CLARK FORK VALLEY NURSING HOME




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Clark Fork Valley Nursing Home has a Trust Grade of C+, which means it is slightly above average but not without concerns. It ranks #10 out of 59 facilities in Montana, placing it in the top half, and is the best option among the two nursing homes in Sanders County. However, the facility is experiencing a worsening trend, with issues increasing from just 1 in the previous year to 16 in the current year. Staffing is a notable strength, rated 5 out of 5 stars with a turnover rate of 48%, which is lower than the state average, indicating that staff members tend to stay and become familiar with the residents. On the downside, the facility has faced serious concerns, including failing to appropriately manage a resident who exhibited aggressive behavior towards others, leading to incidents of resident-to-resident abuse. Additionally, staff did not consistently practice proper hand hygiene during medication administration, posing a risk for infection spread. Overall, while there are strengths in staffing and overall ratings, potential residents and their families should be aware of the serious issues highlighted in recent inspections.
- Trust Score
- C+
- In Montana
- #10/59
- Safety Record
- Moderate
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 48% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Montana facilities.
- Skilled Nurses ✓ Good
- Each resident gets 57 minutes of Registered Nurse (RN) attention daily — more than average for Montana. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 22 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Staffing Rating · Excellent nurse staffing levels
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in staffing levels, quality measures, fire safety.
The Bad
Near Montana avg (46%)
Higher turnover may affect care consistency
The Ugly 22 deficiencies on record
Feb 2025
16 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0744
(Tag F0744)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to address the aggressive and intrusive behavior of a resident with de...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure a comprehensive care plan reflected a high risk medication and side effects for 1 (#8), and account for the sleeping p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a care plan was revised to include comfort care for 1 (#22) of 17 sampled residents. This deficient practice increased the risk of t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a program was in place to maintain or restore bladder function for 2 (#s 8 and 18) of 17 sampled residents. This deficient practice ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure weights were accurate and correct in the medical record and failed to ensure a process was in place and followed for r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0699
(Tag F0699)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to identify and address past trauma for a resident; and provide trauma...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0745
(Tag F0745)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide medical social services for 1 (#24) of 17 sampled residents. This deficient practice had the potential to negatively impact the res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure an as needed antianxiety medication was limited to 14 days, or provide a rationale for continued extension of the medication, for 1 ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure residents were free from resident to resident abuse incidents, and failed to provide protection before or following each event to pr...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to report resident to resident abuse allegations to the State Survey Agency within the required reporting period, for 1 (#19) of 17 sampled re...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to recognize abuse and thoroughly investigate the potential for abuse; and failed to take appropriate action to prevent and protect other resi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to complete MDS assessments accurately for restraint use for 3 (#s 8, 16, and 24), and accurately identify an antidepressant med...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to dispose of expired stock medication, and ensure the m...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility staff failed to complete proper hand hygiene during resident medication pass, and use proper PPE when transporting dirty housekeeping e...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0574
(Tag F0574)
Minor procedural issue · This affected most or all residents
Based on observation and interview, the facility failed to post a list of names and contact information for state regulatory and advocacy groups, the State Survey Agency or State licensure office, or ...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0577
(Tag F0577)
Minor procedural issue · This affected most or all residents
Based on observation and interview, the facility failed to post the results of the most recent recertification survey in an area readily accessible to residents, family members, and residents' legal r...
Read full inspector narrative →
Feb 2024
1 deficiency
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to establish and maintain an antibiotic stewardship program with the required elements, including using a standardized assessment tool and cri...
Read full inspector narrative →
Mar 2023
5 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to protect 1 (#77) of 5 sampled residents from physical and verbal abuse by a staff member. Findings include:
Review of a State Survey Agency ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to complete a comprehensive care plan for 2 (#s 10 and 74) of 23 sam...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to prevent 1 (#74) of 12 sampled residents from falling twice and sustaining injury. Findings include:
During an interview on 2/28/23 at 11:06...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0567
(Tag F0567)
Minor procedural issue · This affected most or all residents
Based on interviews and record review, the facility failed to make personal funds available within the same day, on a weekend, to 1 (#15) of 1 sampled resident. This also had the probability of affect...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0568
(Tag F0568)
Minor procedural issue · This affected most or all residents
Based on interview and record review, the facility failed to provide a quarterly financial statement to a resident, for 1 (#15), of 1 sampled resident. This failure had the potential to affect any oth...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most Montana facilities.
- • 22 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
About This Facility
What is Clark Fork Valley's CMS Rating?
CMS assigns CLARK FORK VALLEY NURSING HOME an overall rating of 4 out of 5 stars, which is considered above average nationally. Within Montana, this rating places the facility higher than 99% of the state's 100 nursing homes. This rating reflects solid performance across the metrics CMS uses to evaluate nursing home quality.
How is Clark Fork Valley Staffed?
CMS rates CLARK FORK VALLEY NURSING HOME's staffing level at 5 out of 5 stars, which is much above average compared to other nursing homes. Staff turnover is 48%, compared to the Montana average of 46%.
What Have Inspectors Found at Clark Fork Valley?
State health inspectors documented 22 deficiencies at CLARK FORK VALLEY NURSING HOME during 2023 to 2025. These included: 1 that caused actual resident harm, 17 with potential for harm, and 4 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Clark Fork Valley?
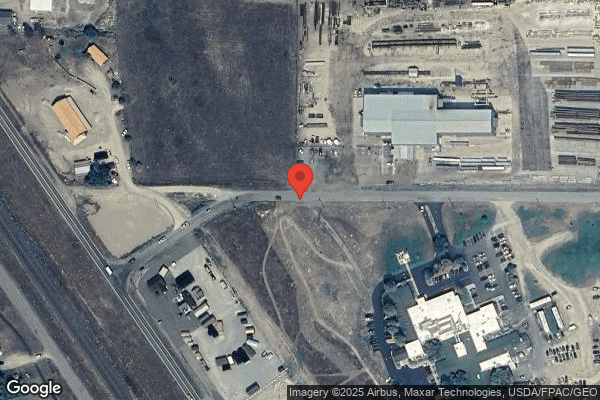
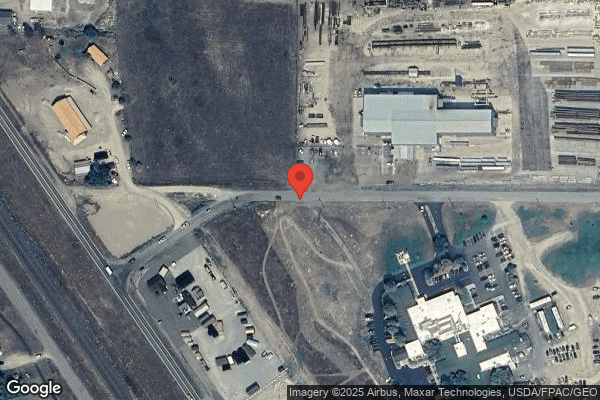
CLARK FORK VALLEY NURSING HOME is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility operates independently rather than as part of a larger chain. With 28 certified beds and approximately 27 residents (about 96% occupancy), it is a smaller facility located in PLAINS, Montana.
How Does Clark Fork Valley Compare to Other Montana Nursing Homes?
Compared to the 100 nursing homes in Montana, CLARK FORK VALLEY NURSING HOME's overall rating (4 stars) is above the state average of 3.0, staff turnover (48%) is near the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Clark Fork Valley?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Clark Fork Valley Safe?
Based on CMS inspection data, CLARK FORK VALLEY NURSING HOME has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 4-star overall rating and ranks #1 of 100 nursing homes in Montana. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Clark Fork Valley Stick Around?
CLARK FORK VALLEY NURSING HOME has a staff turnover rate of 48%, which is about average for Montana nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Clark Fork Valley Ever Fined?
CLARK FORK VALLEY NURSING HOME has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Clark Fork Valley on Any Federal Watch List?
CLARK FORK VALLEY NURSING HOME is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.