OZARK NURSING AND CARE CENTER
Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Ozark Nursing and Care Center has received a Trust Grade of F, indicating poor performance with significant concerns about care quality. It ranks #434 out of 479 nursing homes in Missouri, placing it in the bottom half, and it's the lowest-ranked facility in Christian County. While the facility is showing improvement, having reduced the number of issues from 11 in 2024 to 4 in 2025, there are still serious concerns, including $48,132 in fines, which is higher than 80% of Missouri facilities, signaling ongoing compliance problems. Staffing is a relative strength, with a turnover rate of 0%, which is well below the state average; however, the overall staffing rating is just 1 out of 5 stars, indicating significant challenges. Notable incidents include a critical failure to monitor a resident who was found unresponsive after over 11 hours without checks, and a medication error that contributed to another resident's death. Families should weigh these serious weaknesses against the facility's low turnover as they consider care options.
- Trust Score
- F
- In Missouri
- #434/479
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- Turnover data not reported for this facility.
- Penalties ○ Average
- $48,132 in fines. Higher than 74% of Missouri facilities. Some compliance issues.
- Skilled Nurses ○ Average
- RN staffing data not reported for this facility.
- Violations ⚠ Watch
- 39 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Missouri average (2.5)
Significant quality concerns identified by CMS
Above median ($33,413)
Moderate penalties - review what triggered them
The Ugly 39 deficiencies on record
Jun 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to the resident's right to be free from physical and verbal abuse by staff when one staff member (Certified Nurses Aide (CNA) B)...
Read full inspector narrative →
Mar 2025
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to report an allegation of staff to resident abuse to the Department o...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to take steps to protect all residents after staff failed to report th...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to post the current daily nurse staffing information in a clear and readable format and in a prominent place readily accessible ...
Read full inspector narrative →
Dec 2024
5 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to ensure medications were not left at bedside for a resident that was not assessed to self-administer medications for one resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to develop and implement a complete care plan for each resident when staff failed to care plan smoking on the facility's property for two resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to ensure effective pain management was provided for every resident when staff failed to keep pain medication in stock and faile...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to provide respiratory care per standard of practice for all residents when staff failed to administer oxygen as ordered for one...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and record review, the facility failed to ensure all food stored in the main kitchen was free from possible contamination when staff failed ensure food was appropria...
Read full inspector narrative →
Sept 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide care per standards of practice when staff fai...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure the facility promoted each resident's right to self-determin...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to ensure the Director of Nursing (DON) did not serve as a charge nurse or certified nurse aide (CNA) when the facility census was greater tha...
Read full inspector narrative →
Jul 2024
2 deficiencies
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
Based on record review and interview, the facility failed to protect each resident's right to be free from neglect when staff failed to check on one resident (Resident #1), who resided in the locked s...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to maintain a current and accurate facility assessment when facility staff failed to review and update the comprehensive facility assessment a...
Read full inspector narrative →
Mar 2024
1 deficiency
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0760
(Tag F0760)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure all residents were free from significant medication errors w...
Read full inspector narrative →
Oct 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to protect all residents from misappropriation of resident property when staff could not account for a missing narcotic for one ...
Read full inspector narrative →
Sept 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to immediately report all allegations of abuse to management immediate...
Read full inspector narrative →
Jul 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
1. Please refer F656 at event ID P6OT12, exit date 07/10/23 for citation details.
MO00221048
Read full inspector narrative →
May 2023
12 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to complete a baseline care plan for two residents (Residents #129 an #13) out of a sample of 22 residents including two closed records. The f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure all residents had a comprehensive care plan that addressed e...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0678
(Tag F0678)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure a resident's choice of code status was accessi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure all residents were free from significant medication errors when staff administered insulin medication (used to help co...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure all medication were stored in accordance with accepted professional standards when staff stored intravenous medication...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility staff failed to practice acceptable standards of practice of in...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure staff treated residents with dignity and respect to enhance each residents' quality of life when staff stood while ass...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Review of Resident #60's face sheet showed the following:
-admission date of 2/9/22;
-Diagnoses included atrial fibrillation ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure dietary staff stored, prepared, and served food in a manner that protected it from possible contamination in accordanc...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to adequately equip and maintain the resident call light...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure dietary staff maintained non-food contact surfaces in the kitchen in the a sanitary fashion when there was an accumula...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0882
(Tag F0882)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to designate one or more individuals, qualified by completing specialized training in infection prevention and control, as the Infection Preve...
Read full inspector narrative →
Feb 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to protect all residents' right to be free from verbal abuse by staff when a staff member (Certified Medication Tech (CMT) B) cursed and made ...
Read full inspector narrative →
Jan 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide complete wound assessments, tracking, monitor...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to use appropriate infection control procedures to prevent the spread of bacteria or other infectious carrying contaminants, whe...
Read full inspector narrative →
Dec 2022
2 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that all alleged violations involving abuse were reported im...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to begin an immediate investigation and failed to take steps to immedi...
Read full inspector narrative →
Jan 2020
4 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to provide a Skilled Nursing Facility Advance Beneficiary Notice (SNFABN - form CMS-10055) or a denial letter at the initiation, reduction, or...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to notify the resident and the resident's representative in writing of...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility staff failed to post the required daily nurse staffing hours in a prominent place readily accessible to residents and visitors, failed ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0923
(Tag F0923)
Could have caused harm · This affected most or all residents
Based on observation and interview, the facility failed to maintain the residents' bathroom exhaust ventilation system in proper working condition when all residents' bathrooms did not have functionin...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "What safeguards are in place to prevent abuse and neglect?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: Federal abuse finding, 2 life-threatening violation(s), $48,132 in fines, Payment denial on record. Review inspection reports carefully.
- • 39 deficiencies on record, including 2 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • $48,132 in fines. Higher than 94% of Missouri facilities, suggesting repeated compliance issues.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Ozark Nursing And's CMS Rating?
CMS assigns OZARK NURSING AND CARE CENTER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Missouri, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Ozark Nursing And Staffed?
CMS rates OZARK NURSING AND CARE CENTER's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes.
What Have Inspectors Found at Ozark Nursing And?
State health inspectors documented 39 deficiencies at OZARK NURSING AND CARE CENTER during 2020 to 2025. These included: 2 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death) and 37 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Ozark Nursing And?
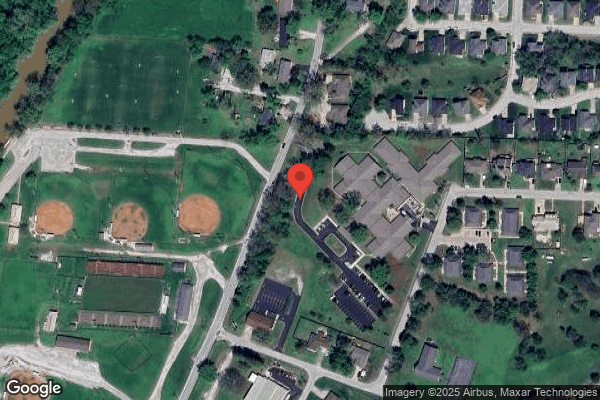
OZARK NURSING AND CARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 93 certified beds and approximately 66 residents (about 71% occupancy), it is a smaller facility located in OZARK, Missouri.
How Does Ozark Nursing And Compare to Other Missouri Nursing Homes?
Compared to the 100 nursing homes in Missouri, OZARK NURSING AND CARE CENTER's overall rating (1 stars) is below the state average of 2.5 and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Ozark Nursing And?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" These questions are particularly relevant given the facility's Immediate Jeopardy citations, the substantiated abuse finding on record, and the below-average staffing rating.
Is Ozark Nursing And Safe?
Based on CMS inspection data, OZARK NURSING AND CARE CENTER has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). Inspectors have issued 2 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Missouri. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Ozark Nursing And Stick Around?
OZARK NURSING AND CARE CENTER has not reported staff turnover data to CMS. Staff turnover matters because consistent caregivers learn residents' individual needs, medications, and preferences. When staff frequently change, this institutional knowledge is lost. Families should ask the facility directly about their staff retention rates and average employee tenure.
Was Ozark Nursing And Ever Fined?
OZARK NURSING AND CARE CENTER has been fined $48,132 across 2 penalty actions. The Missouri average is $33,560. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Ozark Nursing And on Any Federal Watch List?
OZARK NURSING AND CARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.