EASTERN MONTANA VETERANS HOME




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Eastern Montana Veterans Home in Glendive has received a Trust Grade of F, indicating significant concerns about the facility's quality of care. Ranking #40 out of 59 in Montana places it in the bottom half, and as #2 out of 2 in Dawson County, it is clear that there is only one local option that is better. Unfortunately, the facility's condition is worsening, with issues increasing from 4 in 2024 to 13 in 2025. Staffing ratings are relatively strong at 4 out of 5 stars, but the turnover rate is a concerning 83%, significantly higher than the state average of 55%. However, the facility has incurred $70,497 in fines, which is higher than 76% of Montana facilities and suggests ongoing compliance issues. Additionally, RN coverage is below average compared to 76% of state facilities, which raises concerns about the level of oversight for resident care. Specific incidents reported include a resident being left unattended in distress and suffering from skin abrasions, another resident with dementia eloping from the facility and sustaining injuries, and a report of physical and psychological abuse leading to fear and injury for yet another resident. While there are strengths in staffing ratings, the overall picture presents significant risks that families should carefully consider.
- Trust Score
- F
- In Montana
- #40/59
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 83% turnover. Very high, 35 points above average. Constant new faces learning your loved one's needs.
- Penalties ⚠ Watch
- $70,497 in fines. Higher than 90% of Montana facilities. Major compliance failures.
- Skilled Nurses ✓ Good
- Each resident gets 43 minutes of Registered Nurse (RN) attention daily — more than average for Montana. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 32 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in staffing levels, fire safety.
The Bad
Below Montana average (2.9)
Below average - review inspection findings carefully
36pts above Montana avg (46%)
Frequent staff changes - ask about care continuity
Well above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
35 points above Montana average of 48%
The Ugly 32 deficiencies on record
Jun 2025
4 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
Based on record review, the facility staff assigned to a resident neglected to ensure he received necessary ADL care and was left in bed for an extended period of time without help. The resident exper...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to prevent a resident with dementia from eloping from the facility thr...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure nursing staff were adequately trained and had the knowledge necessary to fulfill the nursing role related to the facility's elopemen...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a system of communicable disease surveillance was maintained...
Read full inspector narrative →
Feb 2025
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure POLST forms were completed accurately in the electronic medi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide a clean, sanitary, and homelike environment for 2 (#s 45 and 109) of 17 sampled residents. Findings include:
During a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to create a baseline care plan with pertinent condition ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to update resident care plans in a timely manner for 1 (#33) of 17 sampled residents. Findings include:
Review of resident #33's...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure an as needed (PRN) psychotropic medication was limited to 14 days, for 1 (#26) of 17 sampled residents. Findings include:
During an ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure resident PASRRs (Pre-admission Screening and Resident Review...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to assess a resident for safety with smoking, failed to monitor the resident's location when smoking and ensure the resident signed out of the...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to have an RN working at least eight consecutive hours a day, per the twenty-four-hour period, seven days per week. This deficient practice ha...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure staff prepared food in a sanitary manner; failed to ensure freezer equipment was maintained and that food items in the...
Read full inspector narrative →
Oct 2024
4 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to protect a resident's right to be free from physical...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to honor dining preferences for 1 (#7) of 13 sampled residents. The deficient practice had the potential to impact the resident'...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to review and update a comprehensive care plan for 1 (#8) of 13 sampled residents. The resident experienced grief and sorrow fro...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0745
(Tag F0745)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide social services for a resident who suffered with grief and loss of a spouse, for 1 (#8) of 13 sampled residents. Find...
Read full inspector narrative →
Oct 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0744
(Tag F0744)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to identify and address a resident acted out in willful abusive manner, when the resident (#2) had dementia, and the resident attacked another...
Read full inspector narrative →
MINOR
(C)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Minor Issue - procedural, no safety impact
Deficiency F0943
(Tag F0943)
Minor procedural issue · This affected most or all residents
Based on interview and record review, it was identified the facility abuse education was not adequate to ensure administrative staff had necessary knowledge related the identification of willful abuse...
Read full inspector narrative →
Feb 2023
10 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0692
(Tag F0692)
A resident was harmed · This affected 1 resident
Based on observation, interview, and record review, the facility failed to maintain an effective system for tracking resident weights, identifying weight loss, and implementing nutritional interventio...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0801
(Tag F0801)
A resident was harmed · This affected 1 resident
Based on interview and record review, the facility failed to ensure the dietitian, and the dietary manager, accurately assessed and communicated the nutritional needs of 1 (#49) of 1 sampled resident....
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a resident's physician was notified of a significant change in condition which included severe weight loss for 1 (#49) of 1 sampled ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure allegations of abuse and misappropriation of resident property were reported to the State Survey Agency within 24 hours of the incid...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
3. During an observation on 2/14/23 at 1:23 p.m., resident #19 was observed being assessed by a hospice nurse from an outside agency.
Review of resident #19's hospice documentation, dated 2/9/23, sho...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to update a care plan to show a resident's severe weight loss and fall prevention interventions, for 1 (#49) of 4 sampled reside...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to obtain a follow-up weight to confirm or refute an inconsistent documented 21 pound weight loss in a 14-day period for 1 (#9) of 1 sampled r...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0740
(Tag F0740)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, facility staff failed to offer and attempt to use interventions identified on individualized care plans, or offer activities available and provided ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to implement and/or enforce appropriate Covid-19 source control for vaccine exempt staff. Findings include:
During an interview ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility's abuse investigations failed to show sufficient actions taken to prevent future reoccurrences of resident to resident abuse events, for residents wh...
Read full inspector narrative →
Nov 2022
3 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on observation, interview, and record review, the facility failed to accurately assess and provide supervision for the safety of 1 (#18) of 4 sampled residents for smoking; failed to implement e...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a resident was free from physical restraints for 1 (#19) of 1 sampled resident. Findings include:
Record review of a facility docume...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility staff failed to report suspicion of abuse for investigation for 2 (#13 and #19) of 2 sampled residents. Findings include:
Record review of a facility...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What safeguards are in place to prevent abuse and neglect?"
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: Federal abuse finding, 6 harm violation(s), $70,497 in fines. Review inspection reports carefully.
- • 32 deficiencies on record, including 6 serious (caused harm) violations. Ask about corrective actions taken.
- • $70,497 in fines. Extremely high, among the most fined facilities in Montana. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Eastern Montana Veterans Home's CMS Rating?
CMS assigns EASTERN MONTANA VETERANS HOME an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Montana, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Eastern Montana Veterans Home Staffed?
CMS rates EASTERN MONTANA VETERANS HOME's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 83%, which is 36 percentage points above the Montana average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs. RN turnover specifically is 73%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Eastern Montana Veterans Home?
State health inspectors documented 32 deficiencies at EASTERN MONTANA VETERANS HOME during 2022 to 2025. These included: 6 that caused actual resident harm, 25 with potential for harm, and 1 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
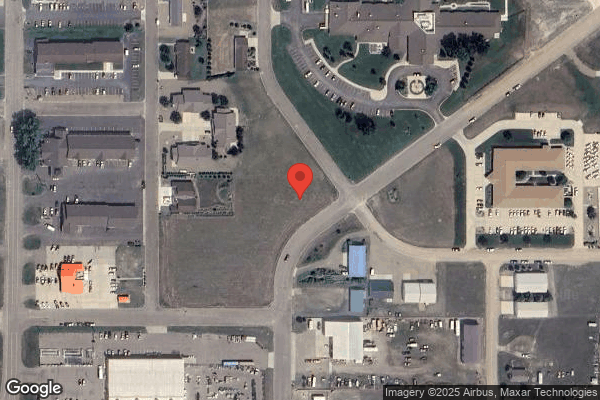
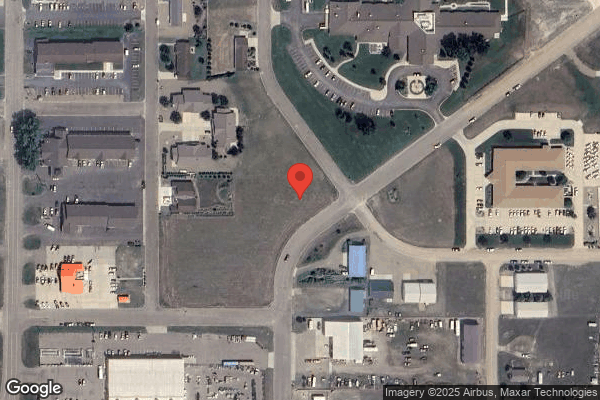
Who Owns and Operates Eastern Montana Veterans Home?
EASTERN MONTANA VETERANS HOME is owned by a government entity. Government-operated facilities are typically run by state, county, or municipal agencies. The facility is operated by EDURO HEALTHCARE, a chain that manages multiple nursing homes. With 80 certified beds and approximately 50 residents (about 62% occupancy), it is a smaller facility located in GLENDIVE, Montana.
How Does Eastern Montana Veterans Home Compare to Other Montana Nursing Homes?
Compared to the 100 nursing homes in Montana, EASTERN MONTANA VETERANS HOME's overall rating (2 stars) is below the state average of 2.9, staff turnover (83%) is significantly higher than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Eastern Montana Veterans Home?
Based on this facility's data, families visiting should ask: "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the substantiated abuse finding on record and the facility's high staff turnover rate.
Is Eastern Montana Veterans Home Safe?
Based on CMS inspection data, EASTERN MONTANA VETERANS HOME has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Montana. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Eastern Montana Veterans Home Stick Around?
Staff turnover at EASTERN MONTANA VETERANS HOME is high. At 83%, the facility is 36 percentage points above the Montana average of 46%. Registered Nurse turnover is particularly concerning at 73%. RNs handle complex medical decisions and coordinate care — frequent RN changes can directly impact care quality. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Eastern Montana Veterans Home Ever Fined?
EASTERN MONTANA VETERANS HOME has been fined $70,497 across 3 penalty actions. This is above the Montana average of $33,784. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Eastern Montana Veterans Home on Any Federal Watch List?
EASTERN MONTANA VETERANS HOME is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.