CROWN REHAB AND HEALTHCARE CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Crown Rehab and Healthcare Center has a Trust Grade of D, indicating below-average performance with some concerns about care quality. It ranks #243 out of 479 facilities in Missouri, placing it in the bottom half of the state, and #4 out of 8 in Cass County, meaning only three local options are better. The facility's situation appears stable, as it reported 11 issues both in 2023 and 2025. Staffing is a weakness, with a poor rating of 1 out of 5 stars, although turnover is slightly better than the state average at 56%. Specific incidents of concern include failures in food safety standards that could affect all residents and not properly notifying residents about their care plan meetings, which can hinder effective communication and care. While there are no fines recorded, and overall health inspections scored average, the facility has significant areas needing improvement.
- Trust Score
- D
- In Missouri
- #243/479
- Safety Record
- Low Risk
- Inspections
- Holding Steady
- Staff Stability ⚠ Watch
- 56% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Missouri facilities.
- Skilled Nurses ⚠ Watch
- Each resident gets only 28 minutes of Registered Nurse (RN) attention daily — below average for Missouri. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 31 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Near Missouri average (2.5)
Below average - review inspection findings carefully
Near Missouri avg (46%)
Frequent staff changes - ask about care continuity
Part of a multi-facility chain
Ask about local staffing decisions and management
8 points above Missouri average of 48%
The Ugly 31 deficiencies on record
Mar 2025
11 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure completion, submission and retention of a Level I Nursing Fa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure bathing/showers were completed twice weekly and...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure communication and coordination of care with a r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to maintain audiological (science and medicine concerned with the sens...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0687
(Tag F0687)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide necessary treatment and foot care for one sam...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0728
(Tag F0728)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure two sampled Nurse Assistants (NAs) (NA A and NA B) completed the Certified Nurse Assistant (CNA) training program within four months...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0553
(Tag F0553)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to notify the resident or the resident's representative of meetings fo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to complete annual evaluations for two sampled Certified Nursing Assistants (CNA),(CNA N and CNA P); and failed to provide the annual twelve h...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
4. During an interview on 3/17/25 at 10:44 A.M., Resident #25 said he/she ate in the Main Dining Room in the assisted section and the food was frequently cold.
5. During an interview on 3/17/25 at 9:4...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to maintain the cleanliness in the kitchen by not removing rust and grime from one shelf in the walk-in cooler; failed to clean and maintain fou...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure accurate and timely tuberculosis (TB - a commu...
Read full inspector narrative →
Jul 2023
11 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure one sampled resident (Resident #64) had a code status upon ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to reassess the effectiveness of individualized resident care and inte...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to complete labs as ordered for one sampled resident (Resident #31) out of five residents sampled for unnecessary medications. The facility ce...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide nail care for one sampled resident (Resident #...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Review of Resident #13's face sheet showed he/she was admitted on [DATE] with the following diagnoses:
-Need for physical ass...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0825
(Tag F0825)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide restorative care (a program to maintain a person's highest level of physical, mental, and psychosocial function in order to prevent...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
3. Review of the CMT medication cart (100/200 hallway) narcotic count sheet on 7/17/23 at 6:07 A.M., showed:
-The off going LPN pre-signed the narcotic count sheet before the day shift CMT or LPN came...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure medications were stored securely; failed to ensure other objects were not in with the residents' prescribed medication...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5. Review of Resident #23's face sheet, undated, showed:
-The resident had the following diagnoses:
--Senile degeneration of the...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to follow pre-prepared menus to ensure they met the nutritional adequacy needs of residents, in accordance with established nati...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to keep the Dry Storage (DS) room, walk-in refrigerator, and walk-in freezer floors clean; to maintain sanitary beverage dispens...
Read full inspector narrative →
Mar 2022
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Record review of Resident #35's undated facesheet showed he/she was admitted to the facility on [DATE] with the following dia...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to administer Levothyroxine (Synthroid used for thyroid ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to identify edema with a weight gain and notify the Phys...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow through with pharmacy recommendations to reduce anti-psychot...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Record review of Resident #35's undated face sheet showed he/she was admitted to the facility on [DATE] with the following di...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure they completed a check of the Employee Disqualification List (EDL) and/or Criminal Background Check (CBC) and/or the Nurse Aide (NA)...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 8. Record review of Resident #73's undated face sheet showed he/she was admitted to the facility on [DATE] with the following di...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to establish and maintain annual competencies and skill sets of at least 12 hours of education in-services/training of facility licensed nursi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to ensure staffing information was posted in a prominent place, readily accessible to residents and visitors. This practice had t...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No major safety red flags. No abuse findings, life-threatening violations, or SFF status.
- • No fines on record. Clean compliance history, better than most Missouri facilities.
- • 31 deficiencies on record. Higher than average. Multiple issues found across inspections.
- • Grade D (45/100). Below average facility with significant concerns.
- • 56% turnover. Above average. Higher turnover means staff may not know residents' routines.
About This Facility
What is Crown Rehab And Healthcare Center's CMS Rating?
CMS assigns CROWN REHAB AND HEALTHCARE CENTER an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Missouri, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Crown Rehab And Healthcare Center Staffed?
CMS rates CROWN REHAB AND HEALTHCARE CENTER's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 56%, which is 10 percentage points above the Missouri average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs. RN turnover specifically is 69%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Crown Rehab And Healthcare Center?
State health inspectors documented 31 deficiencies at CROWN REHAB AND HEALTHCARE CENTER during 2022 to 2025. These included: 31 with potential for harm.
Who Owns and Operates Crown Rehab And Healthcare Center?
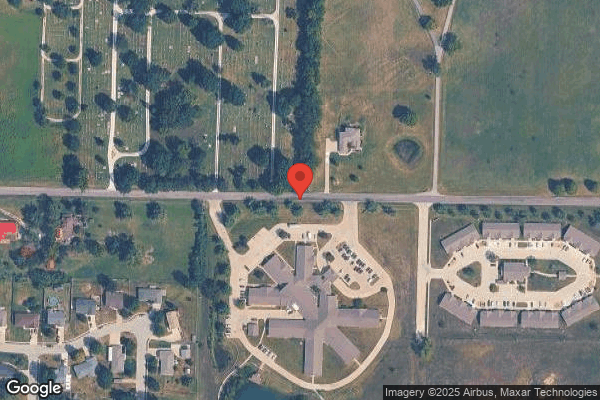
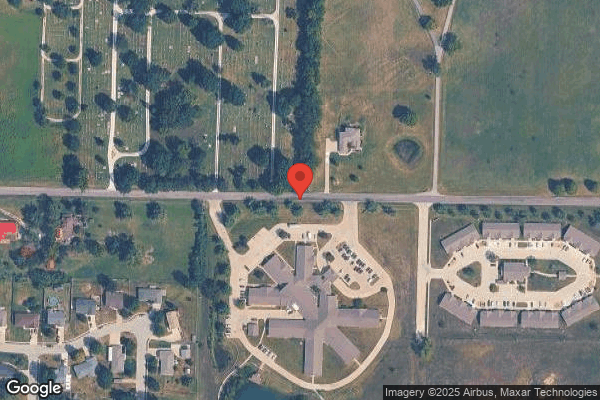
CROWN REHAB AND HEALTHCARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by AMA HOLDINGS, a chain that manages multiple nursing homes. With 118 certified beds and approximately 99 residents (about 84% occupancy), it is a mid-sized facility located in HARRISONVILLE, Missouri.
How Does Crown Rehab And Healthcare Center Compare to Other Missouri Nursing Homes?
Compared to the 100 nursing homes in Missouri, CROWN REHAB AND HEALTHCARE CENTER's overall rating (2 stars) is below the state average of 2.5, staff turnover (56%) is near the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Crown Rehab And Healthcare Center?
Based on this facility's data, families visiting should ask: "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's high staff turnover rate and the below-average staffing rating.
Is Crown Rehab And Healthcare Center Safe?
Based on CMS inspection data, CROWN REHAB AND HEALTHCARE CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Missouri. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Crown Rehab And Healthcare Center Stick Around?
Staff turnover at CROWN REHAB AND HEALTHCARE CENTER is high. At 56%, the facility is 10 percentage points above the Missouri average of 46%. Registered Nurse turnover is particularly concerning at 69%. RNs handle complex medical decisions and coordinate care — frequent RN changes can directly impact care quality. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Crown Rehab And Healthcare Center Ever Fined?
CROWN REHAB AND HEALTHCARE CENTER has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Crown Rehab And Healthcare Center on Any Federal Watch List?
CROWN REHAB AND HEALTHCARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.