resident's TAR.
-The resident's Port-a-cath dressing was dated 11/12/19.
During an observation of the resident and interview on 11/21/19 at 11:45 A.M., the Administrator said:
-He/she expected the ADON to monitor and document the Port-a-cath dressing change at least weekly.
-The resident should have orders for his/her Port-a-cath dressing change.
-He/she would expect the order to be on the resident's POS and transcribed to the resident's MAR/TAR.
-He/she would expect the Port-a-cath dressing change to be documented as completed on the resident's MAR/TAR.
-The resident's Port-a-cath dressing was dated 11/12/19.
-The resident's Port-a-cath dressing was peeling away from the resident and no longer adhering to the resident's skin.
Based on observation, interview and record review, the facility failed to ensure a physician's order for self-administration of medication kept at the bedside was obtained for one sampled resident who was a new admission (Resident #48); and to ensure a resident with a Port-a-cath (a device surgically implanted under the skin attached to a catheter [a thin, narrow tube] that is threaded into a large vein above the heart. It is used to deliver intravenous medications) had orders directing staff to change the transparent dressing to prevent infection for one sampled resident (Resident #197) out of 16 sampled residents. The facility census was 55 residents.
Record review of the facility's Self-Administration of Drugs policy and procedure dated November 2016, showed residents in the facility who wish to self-administer their medications may do so, if it is determined that they are capable of doing so and clinically appropriate. It showed:
-As part of their overall evaluation, the staff and practitioner will assess each resident's mental and physical abilities, to determine whether a resident is capable of self-administering medications and if such is clinically appropriate.
-In addition to general evaluation of decision making capacity, the staff and practitioner will perform a more specific skill assessment, including the resident's ability to read and understand medication labels; comprehension of the purpose and proper dosage and administration time for his/her medications; ability to remove medications from a container and to ingest and swallow them and the ability to recognize risks and major adverse consequences of his/her medications.
1. Record review of Resident #48's Face Sheet showed he/she was admitted on [DATE], with diagnoses including breast, bone and lung cancer, diabetes, indigestion, high cholesterol, atrial fibrillation (irregular heartbeat), asthma and high blood pressure.
Record review of the resident's Medical Record showed the resident did not have an admission Minimum Data Set (MDS a federally mandated assessment tool to be completed by facility staff for care planning) completed yet.
Record review of the resident's Physician's Order Sheet (POS) dated 11/1/19 to 11/30/19 showed there were no physician's orders for the resident to self-administer any prescribed medications and there were no physician's orders showing the resident could keep any medications at bedside.
Observation and interview on 11/19/19 at 6:55 A.M., showed the resident was sitting up in his/her recliner, dressed for the weather and without odors. The nurse was in his/her room administering the resident's medication. The resident complained of pain to his/her right heel. Licensed Practical Nurse (LPN) C assessed the resident's pain and gave him/her pain medication.
Observation and interview on 11/19/19 at 7:15 A.M., showed the Assistant Director of Nursing (ADON) was in the resident's room to provide wound assessment and care to the resident. The resident was sitting in his/her recliner and instructed the ADON to look in his/her dresser drawer for an ointment to place on his/her wound. The ADON was unable to find the ointment, but he/she found a small prescription box labeled Triamcinolone 0.1% with orders to spray in each nostril as needed, in the resident's drawer. The resident said it was a nasal spray he/she used for his/her allergies. He/she said he/she brought the medication in from home. The ADON said that he/she as unaware that the resident had this medication in his/her dresser drawer and had been self-administering it as needed. He/she said he/she would have to take the medication and give it to the nurse to put away and notify the physician to obtain an order for the resident to keep it at bedside.
During an interview on 11/21/19 at 12:48 P.M., the ADON said:
-He/she went back into the resident's room to look for the ointment he/she said he/she had to put on his/her wound and found the resident had Pluragel in his/her room, which is used for moisture and for debridement (removal of dead tissue to promote wound healing) of wounds, in addition to Triamcinolone that was in his/her dresser drawer.
-The resident and his/her family were putting that on his/her wound when the resident was at home.
-When a resident is admitted , if they have medications with them, they are to leave the medications with the nurse and then the Charge Nurse has to get an order from the physician for self-administration of medications.
-If the medication is not on their POS when they are admitted , the charge nurse has to notify the physician for clarification orders for the resident to have the medication.
-The nurse will complete a general assessment to see if the resident is able to self-administer medications.
-The resident did not have a physician's order for Pluragel or Triamcinolone, and did not have an order to self-administer them, so that was why he/she removed them from the resident's room.
-They did not know the resident had the medications in his/her room and will assess the resident's ability to self-administer medications.
-He/She informed the resident that the resident could not have medications in his/her room.
During an interview on 11/21/19 at 2:23 P.M., the Administrator and Director of Nursing (DON) said:
- If a resident comes into the facility with medications from home. they only accept medications from home that they (the facility) have orders for.
-When they complete the resident's inventory, they go through the resident's belongings with the resident and if they discover medications at that time, that they don't have order for, they will call the family and have them pick the medications up.
-If they have orders for the medications, they will take the medications and put them in the medication cart after verifying the medications with the physician.
-The resident should not have had medications in his/her room that the nursing staff was unaware that he/she had.
-Nursing staff should have assessed the resident to self-administer medications.
-The resident should have orders to self-administer medications and it should be on his/her POS.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Record review of Resident #31's admission Face Sheet showed he/she was admitted to the facility on [DATE] and readmitted on [...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Record review of Resident #31's admission Face Sheet showed he/she was admitted to the facility on [DATE] and readmitted on [DATE] with the following diagnosis:
-Necrotizing Fascitis (an infection that results in the death of parts of the body's soft tissue).
-Non-pressure chronic ulcer right foot with necrosis of muscle (sore with blacking/ death of tissue and muscle).
-Sepsis (infection) following a procedure.
-Gangrene of extremities (a type of tissue death caused by a lack of blood supply).
-Left leg above knee amputation (surgical removal of a limb).
Record review of the resident's 5 day MDS assessment dated [DATE] showed he/she:
-Was cognitively intact.
-Was able to understand others and was able make his/her needs known.
-Required assistance of two staff for transfer.
-Was at risk for pressure ulcers (injuries to skin and underlying tissue resulting from prolonged pressure on the skin, they most often develop on skin that covers bony areas of the body, such as the heels, ankles, hips and tailbone) or skin issues.
-Had an infected open area on his/her foot.
-Was receiving dressing changes.
Record review of the resident's Physician Telephone Order (PTO) dated 10/4/19 showed to cleanse the wound between the 4th and 5th toes (did not indicate which foot) with wound cleanser, then apply xeroform and lightly wrap with gauze.
Record review of the resident's POS dated 10/1/19 to 10/31/19 showed no physician order for wound care.
Record review of the resident's POS dated 11/1/19 to 11/30/19 showed no new or old physician's order for wound care to the resident's right foot.
Record review of the resident's Medication Administration Record (MAR) dated November 2019 showed he/she:
-Had order for Augmentin (is a prescription medication that's used to treat infections caused by bacteria) 500-125 milligram (mg) by mouth for seven days for infections.
- Had the last dose on 11/13/19 for a diagnosis of Gangrene.
Record review of the resident's November 2019 TAR showed to cleanse between the resident's little toe and 4th toe with wound cleanser on his/her right foot, then place a folded 4 x 4 gauze pad between the toes was transcribed on to the TAR on 11/13/19.
Record review of the resident's progress note dated 11/6/19 at 10:09 P.M. showed:
-He/she had arrived back to the facility at 5:00 P.M.
-Had a order for an antibiotic for the wound on the right little toe.
-Had a small wound noted between the little toe and forth toe that had a small amount of purulent (containing pus) drainage.
-No dressing was in place and the facility had no orders for treatment from the hospital.
-The resident said it was to be left open to air.
-No documentation that staff had verified the physician orders with the hospital or the resident's physician upon readmission.
Record review of the resident's progress notes from 11/6/19 to 11/12/19 showed:
-No documentation related to verifying with the resident's physician or the hospital physician the discharge plan of care related to the monitoring and treatment of the infected wound on the resident's right little toe and forth toe.
-The wound had been left open to air as documented in nursing progress notes.
Record review of the resident's progress note dated 11/13/19 at 8:56 P.M. showed:
-New treatment order received for his/her little toe on right foot.
-Did not have detailed instructions on how the physician prescribed the wound care treatment.
During an interview on 11/17/19 at 5:40 P.M., in main dining room the resident said:
-He/she came to the facility with gangrene in his/her left leg.
-He/she had to have his/her left leg amputated due to the gangrene.
Observation on 11/17/19 to 11/19/19 of the resident wound care showed multiple attempts were made to observe the wound care and dressing change but resident was not available or the wound care and dressing change had been completed.
Record review of the resident's Daily Pressure Injury Documentation dated 11/19/2019 at 5:02 P.M., showed:
-The resident had a wound on his/her right toes and a dressing was present.
-Gangrene was listed as the description of the wound.
-The dressing was changed and the area was dry and intact.
-No other comments or detailed description of the wound was documented.
During an interview on 11/20/19 at 3:30 P.M., LPN A said:
-His/her normal duties was the desk nurse which included the assessment of residents on Medicare skilled services and other medical assessment as needed.
-The Charge Nurses were assigned the resident's Weekly Skin Assessment and the facility's wound nurse did the resident's Weekly Skin Conditions Wound Assessment.
-He/she would expect to have a physician's order for treatment of the resident's wounds.
-Should had a written physician order if had a received a telephone order or if on site physician order obtained.
-When receive a physician's order should had been transcribed to the resident's POS and to his/her TAR or MAR.
Observation on 11/20/19 and 11/21/19 of the resident wound care showed multiple attempts were made to observe the wound care and dressing change but the resident was not available or the wound care and dressing change had been completed.
During an interview on 11/21/19 at 12:25 P.M., the resident said:
-He/she had a wound on his/her right foot and nursing staff had been changing the dressing daily.
-Staff clean the area first, then place the dressing between the toes.
-The wound on his/her toes was getting better.
-He/she had not had the dressing change done today.
-He/she was not in his/her room much as he/she participated in most facility activities, and smoked outside.
-He/she was getting ready to go out side to smoke.
During interview and record review on 11/21/19 10:10 A.M., LPN D said:
-The resident should have an order for wound treatment.
-Staff should document the wound care on the resident's TAR.
-Staff should not provide care without a physician's order and if not transcribed onto the resident's MAR or TAR.
-Staff should call to verify orders or obtain physician's orders for wound care/treatment and then transcribe the order to the resident's POS, TAR and MAR.
-During end of the month change over, the DON and the ADON would review the resident's POS, TAR and MAR to ensure physician's orders had been transcribed.
-He/she should have verified the resident's physician orders and not provided wound care or treatment to the resident's wound without a physician order.
During an interview on 11/21/19 at 2:17 P.M. the DON and Administrator said:
-When they receive a physician's telephone order, nurses write the order on the POS, the MAR and the TAR.
-On the following morning the DON and other administrative staff check the orders during the morning meeting to ensure the orders were correct and the medications and treatment supplies were obtained.
-The DON and other administrative staff go over the POS, MAR and TAR when there are new orders that come in, to ensure all orders are being accurately transcribed on all three documents and they compare to ensure they are accurate and transcribed correctly.
-The reconciliation of the POS's are done at the end of the month by the DON, ADON and MDS Coordinator.
-He/she would expect to have a physician's order prior to providing wound care or treatment.
-Physician's orders for wound care should have been obtained and should be transcribed onto the resident's POS and TAR.
-He/she expected staff to follow those physician's orders for treatment and care.
-Documentation should be on the TAR showing the treatments were completed as ordered.
-If nursing staff see a wound during the skin or wound assessment, he/she expected nursing staff to call the physician and obtain an order for treatment.
-The nursing staff should document the new and changing skin or wound issue and should be descriptive in documentation to show what it looked like and to include measurements of the wound.
-Documentation should be in the weekly skin assessment document and in nursing progress notes.
-The nurses were responsible for completing the weekly skin assessments and they should be comprehensive in documenting skin issues if the resident had a skin concern.
-The Wound Nurse was responsible for completing the Weekly Skin Conditions Wound Assessment for residents with wounds and the staff should be comprehensive in documenting detailed descriptions of the wound and include measurements.
-He/she expected the wound nurse to be responsible for monitoring and tracking the resident's status with skin issues or wounds to include current physicians order and documentation.
3. Record review of Resident #36's admission face sheet showed he/she was admitted on [DATE] with the following diagnoses Arthritis (joint pain) and depression.
Record review of the resident's Plan of Care dated 7/22/19 showed:
The resident had a potential nutritional problem related to Hypokalemia ( blood's potassium levels are too low).
-Monitor weight monthly and maintain five percent gain or loss through the next review.
Record review of the resident's telephone order dated 7/25/19 showed an order for support stockings.
Record review of the resident's admission POS dated 7/25/19 showed the following orders:
-Lasix (used to treat edema (swelling) 40 mg, give 1 tablet by mouth at 8:00 A.M. and 12:00 P.M. for edema.
-Daily weights and support stockings.
Record review of the resident's Care Plan dated July 2019 showed no documentation to include monitoring for edema or use of support stockings.
Record review of the resident's POS dated 8/1/19 to 8/31/19 showed:
-Lasix 40 mg give 1 tablet by mouth 2 times a day for edema with an order date of 7/25/19.
-No orders transcribed for support stockings or documentation showing they had been discounted.
Record review of the resident's TAR dated September, October and November 2019 showed the TAR was blank.
Record review of the resident's POS for September and October 2019 showed no orders transcribed for support stockings or documentation showing they had been discounted.
Record review of the resident's POS dated 11/1/19 to 11/31/19 showed:
-Lasix 40 mg give 1 tablet by mouth two times a day for edema.
-His/her diet order was a Regular Texture, 2 Gram Low Sodium diet.
-No physician's order for support stockings or [NAME] hose.
During an interview on 11/17/19 at 9:05 A.M., the resident said:
-He/she had concerns with the edema in his/her legs.
-He/she had support knee high stockings in place.
Observation on 11/19/19 at 10:19 A.M. showed the resident had support stocking in place for edema.
During interview and record review on 11/21/19 at 10:10 A.M., LPN D said:
-The resident should have a physician's order and document care on the resident TAR for support hose.
-He/she had monitored the resident for edema in the past, but he/she did not always document the care provided in the resident's medical chart.
-He/she may not know where to document the information of the care or treatment provided due to not transcribed onto the resident's TAR or MAR.
During an interview on 11/21/19 10:20 A.M., Certified Nursing Assistant (CNA) A said:
-He/she reviewed the resident's care plan to check for the type of care to provide for the resident.
-The CNA's document in the electronic record and have some paper records.
-He/she weighs the residents.
-He/she did not think the resident's weight had increased more than two to five pounds depending on fluid due to his/her edema.
-The resident was able to make his/her needs known and was able to put own support stockings on.
-The resident's legs have been swollen for a while and nursing was aware.
Observation on 11/21/19 at 10:25 A.M. showed:
-The resident did not have support stockings on.
-He/she did not have any weeping or open areas on his/her legs.
During an interview on 11/21/19 at 10:25 A.M., the resident said:
-He/she was not able to find the support stockings in his/her room.
-He/she was not sure where he/she put them.
-The staff monitor his/her weight as needed.
-The CNA's assist him/her put on the stockings when he/she request assistance.
-He/she put the support stockings on as he/she needed them or wanted them on.
-The nursing staff and CNA's sometime look at at the swelling of his/her legs during showers.
-He/she had no weeping or open area on his/her legs.
During an interview on 11/21/19 at 2:17 P.M., the DON and Administrator said he/she would expect:
-Staff to have a physician's order for preventative measures and treatment of edema.
-Staff to have a physician's orders for monitoring edema and placement of support stocking.
-Documentation to be on the TAR showing the treatments were completed as ordered.
-A resident to have a care plan that addresses monitoring for and treatment of edema.
Based on observation, interview and record review, the facility failed to ensure physician's wound treatment orders were followed and documented as administered; to ensure the resident's wound care interventions were on the resident's comprehensive care plan for one sampled resident who was admitted with a surgical wound (Resident #45); to ensure physician's wound treatment orders were transcribed to the resident's current Physician's Order Sheet (POS) for two sampled resident's (Residents #45 and #31); to ensure physician's orders for monitoring edema and treatment of support hose were transcribed to the POS and Treatment Administration Record (TAR) and documented as administered, and to ensure the resident's edema care interventions were on the resident's comprehensive care plan for one sampled resident (Resident #36) out of 16 sampled residents. The facility census was 55 residents.
Record review of the facility's Wound Care Guidelines policy and procedure dated May 2013, showed the purpose was to provide guidelines for the care of wounds. The preparation for caring for wounds showed staff should:
-Verify that there is a physician's order for treatment.
-Review the resident's care plan to assess any special needs of the resident.
-Assemble equipment and supplies as needed
-The procedure detailed steps in providing wound care, but did not address assessment or documentation protocols.
1. Record review of Resident #45's Face Sheet showed he/she was admitted to the facility on [DATE], with diagnoses including left hip fracture (with an artificial left and right hip joint), high blood pressure, anemia (low iron) dementia, cardiomyopathy (a disease of the heart muscle that makes it harder for your heart to pump blood to the rest of your body) and muscle weakness.
Record review of the resident's Nursing admission assessment dated [DATE] showed the resident's general overall skin condition was pale, warm with normal skin turgor. It showed the resident had a surgical wound to his/her left hip. There was no additional documentation showing any treatment orders.
Record review of the resident's POS dated 10/17/19, showed physician's orders to cleanse the resident's hip incision with wound cleanser, pat it dry, and apply border gauze (an absorptive dressing that consists of three layers to ensure wound healing) daily until healed.
Record review of the resident's initial Care Plan dated 10/18/19, showed:
-The resident was at risk for skin issues.
-Staff was responsible for inspection and documentation of skin.
-Incontinence care and skin treatments were to be completed as ordered.
-The Care Plan did not show the resident was in the facility for rehabilitation after hip surgery and it did not show the resident had an incision that required treatment daily.
Record review of the resident's admission Minimum Data Set (MDS-a federally mandated assessment tool to be completed by facility staff for care planning) dated 10/30/19, showed he/she:
-Had severe cognitive impairment.
-Needed extensive assistance for bed mobility, transfers, dressing, bathing, and toileting.
-Was at risk for developing wounds.
-Had a surgical wound and received surgical wound care to include the application of surgical dressings and application of ointments.
-Also received preventive interventions such as a pressure relieving device for his/her bed and chair, turning and repositioning program and nutrition/hydration interventions to manage skin problems.
Record review of the resident's Daily Pressure Injury Documentation dated 10/18/19, 10/19/19, 10/20/19, 10/21/19, and 10/22/19, showed:
-A dry intact odorless dressing was present.
-There were no additional comments documented.
-There was no documentation showing the dressing had been changed or that the treatment had been completed on those dates. There was no description showing what the progression of the incision was, what the incision looked like or if the incision was healing/healed.
Record review of the resident's TAR dated 10/17/19 to 10/31/19, showed:
-A physician's order instructing nursing staff to cleanse the resident's hip incision with wound cleanser, pat it dry and apply border gauze daily, until healed.
-Treatments were not administered from 10/17/19 to 10/25/19 (there were no initials on each date showing treatments were administered).
-Nursing staff documented they administered the treatment every day from 10/26/19 to 10/31/19 except on 10/28/19.
-Did not show why wound treatment was not administered to the resident on the dates that were not initialed.
Record review of the resident's Nursing Notes from 10/17/19 to 10/31/19 showed there were no nursing notes that the resident received any wound care treatment from 10/17/19 to 10/25/19. There were no notes showing any wound care treatments or description of the resident's incision or healing process.
Record review of the resident's Weekly Skin Evaluation dated 10/24/19 and 10/31/19, showed the resident's skin was dry and intact and the resident had no open areas. There was no documentation identifying the resident's incision on his/her left hip or that he/she was receiving treatments for it.
Record review of the resident's POS dated 11/1/2019 to 11/30/19, showed there were no treatment orders for the resident's surgical hip wound documented and there were no physician's orders showing the resident's wound care treatment had been discontinued.
Record review of the resident's Comprehensive Care Plan dated 11/7/19, showed the resident had fall/gait and balance problems and showed interventions to help with preventing falls. It did not show the resident had a surgical wound due to hip surgery. It did not show when the resident's incision was healed and did not show any after care to the site.
Observation and interview on 11/19/19 at 6:47 A.M., showed the resident was up and dressed for the weather sitting in his/her wheelchair, groomed without odor. The resident was pleasantly confused and said he/she was here for rehabilitation and was waiting for his/her spouse because he/she was leaving today to go home (the resident was not discharging to go home). At 6:52 A.M., nursing staff came to give the resident his/her medication. The resident was able to self-propel in and around the facility without assistance. At this time observation of his/her incision site was not completed. Nursing staff said the resident no longer had a wound at his/her left hip.
During an interview on 11/20/19 at 4:00 P.M., Licensed Practical Nurse (LPN) D said:
-When a resident is admitted , the nurse who is completing the admit is supposed to complete a comprehensive evaluation of the resident to include the physical and skin evaluation within four hours of the residents admission.
-During the assessment, they should see if a resident has a wound and if so, the nurse should measure it and document what they saw, cover it and notify the wound care nurse.
-If the resident came in with orders for treatment the can use those orders until the wound nurse sees the resident If the resident did not have orders,the nurse should notify the physician to obtain orders for treatment of the wound within the four hour admission period.
-The resident's care plan should show that the resident has a wound and treatment orders until the comprehensive care plan is developed and the comprehensive care plan should show that the resident had a wound and received treatment for it. It should show interventions for care and treatment.
During an interview on 11/21/19 at 12:48 P.M., the Assistant Director of Nursing (ADON) said:
-He/she was also the Wound Care Nurse in the facility.
-When they have a new admission, the charge nurse completes the initial assessment of the resident and they should complete a full body assessment.
-If they see any skin issues, they are to document it on the initial assessment in the skin section and notify him/her.
-He/she will then complete a wound assessment and and if there are no orders for wound care, he/she will notify the physician for orders and then he/she will start weekly wound assessments.
-If the resident had physician's orders upon admission, he/she will verify those orders with the physician.
-There should be documentation showing the resident had a wound, and treatment should be initiated within 24 hours.
-A resident with a physician's order for wound care should receive their ordered treatment within 24 hours.
-He/she should be notified of all wounds ore pressure sores.
-If wound treatment is not given, there should be documentation showing why it was not given.
-It should be documented that treatment was offered and why it was was not administered on the TAR.
-He/she was unaware that Resident #45's treatment record showed no treatments were administered until 11/25/19.
-Documentation showing what the wound looked like, measurements and overall assessment should have also been in the resident's nursing notes.
During an interview on 11/21/19 at 2:23 P.M., with the Administrator and Director of Nursing (DON):
-The DON said there should be a full body assessment completed upon admission and it should show any wounds on the resident or any skin concerns.
-If nursing staff see a wound during the assessment, nursing staff should call the physician and obtain an order for treatment.
-The documentation of the wound should be descriptive to show what it looked like and include measurements. Documentation should be in the initial admission assessment, and on the weekly skin assessment document.
-The nurse is responsible for completing the weekly skin assessments and they should be comprehensive and show/describe the skin issue if the resident has a skin concern.
-Physician's orders for wound care should be obtained, should be documented on the resident's POS and TAR and he/she expects staff to follow those orders.
-She said documentation should be on the TAR showing the treatments were completed as prescribed and if they are unable to complete the treatment, nursing staff should document the reason on the back of the TAR.
-The Administrator said it seems a full body assessment is not being done on admission or with re-admissions.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. Record review of Resident #41's admission Face Sheet showed he/she was admitted on [DATE] and readmitted on [DATE] with the f...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. Record review of Resident #41's admission Face Sheet showed he/she was admitted on [DATE] and readmitted on [DATE] with the following diagnoses:
-Benign Prostatic hyperplasia with lower urinary track symptoms (BPH enlarged prostate with difficulty in urination).
-Neuromuscular Dysfunction of Bladder (neurogenic bladder when a person lacks bladder control due to a brain, spinal cord, or nerve condition).
-Has a supra pubic catheter and a colostomy.
Record review of the resident's Quarterly MDS dated [DATE] showed he/she:
-Was severely cognitively impaired and had short term and long term memory problems.
-He/she was able to understand others and make his/her needs known.
-Required total assistance for staff for all cares and transfers.
-Had a diagnosis of neurogenic bladder.
-Had an indwelling catheter and colostomy.
Record review of the resident's TAR and MAR dated 10/1/19 to 10/31/19 showed no detailed physician's order for supra pubic catheter site care, monitoring and changing urinary drainage bag.
Record review of the resident's nursing progress notes dated 10/1/19 to 11/19/19 showed no documentation related to the monitoring and care of the resident's supra pubic catheter.
Record review of the resident's personalized Care Plan as of 11/19/19 showed no plan of care for the supra pubic catheter site cleaning, monitoring and changing, care or emptying of the urinary drainage bag.
Record review of the resident's POS dated 11/1/19 to 11/30/19 showed no detailed physician's order for supra pubic catheter site care, monitoring and changing urinary drainage bag.
Record review of the resident's TAR and MAR dated 11/1/19 to 11/30/19 showed no detailed physician's order for supra pubic catheter site care, monitoring and changing urinary drainage bag:
Observation on 11/17/19 at 3:41 P.M., showed:
-The resident was laying in bed with his/her eyes open, but did not respond when asked a question.
-The urinary drainage bag and tubing were lying on the floor not in a dignity bag.
-The urinary drainage bag had 350 cubic centimeter (cc) of urine inside the bag that was the color of apple juice.
-There was an open container of personal care wipes at the foot of his/her bed.
-There was an uncovered graduate measuring container on the back of the toilet.
Observation on 11/18/19 at 1:10 P.M., showed the resident had a supra pubic catheter.
Record review of the resident's Weekly Skin Condition Report (Pressure and Non Pressure Combined) dated 11/19/2019 10:33 showed no documentation related to the resident's supra pubic site.
Observation on 11/20/19 at 3:25 P.M., showed:
-The resident was reclined in his/her broda chair (a specialized wheelchair) by the nurse's station most of the day.
-He/she had a catheter bag in a dignity bag.
During an interview on 11/21/19 at 10:20 A.M., Certified Nurses Aide (CNA) A said the resident's catheter bag should be placed in privacy bag and not touching the floor.
During an interview and record review on 11/21/19 at 10:10 A.M., Licensed Practical Nurse (LPN) D said:
-The resident should have a physician's order for catheter care and should document care on the resident's TAR.
-He/she had cleaned the resident's supra pubic site with wound cleanser and then applied a gauze pad.
-He/she had not been documenting care on the resident's TAR.
-The resident's current POS did not have a physician's order for the supra pubic catheter.
-Staff should not provide care without a physician's order and if not transcribed on the MAR or TAR.
-If a resident does not have orders, staff should obtain orders for supra pubic catheter care and then transcribe the orders to the resident's TAR.
During an interview on 11/21/19 at 2:17 P.M. the DON and Administrator said:
-When staff receive a physician's telephone order, nurses write the order on the POS, the MAR and TAR.
-On the following morning the DON and other administrative staff check the orders during the morning meeting to ensure the orders are correct and the medications and treatment supplies were obtained.
-They go over the POS, MAR and TAR when there are new orders to ensure all orders are being accurately transcribed on all three documents and they compare to ensure they are accurate and transcribed correctly.
-The reconciliation of the POS's are done at the end of the month by the DON, ADON and MDS Coordinator.
-He/she would expect to have physician order prior to providing catheter care or treatment.
-Physician's Orders for catheter care should have been obtained and should have been transcribed onto the resident's POS and TAR.
-He/she expects staff to follow physician's orders for treatment and care.
-Documentation should be on the TAR showing the treatments were completed as ordered.
-The urinary drainage bag should be stored in a dignity bag.
-The urinary drainage bag and catheter tubing should not be touching the floor.
Based on observation, interview and record review, the facility failed to obtain a physician's order for a suprapubic catheter (a urinary bladder catheter inserted through the skin about one inch above the symphysis pubis) to include the reason for a suprapubic catheter, to obtain a physician's order for the care of the resident's suprapubic catheter for three sampled residents (Resident #40, #197, and #41), and to ensure proper placement of the resident's catheter bag for two sampled resident's (Resident #197 and #41), out of 16 sampled residents. The facility census was 55 residents.
Record review of the facility Indwelling Urinary Catheter Policy revised on November 2017 showed:
-Cover the urine bag to provide privacy.
-Drainage bag and tubing are to kept of the floor.
1. Record review of Resident #40's Face Sheet showed he/she was admitted to the facility on [DATE] and readmitted on [DATE] with the following diagnoses:
-Anxiety disorder.
-Pressure ulcer (localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear and/or friction) of sacral region (tailbone), unstageable (Full thickness tissue loss in which the base of the ulcer is covered by slough [necrotic/avascular tissue in the process of separating from the viable portions of the body & is usually light colored, soft, moist, & stringy] and/or eschar (tan, brown or black) in the wound bed).
-Bipolar disorder (mood disorders characterized usually by alternating episodes of depression and mania).
-Major Depressive Disorder.
-Neuromuscular dysfunction of the bladder.
Record review of the resident's August 2019, September 2019, and October 2019 Physician's Order Sheet (POS), Medication Administration Record (MAR) and Treatment Administration Record (TAR) showed:
-No order for a suprapubic catheter, including a reason for the suprapubic catheter.
-No order for suprapubic catheter care.
-No documentation by the facility staff of providing suprapubic catheter care.
Record review of the resident's annual Minimum Data Set (MDS - a federally mandated assessment instrument completed by facility staff for care planning) dated 10/20/19 showed he/she:
-Was cognitively intact with a Brief Interview for Mental Status (BIMS) of 15 out of 15.
-Required extensive staff assistance with bed mobility, transfers, dressing, toileting, and personal hygiene.
-Had a urinary catheter and colostomy (an alternative exit from the colon created to divert waste through a hole in the colon and through the wall of the abdomen).
-Had no pressure ulcers or skin issues.
Record review of the resident's November 2019 POS, MAR, and TAR showed:
-No order for a suprapubic catheter, including a reason for the suprapubic catheter.
-No order for suprapubic catheter care.
-No documentation by the facility staff of providing suprapubic catheter care.
Observation on 11/20/19 at 10:46 A.M., showed the resident had a suprapubic catheter.
2. Record review of Resident #197's Face Sheet showed he/she was admitted to the facility on [DATE] and readmitted on [DATE] with the following diagnoses:
-Urinary Tract Infection (UTI - an infection of one or more structures in the urinary system).
-Pressure ulcer, unspecified stage.
-Right below the knee amputation.
-Left below the knee amputation.
-Colostomy (surgical operation in which a piece of the colon is diverted to an artificial opening in the abdominal wall).
-Major Depressive disorder.
-Anxiety.
-Paraplegia (loss of movement of both legs and generally the lower trunk).
Record review of the resident's quarterly MDS dated [DATE] showed he/she:
-Was cognitively intact with a BIMS of 15 out of 15.
-Required total staff dependence for bed mobility, transfers, dressing, toileting, and personal hygiene.
-Had a urinary catheter and colostomy.
-Had Stage III pressure ulcer (a full thickness tissue loss. Subcutaneous fat may be visible but bone, tendon or muscle is not exposed. Slough may be present but does not obscure the depth of tissue loss. May include undermining or tunneling) and Stage IV pressure ulcer (Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present on some parts of the wound bed. Often includes undermining and tunneling).
Observation on 11/19/19 at 8:33 A.M., 10:15 A.M., and 2:30 P.M. showed:
-The resident was in his/her room in bed.
-His/her Foley catheter bag was hanging from the side of the bed without a dignity bag.
-The resident's uncovered Foley catheter bag was touching the floor.
3. During an interview on 11/21/19 at 3:12 P.M., the Administrator and Director of Nursing (DON) said:
-A resident should have an order for catheter care.
-A resident should have an order for a suprapubic catheter, including the reason for the suprapubic catheter.
-The catheter bag and/or tubing should never touch the floor.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to complete a comprehensive pain assessment once one samp...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to complete a comprehensive pain assessment once one sampled resident (Resident #29) began having chronic pain and to ensure documentation was completed upon administration of as needed (PRN) pain medication, to include the date, time, reason for administering pain medication, pain intensity assessment before and after administration and non-pharmacological interventions for two sampled residents (Resident #28 and #29) out of 16 residents. The facility census was 55 residents.
Record review of the facility's Pain Assessment and Management policy and procedure dated October 2010, showed the purpose was to help staff identify pain in the resident and to develop interventions that are consistent with the resident's goals and needs and that address the underlying causes of pain. The procedure instructed staff to:
-Conduct a comprehensive pain assessment upon admission to the facility, at the quarterly review, whenever there is a significant change in condition and when there is an onset of new pain or worsening of pain.
-Assess the resident's pain and consequences of pain at least each shift for acute pain or significant changes in levels of chronic pain and at least weekly in stable chronic pain.
-During the comprehensive pain assessment, gather the following information as indicated from the resident or responsible party: a history of pain and treatment, including pharmacological and non-pharmacological interventions; characteristics of pain (intensity, description of pain, pain pattern, location and radiation of pain, frequency, timing and duration); impact on quality of life;factors that precipitate or exacerbate pain; strategies that reduce pain and symptoms that accompany pain.
-Documentation: Document the resident's level of pain with adequate detail as necessary and in accordance with the pain management program. Upon completion of the pain assessment, the person conducting the assessment shall record the information obtained from the assessment in the resident's medical record.
-Pain Management interventions shall be consistent with the resident's goals for treatment. They shall reflect sources, type and severity of pain. They shall address the underlying causes of the resident's pain.
-Non-pharmacological interventions may be appropriate alone or in conjunction with medications.
1. Record review of Resident #28's Face Sheet showed he/she was admitted on [DATE] with diagnoses including schizoaffective disorder (a chronic mental health condition characterized primarily by symptoms of schizophrenia, such as hallucinations or delusions, and symptoms of a mood disorder, such as mania and depression), anxiety and psychosis (a severe mental disorder in which thought and emotions are so impaired that contact is lost with external reality).
Record review of the resident's Pain assessment dated [DATE], showed the resident had no current complaints of pain.
Record review of the resident's Care Plan dated 9/19/19, showed the resident had an alteration in his/her cardiovascular function related to complaints of chest wall pain. Interventions showed nursing staff would:
-Administer medications as prescribed.
-Assess for signs and symptoms of cardiac decompensation and report to the physician.
-Minimize agitation or situations which cause anxiety.
Record review of the resident's quarterly Minimum Data Set (MDS-a federally mandated assessment tool to be completed by facility staff for care planning) dated 9/19/19, showed the resident:
-Had severe cognitive incapacity and had no behaviors or mood disturbance.
-Needed supervision with transfers, but was independent with walking, bathing, dressing, grooming eating and toileting.
-Did not have pain and did not receive any scheduled or prn pain medication during the review period.
Record review of the resident's Physician's Order Sheet (POS) dated 11/1/19 to 11/30/19, showed physician's orders for:
-Tramadol (an opioid pain medication used to treat moderate to severe pain) HCL 50 milligrams (mg) every six hours as needed for pain (The original order was dated 8/26/19).
Record review of the resident's Medication Administration Record (MAR) showed:
-September 2019 the resident was administered Tramadol on 22 days (out of 30 days).
--Documentation on the MAR showed the nurse documented the resident's pain intensity level prior to administering Tramadol, where the resident's pain was located, any non-pharmacological interventions initiated, and the resident's pain intensity level after Tramadol was administered only 14 times Tramadol was administered to the resident.
-October 2019 the resident was administered PRN Tramadol on 21 days (out of 31 days).
--The documentation on the MAR did not show the resident's pain intensity level prior to administering Tramadol, where the resident's pain was located, any non-pharmacological interventions initiated, or the resident's pain intensity level after Tramadol was administered to the resident.
-November 2019 the resident was administered PRN Tramadol on 15 days (out of 30 days).
--The documentation on the MAR did not show the resident's pain intensity level prior to administering Tramadol, where the resident's pain was located, any non-pharmacological interventions initiated, or the resident's pain intensity level after Tramadol was administered to the resident.
Record review of the resident's nursing notes from 9/1/19 to 11/18/19, showed there was no documentation showing the frequency the resident requested pain medications, the assessment of the resident's pain each time he/she requested pain medications or the nursing assessment of the resident's pain when he/she requested pain medications.
Observation on 11/18/19 at 11:18 A.M., showed the resident was standing in the hallway dressed for the weather. He/She was groomed and was not odorous. He/she was ambulatory without an assistive device and said he/she was doing fine (his/her speech was difficult to understand, but nursing staff was able to communicate with him/her and he/she was able to make his/her needs known). He/she showed no signs or symptoms of pain.
2. Record review of Resident #29's Face Sheet showed he/she was admitted to the facility on [DATE], with diagnoses including high blood pressure, indigestion, stroke, high cholesterol, lung cancer and pain.
Record review of the resident's Pain assessment dated [DATE], showed the resident had no complaints of pain during the assessment period. The document showed the rest of the form was not completed.
Record review of the resident's Medical Record showed there were no additional pain assessments in the resident's medical record after the resident began having pain and taking pain medication.
Record review of the resident's quarterly MDS dated [DATE], showed the resident:
-Was cognitively intact and had no memory problems.
-Was independent with dressing, toileting, eating, grooming; needed supervision with bathing and used a wheelchair for mobility.
-Did not have pain and did not receive any pain medication during the assessment period.
Record review of the resident's POS dated 11/1/19 to 11/30/19, showed the following physician's orders:
-Fentanyl patch (an opioid pain medication applied to the skin in a patch) 50 mg change every 72 hours (discontinued on 11/5/19).
-Hydrocodone (Norco) 10/325 mg give two tablets every 6 hours as needed for pain (initially ordered on 10/25/19).
-Roxanol (morphine a pain medication) 0.25 milliliter (ml) to 1 ml every hour for pain (ordered on 11/10/19).
-Oxycontin (a time release morphine like pain medication) 10 mg every 12 hours for pain (10/22/19).
Record review of the resident's Nursing Notes showed:
-10/19/19-the nurse documented the resident had complained of pain constantly at 8/10 (on the pain scale,10 represents intense pain) despite pain medication. He/she called hospice and received a physician's order to increase the Roxanol to Roxanol 20mg/ml-give 0.25-1 ml every two hours PRN for pain. He/she documented the resident tolerated Roxanol 0.5ml and reported his/her pain intensity at 5/10 and his/her pain was much more tolerable.
-11/5/2019 the nurse documented the resident complained of severe pain that was not relieved by his/her current pain regimen. Hospice was notified and the nurse received new physician's orders to increase Roxanol to every hour as needed. and to increase Hydrocodone to one to two tablets every four hours as needed. The note showed pain medication was administered as ordered and the resident was resting quietly in bed at this time.
-There were no additional notes showing the resident's pain intensity level before and after each PRN pain medication administration.
Record review of the resident's MAR dated 10/1/19 to 10/31/19 showed physician's orders for Oxycontin 20 mg twice daily for pain (start date 10/10/19 to discontinue date 10/25/19 and reordered from 10/25/19 to 10/31/19); Norco 7.5/325 mg give two tablets every four hours as needed for pain; Roxanol 20 mg/ml give 0.25 ml sublingually (under the tongue) every four hours as needed for pain and Roxanol 20 mg/ml give 0.25 ml sublingually every two hours as needed for pain. The MAR showed:
-Scheduled Oxycontin was administered as ordered.
-PRN Norco was administered on 20 days from 10/10/19 to 10/31/19.
-PRN Roxanol was administered 14 days from 10/12/19 to 10/31/19.
-The MAR showed the nurse only documented the resident's pain intensity level prior to administering pain medication, where the resident's pain was located, any non-pharmacological interventions initiated, or the resident's pain intensity level after pain medication was administered to the resident on three dates that he/she administered pain medication to the resident.
Record review of the resident's MAR dated 11/1/19 to 11/30/19, showed physician's orders for Hydrocodone 10/325 mg give one to two tablets every six hours as needed for pain (ordered on 10/25/19-the order was changed on 11/5/19 to show Hydrocodone 10/325 mg every four hours as needed for pain); and Roxanol 0.25 ml to 1 ml every hour as needed for pain. The MAR showed:
-PRN Hydrocodone was administered to the resident on 14 days from 11/1/19 to 11/18/19.
-PRN Roxanol was administered to the resident on 16 days from 11/1/19 to 11/18/19.
-The documentation on the MAR did not show the resident's pain intensity level prior to administering pain medication, where the resident's pain was located, any non-pharmacological interventions initiated, or the resident's pain intensity level after pain medication was administered to the resident.
Observation on 11/18/19 at 12:06 P.M., showed the resident was laying down in his/her bed with his/her call light within reach. His/her bed was in a low position. The resident's eyes were closed and he/she was resting comfortably without signs or symptoms of pain or distress.
Observation on 11/19/19 at 6:30 A.M., showed the resident was sitting up in his/her wheelchair by the nursing station with other residents. He/she was alert but was not interacting with anyone. He/she was dressed for the weather without odor and showed no signs or symptoms of pain or discomfort. When trying to speak with the resident, resident did not respond.
3. During an interview on 11/20/19 at 4:00 P.M., Licensed Practical Nurse (LPN) D said:
-When a resident complains of pain, the nurse is supposed to ask about their pain, where their pain is located and what the intensity of their pain is.
-They usually have the resident rate their pain from 1-10 (10 represents intense pain) then, if they can give a pain medication, the nurse should check to see what pain medication they have, give the pain medication, then about an hour later they are supposed to check back with the resident to see if the pain medication was effective.
-The nurse was supposed to document on the back of the MAR the date they gave the pain medication, what they gave, why they gave it, location of the resident's pain, the resident's pain intensity prior to administration and if it was effective.
-They also were supposed to document the resident's pain intensity level after giving the pain medication.
-If they have non-pharmacological interventions that they can use to try to keep from giving pain medication, they will also use those and they should be documented.
During an interview on 11/21/19 at 12:19 P.M., Certified Medication Technician (CMT) A said:
-Whenever the resident requests pain medication, they were supposed to ask the resident where their pain is located and to rate their pain intensity.
-Depending on the resident's level of pain, they will determine what type of pain medication to give.
-They inform the nurse that the resident has pain and then once they give the pain medication, they are supposed to document the date and time they gave the pain medication and on the back of the MAR they document what they gave, the location of the resident's pain and the pain intensity level before and after giving pain medication.
During an interview on 11/21/19 at 12:48 P.M., the Assistant Director of Nursing (ADON) said:
-He/she expects the nursing staff to assess the residents pain prior to giving pain medication.
-They should ask the location and intensity (if the resident can tell them) of their pain, or look for signs and symptoms of pain and assess their vital signs (temperature, respirations, pulse and blood pressure).
-They should assess the resident's pain intensity again 35 to 45 minutes after giving pain medication.
-They should be documenting this information on the back of the MAR and with the transition to e-charting, it should be documented in the computer on the MAR.
During an interview on 11/21/19 at 2:23 P.M., the Administrator and Director of Nursing (DON) said:
-When a resident complains of pain nursing staff should assess the resident's pain intensity level then attempt non-pharmacological interventions first, then if they do not work, administer pain medication.
-After giving the resident pain medication, they should follow up and complete another pain assessment.
-Documentation showing the resident's pain intensity level before and after administering pain medication, the time they administered pain medication and where the resident's pain was located should be documented on the back of the MAR each time they administer pain medication.
-They should initial that they gave the pain medication on the front of the MAR.
-Documentation for non-pharmacological interventions implemented should also be documented on the back of the MAR.
-The DON and ADON should be monitoring for accuracy and completion.
-They should complete a comprehensive pain assessment on any resident who has pain.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0710
(Tag F0710)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure a resident's physician was notified of his/her...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure a resident's physician was notified of his/her significant weight gain; to follow the Registered Dietitian's (RD) recommendations of stopping the resident's double portions at meals, and to address the resident's clothing no longer being able to fit the resident comfortably due to his/her significant weight gain for one sampled resident (Resident #13) out of 16 sampled residents. The facility census was 55 residents.
Record review of the facility's Weight Assessment and Intervention policy revised September 2012 showed:
-The interdisciplinary team will strive to prevent, monitor, and intervene for undesirable weight loss or gain for residents.
-Any weight change of 5% or more since the last weight assessment will be retaken the next day for confirmation. If the weight change is verified, nursing will notify the Registered Dietician (RD) per facility protocol.
-The threshold for significant unplanned and undesired weight change will be based on the following criteria [where percentage of body weight loss = (usual weight - actual weight)/(usual weight) x 100]:
--One month - 5% weight change is significant; greater than 5% is severe.
--Three months - 7.5% weight change is significant; greater than 7.5% is severe.
--Six months - 10% weight change is significant; greater than 10% is severe.
-If the weight change is desirable, this will be documented and no change in the care plan will be necessary.
-Individualized care plans shall address, to the extent possible, the identified causes of weight gain.
-Interventions for undesirable weight gain shall be based on careful consideration of the the following:
--Resident choice and preferences.
--Nutrition and hydration needs of the resident.
--Functional factors that may inhibit independent eating.
--Environmental factors that may inhibit appetite or desire to participate in meals.
1. Record review of Resident #13's Face Sheet showed he/she was admitted to the facility on [DATE] and readmitted on [DATE] with the following diagnoses:
-Major Depressive disorder.
-Anxiety.
-Hepatitis C (a viral infection that attacks the liver).
-Chronic kidney disease (CKD - gradual loss of kidney function over time).
-Chronic Obstructive Pulmonary Disease (COPD - a disease process that decreases the ability of the lungs to perform ventilation).
-The resident had a Do Not Resuscitate (DNR - do not perform chest compressions or artificial breathing in the case of an emergency; allow natural death).
-The resident had a guardian.
Record review of the resident's care plan dated 2/6/19 showed:
-The resident had a potential nutritional problem related to his/her COPD.
-The resident will maintain his/her current weight plus or minus five percent (5%) through the next review date.
-Monitor the resident's weight monthly.
-Provide diet and consistency per the resident's physician's orders.
Record review of the resident's weight record showed on 2/9/19 he/she weighed 255 pounds.
Record review of the resident's Dietary Nutrition assessment dated [DATE] showed:
-The resident had a regular diet order.
-He/she weighed 255 pounds.
-The resident had a significant weight change.
-The resident had weighed 275 pounds at the time of his/her discharge in December 2018.
-The resident had a 25 pound weight loss (this was actually 20 pounds of weight loss).
-The resident had been living in the community and not eating well after his/her discharge from the facility.
-He/she did not refuse food and generally ate 50 - 75% of his/her meals.
-The resident's dietary intake had decreased to less than 50% for most meals
-His/her goal was to maintain his/her weight.
-It was recommended by the RD the resident was offered high calorie snacks between meals and at bedtime and for the staff to complete weekly weights for for weeks.
--Weekly weights were not documented as being completed by the staff.
Record review of the resident's weight record showed:
-On 2/20/19 he/she weighed 256 pounds.
-On 3/3/19 he/she weighed 253.6 pounds.
-On 4/1/19 he/she weighed 255 pounds.
-On 5/5/19 he/she weighed 260 pounds.
Record review of the resident's quarterly Minimum Data Set (MDS - a federally mandated assessment instrument completed by the facility staff for care planning) dated 5/29/19 showed:
-The resident was cognitively intact with a Brief Interview for Mental Status (BIMS) of 15 out of 15.
-Was independent with bed mobility.
-Required staff supervision for dressing, eating, and personal hygiene,
-Required limited staff assistance for transfers and toileting.
-Weighed 255 pounds.
Record review of the resident's weight record showed:
-On 6/2/19 he/she weighed 275 pounds.
--This was a 15 pound weight gain in one month (5.77% in one month).
Record review of the resident's Nursing Notes for June 2019 showed no documentation staff notified the resident's physician of his/her 15 pound weight gain in one month.
Record review of the resident's July 2019 Physician's Order Sheet (POS) showed his/her diet order was a regular diet with double portions.
Record review of the resident's weight record showed:
-On 7/3/19 he/she weighed 312.6 pounds.
--This was a 37.6 pound weight gain in one month (13.67% in one month) and 57.6 pound weight gain in three months (22.59% in three months).
Record review of the resident's Nursing Notes for July 2019 showed no documentation staff notified the resident's physician of his/her 37.6 pound weight gain in one month and 57.6 pound weight gain in three months.
Record review of the resident's weight record showed:
-On 8/2/19 he/she weighed 312 pounds.
--This was a 57.6 pound weight gain in six months (22.59% in six months).
Record review of the resident's Nursing Notes for August 2019 showed no documentation staff notified the resident's physician of his/her 57.6 pound weight gain in six months.
Record review of the resident's August 2019 (POS) showed his/her diet order was a regular diet with double portions.
Record review of the resident's Dietary Nutritional Quarterly Assessment completed by the dietary manager dated 8/28/19 showed:
-The resident was on a regular diet.
-His/her weight was 312 pounds on 9/4/19.
--This weight was after the date the quarterly assessment was completed.
-He/she ate 76% or more of his/her meals.
-He/she would refuse food.
-The resident eats 75-100% of his/her meals.
-He/she had requested to be taken off double portions because he/she had gained too much weight.
-Had a 10% weight gain since 4/1/19.
--The resident weighed 255 pounds on 4/1/19 and 312 pounds on 9/4/19. This was a 57 pound weight gain (22.35%) since 4/1/19.
-The resident will refuse breakfast at times.
Record review of the resident's quarterly MDS dated [DATE] showed the resident:
-Was cognitively intact with a BIMS of 13 out of 15.
-Was independent with bed mobility.
-Required staff supervision for dressing, eating, toileting, and personal hygiene,
-Required limited staff assistance for transfers.
-Weighed 312 pounds.
-Had a significant weight gain that was not part of a physician prescribed weight gain regimen.
Record review of the resident's September 2019 and October 2019 POS showed his/her diet order was a regular diet with double portions.
Record review of the resident's weight record showed:
-On 9/4/19 he/she weighed 312 pounds.
-On 10/7/19 he/she weighed 304.8 pounds.
Record review of the resident's November 2019 POS showed his/her diet order was a regular diet with double portions.
Record review of the resident's weight record showed a weight had not been recorded for November 2019 as of 11/21/19.
Observation on 11/18/19 at 1:50 P.M. showed the bottom of the resident's shirt in front came down to the middle of his/her abdomen, exposing the resident's abdomen as he/she was in the hall in his/her wheelchair.
During an interview on 11/18/19 at 1:56 P.M., the resident said:
-He/she had gained between 80 to 100 pounds since July 2018.
-His/her shirts no longer fit correctly.
-His/her shirts were so small they only covered to the middle of his/her belly.
-He/she thought some of his/her breathing problems may have been due to his/her weight gain.
Observation of the resident on 11/19/19 at 12:00 P.M., 11/20/19 at 8:20 A.M., and 11/21/19 at 10:50 A.M. showed the bottom of the resident's shirt in front came down to the middle of his/her abdomen, exposing the resident's abdomen as he/she was in the hall in his/her wheelchair.
During an interview on 11/21/19 at 10:56 A.M. the resident said:
-He/she had some clothes that fit correctly.
-He/she needed some shirts in a bigger size because the ones that he/she had only fit to the middle of his/her belly.
-He/she did not think he/she had money to get shirts, even from a thrift store, because he/she used his/her money for cigarettes each month.
-His/her weight gain and clothing not fitting correctly bothered him/her and made him/her feel badly about his/her appearance, especially when staff would come up to him/her and pull his/her shirt down in front to cover his/her belly.
-It made him/her feel like a character in a movie known for being excessively overweight.
-He/she was getting double portions of food at one time, and sometimes still does, but he/she had asked to only get a regular portion due to his/her significant weight gain.
During an interview on 11/21/19 at 3:28 P.M., the Administrator and Director of Nursing (DON) said:
-He/she would expect staff notify the resident's physician of recommendation by the RD and/or Dietary Manager.
-He/she would expect staff to notify the resident's physician of his/her significant weight gain.
-He/she would expect staff to document in the Nursing Notes of the resident's physician notification and of any orders received.
-He/she had noticed the resident's shirts did not fit him/her properly, but he/she did not think it bothered the resident.
-The resident did not have any money in his/her resident trust account to purchase new shirts.
-He/she would inform the resident's guardian about his/her clothing not fitting.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a resident was free from unnecessary medications for one sam...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a resident was free from unnecessary medications for one sampled resident (Resident #4) out of 16 sampled residents. The facility census was 55 residents.
Record review of the facility's Medication Regimen Review policy and procedure dated June 2012, showed:
-Unnecessary drugs are medications given in excessive dose, in excessive duration, without adequate monitoring, without adequate indications for use, or in the presence of adverse consequences which indicate the dose should be reduced or discontinued.
-Regarding Psychotropic medications it showed:
--A review of new orders for this class of drugs to include the documentation of a specific condition as diagnosed and documented in the clinical record.
--Need for gradual dose reductions.
--Need for behavioral interventions unless clinically contraindicated.
1. Record review of Resident #4's Face Sheet showed he/she was admitted to the facility on [DATE] and readmitted on [DATE] with the following diagnoses:
-Acute respiratory failure.
-Anxiety.
-Major Depressive Disorder.
-Quadriplegia (paralysis of all four extremities and usually the trunk).
Record review of the resident's care plan dated 12/26/17 and revised on 1/22/18 showed:
-The resident uses psychotropic medications for depression.
-He/She will have minimal side effects or adverse reactions related to the use of psychotropic medications.
-Educate the resident family/caregivers about risks, benefits, and the side effects and/or toxic symptoms of psychotropic medications.
-Give medications as ordered by his/her physician.
-Monitor/document side effects and effectiveness.
Record review of the resident's Note to Attending Physician/Prescriber dated 5/23/19 showed:
-The pharmacist recommended the following:
--Please assess if there is a potential for gradual dose reduction of the resident's Fluoxetine (Prozac - an anti-depressant medication).
--He/she is currently prescribed 20 milligrams (mg) daily.
--Consider a trial reduction to 10 mg if clinically appropriate.
-If no reduction is made please provide a brief rationale as to why in order to help the facility remain in compliance with state regulations.
-The resident's physician marked the box to disagree with the pharmacist's recommendation.
-The resident's physician did not provide a brief rationale for the disagreement.
-The form was signed by the physician on 6/7/19.
Record review of the resident's quarterly Minimum Data Set (MDS - a federally mandated assessment instrument completed by facility staff for care planning) dated 8/7/19 showed he/she:
-Was cognitively intact with a Brief Interview for Mental Status (BIMS) of 15 out of 15.
-Had a Mood Assessment Score for depression was zero, indicating no signs or symptoms of depression.
Record review of the resident's November 2019 POS and MAR showed:
-Fluoxetine (Prozac - an anti-depressant medication) 20 mg daily for depression.
-Staff documented Fluoxetine 20 mg was administered to the resident daily.
During an interview on 11/21/19 at 10:45 A.M., Licensed Practical Nurse (LPN) C said he/She thought the Director of Nursing (DON) was responsible to check for pharmacy recommendations and to notify the resident's physician if there were any recommendations.
During an interview on 11/21/19 at 2:44 P.M., the Administrator and DON said:
-The DON was responsible to monitor recommendations from the pharmacist regarding drug regime review and gradual dose reduction.
-The resident's physician needed to document a reason why he/she declined the pharmacist's recommendations.
-If the resident's physician did not document a reason why he/she declined the pharmacist's recommendations, he/she should contact the physician for clarification.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure the physician re-evaluated one sampled resident...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure the physician re-evaluated one sampled resident (Resident #35) after 14 days for continued use of as needed (PRN) psychotropic medication out of 16 sampled residents. The facility census was 55 residents.
Record review of the facility's Medication Regimen Review policy and procedure dated June 2012, showed unnecessary drugs are medications given in excessive dose, in excessive duration, without adequate monitoring, without adequate indications for use, or in the presence of adverse consequences which indicate the dose should be reduced or discontinued. Regarding Psychotropic medications it showed:
-A review of new orders for this class of drugs to include the documentation of a specific condition as diagnosed and documented in the clinical record.
-Need for gradual dose reductions.
-Need for behavioral interventions unless clinically contraindicated.
-A review of the resident's with as needed (PRN) psychotropic medications for a documented diagnoses specific condition and they are limited to 14 days. If greater than 14 days, the rationale for such listed in the medical record.
-A review of residents with PRN anti-psychotic orders is limited to 14 days. Review of documentation for an attending physician or nurse practitioner evaluations to justify the continued need of the medication.
-Residents who have not used psychotropic drugs are not given them unless the medication is necessary to treat a specific condition as diagnosed.
1. Record review of Resident #35's Face Sheet showed he/she was admitted on [DATE], with diagnoses including schizoaffective disorder (a chronic mental health condition characterized primarily by symptoms of schizophrenia, such as hallucinations or delusions, and symptoms of a mood disorder, such as mania and depression), psychosis (a severe mental disorder in which thought and emotions are so impaired that contact is lost with external reality), delusional disorder and hallucinations.
Record review of the resident's quarterly Minimum Data Set (MDS-a federally mandated assessment tool to be completed by facility staff for care planning) dated 7/16/19, showed the resident:
-Was cognitively intact with no memory problems.
-Was independent with bathing, dressing, grooming, toileting and ambulation.
-Received antidepressant medication.
Record review of the resident's Physician's Order Sheet (POS) dated 9/1/19 to 9/30/19, showed a physician's order for Haldol Deconate injection 100 milligrams (mg)/milliliters (ml), inject 1 ml intramuscular (IM) for outbursts as needed (the origin of the order dated 8/23/19 with no end date documented) for agitation.
Record review of the resident's Physician's Telephone Order dated 9/4/19, showed the following physician's orders:
-Discontinue Haldol Deconate.
-Zyprexa 5 mg every 6 hours as needed for agitation with no end date documented.
-Zyprexa 5 mg IM every 6 hours as needed for agitation with no end date documented.
Record review of the resident's Physician's Telephone Orders showed:
-There were no orders showing Zyprexa 5 mg every six hours as needed for agitation and Zyprexa 5 mg IM as needed for agitation were discontinued after 14 days (from the start date).
-There were no orders showing Zyprexa 5 mg every six hours as needed for agitation and Zyprexa 5 mg IM as needed for agitation were reordered after 14 day duration (from the order start date).
Record review of the resident's Physician's Notes showed:
-There were no physician's notes since 8/22/19.
-There was no physician's note documented from 9/1/19 to 9/30/19.
Record review of the resident's Medical Record showed there was no documentation showing the resident's physician re-evaluated the resident in person after 14 days of the physician ordered Zyprexa (on 9/4/19).
Record review of the resident's Drug Regimen Review dated 9/23/19, showed the Pharmacist's recommendation stating PRN Zyprexa must be written for a 14 day duration; cannot be indefinite in duration due to new regulations. PRN anti-psychotics must be re-evaluated in person after 14 days before writing a new order. The review showed the Physician responded on 10/25/19 stating the resident was stable with his/her current dose.
Record review of the resident's POS dated 10/1/19 to 10/31/19, showed the following orders:
-Zyprexa 15 mg daily for agitation.
-Zyprexa 5 mg dissolve tablet on tongue every 6 hours as needed for agitation (ordered 9/25/19).There was no end date documented and no re-order date documented.
-Zyprexa 10 mg inject 5 mg intramuscular every 6 hours as needed for agitation (ordered 9/25/19). There was no end date documented and no re-order date documented.
Record review of the resident's Physician's Notes dated 10/23/19, showed the physician visited the resident during rounds at the facility. The Physician documented the resident had anxiety, and confusion with delusional thought processes. The recommendation was to continue his/her current plan of care, the resident was followed by psychiatry and refuses medications. There were no notes or orders regarding the resident's Zyprexa medications.
Record review of the resident's Medical Record showed there was no documentation showing the most recent observation and re-evaluation of the resident's for continuing his/her PRN Zyprexa medications.
Observation and interview on 11/18/19 at 11:32 A.M., showed the resident was in his/her room listening to music. He/she said:
-He/she has lived at other nursing homes and this one is the best so far because the staff treated him/her with dignity and respect.
-He/she had been on Lithium (an anti-psychotic) for schizoaffective disorder and grandiose ideas but he/she experienced several bad side effects.
-He/she was hospitalized for seven days at the psychiatric hospital and discussed the side effects he/she was having.
-The physician's in the hospital discontinued Lithium and started him/her on Zyprexa and Zyprexa seems to make him/her feel more balanced.
During an interview on 11/21/19 at 2:23 P.M., the Administrator and Director of Nursing (DON) said:
-Whenever a resident is prescribed PRN antipsychotic medications, the physician should complete a re-evaluation of the resident after 14 days in order to continue the medications.
-If on the Drug Regimen Review the Pharmacist documents that the resident should be re-evaluated after 14 days of having a PRN anti-psychotic, the expectation is for the physician to re-evaluate the resident and then re-order the anti-psychotic if he/she wanted the PRN to continue.
-The Administrator said all PRN anti-psychotic medications should be ordered for a 14 day duration.
-The DON is expected to review the Drug Regimen Review and upon observing the recommendation, they would call the physician to let him/her know he/she needs to complete a face to face evaluation of the resident if he/she wants the PRN to continue.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility staff failed to puree (make food into a paste or thick liquid suspension usually made from cooked food that was ground finely) the ranch...
Read full inspector narrative →
Based on observation, interview and record review, the facility staff failed to puree (make food into a paste or thick liquid suspension usually made from cooked food that was ground finely) the ranch potatoes to be smooth and without chewable bits and pieces and to have recipes for pureed foods available for the Dietary [NAME] (DC) to use. This practice potentially affected three residents with pureed diets. The facility census was 55 residents.
1. Observation on 11/18/19, showed:
- At 5:21 P.M., the Dietary [NAME] (DC) made pureed ranch potatoes.
- At no time, was there a recipe book open.
- At 5:21 P.M. and 40 seconds, the DC added milk to the food processor and still, no recipe book was opened, and
- At 5:22 P.M., the DC did not taste the product when he/she placed the pureed ranch potato mixture into a metal pan, the mixture still had visible pieces of the ingredients such as the bacon and the herbs.
Observation with the Dietary Manager (DM) on 11/18/19 at 5:46 P.M., during a taste test of the pureed ranch potatoes, the DM said he/she noticed the pureed ranch potatoes were gritty to the taste.
Record review of the recipe book with the DM on 11/18/19 at 5:52 P.M., showed the absence of recipes and instructions for pureed foods.
During an interview on 11/18/19 at 5:53 P.M., the DM said:
- There were not any pureed recipes to be used because they did not print off with the regular recipes and
- The recipes for pureed items are on the computerized system but he/she did not know why they did not print.
During an interview on 11/18/19 at 6:05 P.M., the DC said:
- He/she cannot eat a lot of the prepared foods items, because of onions, and
- He/she did not ask anyone to taste the pureed foods that day.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0568
(Tag F0568)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to maintain records of reconciled bank statements (a form where outstanding checks that were not cashed were subtracted from the ending bank b...
Read full inspector narrative →
Based on interview and record review, the facility failed to maintain records of reconciled bank statements (a form where outstanding checks that were not cashed were subtracted from the ending bank balance) for the months of 11/18 and 12/18; to account for the occurrence of $30 that was still in the account for one sampled resident (Resident #1000) that was discharged ; to have documentation that the Supplemental Security Income (SSI) agency was notified; and to have an accounting of what Resident #1001 had in his/her account after the resident was discharged to another facility, and to prepare and send quarterly statements for 28 residents who allowed the facility to hold and manage funds. This practice potentially affected 28 residents who resided at the facility and two discharged residents. The facility census was 55 residents.
1. Record review of the reconciled bank statements from 11/18 through 10/19 showed the absence of the reconciled statements for 11/18 and 12/18.
During an interview on 11/20/19 at 8:13 A.M., the Business Office Manager (BOM) said there were no reconciled bank statements for 11/18 and 12/18, because some records were lost in the computerized files after the changeover form one management entity to another management entity.
2. Record review of Resident #1000's records showed the following:
- The resident was discharged on 9/26/19.
- An e-mail dated 11/20/19 from a corporate person which showed the Resident's account was closed, and
- A balance of $30.00 in the Resident's account.
During an interview on 11/20/19 at 10:41 A.M., the BOM said:
- The $30 came into the Resident's account on 11/1/19.
- There was not documentation to show the facility notified the SSI agency to not send that resident's money to this facility.
- No documentation to show why that $30 was still in the resident's account even though the resident was discharged 55 days prior to this resident fund review, and
- They (facility personnel) have taken $30 to the resident at another facility in the past.
3. Record review of Resident #1001's records showed the following:
- The Resident was discharged on 10/17/19 to another facility.
- The absence of the amount of funds the resident had in his/her account on 10/17/19.
- The absence of records to show where that resident's funds went, and
- A balance of negative $50 as of 11/20/19.
During an interview on 11/20/19 at 10:46 A.M., the BOM said he/she could not get into the resident fund account back in 9/19 and 10/19.
4. Record review of the resident fund documentation showed the absence of quarterly statements for all 28 residents who resided at the facility and allowed the facility to manage funds for them.
During an interview on 11/20/19 at 11:24 A.M., the Business Office Manager (BOM) said he/she did not know about the quarterly statements being sent to the residents.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. Record review of Resident #26's admission face sheet showed he/she was admitted on [DATE] with the following diagnoses:
-Deme...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. Record review of Resident #26's admission face sheet showed he/she was admitted on [DATE] with the following diagnoses:
-Dementia (is a general term for loss of memory and other mental abilities severe enough to interfere with daily life).
-Palliative Care (is need for additional care services for chronic health condition provide by Hospice care agency).
Record review of the resident's Quarterly MDS dated [DATE] showed he/she:
-Was severely cognitively impaired and had short term and long term memory problems.
-He/she was rarely able to understand others and rarely able make his/her needs known.
-Required total assistance from staff for all cares and transfers.
-Was at risk for pressure ulcers or skin issues.
Record review of the resident's POS dated 11/1/19 to 11/30/19 showed:
-The resident's was on Hospice services.
-The resident did not have a physician's order for wound care treatment or skin monitoring.
-The nursing staff had been providing wound care without a physician's orders on the resident's POS.
Record review of Facility Wound Care Log dated 11/4/2019, showed the resident:
-Had a skin tear on his/her left hip that measured 0.4 cm in length (l) by 0.4 cm in width (w).
-Had a small amount of drainage, the area around the site was red without warmth, and was 100% pink granulation tissue (healing tissue that is lighter than surrounding tissue).
-The treatment order was to cleanse the area with wound cleanser, allow to dry, then apply hydrogel (used to help heal open wounds) and secure with border gauze.
-No other wounds were documented.
Record review of the resident's bath sheet dated 11/13/19 showed he/she:
-Had a red area documented on his/her bottom.
-The Certified Nursing Assistant (CNA) had signed off by his/her signature.
-The bath-sheet had been reviewed by the charge nurses on duty and reviewed by the DON on 11/14/19.
-Did not have any documentation related to plan of treatment or if the resident's physician was notified of the red area.
Record review of resident's Weekly Skin Condition Report (Pressure and Non Pressure Combined) dated 11/14/2019 at 3:40 P.M. showed the resident:
-Had a skin tear on his/her left hip and the measurement was 0.4 cm (l) by 0.4 cm (w).
-Had treatment orders to cleanse the area with wound cleanser, allow to dry, apply hydrogel and secure with border gauze.
-Had a new wound that was first observed on 11/14/19 of a Stage II pressure ulcers to his/her coccyx (tail bone) that measured 0/4 cm (l) by 0.3 cm (w) by 0.1 cm depth (d) and was pale pink in color.
-The treatment was was documented as, cleanse with the area with wound cleanser, allow to dry, apply skin barrier cream and cover with bordered gauze.
-No documentation was found on the POS for the treatment orders.
-No documentation was found in the resident's progress notes that Hospice was notified of the Stage II pressure ulcer to the coccyx.
-No documentation was found in the resident's progress notes that the resident's physician or family had been notified of the Stage II pressure ulcer to the coccyx.
Record review of the resident's Weekly Skin assessment dated [DATE] showed the resident's skin was intact and had no other documentation noted.
Record review on 11/19/19 of the Facility Initial Entrance Matrix showed the resident:
-Had no documentation of skin issue/wounds.
-Had been on hospice services.
Record review of the resident's TAR dated 11/1/19 to 11/30/19 showed:
-Cleanse left hip wound with wound cleanser, pat dry, apply foam adhesive dressing, change daily until healed.
-Cleanse right hip wound with wound cleanser, pat dry, apply foam adhesive dressing, change daily until healed (dated 11/4/19).
-Cleanse right shoulder with wound cleanser, pat dry, apply skin prep daily until healed.
-From 11/1/19 to 11/18/19 the 7:00 A.M. to 3:00 P.M. shift had initialed the treatments were completed.
-On 11/19/19 Hospice was documented for all three wound treatments (left hip, right hip and right shoulder).
Record review of the resident's medical record dated 11/1/19 to 11/20/19 showed:
-No nursing progress notes related to obtaining a physician's order for a treatment for the new coccyx wound.
-No documentation on reporting the resident's new Stage II Coccyx wound to his/her physician, Hospice, or family.
Observation on 11/20/19 at 1:50 P.M., of the resident's wound care by LPN A and the ADON showed:
-Staff had washed their hands upon entry of the resident's room and applied gloves.
-LPN A removed the old dressing that was dated 11/18/19 from the resident's left hip.
-The ADON measured the red wound area on the left hip at 1 cm (l) by 1.3 cm (w) and said
the wound was partial thickness (loss of the first two layers of skin).
-The resident also had a new area possibly from the dressing that measured 2.1 cm in (l) by 0.5 cm in (w) to the left hip and had partial thickness tissue loss.
-With new gloves on his/her hands, LPN A cleaned area with wound cleanser, pat the area dry, and applied a foam adhesive dressing.
-LPN A removed gloves and washed his/her hands.
-LPN A removed the old dressing that was dated 11/18/19 from the resident's right hip and then removed his/her gloves and washed his/her hands.
-The ADON measured the red wound area on the right hip at 5.0 cm (l) by 4.6 cm (w) with a darker area in the middle that measured 0.5 cm (w).
-With new gloves on his/her hands, LPN A cleaned area with wound cleanser, pat the area dry, and applied a foam adhesive dressing.
-LPN A removed gloves and washed his/her hands.
-The ADON measured the resident's right shoulder at 5.0 cm (l) by 4.5 cm (w) and also measured an area that was not red in color at 2.5 cm (l).
-LPN A cleaned the area with wound cleanser and then applied skin prep.
--The surveyor requested to see the resident's coccyx and heels.
-LPN A and the ADON were not aware of any areas on the resident's bottom or heels.
-Per the ADON and LPN A the resident's coccyx area had a redden area and a new open area.
-The ADON measured the redden area on the resident's coccyx at 5.0 cm in (l) by 7.7 cm (w) and at the top of the coccyx had a small slit area that had opened and measured 0.8 cm (l) by 1.0 cm (w) by 0.2 (d), was macerated (in contact with moisture too long and skin is lighter in color and wrinkled) and had 50-75% slough (dying or dead tissue).
-The ADON said he/she was not aware of the coccyx wound and had to call the resident's physician to obtain physician's orders.
-Observation of the resident's heels showed no open areas but they were mushy and soft.
Record review of the resident's Registered Nurse (RN) Hospice Visit Note dated 11/20/19 showed:
-The resident's had a Stage II Coccyx Pressure ulcer that measured 0.5 cm (l) by 0.5 cm (w) by 0.1 cm (d).
-Treatment was to cleanse the area with wound cleanser, apply hydrogel, then cover with bordered gauze. The resident physician orders was for daily dressing changes.
During an interview on 11/20/19 at 2:15 P.M., CNA A said:
-He/she had provided personal care for the resident and was not aware of any open areas at that time.
-The resident's bottom had been red.
-He/she said the Hospice Health Aide and the facility CNA both do showers and personal cares for the resident.
-If he/she found a new open or red skin area, he/she would notify the charge nurse.
During an interview on 11/20/19 at 2:31 P.M., the ADON said:
-He/she did the resident's Weekly Wound Assessment and the nurses do the Resident's Weekly Skin Assessment.
-CNA's complete the bath-sheets.
During an interview on 11/20/19 at 3:30 P.M., LPN B said:
- Resident #26 did not have an order for wound care or any skin treatment orders on his/her November 2019 POS.
-He/she would expect to have physician's order for treatment of the resident wounds.
During an interview on 11/20/19 at 3:30 P.M., LPN A said:
-His/her normal duties was the desk nurse, which included the assessment of residents on Medicare skilled services and other medical assessment as needed.
-The Charge Nurses were assigned the resident's Weekly Skin Assessment and the facility's wound nurse did the resident's Weekly Skin Conditions Wound Assessment.
-In review of Resident #26's medical record, he/she was not able to find a physician's order for the resident's wound care treatments or any other skin treatment or monitoring orders.
-He/she would expect to have a physician's order for treatment of the resident's wounds.
-When staff receive a physician's order, it should be transcribed to the resident's POS and to his/her TAR or Medication Administration Record (MAR).
During interview on 11/20/19 3:33 P.M., the ADON said:
-He/she had just talked with the resident's Hospice nurse on 11/20/19 and he/she had reported to the facility the resident had three wound areas.
-The ADON said he/she was not aware of the new area until it was found today during observation of wound care.
-The ADON was not able to explain how the coccyx wound had been documented on 11/14/19 on the resident's Weekly Skin Condition Report as a Stage II coccyx pressure ulcer.
During an interview and record review on 11/21/19 10:10 A.M., LPN D said:
-Staff should have physician's orders and should document care on the resident's TAR for wound treatments.
-Staff should not provide care without a physician's order and if not transcribed onto the MAR or TAR.
-Staff should call to verify orders or obtain a physician's orders for care and treatment and then transcribe the order to the resident's POS, TAR and MAR.
-The DON and the ADON review the resident's POS, TAR and MAR to ensure physician's orders had been transcribed during the end of month change over.
During an interview on 11/21/19 at 2:17 P.M. the DON and Administrator said:
-When they receive a physician's telephone order, nurses write the order on the POS, the MAR and TAR.
-On the following morning the DON and other administrative staff check the orders during the morning meeting to ensure the orders are correct and verify the medications and treatment supplies were obtained.
-They go over the POS, MAR and TAR when there are new orders, to ensure all orders are being accurately transcribed on all three documents and they compare to ensure they are accurate and transcribed correctly.
-The reconciliation of the POS's are done at the end of the month by the DON, ADON and MDS Coordinator.
-He/she would expect to have a physician's order prior to providing wound care or treatments.
-Physician's orders for wound care should have been obtained, and transcribed onto the resident's POS and TAR.
-He/she expects staff to follow those physician's orders for treatment and care.
-Documentation should be on the TAR showing the treatments were completed as ordered.
-If nursing staff see a wound during the skin or wound assessment, he/she expect nursing staff to call the physician and obtain an order for treatment.
-The nursing staff should document the new or changing skin or wound issues and should be descriptive to show what it looked like and to include measurements of the wound.
-Documentation should be in the weekly skin assessment document and in progress notes.
-The nurses were responsible for completing the weekly skin assessments and they should be comprehensive in documenting skin issues if the resident has a skin concern.
-The Wound Nurse was responsible for completing the Weekly Skin Conditions Wound Assessment for residents with wounds and he/she should be comprehensive in documenting detailed descriptions of the wound and include measurements.
-He/she expected the wound nurse to be responsible in monitoring and tracking the resident's status with skin issues or wounds to include current physician's orders and documentation.5. Record review of Resident #40's Face Sheet showed he/she was admitted to the facility on [DATE] and readmitted on [DATE] with the following diagnoses:
-Pressure ulcer (localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear and/or friction) of sacral region (large, triangular bone at the base of the spine and at the upper and back part of the pelvic cavity), untraceable (Full thickness tissue loss in which the base of the ulcer is covered by slough [necrotic/avascular tissue in the process of separating from the viable portions of the body and is usually light colored, soft, moist, & stringy] and/or eschar (tan, brown or black) in the wound bed).
Record review of the resident's outside wound care provider documentation dated 5/7/19 showed the resident:
-Had a Stage III pressure ulcer (a full thickness tissue loss. Subcutaneous fat may be visible but bone, tendon or muscle is not exposed. Slough may be present but does not obscure the depth of tissue loss. May include undermining or tunneling) to his/her coccyx (tailbone) that was not healed.
-The pressure ulcer measured 3 cm in length by 2.3 cm in width by 2 cm in depth with moderate amount of serosanguineous (containing blood and watery drainage) drainage.
-The wound bed had 76-100% pink granulation (any soft pink fleshy projections that form during the healing process in a wound that does not heal by first intention), no slough, no eschar, and no epithelialization present.
-The wound was deteriorating.
Record review of the resident's outside wound care provider documentation dated 6/18/19 showed the resident:
-Had a wound to his/her coccyx.
--The documentation did not identify the wound as pressure or non-pressure and did not include measurements.
--The wound to the resident's coccyx was documented by the resident's wound care provider as a Stage III pressure ulcer on 5/7/19.
Record review of the resident's Initial Wound assessment dated [DATE] showed:
-The resident had a surgical wound to his/her coccyx measuring 11.5 cm in length by 1 cm in width with no documented depth.
--The wound to the resident's coccyx was documented by the resident's wound care provider as a Stage III pressure ulcer on 5/7/19.
Record review of the resident's Weekly Wound assessment dated [DATE] showed:
-The resident had a surgical wound to his/her coccyx measuring 11.5 cm in length by 1 cm in width with no document depth.
-Had a small amount of serosanguineous drainage with a no amount of odor.
-The wound was closed or was a suspected deep tissue injury (may be characterized by a purple or maroon localized area of discolored intact skin or a blood-filled blister due to damage of underlying soft tissue from pressure and/or shear. Presentation may be preceded by tissue that is painful, firm, mushy, boggy, and warmer or cooler as compared to adjacent tissue).
--The wound to the resident's coccyx was documented by the resident's wound care provider as a Stage III pressure ulcer on 5/7/19.
Record review of the resident's Weekly Wound assessment dated [DATE] showed:
-The resident had a surgical wound to his/her coccyx measuring 5 cm in length by 0.6 cm in width with no document depth.
-Had a small amount of purulent (a thick, milky discharge often indicating an infection) drainage with a moderate amount of odor.
--The wound to the resident's coccyx was documented by the resident's wound care provider as a Stage III pressure ulcer on 5/7/19.
Record review of the resident's Weekly Skin Condition Report dated 9/30/19 showed the resident:
-Had an unspecified wound to his/her coccyx with no measurements.
-There was no documentation of the description about the wound.
-There was no documentation of the type of wound the resident had.
Record review of the resident's outside wound care provider documentation dated 10/1/19 showed:
-The resident had a pressure ulcer of his/her sacral region, unspecified stage.
-The pressure ulcer onset date was 10/20/18.
-The pressure ulcer had several measurements from top to bottom as follows:
--1.1 cm in length by 0.3 cm in width by 0.1 cm in depth.
--0.3 cm in length by 0.3 cm in width by 0.1 cm in depth.
--0.3 cm in length by 0.3 cm in width by 0.1 cm in depth.
--2.5 cm in length by 1 cm in width by 3.5 cm in depth.
--0.3 cm in length by 0.3 cm in width by 0.2 cm in depth.
--0.3 cm in length by 0.2 cm in width by 0.1 cm in depth.
-Wound care orders were to apply with silvercell wick (a wound treatment) to largest wound in the center and Aquacel AG strip (a wound treatment) applied over all wounds, cover with tegaderm sacral foam. Skin barrier wipe was applied before and after foam to improve dressing adherence. Additional 4X4 optifoam AG gentle silicone faced and bordered applied at the top portion of the dressing to fully cover the area.
Record review of the resident's outside wound care provider documentation dated 10/9/19 showed:
-The resident had an unspecified stage pressure ulcer to his/her sacral region.
-The wound measured 2.2 cm in length by 1.3 cm in width by 3 cm in depth.
-The wound bed was pink with copious amounts of serosanguineous drainage.
-The wound had undermining (the destruction of tissue or ulceration extending under the skin edges so that the pressure is larger at its base than at the skin surface. Undermining often develops from shearing forces and is differentiated from tunneling by the larger extent of the wound edge involved in undermining and the absence of a channel or tract extending from the pressure ulcer under the adjacent intact skin) present: at noon: 1.5 cm; at 3 o'clock 2 cm; at 6 o'clock 1.7 cm; at 9 o'clock 2 cm.
Record review of the resident's Weekly Skin Condition Report dated 10/14/19 showed the resident:
-Had a surgical incision to his/her sacral region measuring 2.9 cm in length by 1 cm in width by 3.6 cm in depth with large amount of serosanguineous drainage.
-NOTE: The resident's outside wound care provider documented the resident's wound as a pressure ulcer.
Record review of the resident's Daily Skilled Nursing Note dated 10/19/19 showed:
-The resident had a wound to his/her sacral area described as other skin issues.
-The documentation did not identify the type of wound the resident had, whether it was pressure ulcer or non-pressure ulcer, did not describe the appearance of the wound, if the wound had any drainage or odor, or any wound measurements.
Record review of the resident's annual MDS dated [DATE] showed the resident:
-Was cognitively intact with a Brief Interview for Mental Status (BIMS) of 15 out of 15.
-Required extensive staff assistance with bed mobility, transfers, dressing, toileting, and personal hygiene.
-Had a urinary catheter and colostomy (an alternative exit from the colon created to divert waste through a hole in the colon and through the wall of the abdomen).
-Had no pressure ulcers or skin issues.
Record review of the resident's Weekly Skin Condition Report dated 10/21/19 showed the resident:
-Had a surgical incision to his/her sacral region measuring 1.7 cm in length by 0.8 cm in width by 3.3 cm in depth with large amount of serosanguineous drainage.
-The wound condition had improved.
-NOTE: The resident's outside wound care provider documented the resident's wound as an untraceable pressure ulcer.
Record review of the resident's Weekly Skin Condition Report dated 10/28/19 showed the resident:
-Had a surgical incision to his/her sacral region measuring 1.2 cm in length by 0.7 cm in width by 3 cm in depth with moderate serosanguineous drainage.
-The wound condition had improved.
-The pressure ulcer had undermining starting at 1 o'clock around to the 12 o'clock position with a maximum distance of 0.5 cm.
-NOTE: The resident's outside wound care provider documented the resident's wound as a pressure ulcer.
Record review of the resident's outside wound care provider documentation dated 10/30/19 showed:
-The resident had a stage IV pressure ulcer of his/her sacral region.
-Had a pressure ulcer in the middle of the sacral region.
-The documentation did not include measurements.
-Staff were directed to clean the wound by flushing the wound with 30 milliliters (ml) normal saline, then absorb excess normal saline with 4X4s before repacking the wound and to change the dressing every third day or more often if needed if outer dressing is saturated.
Record review of the resident's November 2019 POS showed:
-Wound care treatment: With the resident on his/her left side, remove the old dressing.
-Cleanse the wound with sterile saline and 4x4, apply skin barrier to intact skin surrounding the wound
-Xerofoam to wound bed, cover with two Allvyn (a wound dressing) foams.
-Skin barrier to dressing edges to improve adherence.
-Change dressing every two days and as needed if soiled.
--NOTE: The new wound care orders by the resident's wound care physician dated 10/30/19 were not transcribed to the resident's current POS.
Record review of the resident's November 2019 MAR and TAR showed:
-Clean wound with normal saline and pat dry.
-Apply Aquacel AG rope (a wound treatment used to pack a wound for healing).
-Use skin prep to assist with dressing adhesion.
-Change every three days.
Record review of the facility's Weekly Skin Condition Report dated 11/4/19 showed:
-The resident had a surgical wound in the sacral region measuring 1.5 cm in length by 1 cm in width by 2.7 cm in depth.
-The wound bed was dark pink/red and had slough.
-There was no change in the wound from the previous assessment.
-The pressure ulcer had undermining starting at 1 o'clock around to the 12 o'clock position with a maximum distance of 0.5 cm.
-The wound had deteriorated since the previous assessment.
--NOTE: the resident's wound care provider documented the resident's wound was a stage IV pressure ulcer, not a surgical wound.
Record review of the resident's outside wound care provider documentation dated 11/12/19 showed:
-The resident had a stage IV pressure ulcer to his/her sacral region.
-He/she had osteomyelitis (infection of the bone) of the vertebra, sacral and sacrococcygeal region.
-Had a pressure ulcer in the middle of the sacral region.
-The documentation did not include measurements.
-Staff were directed to clean the wound by flushing the wound with 30 ml normal saline, then absorb excess normal saline with 4X4s before repacking the wound and to change the dressing every third day or more often if needed if outer dressing is saturated.
Record review of the facility's Weekly Skin Condition Report dated 11/13/19 showed:
-The resident had a surgical wound in the sacral region measuring 1.5 cm in length by 1 cm in width by 2.7 cm in depth.
-The wound bed was dark pink/red and had slough.
-There was no change in the wound from the previous assessment.
--NOTE: the resident's wound care provider documented the resident's wound was a stage IV pressure ulcer, not a surgical wound.
Observation of the resident on 11/20/19 at 10:59 A.M. showed LPN D:
-Placed the resident's wound care supplies on his/her bedside table without a barrier.
-Said the resident's wound care orders were for the wound to be cleansed with wound cleanser and pack with Aquacel rope, but he/she did not have any Aquacel rope in his/her treatment cart.
-He/She completes the resident's wound care weekly and the resident's wound care provider does it on the other days.
-He/She washed his/her hands and put on clean gloves.
-CNA C washed his/her hands and put on clean gloves.
-LPN D removed the resident's Foley catheter from the side of the bed and handed it to CNA C.
-Both LPN D and CNA C touched the resident to assist him/her to turn to his/her left side.
-LPN D removed the resident's old undated dressing.
-LPN D removed the packing from the resident's wound, removed his/her gloves, washed his/her hands and put on clean gloves.
-LPN D sprayed the resident's wound with wound cleanser and wiped it with gauze.
-He/She removed his/her gloves, washed his/her hands and put on clean gloves.
-He/She applied 6 x 6 bordered gauze dressing to the sacral wound.
During an interview on 11/20/19 at 11:15 A.M., LPN D said:
-He/She should have placed the resident's wound care supplies on a barrier.
-The resident did not have Aquacel rope so he/she was not able to do the resident's wound care as it was ordered by his/her physician.
During an interview on 11/21/19 at 10:31 A.M., the ADON said:
-He/She was responsible for wound documentation in the facility.
-The resident had a pressure ulcer to his/her coccyx/sacral area, but then had surgical repair to the site.
-After the physician did a surgical repair to the resident's pressure ulcer, he/she thought the type of wound would change from pressure ulcer to surgical wound.
-The resident's wound care orders should match on his/her POS and MAR/TAR.
-He/she could not find an order to cleanse the resident's wound and put on a dry dressing if he/she did not have Aquacel rope to pack the resident's wound.
-Staff should follow the resident's physician's order for wound care.
During an interview on 11/21/19 at 3:11 P.M., the Administrator and DON said:
-Staff should follow the resident's physician's orders for wound care.
-The resident should have plenty of Aquacel rope and if he/she did not, he/she would expect staff to notify him/her to order more.
-He/She expected staff to accurately document the type of wound a resident had, if the wound was pressure or non-pressure, the measurements, and description of the resident's wound.
6. Record review of Resident #197's Face Sheet showed he/she was admitted to the facility on [DATE] and readmitted on [DATE] with the following diagnoses:
-Urinary Tract Infection (UTI - an infection of one or more structures in the urinary system).
-Pressure ulcer, unspecified stage.
-Right below the knee amputation.
-Left below the knee amputation.
-Colostomy.
-Paraplegia (loss of movement of both legs and generally the lower trunk).
Record review of the resident's Weekly Wound assessment dated [DATE] showed:
-The resident had a stage IV pressure ulcer to his/her right and left buttocks measuring 15 cm in length by 24 cm in width and 3.3 cm in depth.
-The wound had undermining the full circumference of the wound measuring a maximum of 4.5 cm.
-The wound had tunneling (a passageway of tissue destruction under the skin surface that has an opening at the skin level from the edge of the wound) at the 6 o'clock position with measuring a maximum of 7 cm.
-The wound had a large amount of purulent foul smelling drainage.
-The wound bed had 25% epithelial tissue, 25% granulation, and 50% slough.
Record review of the resident's Weekly Wound assessment dated [DATE] showed:
-The resident had a stage IV pressure ulcer to his/her sacral area measuring 14 cm in length by 25 cm in width and 0.7 cm in depth.
-The wound had undermining at 1 o'clock to 7 o'clock with a maximum of 2.1 cm.
-The wound had tunneling at the 12 o'clock position with measuring a maximum of 0.7 cm.
-The wound had a large amount of serosanguineous slight smelling drainage.
-The wound bed had 50% epithelial tissue, 25% granulation, and 25% slough.
--The documentation did not address the resident's right or left buttocks pressure ulcers.
Record review of the resident's Weekly Wound assessment dated [DATE] showed:
-The resident had a stage IV pressure ulcer to his/her sacral area measuring 9 cm in length by 25 cm in width and 0.7 cm in depth.
-The wound had undermining at 12 o'clock to 6 o'clock with a maximum of 0.6 cm.
-The wound had no tunneling.
-The wound had a large amount of serosanguineous slight smelling drainage.
-The wound bed had 50% epithelial tissue, 25% granulation, and 25% slough.
Record review of the resident's Weekly Wound assessment dated [DATE] showed:
-The resident had a stage IV pressure ulcer to his/her sacral area measuring 15 cm in length by 23 cm in width and 1 cm in depth.
-The wound had no undermining or tunneling.
-The wound had a large amount of serosanguineous foul smelling drainage.
-The wound bed had 25% epithelial tissue, 25% granulation, and 50% slough.
Record review of the resident's Weekly Wound assessment dated [DATE] showed:
-The resident had a stage IV pressure ulcer to his/her sacral area measuring 12.5 cm in length by 26 cm in width and 2 cm in depth.
-The wound had no undermining.
-The wound had tunneling at the 12 o'clock position with a maximum of 1.5 cm.
-The wound had a large amount of serosanguineous slight smelling drainage.
-The wound bed had 100% slough.
Record review of the resident's Weekly Wound assessment dated [DATE] showed:
-The resident had a stage IV pressure ulcer to his/her left buttock measuring 7 cm in length by 5 cm in width and 0.7 cm in depth.
-The wound had no undermining or tunneling.
-The wound had a moderate amount of serosanguineous slight smelling drainage.
-The wound bed had 50% epithelial and 50% slough.
-The resident had a stage III pressure ulcer to his/her right buttock measuring 5 cm in length by 2 cm in width by 1.3 cm in depth.
-The wound had no undermining or tunneling.
-The wound had a small amount of serosanguineous slight odor drainage,
-The wound had 50% granulation and 50% slough.
--No documentation the resident's physician was notified of the new pressure ulcers to the resident's right and left buttocks or that the resident's sacral pressure ulcer had healed.
Record review of the resident's quarterly MDS dated [DATE] showed he/she:
-Was cognitively intact with a BIMS of 15 out of 15.
-Required total staff dependence for bed mobility, transfers, dressing, toileting, and personal hygiene.
-Had a urinary catheter and colostomy.
-Had Stage III pressure ulcer and Stage IV pressure ulcer (Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present on some parts of the wound bed. Often includes undermining and tunneling).
Record review of the resident's outside wound care provider dated 10/28/19 showed:
-The resident had a stage IV pressure ulcer on his/her left buttock.
-The resident had a stage IV pressure ulcer on his/her right buttock.
-Staff were to clean the resident's wound with Normal Saline and change dressings every day.
-The documentation did not include measurements of the wounds or descriptions of the pressure ulcers.
Record review of the resident's Weekly Skin Condition Report dated 10/28/19 showed:
-The resident had a stage IV pressure ulcer to his/her left buttock measuring 5.5 cm in length by 2.5 cm in width and 1 cm in depth.
-The wound had a moderate amount of serosanguineous drainage.
-The wound bed was dark pink/red and had slough.
-The wound had improved.
-The resident had a stage III pressure ulcer to his/her right buttock measuring 6 cm in length by 1 cm in width by 1 cm in depth.
-The wound had a moderate amount of foul smelling drainage,
-The wound bed was pale pink and had slough.
-The wound had improved.
--The resident's outside wound care provider documented the resident's right buttock pressure ulcer as a stage IV pressure ulcer, not a stage III pressure ulcer.
Record review of the resident's November 2019 POS showed:
-Dakins solution 0.125%, dilute to 1/4 strength and apply to the resident's left buttock wound and right buttock wound twice daily, dated 11/14/19.
-Wound treatment to the resident's right and left buttocks: clean with wound cleanser, pat dry, apply calcium alginate to wound bed and cover with bordered gauze and reinforce with mefix tape if needed, change twice daily - undated order.
R
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure staff documented the shift change narcotic cou...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure staff documented the shift change narcotic count; to ensure a resident's Fentanyl patch (a narcotic medication) was signed off by two staff members when the patch was removed from a resident for destruction for two sampled residents (Resident #40 and #197), and to ensure a narcotic medication brought into the facility from the resident was verified by the facility pharmacy and accurately accounted for for one supplemental resident (Resident #27). The facility census was 55 residents.
Record review of the facility's Discarding and Destroying Medications policy dated 6/12:
-Medications that cannot be returned to the dispensing pharmacy shall be destroyed as permitted by state regulations.
-All controlled substances shall be retained in a securely locked area with restricted access until authorized individuals destroy them.
-Scheduled II, III, and IV controlled drugs must be destroyed by the Director of Nursing (DON) and another licensed nurse or per state law.
-The medication disposition record must contain, as a minimum, the following information:
--The resident's name; the date the medication was destroyed; the name and strength of the medication; the quantity destroyed; reason for destruction; and signature of witnesses.
-Whoever witnesses the destruction/disposal of medications must sign and date the medication disposition record.
Record review of the facility's Medications Brought to the Facility by the Resident/Family revised April 2007 showed:
-The facility ordinarily shall not permit residents and families to bring medications into the facility.
-Residents and families must report to the nursing staff any medications that they want to bring, or have brought, into the facility.
-The facility discourages the use of medications brought in from outside, and will inform residents and families of that policy, as well as applicable laws and regulations.
-If a medication is not otherwise available and/or it is determined to be essential to the resident's life, health, safety, or well-being to be able to take a medication brought in from outside, the Director of Nursing Services and nursing staff, with support of the Attending Physician and Consultant Pharmacist, shall check to ensure that the contents of each container have been verified by a licensed pharmacist.
-Medications brought into the facility that are not approved for the resident's use shall be returned to the family. If the family does not pick up those medications within thirty (30) days, the facility may destroy them in accordance with established policies.
1. Observation of the narcotic shift count on 11/19/19 at 6:40 A.M. showed:
-An unidentified night nurse and Licensed Practical Nurse (LPN) C completed the narcotic count for the 100/200 medication cart and for the 300/400 medication cart.
-LPN C did not sign as the nurse oncoming nurse the count was completed for either medication cart.
Record review of the 100/200 medication cart Change of Shift Narcotic Count record showed:
-Staff were instructed the narcotic count must be completed and signed by two staff members at each change of shift.
-The form had a space for three shifts each day, a space for the staff coming on duty to sign, a space for the staff going off duty to sign, the count, and any comments.
-A notation on 9/15/19 3-11 shift correct count on three with no further comments.
-Between 10/11/19 -11/19/19 two staff did not sign the count sheet 54 times out of 236 opportunities.
-The oncoming nurse did not sign he/she performed the narcotic count on 11/19/19.
Record review of the 300/400 medication cart Change of Shift Narcotic Count record showed:
-Staff were instructed the narcotic count must be completed and signed by two staff members at each change of shift.
-The form had a space for three shifts each day, a space for the staff coming on duty to sign, a space for the staff going off duty to sign, the count, and any comments.
-Between 8/31/19 -11/19/19 two staff did not sign the count sheet 61 times out of 482 opportunities.
-The oncoming nurse did not sign he/she performed the narcotic count on 11/19/19.
-After a copy was requested of the Change of Shift Narcotic Count record, LPN D signed in the spot the oncoming staff who counted the narcotics on 11/19/19 should have signed.
--LPN D did not perform the count during the change of shift on 11/19/19.
During an interview on 11/20/19 at 3:11 P.M., LPN D said:
-Staff should complete the Change of Shift Narcotic count at each shift.
-He/She did not do the narcotic count at the beginning of the shift on 11/19/19, the other day nurse, LPN C did.
-He/She should not have signed the Change of Shift Narcotic count record as the oncoming staff who did the count on 11/19/19 since he/she did not do the count.
-The staff person who did the count should have been the person to sign the shift change narcotic count record,
During an interview on 11/21/19 at 2:44 P.M., the Administrator and DON said:
-He/she expected oncoming staff to count narcotics with the off-going staff each shift.
-He/she expected the staff who counted the narcotics sign the Narcotic Count record to show it was performed and that it was correct.
-It was not appropriate for staff who did not perform the count to sign the Change of Shift Narcotic Count record.
2. Record review of Resident #40's Face Sheet showed he/she was admitted to the facility on [DATE] and readmitted on [DATE] with the following diagnoses:
-Anxiety disorder.
-Pressure ulcer (localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear and/or friction) of sacral region (tailbone), unstageable (Full thickness tissue loss in which the base of the ulcer is covered by slough [necrotic/avascular tissue in the process of separating from the viable portions of the body & is usually light colored, soft, moist, & stringy] and/or eschar (tan, brown or black) in the wound bed).
-Bipolar disorder (mood disorders characterized usually by alternating episodes of depression and mania).
-Major Depressive Disorder.
Record review of the resident's Care Plan dated 10/15/18 and revised on 10/17/19 showed no care plan for the resident's pain medication.
Record review of the resident's September 2019 Physician's Order Sheet (POS) and Medication Administration Record (MAR) showed:
-Fentanyl 12 microgram per hour (mcg/hr) patch - remove old patch and apply new patch every 72 hours with a 25 mcg/hr patch.
-Fentanyl 25 mcg/hr patch - remove old patch and apply new patch every 72 hours with a 12 mcg/hr patch.
--The MAR showed one staff member signed each time the patches were removed and new patches applied on 9/3/19, 9/6/19, 9/12/19, 9/15/19, 9/18/19, 9/21/19, 9/24/19, 9/27/19, and 9/30/19.
Record review of the resident's Fentanyl 25 mcg/hr Controlled Medication Utilization Record showed:
-One nurse signed out the 25 mcg/hr Fentanyl patch on 9/3/19, 9/6/19, 9/12/19, 9/15/19, 9/18/19, 9/21/19, 9/24/19, 9/27/19, and 9/30/19.
-No documentation by the facility staff that the old patch was destroyed, how it was destroyed, or who witnessed the destruction.
Record review of the resident's Fentanyl 12 mcg/hr Controlled Medication Utilization Record showed:
-One nurse signed out the 12 mcg/hr Fentanyl patch on 9/3/19, 9/6/19, 9/12/19, 9/15/19, 9/18/19, 9/21/19, 9/24/19, 9/27/19, and 9/30/19.
-No documentation by the facility staff that the old patch was destroyed, how it was destroyed, or who witnessed the destruction.
Record review of the resident's October 2019 POS and MAR showed:
-Fentanyl 12 mcg/hr patch - remove old patch and apply new patch every 72 hours with a 25 mcg/hr patch.
-Fentanyl 25 mcg/hr patch - remove old patch and apply new patch every 72 hours with a 12 mcg/hr patch.
--The MAR showed one staff member signed each time the patches were removed and new patches applied on 10/3/19, 10/6/19, 10/9/19, 10/12/19, 10/14/19, 10/17/19, 10/20/19, and 10/23/19.
--The remainder of the month was crossed out with discontinued handwritten across the MAR.
Record review of the resident's Fentanyl 25 mcg/hr Controlled Medication Utilization Record showed:
-One nurse signed out the 25 mcg/hr Fentanyl patch on 10/3/19, 10/6/19, 10/14/19, 10/18/19, 10/20/19, 10/23/19, and 10/25/19.
--No documentation a 25 mcg/hr Fentanyl patch was signed out between 10/6/19 - 10/14/19.
--The patch was ordered to be changed every 72 hours (3 days). The administration between 10/14/19 - 10/18/19 was 4 days, and 10/23/19 - 10/25/19 was 2 days.
-No documentation by the facility staff that the old patch was destroyed, how it was destroyed, or who witnessed the destruction.
Record review of the resident's Fentanyl 12 mcg/hr Controlled Medication Utilization Record showed:
-One nurse signed out the 12 mcg/hr Fentanyl patch on 10/3/19, 10/6/19, 10/9/19, and 10/10/19.
--No documentation a 12 mcg/hr Fentanyl patch was signed out after 10/10/19.
--The patch was ordered to be changed every 72 hours (3 days). The administration between 10/9/19 and 10/10/19 was 24 hours, or one day.
--The resident had orders to receive a 12 mcg/hr patch with a 25 mcg/hr patch. The facility was unable to provide documentation a 12 mcg/hr patch was received, signed out, and available to be placed on the resident per the resident's physician's orders.
-No documentation by the facility staff that the old patch was destroyed, how it was destroyed, or who witnessed the destruction.
Record review of the resident's Fentanyl 50 mcg/hr Controlled Medication Utilization Record showed:
-One nurse signed out the 50 mcg/hr Fentanyl patch on 10/26/19 and 10/29/19.
-No documentation by the facility staff that the old patch was destroyed, how it was destroyed, or who witnessed the destruction.
Record review of the resident's annual Minimum Data Set (MDS - a federally mandated assessment instrument completed by facility staff for care planning) dated 10/20/19 showed the resident:
-Was cognitively intact with a Brief Interview for Mental Status (BIMS) of 15 out of 15.
-Required extensive staff assistance with bed mobility, transfers, dressing, toileting, and personal hygiene.
-Had a urinary catheter and colostomy (an alternative exit from the colon created to divert waste through a hole in the colon and through the wall of the abdomen).
-Had no pressure ulcers or skin issues.
-Had pain and received scheduled pain medications.
-Received an opioid medication seven out of seven days during the look-back period.
Record review of the resident's November 2019 POS and MAR showed:
-Fentanyl 50 mcg/hr patch apply and remove one patch every 72 hours for right hip pain dated 10/25/19.
--The MAR showed one staff member signed each time the patches were removed and new patches applied on 11/2/19, 11/5/19, 11/8/19, 11/11/19, 11/14/19, and 11/17/19.
Record review of the resident's Fentanyl 50 mcg/hr Controlled Medication Utilization Record showed:
-One nurse signed out the 50 mcg/hr Fentanyl patch on 11/2/19, 11/5/19, 11/8/19, 11/11/19, 11/14/19, and 11/17/19.
-No documentation by the facility staff that the old patch was destroyed, how it was destroyed, or who witnessed the destruction.
3. Record review of Resident #197's Face Sheet showed he/she was admitted to the facility on [DATE] and readmitted on [DATE] with the following diagnoses:
-Urinary Tract Infection (UTI - an infection of one or more structures in the urinary system).
-Pressure ulcer, unspecified stage.
-Right below the knee amputation.
-Left below the knee amputation.
-Colostomy.
-Major Depressive disorder.
-Anxiety.
-Paraplegia (loss of movement of both legs and generally the lower trunk).
Record review of the resident's September 2019 POS and MAR showed:
-Fentanyl 25 mcg/hr apply and remove one patch with a 12 mcg/hr patch to equal 37 mcg/hr every 72 hours.
-The MAR showed one staff member signed each time an old patch was removed and a new patch was applied on 9/2/19, 9/5/19, 9/8/19, 9/11/19, 9/14/19, 9/17/19, 9/20/19, 9/23/19, 9/26/19, and 9/29/19.
-Fentanyl 12 mcg/hr apply and remove one patch with a 25 mcg/hr patch to equal 37 mcg/hr every 72 hours.
-The MAR showed one staff member signed each time an old patch was removed and a new patch was applied on 9/2/19, 9/20/19, 9/23/19, 9/26/19, and 9/29/19. The 12 mcg/hr patch was marked as not available on 9/5/19, 9/8/19, 9/11/19, 9/14/19, and 9/17/19.
Record review of the resident's Fentanyl 25 mcg/hr Controlled Medication Utilization Record showed:
-One nurse signed out the 25 mcg/hr Fentanyl patch on 9/5/19, 9/8/19, 9/11/19, 9/14/19, 9/17/19, 9/20/19, 9/23/19, 9/26/19, and 9/29/19.
-No documentation by the facility staff that the old patch was destroyed, how it was destroyed, or who witnessed the destruction.
Record review of the resident's Fentanyl 12 mcg/hr Controlled Medication Utilization Record showed:
-One nurse signed out the 12 mcg/hr Fentanyl patch on 9/20/19, 9/23/19, 9/26/19, and 9/29/19.
-No documentation by the facility staff that 12 mcg/hr Fentanyl patches were received or available for the resident between 9/1/19 - 9/20/19.
-No documentation by the facility staff that the old patch was destroyed, how it was destroyed, or who witnessed the destruction.
Record review of the resident's October 2019 POS showed:
-Fentanyl 25 mcg/hr apply and remove one patch with a 12 mcg/hr patch to equal 37 mcg/hr every 72 hours.
-The MAR showed one staff member signed each time an old patch was removed and a new patch was applied on 10/2/19, 10/6/19, 10/9/19, 10/14/19, 10/17/19, 10/20/19, 10/23/19, 10/26/19, and 10/29/19.
-Fentanyl 12 mcg/hr apply and remove one patch with a 25 mcg/hr patch to equal 37 mcg/hr every 72 hours.
-The MAR showed one staff member signed each time an old patch was removed and a new patch was applied on 10/6/19, 10/10/19, 10/14/19, 10/17/19, 10/20/19, 10/23/19, 10/26/19, and 10/29/19. The 12 mcg/hr patch was not available on 10/2/19.
Record review of the resident's Fentanyl 25 mcg/hr Controlled Medication Utilization Record showed:
-One nurse signed out the 25 mcg/hr Fentanyl patch on 10/2/19, 10/17/19, 10/20/19, 10/23/19, 10/26/19, 10/29/19.
--No documentation by the facility to show the resident had 25 Fentanyl patches received or available between 10/2/19 - 10/17/19.
-No documentation by the facility staff that the old patch was destroyed, how it was destroyed, or who witnessed the destruction.
Record review of the resident's Fentanyl 12 mcg/hr Controlled Medication Utilization Record showed:
-One nurse signed out the 12 mcg/hr Fentanyl patch on 10/2/19, 10/14/19, 10/17/19 10/20/19, 10/23/19, and 10/26/19.
-No documentation by the facility staff that the old patch was destroyed, how it was destroyed, or who witnessed the destruction.
Record review of the resident's quarterly MDS dated [DATE] showed he/she:
-Was cognitively intact with a BIMS of 15 out of 15.
-Required total staff dependence for bed mobility, transfers, dressing, toileting, and personal hygiene.
-Had a urinary catheter and colostomy.
-Had Stage III pressure ulcer (a full thickness tissue loss. Subcutaneous fat may be visible but bone, tendon or muscle is not exposed. Slough may be present but does not obscure the depth of tissue loss. May include undermining or tunneling) and Stage IV pressure ulcer (Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present on some parts of the wound bed. Often includes undermining and tunneling).
-Received opioid pain medications seven out of seven days during the look-back period.
-Received scheduled pain medication.
Record review of the resident's November 2019 POS showed:
-Fentanyl 25 mcg/hr apply and remove one patch with a 12 mcg/hr patch to equal 37 mcg/hr every 72 hours.
-Fentanyl 12 mcg/hr apply and remove one patch with a 25 mcg/hr patch to equal 37 mcg/hr every 72 hours.
Note: Fentanyl 25 mcg/hr and Fentanyl 25 mcg/hr patch Controlled Medication Utilization Records for November 2019 were requested and not received at the time of survey.
During an interview on 11/20/19 at 3:03 P.M., LPN A said:
-One nurse signs the MAR they have removed the Fentanyl patch.
-He/she did not think two nurses had to sign for the removal of a Fentanyl patch.
During an interview on 11/20/19 at 3:11 P.M., LPN D said:
-One nurse signs the MAR they have removed the Fentanyl patch.
-He/She did not think two nurses had to sign for the removal of a Fentanyl patch.
During an interview on 11/21/19 at 2:44 P.M., the Administrator and DON said:
-He/she expected two staff to document the removal of a Fentanyl patch.
-He/she expected staff to document the destruction of the Fentanyl patch on the resident's MAR.
4. Record review of supplemental Resident #27's admission MDS dated [DATE] showed the resident:
-Was cognitively intact with a BIMS of 13 out of 15.
-Was on hospice services.
-Received an anti-anxiety seven out of seven days during the look-back period.
Observation on 11/19/19 at 8:07 A.M. of the medication room refrigerator showed:
-An opened bottle of a liquid substance in an Ativan Intensol bottle with approximately 25 milliliters (ml) in the bottle, not double locked in the refrigerator.
-The bottle had Resident #27's name on the label.
During an interview on 11/19/19 at 8:07 A.M., the Assistant Director of Nursing (ADON) said:
-He/she could see that the Ativan bottle had been opened with some contents missing.
-He/she thought the bottle of Ativan was brought in by the resident, his/her family, or his/her hospice (end of life care) provider when the resident was admitted .
-The resident's Narcotic Record showed the Ativan bottle should have a full 30 ml in the bottle.
-The bottle was in the medication room refrigerator and not in a double locked system.
-The bottle of Ativan should have been double locked in the medication refrigerator.
-He/She could not say for certain the bottle contained Ativan since it had not been obtained through the facility pharmacy.
Record review of the resident's Individual Patient Narcotic Record showed:
-The resident's name handwritten on the form.
-Ativan 2 milligrams (mg) per ml handwritten on the form.
-Administer 0.25 - 1 ml every four hours as needed handwritten on the form.
-The form was dated 9/6/19.
-The amount on hand was documented as 30 ml.
--A copy of the form was requested and upon receipt, 30 ml was crossed out with a notation correct count 25 ml. The notation was signed by LPN C and the MDS Coordinator.
During an interview on 11/19/19 at 8:30 A.M., LPN C said:
-He/she thought the bottle of Ativan may have been brought in by the resident's hospice provider when he/she was admitted to the facility, but he/she was not certain of that.
-The bottle of Ativan had been opened and the bottle was not full.
-He/she did not think the facility pharmacy had verified the contents of the bottle.
During an interview on 11/20/19 at 8:55 A.M., the MDS Coordinator said:
-He/she signed the corrected total on the Ativan narcotic record without checking with pharmacy to verify the contents of the bottle.
-He/she did not know when the bottle of Ativan was opened or if it was received in the facility opened.
-He/she did not know who brought in the bottle of Ativan for the resident.
-He/she did not know what happened to the unaccounted for 5 ml's of Ativan from the bottle.
-He/she thought LPN A admitted the resident and may have received the bottle during the resident's admission process.
During an interview on 11/20/19 at 3:03 P.M., LPN A said:
-He/she did not accept a bottle of Ativan from the resident, the resident's family, or the resident's hospice provider during the resident's admission process.
-He/she would not accept a narcotic medication brought in from an outside source.
-The medication should have been verified by the pharmacy.
-If the bottle of Ativan had been received during the admission process, staff should have written a note about it, including the name of the medication, the amount of the medication, what the medication was, and that it was going to be verified by pharmacy.
-Staff should have noticed during the shift change count that the bottle did not have 30 ml's in it.
-Staff sign the shift count sheet acknowledging they witnessed the narcotic count and verify the count is correct.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0800
(Tag F0800)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to maintain the temperature of the mechanical soft pork riblet at or above 135 degrees Fahrenheit (ºF) for the duration of t...
Read full inspector narrative →
Based on observation, interview, and record review the facility failed to maintain the temperature of the mechanical soft pork riblet at or above 135 degrees Fahrenheit (ºF) for the duration of the dinner meal service and to implement measures to ensure the whole roasted turkeys were cooled to at least 70 ºF within two hours after being removed from the oven. This practice potentially affected all residents. The facility census was 55 residents.
1. Observation on 11/18/19, during the dinner meal preparation and service, showed:
- At 4:57 P.M., the Dietary [NAME] (DC) placed six pieces of pork riblets in the food processor to grind into a mechanical soft texture.
- At 5:07 P.M., the DC placed ground meat on steam table and failed to check the temperature after the mechanical soft meat was left in the food processor for about 10 minutes.
- At 5:32 P.M., the temperature of the mechanical soft riblet was 129.5 ºF, and
- At 5:54 P.M., the temperature of the mechanical soft riblet, was 119.6 ºF with seven residents left to serve.
During an interview on 11/18/19 at 6:06 A.M., the DC acknowledged that he/she did not check the temperature of the mechanical soft riblet before he/she placed it on the steam table.
2. Observation on 11/18/19 between 3:30 P.M. through 3:40 P.M., showed the Dietary Manager (DM) took whole roasted turkeys out of the ovens and at that time all temperatures of the roasted turkeys were above 190 ºF.
- At 4:00 P.M., the DM placed the roasted turkeys into the walk-in refrigerator and
- At 6:22 P.M., over two hours after the roasted turkeys were placed into the walk-in refrigerator, the temperature of one of the whole roasted turkeys was 153.4 ºF, which was 83.4 ºF above the required goal temperature of 70 ºF.
Record review of the following chapter of the 2017 Food and Drug Administration (FDA) Food Code, showed:
-Chapter 3-501.16 Time/Temperature Control for Safety Food, Hot and Cold Holding.
A) Except during preparation, cooking, or cooling, or when time is used as the public health control as specified under 3-501.19, and except as specified under paragraphs B and C of this section, TIME/TEMPERATURE CONTROL FOR SAFETY FOOD shall be maintained:
1) At 135 ºF or above, except that roasts cooked to a temperature and for a time specified in paragraphs 3-401.11(B) or reheated as specified in paragraph 3-403.11(E) may be held at a temperature of 135 ºF or above.
Chapter 3-501.14 Cooling.
A)
Cooked TIME/TEMPERATURE CONTROL FOR SAFETY FOOD shall be cooled:
Within 2 hours from 135ºF to 70°F; and
(2) Within a total of 6 hours from 135ºF to 41°F or less.
-3-501.15 Cooling Methods.
A) Cooling shall be accomplished in accordance with the time and temperature criteria specified under
-3-501.14 by using one or more of the following methods based on the type of FOOD being cooled:
1) Placing the FOOD in shallow pans;
2) Separating the FOOD into smaller or thinner portions;
3) Using rapid cooling EQUIPMENT;
4) Stirring the FOOD in a container placed in an ice water bath;
5) Using containers that facilitate heat transfer;
6) Adding ice as an ingredient; or
7) Other effective methods.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to do or maintain the following: maintain the pipes of the suppression system above the six burner stove free of dust, maintain t...
Read full inspector narrative →
Based on observation, interview and record review, the facility failed to do or maintain the following: maintain the pipes of the suppression system above the six burner stove free of dust, maintain the area where the fan vent covers were screwed into the walk-in refrigerator, maintain the light fixtures above the steam table free from a buildup of dust, maintain the floor behind the table with the large mixer on it free from food crumbs and debris, maintain the gasket (a seal which fills the space between two or more mating surfaces, generally to prevent leakage from or into the joined objects while under compression) in the walk-in refrigerator to be tight fitting, maintain the floor of the dry goods storage room free from food crumbs, and maintain two the handles of two utensils in an easily cleanable condition, This practice potentially affected all residents. The facility census was 55 residents.
1. Observation and interview on 11/18/19 from 2:19 P.M. through 6:19 P.M, during the dinner preparation, showed:
- At 2:21 P.M., dust on range hood extinguishing pipes above stove top.
- At 2:25 P.M., there was a dust buildup on fan vent covers in walk-on fridge.
- At 2:28 P.M., there was dust on light fixtures above juice machine table, and the steam table.
- At 2:34 P.M., there were food crumbs behind the table with big mixer on it.
- At 3:24 P.M., a length of the gasket equivalent to 46 inches from the bottom of the walk-in refrigerator door, was peeling away.
- At 3:25 P.M., the Dietary Manager (DM) said the gasket has been coming away from the door for the last month, and
- At 3:27 P.M., there were two utensils in the utensil storage bin with handles that had melted areas, which made them not easily cleanable.
During and interview on 11/18/19 at 6:11 P.M., the DM said:
- He/she told her evening person about mopping that store room on a previous night but he/she must have missed it.
- The table with the mixer did not get moved very often.
- The dietary staff cleaned the fan vent covers of the walk-in refrigerator once per month but not the lip of where the cover was attached to the walk-in refrigerator itself, meet the base.
- He/she did not notice the gasket peeling away until the day of the kitchen observations, and
- The dishwasher should check for the damaged utensils with melted handles.
Record review of the 2009 Food and Drug Administration (FDA) Food Code and Missouri Food Codes, showed:
In Chapter 4-501.11, showed Good Repair and Proper Adjustment.
A) EQUIPMENT shall be maintained in a state of repair and condition that meets the requirements specified under Parts 4-1 and 4-2.
(B) EQUIPMENT components such as doors, seals, hinges, fasteners, and kick plates shall be kept intact, tight, and adjusted in accordance with manufacturer's specifications.
- In Chapter 4-602.13, non-FOOD-CONTACT SURFACES of EQUIPMENT shall be cleaned at a frequency necessary to preclude accumulation of soil residues
- In Chapter 6-501.12, paragraph A, The physical facilities shall be cleaned as often as necessary to keep them clean.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to maintain commode risers in good condition in resident rooms [ROOM NUM...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to maintain commode risers in good condition in resident rooms [ROOM NUMBERS]; to maintain the backing of the 400 Hall shower chair without rips; and to maintain the drawers in resident rooms [ROOM NUMBERS] in good repair. This practice potentially affected at least 20 residents who resided in or used those areas. The facility census was 55 residents.
1. Observation on 11/18/19 11:55 A.M., showed the drawers were off of the slides (the metal pieces that are a part of a drawer unit that allows the actual drawer to move in and out, and facilitated by ball bearings, ensuring that movement is smooth) of the night stand and not closing completely in resident room [ROOM NUMBER].
2. Observations on 11/19/19 showed the following:
- At 8:43 A.M., there was rust on the commode riser in the restroom of 206.
- At 8:50 A.M., the drawer in resident room [ROOM NUMBER] was broken.
- At 10:06 A.M., there were three 3 inch (in) rips in the backing of the shower chair in the 400 Hall Central Bath.
- At 10:14 A.M., the Central Supply Coordinator said no one notified him/her of the damaged shower chair.
- At 11:01 A.M., there was a 10 in crack in the handle of the commode riser in the restroom of resident room [ROOM NUMBER].
- At 11:02 A.M., the Maintenance Director said he/she did not know about the damaged handle of the commode riser.
- At 11:06 A.M., the night stand in resident room [ROOM NUMBER] was damaged.
- At 11:07 A.M., the Maintenance Director said the wheel for one of the drawers in the night stand was absent.
- At 11:19 A.M., the Central Supply Coordinator said no one informed him/her of the rusty commode riser.
- At 11:21 A.M., Housekeeper A said he/she saw the rusty commode riser in the past but has not informed the Central Supply Coordinator of the rusty commode riser, and
- At 11:23 A.M., the Central Supply Coordinator said he/she was not informed of the damaged commode riser in the restroom of resident room [ROOM NUMBER].
During interviews on 11/20/19 at 2:11 P.M., the Housekeeping Supervisor said the following:
- He/she has been the Housekeeping Supervisor since April 2018, and
- He/she has not done a formal training with her housekeeping staff in the reporting of damaged items.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure expired medications were removed from the medication delivery system; discontinued medications were returned to the ph...
Read full inspector narrative →
Based on observation, interview, and record review, the facility failed to ensure expired medications were removed from the medication delivery system; discontinued medications were returned to the pharmacy in a timely manner; multi-dose vials were marked with the date the vial was opened and accessed; narcotic medications were stored in a double-locked system; and medication refrigerator temperatures were monitored to ensure safe storage of refrigerated medications. This deficient practice had the potential to effect all residents who had medications which required refrigeration. The facility census was 55 residents.
Record review of the facility's Refrigerator and Freezer Temperature Log showed:
-The refrigerator needs to be at 36 - 46 degrees Fahrenheit (F).
-The ideal refrigerator temperature was 40 degrees F.
Record review of the facility's Discarding and Destroying Medications policy dated 6/12:
-Medications that cannot be returned to the dispensing pharmacy shall be destroyed as permitted by state regulations.
-All controlled substances shall be retained in a securely locked area with restricted access until authorized individuals destroy them.
-The medication disposition record must contain, as a minimum, the following information:
--The resident's name; the date the medication was destroyed; the name and strength of the medication; the quantity destroyed; reason for destruction; and signature of witnesses.
-Whoever witnesses the destruction/disposal of medications must sign and date the medication disposition record.
Record review of the facility's Storage of Medications policy revised April 2007 showed:
-The facility shall store all drugs and biologicals in a safe, secure, and orderly manner.
-The nursing staff shall be responsible for maintaining medication storage and preparation areas in a clean, safe, and sanitary manner.
-The facility shall not use discontinued, outdated, or deteriorated drugs or biologicals. All such drugs shall be returned to the dispensing pharmacy or destroyed.
-Only persons authorized to prepare and administer medications shall have access to the medication room, including any keys.
1. Record review of the facility's Refrigerator and Freezer Temperature Log for the medication refrigerator showed:
-Medication refrigerator temperatures were to be checked twice daily.
-March 2019 showed temperatures were documented 41 out of 62 opportunities.
-Medication refrigerator temperature logs could not be located for April 2019, May 2019, June 2019, and July 2019.
-August 2019 showed temperatures were documented nine out of 62 opportunities.
-Medication refrigerator temperature logs could not be located for September 2019, October 2019, or November 2019.
During an interview on 11/19/19 at 8:44 A.M., the Assistant Director of Nursing (ADON) said he/She was not sure who was responsible for ensuring the medication refrigerator temperature logs were maintained.
During an interview on 11/19/19 at 9:00 A.M., the Housekeeping Supervisor said:
-Housekeeping staff was responsible for checking the medication refrigerator temperatures.
-He/She was responsible for auditing to ensure the refrigerator temperatures were completed, but he/she had not been doing that.
2. Observation on 11/19/19 at 7:42 A.M. of the 300/400 hall nurse medication cart showed a bottle of Milk of Magnesia with an expiration date of 10/2019.
During an interview and observation of the medication room on 11/19/19 at 7:55 A.M. showed:
-One cardboard box overfilled with medications to return to the pharmacy.
-One medium sized plastic container overfilled with medications to return to the pharmacy.
-Licensed Practical Nurse (LPN) C said he/she thought the medications that need to be returned to the pharmacy have been collected for about a month. The facility was waiting for a pharmacy driver to take them back, but the pharmacy has not had anyone going to the city recently, so they have not been collected for return.
-The medication refrigerator temperature logs had not been completed since 8/31/19. The following medications were stored in the medication refrigerator:
--One bottle of Haldol (an anti-psychotic medication) that had expired on 3/27/19.
--Two opened vials of Tubersol (a medication used for tuberculosis screening) that were not marked with the date the vial was opened.
--16 medication bulbs of Meropenem (an antibiotic).
--Two Lantus pens (a long acting insulin).
--Two bottles of Ativan Intensol (an anti-anxiety medication) which were not in a double locked system.
-A locked box narcotics were stored in contained the following medications:
--Four bottles of Ativan Intensol.
---Two bottles were opened with no date on the bottle when it was opened. LPN C said one bottle belonged to a resident who had expired a while ago and the bottle should have had the contents destroyed.
--11 vials of Ativan 2 milligram/milliliter (mg/ml).
-A second locked box for emergency medications contained the following medications:
--Three Lantus pens (a long acting insulin).
--Three Levemir pens (a long acting insulin).
--Two Novolog pens (a short acting insulin).
--Two Humalog vials (a short acting insulin).
--One Ativan Intensol bottle.
During an interview on 11/19/19 at 8:07 A.M., the Assistant Director of Nursing (ADON) said:
-Staff should check for expired medications on a monthly basis and remove the expired medications from the delivery system.
-Multidose vials should be marked with the date the medication vial was opened.
-Medications removed from the delivery system and placed in the box for return should not be stored for a month or more, however sometimes the pharmacy delivery driver will not pick up the medications because they are not going to the city to the pharmacy to return them.
-He/she thought medications should be returned to the pharmacy at least on a monthly basis.
-The Ativan Intensol for the expired resident should have been destroyed before now.
-He/She thought housekeeping was monitoring the refrigerator temperatures.
-It was important for the medication refrigerator to be maintained within a certain temperature range due to the medications stored in the refrigerator.
3. During an interview on 11/21/19 at 2:44 P.M., the Administrator and Director of Nursing (DON) said:
-He/she expected nursing staff to monitor the medication refrigerator temperatures, not housekeeping staff.
-All expired medications should be removed from the medication delivery system immediately and either returned to the pharmacy or destroyed.
-He/She expected medications that need to be returned to the pharmacy be sent back timely and not overfill two storage containers.
-Multiuse medications should be marked with the date the medication was opened.
-Expired narcotics or narcotics for expired residents should be destroyed immediately
-Staff should check for expired and undated medications on a daily basis, or at least weekly.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Record review of Resident #14's admission Face Sheet showed he/she was admitted to the facility on [DATE] with a diagnosis of...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Record review of Resident #14's admission Face Sheet showed he/she was admitted to the facility on [DATE] with a diagnosis of Type II Diabetes Mellitus (is a disease in which the body does not make enough insulin to control blood sugar levels).
Record review of the resident's Medication Administration Record (MAR) dated 11/1/19 to 11/30/19 showed:
-Accuchecks (blood sugar checks) before meals and at bedtime.
-Novolog Injection flex pen subcutaneous injection (sub-Q) based on a sliding scale.
Record review of the resident's Physician Order Sheet (POS) dated 11/1/19 to 11/30/19 showed:
-Accuchecks (blood sugar checks) before meals and at bedtime.
-Novolog Injection flex pen sub-Q based on a sliding scale (what blood sugar was).
3. Record review of Resident #10's admission Face Sheet showed he/she was admitted to the facility on [DATE] with the following diagnosis of Type I Diabetes Mellitus (insulin-dependent diabetes or juvenile diabetes).
Record review of the resident's MAR dated 11/1/19 to 11/30/19 showed:
-Accuchecks before meals and at bedtime.
-Humalog Kwik 100u/ml sub-Q based on a sliding scale.
Record review of the resident's POS dated 11/1/19 to 11/30/19 showed:
-Accuchecks before meals and at bedtime.
-Humalog Kwik 100u/ml sub-Q based on a sliding scale.
4. Observation on 11/19/19 at 7:16 A.M. of accu check and the glucometer cleaning showed:
-With ungloved hands, LPN D cleaned the glucometer machine with micro kill wipes while in the resident's room.
-With contaminated ungloved hands, LPN D carried the cleaned glucometer out of the resident's room with no barrier or gloves.
-LPN D placed the glucometer on top of the medication cart without a barrier, then sanitized his/her hands.
5. Record review of Resident #20's admission Face sheet showed, he/she was admitted to the facility on [DATE] with a diagnosis of Type II Diabetes Mellitus.
Record review of the resident's MAR dated 11/1/19 to 11/30/19 showed:
-Accuchecks before meals and at bedtime.
-Humalog Kwik 100u/ml sub-Q to give 2 units before meals and at bedtime.
Record review of the resident's POS dated 11/1/19 to 11/30/19 showed:
-Accuchecks before meals and at bedtime.
-Humalog Kwik 100u/ml sub-Q to give 2 units before meals and at bedtime.
Observation on 11/19/19 at 7:35 A.M. of accu check and the glucometer cleaning showed:
-With ungloved hands, LPN D cleaned the glucometer machine with micro kill wipes while in the resident's room.
-With contaminated ungloved hands, LPN D then carried the cleaned glucometer out of the resident room with no barrier or gloves.
-LPN D placed the glucometer on top of the medication cart without a barrier, then sanitized his/her hands.
Observation on 11/19/19 at 7:40 A.M., of insulin administration showed:
-LPN D did not wash or sanitize his/her hands upon entering the resident's room.
-LPN D placed the resident's insulin pen on the resident's bedside table without a protective barrier.
-LPN D did not wash or sanitize his/her hands before leaving the resident's room.
-LPN D exited the resident's room and placed the resident's insulin pen back into the medication cart without sanitizing the insulin pen.
6. During an interview on 11/19/19 at 7:50 A.M., LPN D said:
-He/she should have washed or sanitized his/her hands when entering and before leaving the resident's room.
-He/she should not have put the insulin pen on the resident's bedside table without a barrier.
-He/she should have worn gloves to clean the glucometer and should have had a barrier on the medication cart.
During an interview on 11/21/19 at 2:17 P.M., the DON said:
-He/she expected staff to wash and/or sanitize their hands before placing gloves on hands.
-He/she expected staff to have a clean barrier for clean supplies.
-Staff should have a dirty barrier for contaminated supplies when completing blood glucose monitoring and for insulin.
-He/she expected staff to remove their gloves, and wash or sanitize their hands after removing their gloves before putting on clean gloves.
-It was not appropriate to place contaminated supplies in the medication cart without first sanitizing them.
7. Record review of Resident #32's Face Sheet showed he/she was admitted to the facility on [DATE] and readmitted on [DATE] with the following diagnoses:
-Acute respiratory failure.
-Major Depressive disorder.
-Chronic Obstructive Pulmonary Disease (COPD - a disease process that decreases the ability of the lungs to perform ventilation).
Record review of the resident's electronic medical record and paper medical record showed:
-No documentation of the resident's two-step TB test upon admission to the facility.
-No documentation of the resident's yearly TB test for 2018 or 2019.
8. Record review of Resident #20's Face Sheet showed he/she was admitted to the facility on [DATE].
Record review of the resident's electronic medical record and paper medical record showed:
-No documentation of the resident's two-step TB test upon admission to the facility.
-No documentation of the resident's yearly TB test for 2019.
9. Record review of Resident #198's Face Sheet showed he/she was admitted to the facility on [DATE] with a diagnosis of peripheral neuropathy (damage to the nerves resulting in sensory loss in the extremities).
Record review of the resident's electronic medical record and paper medical record showed no documentation of the resident's two-step TB test upon admission to the facility.
10. Record review of Resident #13's Face Sheet showed he/she was admitted to the facility on [DATE] and readmitted on [DATE] with the following diagnoses:
-Hepatitis C (a viral infection that attacks the liver).
-Chronic kidney disease (CKD - gradual loss of kidney function over time).
-Chronic Obstructive Pulmonary Disease (COPD - a disease process that decreases the ability of the lungs to perform ventilation).
Record review of the resident's electronic medical record and paper medical record showed:
-No documentation of the resident's two-step TB test upon admission to the facility.
-No documentation of the resident's yearly TB test for 2019.
11. Record review of Resident #197's Face Sheet showed he/she was admitted to the facility on [DATE] and readmitted on [DATE] with the following diagnoses:
-Urinary Tract Infection (UTI - an infection of one or more structures in the urinary system).
-Pressure ulcer, unspecified stage.
-Right below the knee amputation.
-Left below the knee amputation.
-Colostomy.
-Paraplegia (loss of movement of both legs and generally the lower trunk).
Record review of the resident's electronic medical record and paper medical record showed:
-The resident had a TB skin test administered on 1/2/18 that was documented as zero millimeters (mm) of induration, indicating a negative test result. The test result documentation did not include the date the test was read.
-No documentation of the resident's a second step TB test was administered seven to 10 days after the first test was read in 2018.
-No documentation of the resident's yearly TB test for 2019.
During an interview on 11/21/19 at 2:48 P.M., the Administrator and DON said:
-The facility started a facility-wide sweep to determine who had received the TB skin testing after discovering during the survey TB skin tests could not be located on the sampled residents.
-The facility was able to locate documentation of a TB skin test for seven residents in 2017, but nothing current for those seven residents.
-A one-step TB skin test was located for a resident admitted earlier this year, but not the second step.
-One new admission in February had both the first step and second step TB skin test completed within the prescribed time frames.
-He/She could not locate TB skin tests for the remaining residents in the facility (46 remaining residents).
-One resident who was a new admission in the last four weeks refused to have a TB skin test when asked during the facility-wide sweep.
-He/She expected staff to administer the first step TB skin test upon admission and read within 48-72 hours.
-He/She expected staff to administer the second step TB skin test seven to 10 days after the first step and read within 48-72 hours.
-He/She expected staff to administer a TB skin test to all residents yearly and read within 48-72 hours.
-Staff had previously documented the TB skin test on paper, but now the documentation should be on the resident's electronic medical record.
12. Record review of the facility's 12 month Infection Control Tracking and Monitoring program showed:
-Only one month tracking, trending, and monitoring could be located, and that was for October 2019.
-No tracking, trending, or monitoring of infections or antibiotics could be located for November 2018 - September 2019.
During an interview on 11/21/19 at 1:33 P.M., the Infection Preventionist said:
-He/she took over as the Infection Control Preventionist on 9/30/19.
-He/she could not locate an Infection Control tracking, trending, or monitoring data previous to his/her taking over the program.
-He/she was able to locate some antibiotic use sheets for June 2019 and August 2019.
-The Infection Control program should have a year's worth of data.
During an interview on 11/21/19 at 2:48 P.M., the Administrator and DON said:
-He/she expected the facility to have an Infection Control Program which consisted of tracking, trending, and monitoring of infections and antibiotic use monthly.
-The Infection Control program should have at least 12 months worth of data to monitor for trends.
-Infection Control program data could not be located prior to the new Infection Preventionist starting in September 2019.
13. Record review of Resident #48's Face Sheet showed he/she was admitted on [DATE] with a diagnosis of diabetes.
During an observation of the resident's blood sugar monitoring on 11/19/19 at 7:02 A.M. with LPN C showed:
-He/she removed and sanitized the glucometer and placed it on a clean barrier in the medication cart drawer.
-He/she administered the resident's medications then exited the resident's room.
-He/she gathered the blood sugar monitoring supplies, removed the glucometer from the medication cart drawer, and put on clean gloves without washing or sanitizing his/her hands.
-He/she entered the resident's room and placed the glucometer, without a barrier, on top of the resident's blanket covering the resident.
-He/she obtained the resident's blood sugar sample, removed his/her gloves, and with ungloved hands, carried the contaminated glucometer out of the resident's room and placed it on top of his/her medication cart without a barrier.
-He/she then sanitized his/her hands, put on gloves, sanitized the glucometer, and placed the glucometer in the medication cart drawer.
-He/She sanitized the top of the medication cart.
14. Record review of Resident #47's Face Sheet showed he/she was admitted to the facility on [DATE].
During an observation of the resident on 11/19/19 at 7:18 A.M. showed LPN C:
-Gathered the resident's glucose monitoring supplies and donned gloves without washing or sanitizing his/her hands.
-Placed the glucometer on the resident's bedside table without a barrier, then removed the now contaminated glucometer to obtain the resident's blood sample.
-He/she placed the contaminated glucometer on the resident's bedside table without a barrier, removed his/her gloves, washed his/her hands, and put on gloves to administer the resident's medications.
-He/she removed his/her gloves, did not wash or sanitize his/her hands, and with ungloved hands, picked up the contaminated glucometer and exited the resident's room.
-He/she placed the contaminated glucometer on top of his/her medication cart without a barrier, and with ungloved contaminated hands, sanitized the glucometer with a bleach wipe and placed the contaminated glucometer in his/her medication cart drawer on top of a barrier.
-He/she sanitized his/her hands, then with ungloved hands, administered the resident's insulin injection.
During an interview on 11/19/19 at 7:33 A.M., LPN C said:
-He/she should have had gloves on when he/she administered the resident's insulin injection.
-He/she should have washed or sanitized his/her hands before and after every glove change.
-He/she should have placed the glucometer on a barrier in the resident room and not on a blanket or bedside table.
-He/she should have had gloves on when handling the contaminated glucometer.
During an interview on 11/21/19 at 2:27 P.M., the Administrator and DON said:
-Staff should only place glucometers on a barrier, it was not appropriate to place the glucometer on top of a resident blanket or on top of a resident bedside table.
-Staff should wash or sanitize their hands after every glove change.
-Staff should not touch a contaminated glucometer with ungloved hands.
15. Record review of Resident #22's Face Sheet showed he/she was admitted to the facility on [DATE] and readmitted on [DATE].
Record review of the resident's quarterly MDS dated [DATE] showed he/she:
-Was severely cognitively impaired.
-Had an indwelling catheter.
-Required limited staff assistance for toileting and personal hygiene.
Record review of the resident's November 2019 POS showed the resident had a suprapubic catheter (a urinary bladder catheter inserted through the skin about one inch above the symphysis pubis).
Record review of the resident's urine culture dated 11/18/19 showed the resident's urine specimen was positive for Methicillin Resistant Staphylococcus Aureus (MRSA - a type of bacteria that is resistant to many antibiotics).
Observation on 11/18/19 at 3:29 P.M., 11/19/19 at 7:30 A.M. and 12:05 P.M. showed:
-A cart with personal protection equipment (PPE) such as gowns, gloves, and masks was outside his/her room and two red barrels were inside his/her room by the door.
-No sign directing staff and visitors to see the nurse.
Observation on 11/20/19 at 8:31 A.M., 10:45 A.M., and 11:25 A.M. showed the isolation cart was inside the resident's room in front of his/her window.
During an interview on 11/20/19 at 11:26 A.M., Certified Nursing Assistant (CNA) C said:
-He/she was not aware of any resident on isolation precautions.
-If a resident was on isolation precautions, an isolation cart should be outside the resident's door and not in the resident's room by the window.
-He/she was not aware the resident was on isolation precautions.
Observation on 11/21/19 at 9:20 A.M. showed the isolation cart was inside the resident's room in front of his/her window
During an interview on 11/21/19 at 12:46 P.M., CNA D said:
-Staff did not need to do anything special when emptying the resident's Foley catheter.
-He/she did not know of any resident's on contact isolation precautions.
-He/she was not aware the resident was on contact isolation precautions.
-If a resident was on isolation precautions, there would be a sign outside his/her door to see the nurse.
-If a resident was on isolation precautions, an isolation cart would be outside the resident's door and not in the resident's room.
During an interview on 11/21/19 at 1:33 P.M., the Infection Preventionist said:
-If a resident is positive for MRSA, he/she should have an isolation cart outside his/her room with PPE supplies in the cart.
-Staff and visitors were expected to put on a gown and gloves prior to entering the resident's room, especially if they may come in contact with the source of the resident's infectious organism.
-He/she did not know why the isolation cart would be in the resident's room.
During an interview on 11/21/19 at 2:48 P.M., the Administrator and DON said:
-If a resident has an infection that required isolation precautions, the resident should have an isolation cart outside his/her room and not in his/her room.
-A sign should be posted outside the resident's room for staff and visitors to see the nurse prior to entering the resident's room.
-Staff should gown and glove before entering the resident's room to provide catheter care or emptying the resident's catheter.Based on observation, interview, and record review, the facility failed to ensure infection control practices to prevent cross contamination were implemented by failing to ensure proper hand hygiene was completed according to standards of practice during wound care for one sampled resident (Resident #47); to ensure proper hand hygiene and gloving was practiced during a glucometer cleaning and insulin administration for three sampled residents (Residents #14, #10, and #20); to have an Infection Control tracking and trending program for the previous 12 month cycle;to ensure residents were assessed and monitored for signs and symptoms of tuberculosis upon admission and annually for five out of five sampled residents (Resident #13, #20, #32, #197, and #198); to ensure infection control protocols were maintained to prevent cross contamination during blood glucose monitoring for two sampled resident's (Resident #47 and #48), and to ensure infection control protocols were maintained for one supplemental resident on contact isolation precautions (Resident #22) out of 16 sampled residents. The facility also failed to include text flow diagrams of where the pipes from the various hot water heater were directed to and a listing of areas where Legionella sp. (a form of pneumonia, caused by the bacterium Legionella pneumophila found in both potable and nonpotable water systems could grow and spread), in the facility's waterborne illness prevention plan. This practice potentially affected all residents and facility staff. The facility census was 55 residents.
Record review of the facility's Personal Protective Equipment - Gloves policy revised August 2009 showed:
-All employees must wear gloves when touching blood, body fluids, secretions, excretions, mucous membranes, and/or non-intact skin.
-The use of disposable gloves is indicated during all cleaning of blood, body fluids, and decontaminating procedures.
-Wash your hands after removing gloves.
Record review of the facility's Infection Control Program - Antibiotic Stewardship policy dated November 2017 showed:
-This community has established an infection prevention and control program that includes protocols to establish a system for the use and monitoring of adverse effects of antibiotics.
-Residents who need an antibiotic are prescribed an antibiotic.
-Antibiotic Stewardship: a set of commitments and actions designed to optimize the treatment of infections while reducing the adverse effects associated with antibiotic use.
-Loeb Criteria: minimum criteria for the initiation of antibiotics.
-McGeer Criteria: surveillance criteria.
-The basic tenets of an antibiotic stewardship program include:
--Appropriate prescribing.
--Appropriate administration.
--Management practices to reduce inappropriate use to ensure that residents receive the right antibiotic for the right indication, right does, and right duration.
-Potential side effects to monitor for with use of antibiotics:
--Increased adverse drug events and drug interactions.
--Serious diarrheal infections for Clostridium Difficile.
--Colonization and/or infection with antibiotic resistant organisms.
-Core elements of an antibiotic stewardship program:
--Track measures of antibiotic use on the facility, one process, and one outcomes measure.
--Regular reporting on antibiotic use and resistance to relevant staff, such as prescribing clinicians and nursing staff.
-The program is a portion of the overall Infection Prevention and Control Program.
-Monitoring of Antibiotic Use:
--Monitoring is initiated with any order written at any time for an antibiotic.
--Obtaining Antibiogram from a contracted laboratory as a summary of antibiotic susceptibility over the past 12 - 24 months.
--Compile a report on antibiotic utilization (from sources such as the pharmacy and the electronic health record itself) and provide feedback at least quarterly to each practitioner.
Record review of the facility's Tuberculosis Screening - Administration and Interpretation of Tuberculin Skin Tests revised December 2009 showed:
-The facility will administer and interpret tuberculin skin tests (TST) in accordance with recognized guidelines and pertinent regulations.
-Only qualified healthcare practitioners will administer and interpret the TST for employees and/or residents.
-Individuals with less than 10 millimeters (mm) of induration, unless otherwise indicated, will receive a booster of 0.1 ml (5 tuberculin units) of purified protein derivative (PPD) one to two weeks after the initial TST.
-A qualified nurse or healthcare practitioner will interpret the TST 48 to 72 hours after administration. All test results must be read in mm.
-The facility will not accept an interpretation of the TST by an employee or resident, but will accept an interpretation by a private physician within the 48 to 72 hour time frame.
Record review of the facility's Handwashing/Hand Hygiene policy revised April 2010 showed:
-All personnel shall follow the handwashing/hand hygiene procedures to help prevent the spread of infections to other personnel, residents, and visitors.
-Employees must wash their hands for at least fifteen (15) seconds using antimicrobial or non-antimicrobial soap and water under the following conditions:
--Before and after direct resident contact (for which hand hygiene is indicated by acceptable professional practice).
--Before and after entering isolation precaution settings.
--Before and after assisting a resident with personal care (e.g., oral care, bathing).
--Before and after changing a dressing.
--After handling soiled or used linens, dressings, bedpans, catheters and urinals.
--After handling soiled equipment.
--After removing gloves.
-Hand hygiene is always the final step after removing and disposing of personal protective equipment.
Record review of the facility's Infection Control Guidelines for Nursing Procedures revised June 2013 showed:
-Transmission-Based Precautions will be used whenever measures more stringent than Standard Precautions are needed to prevent the spread of infection.
-Recommended hand-washing techniques include: Washing hands for ten (10) to fifteen (15) seconds using antimicrobial or non-antimicrobial soap and water under the following conditions:
--Before and after direct contact with residents.
--When hands are visibly dirty or soiled with blood or other body fluids.
--After contact with blood, body fluids, secretions, mucous membranes, or non-intact skin.
--After removing gloves.
--After handling items potentially contaminated with blood, body fluids, or secretions.
-In most situations, the preferred method of hand hygiene is with an alcohol-based hand rub. If hands are not visibly soiled, use an alcohol-based hand rub containing 60-95% ethanol or isopropanol for the following situations:
--Before and after direct contact with residents.
--Before donning (putting on) sterile gloves.
--Before performing any non-surgical invasive procedures.
--Before preparing or handling medications.
--Before handling clean or soiled dressings, gauze pads, etc.
--Before moving from a contaminated body site to a clean body site during resident care.
--After contact with a resident's intact skin.
--After handling used dressings, contaminated equipment, etc.
--After contact with objects (e.g., medical equipment) in the immediate vicinity of the resident.
--After removing gloves.
Record review of the facility's Infection Control Program - Antibiotic Stewardship policy dated November 2017 showed:
-This community has established an infection prevention and control program that includes protocols to establish a system for the use and monitoring of adverse effects of antibiotics.
-Residents who need an antibiotic are prescribed an antibiotic.
-Antibiotic Stewardship: a set of commitments and actions designed to optimize the treatment of infections while reducing the adverse effects associated with antibiotic use.
-Loeb Criteria: minimum criteria for the initiation of antibiotics.
-McGeer Criteria: surveillance criteria.
-The basic tenets of an antibiotic stewardship program include:
--Appropriate prescribing.
--Appropriate administration.
--Management practices to reduce inappropriate use to ensure that residents receive the right antibiotic for the right indication, right does, and right duration.
-Potential side effects to monitor for with use of antibiotics:
--Increased adverse drug events and drug interactions.
--Serious diarrheal infections for Clostridium Difficile.
--Colonization and/or infection with antibiotic resistant organisms.
-Core elements of an antibiotic stewardship program:
--Track measures of antibiotic use on the facility, one process, and one outcomes measure.
--Regular reporting on antibiotic use and resistance to relevant staff, such as prescribing clinicians and nursing staff.
-The program is a portion of the overall Infection Prevention and Control Program.
-Monitoring of Antibiotic Use:
--Monitoring is initiated with any order written at any time for an antibiotic.
--Obtaining Antibiogram from a contracted laboratory as a summary of antibiotic susceptibility over the past 12 - 24 months.
--Compile a report on antibiotic utilization (from sources such as the pharmacy and the electronic health record itself) and provide feedback at least quarterly to each practitioner.
Record review of the facility's Isolation-Initiating Transmission-Based Precautions policy revised November 2017 showed:
-When Transmission-Based Precautions are implemented, the following is recommended:
--Protective equipment (i.e., gloves, gowns, masks, etc.) is maintained near the resident's room so that everyone entering the room can access what they need.
--Post the appropriate notice on the room entrance door and on the front of the resident's chart so that all personnel will be aware of precautions, or be aware that they must first see a nurse to obtain additional information about the situation before entering the room.
Record review of the facility's Infection Prevention and Control Program revised November 2017 showed:
-The infection prevention and control program (IPCP), that follows national standards, will at a minimum include systems for:
--Prevention.
--Identification.
--Reporting.
--Investigating.
--Controlling infections and communicable diseases for all residents, staff, volunteers, visitors, and other individuals providing services under a contractual assessment.
-The objectives of our infection control policies and practices are to:
--Prevent, detect, investigate, and control infections in the facility.
--Establish guidelines for implementing Isolation Precautions, including Standard and Transmission-Based Precautions.
--Maintain records of incidents and corrective actions related to infections.
--Provide guidelines for the safe cleaning and reprocessing of reusable resident-care equipment.
-[The] Infection Control Program is reviewed at least annually with the Facility Assessment.
Record review of the Centers for Medicare and Medicaid Services (CMS) Survey and Certification letter dated 6/2/17, showed the facility should develop and implement a water management program that considers the American Society of Heating Refrigerating and Air Conditioning Engineers (ASHRAE) industry standard and the CDC toolkit.
The toolkit should contain the following: text and flow diagrams, identify areas where Legionella could grow and spread, that the team has conducted a water program review at least annually, as stated. The annual review should: 1) be implemented; 2) record findings and updates; 3) record participants; and 4) be submitted to the Executive Director.
1. Record review of Resident #47's Face Sheet showed he/she was admitted to the facility on [DATE] with diagnoses including acute respiratory failure, chronic obstructive pulmonary disease (COPD-progressive lung disease), kidney disease, heart disease, heart failure, peripheral vascular disease (PVD-a blood circulation disorder that causes the blood vessels outside of your heart and brain to narrow, block, or spasm), high blood pressure and obesity.
Record review of the resident's Medical Record showed the resident did not have an admission Minimum Data Set (MDS a federally mandated assessment tool to be completed by facility staff for care planning) completed yet.
Record review of the resident's Physician's Telephone Order dated 11/15/19, showed a physician's orders:
-No Physical Therapy and keep legs elevated for five days, perform daily weights and Levaquin 500 milligrams (mg) daily for seven days for cellulitis (fluid in the tissues).
-Cleanse the wound with wound cleanser, pat dry, cover with Xeroform and border gauze (an absorptive dressing that consists of three layers to ensure wound healing) daily until healed.
Observation on 11/20/19 at 10:34 A.M., Licensed Practical Nurse (LPN) A brought his/her supplies into the residents room and placed them on a clean paper towel on the resident's dresser. He/she then:
-Washed his/her hands, using her hand to dispense the paper towels, dried his/her hands and used the paper towel to turn off the water, then gloved.
-The resident was sitting in his/her wheelchair with a sock on his/her right foot that was elevated. LPN A placed a pad on the floor then removed the resident's old dressing.
-The resident had very dry, flaky skin on his/her foot and leg and there was a wound that was circular and quarter sized, right over his/her ankle bone. There was a flap of skin covering most of the wound and the open area was the shape of a crescent, along the right edge of the wound. There was minimal drainage on the old dressing and no odor.
-Using wound cleanser and a clean cotton swab, LPN A sprayed the resident's skin with wound cleanser and cleaned the wound.
-He/she then de-gloved, washed his/her hands and used his/her clean hand to pull the paper towel dispenser. He/she dried his/her hands and used the paper towel to turn off the water.
-He/she then gloved, opened two packets of skin prep and wiped the wound area with the skin prep pads.
-He/she then cut Xeroform and placed it on the wound, then covered it with a dated dressing and placed the resident's sock back on. He/She placed the resident's soft brace over his/her.
-LPN A then picked up all of the used supplies and discarded them, degloved and placed them in the trash, dispensed the paper towels then washed his/her hands, turning off the water with the paper towel.
During an interview on 11/20/19 at 10:48 A.M., LPN A said he/she may not have used his/her paper towel to pull down the paper towels during handwashing every time he/she washed his/her hands, but remembered pulling it down with the tip of the paper towel once.
During an interview on 11/21/19 at 2:23 P.M., the Administrator and Director of Nursing (DON) said:
-Nursing staff were supposed to wash their hands before and after removing gloves.
-The nursing staff not use their hand to dispense the paper towels after washing their hands.
-They should not turn off the water with their hands once done washing their hands.
16. Record review of the facility's Legionella/Waterborne Illness plan dated 11/17, showed the absence of the following:
-Text and flow diagrams of pipes from various hot water heaters in the facility and the destinations of those pipes.
-Areas or rooms which cont