IVY AT DEER LODGE




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Ivy at Deer Lodge has received a Trust Grade of F, indicating significant concerns about its quality of care. It ranks #50 out of 59 facilities in Montana, placing it in the bottom half, and is the only option in Powell County. Unfortunately, the facility is worsening, with the number of issues increasing from 15 in 2023 to 17 in 2024. Staffing is below average, with a rating of 2 out of 5 stars and a concerning turnover rate of 68%, higher than the state average. There have been serious incidents, including a resident who developed severe pressure ulcers and another who suffered from inadequate pain management during care, ultimately leading to a decline in health. While the facility does have good quality measures rated at 4 out of 5 stars, the overall picture raises significant red flags for families considering this home.
- Trust Score
- F
- In Montana
- #50/59
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 68% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ⚠ Watch
- $82,446 in fines. Higher than 83% of Montana facilities, suggesting repeated compliance issues.
- Skilled Nurses ⚠ Watch
- Each resident gets only 24 minutes of Registered Nurse (RN) attention daily — below average for Montana. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 41 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Below Montana average (2.9)
Significant quality concerns identified by CMS
22pts above Montana avg (46%)
Frequent staff changes - ask about care continuity
Well above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
20 points above Montana average of 48%
The Ugly 41 deficiencies on record
Nov 2024
3 deficiencies
3 IJ (1 affecting multiple)
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. During an interview on 11/20/24 at 9:49 a.m., staff member F said resident #3 was able to walk prior to his hip fracture. Sta...
Read full inspector narrative →
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0697
(Tag F0697)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to assess, document, treat, and monitor pain for 1 (#4) of 6 sampled r...
Read full inspector narrative →
CRITICAL
(K)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Pressure Ulcer Prevention
(Tag F0686)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. During an interview on 11/20/24 at 9:49 a.m., staff member F said resident #3 was able to walk prior to his hip fracture. Sta...
Read full inspector narrative →
Oct 2024
5 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide written notice of the reason for a facility-initiated transfer to a resident or the resident's representative, for 3 (#s 36, 54, an...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to remove and dispose of expired medical supplies in the medication room. These failures increased the risk of expired medical supplies being us...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure food items in the refrigerator and freezer were labeled and dated, failed to maintain a clean and sanitary environment...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0565
(Tag F0565)
Minor procedural issue · This affected multiple residents
Based on interview and record review, the facility failed to provide evidence to show the facility took action to acknowledge and resolve, or attempt to resolve, all concerns brought forth by the resi...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0625
(Tag F0625)
Minor procedural issue · This affected multiple residents
Based on interview and record review, the facility failed to provide the required bed hold notice to the resident or the resident's representatives prior to, or timely after, a transfer, for 2 (#s 54 ...
Read full inspector narrative →
Sept 2024
5 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0563
(Tag F0563)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to allow free access to visitors for 1 (#2) of 2 sampled residents. Findings include:
During a telephone interview on 9/18/24 at 8:46 a.m., NF2...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to meet professional standards for medications being administered, per the physician's order, and the resident had insomnia, for 1(#2) of 1 sa...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0849
(Tag F0849)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to provide hospice services in coordination with the management and staff of the nursing home per the hospice agreement for 1 (#2...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0555
(Tag F0555)
Could have caused harm · This affected multiple residents
Based on interviews and record reviews the facility failed to allow the residents a choice for their attending physician for 3 (#s 2, 3, and 4) of 3 sampled residents for physician services. Findings ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation and interview the facility failed to provide a clean homelike environment for 3 (#s 2, 3, and 4) of 3 sampled residents and had the potential to affect all residents who go to the...
Read full inspector narrative →
Jul 2024
4 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected multiple residents
Based on interviews and record review, the facility failed to refund the resident or resident representative refunds within 30 days from the resident's date of discharge from the facility for 2 (#s 1 ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected multiple residents
Based on interviews and record review, it was identified the facility had a system breakdown when a new CNA was hired and left alone prior to the end of the new hire orientation period, and the employ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected multiple residents
Based on interviews and record review, the facility failed to thoroughly investigate allegations of neglect, misappropriation of resident property, and abuse for 7 (#s 3, 4, 5, 6, 7, 8, and 9) of 14 s...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
Based on interviews and record review, the facility failed to provide to provide necessary staff training for a new employee, and ensure the employee was competent, and then provide sufficient supervi...
Read full inspector narrative →
Nov 2023
10 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to develop and implement a comprehensive person-centered care plan for each resident, including the resident's preferences and f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to identify the extent of the weight loss for 1 (#34) of...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure resident POLST forms were complete, and included the patients/legal decision maker signature, date, and time, for 4 (#s 3, 6, 11, an...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to maintain a clean environment, related to housekeeping services, for 5 (#s 7, 10, 24, 26, and 34) of 15 sampled residents. Thi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected multiple residents
2. During an interview on 11/6/23 at 11:59 a.m., resident #37 stated she is only in the nursing home for rehabilitation and will be leaving soon.
During an interview on 11/6/23 at 1:46 p.m., resident...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected multiple residents
During an interview on 11/6/23 at 11:59 a.m., resident #37 stated she thought the food was awful.Based on observation and interview, the dietary department failed to honor resident food preferences an...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to provide oversight to ensure the dietary manager had the appropriate competencies and skills to carry out the functions for th...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to identify quality deficiencies through the utilization of their QAPI process related to qualified dietary staff and resident f...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0582
(Tag F0582)
Minor procedural issue · This affected multiple residents
Based on record review and interview, the facility failed to complete and provide a NOMNC (CMS-10123) for 3 (#s 48, 154, 155) of 6 sampled residents. Findings include:
1. Review of resident #48's SNF...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Respiratory Care
(Tag F0695)
Minor procedural issue · This affected multiple residents
Based on observation and interview, the facility failed to change oxygen tubing and supplies for 2 (#s 11 and 27) of 5 sampled residents having oxygen in their rooms, increasing the risk for respirato...
Read full inspector narrative →
Aug 2023
5 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility staff failed to intervene when noticing 1 (#1) of 1 sampled resident vaping i...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility staff failed to revise the care plan for 1 (#1) of 1 sampled resident after a significant medical event, when the resident was found unresponsive, re...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on interview and record review, facility staff failed to evaluate and enforce the smoking policy at the facility, for 1 (#1), of 1 sampled resident. This resulted in the resident needing to be t...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0729
(Tag F0729)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to complete and verify a travel CNA from out of state, had an approved...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0839
(Tag F0839)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure a travel CNA had the required trainings and competency prior to and during her employment contract and assignment at the facility. T...
Read full inspector narrative →
Sept 2022
9 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0805
(Tag F0805)
A resident was harmed · This affected 1 resident
Based on interview and record review, the facility failed to provide a therapeutic diet to 1 (#21) of 2 sampled residents, and had incorrectly ordered food preparation cards for 2 (#s 21 and 24) of 2 ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure the base of the toilet and sink countertop were clean for 1 (#37) of 2 sampled residents. Findings include:
During an ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0635
(Tag F0635)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to obtain admission physician orders to help maintain or improve a Stage I pressure ulcer for 1 (#98) of 3 sampled residents. Findings include...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to complete a Significant Change assessment within 14 days of admission to hospice care for 1 (#41) of 1 sampled resident. This failure had th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to include both a resident receiving hospice care, and the hospice provider in care planning goals, for 1 (#41) of 1 sampled res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a licensed nurse had the competency to complete a gastrostomy tube medication administration, resulting in a resident not receiving ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a resident received the ordered medication for two days, resulting in a significant medication error with the resident having decrea...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to remove expired thickening agents from use and storage. This failure had the potential to cause all residents receiving thicke...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to ensure staff members adhered to proper PPE practices for 1 (#26) of 1...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "What safeguards are in place to prevent abuse and neglect?"
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: Federal abuse finding, 3 life-threatening violation(s), Special Focus Facility, 2 harm violation(s), $82,446 in fines. Review inspection reports carefully.
- • 41 deficiencies on record, including 3 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • $82,446 in fines. Extremely high, among the most fined facilities in Montana. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Ivy At Deer Lodge's CMS Rating?
CMS assigns IVY AT DEER LODGE an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Montana, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Ivy At Deer Lodge Staffed?
CMS rates IVY AT DEER LODGE's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 68%, which is 22 percentage points above the Montana average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs. RN turnover specifically is 73%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Ivy At Deer Lodge?
State health inspectors documented 41 deficiencies at IVY AT DEER LODGE during 2022 to 2024. These included: 3 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 2 that caused actual resident harm, 32 with potential for harm, and 4 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Ivy At Deer Lodge?
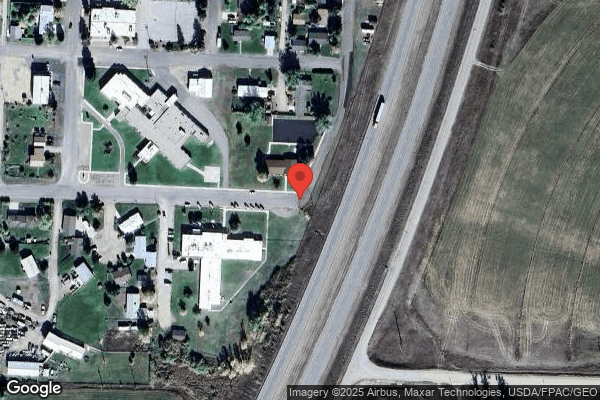
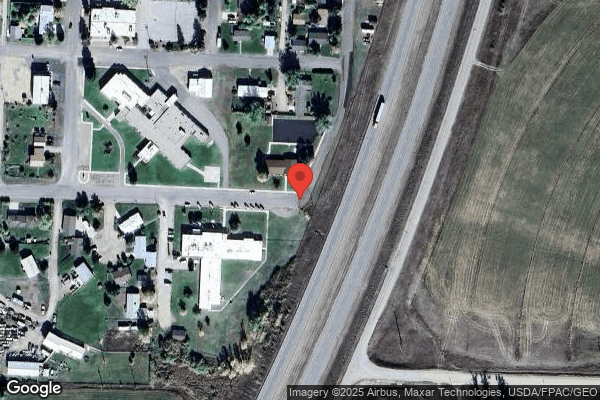
IVY AT DEER LODGE is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by SIMCHA HYMAN & NAFTALI ZANZIPER, a chain that manages multiple nursing homes. With 60 certified beds and approximately 40 residents (about 67% occupancy), it is a smaller facility located in DEER LODGE, Montana.
How Does Ivy At Deer Lodge Compare to Other Montana Nursing Homes?
Compared to the 100 nursing homes in Montana, IVY AT DEER LODGE's overall rating (1 stars) is below the state average of 2.9, staff turnover (68%) is significantly higher than the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Ivy At Deer Lodge?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" These questions are particularly relevant given the facility's Immediate Jeopardy citations, the substantiated abuse finding on record, the facility's high staff turnover rate, and the below-average staffing rating.
Is Ivy At Deer Lodge Safe?
Based on CMS inspection data, IVY AT DEER LODGE has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). Inspectors have issued 3 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility is currently on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes nationwide). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Montana. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Ivy At Deer Lodge Stick Around?
Staff turnover at IVY AT DEER LODGE is high. At 68%, the facility is 22 percentage points above the Montana average of 46%. Registered Nurse turnover is particularly concerning at 73%. RNs handle complex medical decisions and coordinate care — frequent RN changes can directly impact care quality. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Ivy At Deer Lodge Ever Fined?
IVY AT DEER LODGE has been fined $82,446 across 2 penalty actions. This is above the Montana average of $33,903. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Ivy At Deer Lodge on Any Federal Watch List?
IVY AT DEER LODGE is currently an SFF Candidate, meaning CMS has identified it as potentially qualifying for the Special Focus Facility watch list. SFF Candidates have a history of serious deficiencies but haven't yet reached the threshold for full SFF designation. The facility is being monitored more closely — if problems continue, it may be added to the official watch list. Families should ask what the facility is doing to address the issues that led to this status.