La Vida Buena Healthcare
Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
La Vida Buena Healthcare in Las Vegas, New Mexico has received a Trust Grade of F, indicating significant concerns regarding the quality of care provided. It ranks #59 out of 67 facilities in the state and is in the bottom half of options in San Miguel County, with only one local alternative available. While the facility is improving from 25 issues in 2024 to 14 in 2025, the presence of $96,079 in fines is troubling, as it is higher than 83% of other facilities in New Mexico. Staffing is a relative strength with a 3/5 star rating and a low turnover rate of 29%, which is much better than the state average. However, specific incidents raise serious red flags, including a critical finding where a resident's untreated wound led to an amputation and serious delays in care for pressure ulcers that worsened significantly, indicating a need for improved oversight and adherence to care standards.
- Trust Score
- F
- In New Mexico
- #59/67
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ✓ Good
- 29% annual turnover. Excellent stability, 19 points below New Mexico's 48% average. Staff who stay learn residents' needs.
- Penalties ✓ Good
- $96,079 in fines. Lower than most New Mexico facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 37 minutes of Registered Nurse (RN) attention daily — about average for New Mexico. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 72 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Low Staff Turnover (29%) · Staff stability means consistent care
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover is low (29%)
19 points below New Mexico average of 48%
Facility shows strength in quality measures, staff retention, fire safety.
The Bad
Below New Mexico average (2.9)
Significant quality concerns identified by CMS
Well above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 72 deficiencies on record
Jul 2025
11 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview the facility failed to ensure a resident was treated with respect and dignity for 1 (R #5) ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure staff revised the care plan for 1 (R #5) of 3 (R #1, 2 and 5...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to have competent (aware of each resident's current health status and ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to notify the facility providers (Nurse Practitioner, Physician, and t...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to make prompt (done without delay; immediate) efforts to resolve resident's grievances for 4 (R #'s 13, 14, 16, and 17) of 4 (R #'s 13, 14, 1...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to report an investigation regarding allegations abuse and neglect within the required timeframe (2 hours) for 3 (R #'s 13, 14, and 17) of 4 (...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to complete a thorough investigation and report the investigation findings within five working days, for allegations of abuse and neglect for ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to provide quality care that meets professional standard...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to provide a program of activities sufficient to meet each resident's ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure residents received the necessary treatment and services to p...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0728
(Tag F0728)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to utilize Nursing Assistants (NAs) appropriately by using NAs for more than 4 months, on a full-time basis to provide nursing and nursing rel...
Read full inspector narrative →
Apr 2025
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to promote resident choices for 1 (R #3) of 2 (R #'s 2 and 3) resident...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to notify the facility providers (Nurse Practitioner, Physician) when ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure medical records were updated and accurate for 1 (R #1) of 1 ...
Read full inspector narrative →
Oct 2024
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on record review and interview, the facility failed to ensure residents received treatment and care in accordance with professional standards of practice for 1 (R #1) of 3 (R #1, R #2, and R #3)...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to conduct a through investigation and failed to report timely to the State Survey Agency for 1 (R #1) of 3 (R #1, 2, 3) residents reviewed fo...
Read full inspector narrative →
Aug 2024
1 deficiency
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0809
(Tag F0809)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to deliver meals consistently and timely to 84 residents that received room trays or ate in the dining room, as identified on th...
Read full inspector narrative →
Aug 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure 1 (R #1) of 3 (R #1, #2 and #3) residents reviewed for pressure ulcers (a wound caused by prolonged pressure occurring in boney area...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to maintain proper infection prevention measures when the facility experienced an outbreak of coronavirus disease (COVID; a contagious viral dis...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation and interview, the facility failed to store and serve food under sanitary conditions when staff failed to:
1. Properly label and store food items.
2. Maintain the facility kitchen...
Read full inspector narrative →
Jun 2024
19 deficiencies
1 Harm
SERIOUS
(H)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure residents received care consistent with professional standar...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0569
(Tag F0569)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to notify 2 (R #4 and #44) of 2 (R #4 and #44) residents when their balance was within or approached $200.00 of the maximum amount a Medicaid ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to meet professional standards of care related to the us...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to effectively manage pain for 1 (R #386) of 1 (R #386) residents rev...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0740
(Tag F0740)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure 1 (R #29) of 1 (R #29) residents reviewed for behavioral hea...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation and interview the facility failed to:
1. Ensure all medications were stored properly and in the original, labeled packaging.
2. Ensure medical supplies in the medication storage ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to provide food that accommodated resident preferences f...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to provide reasonable accommodations of resident needs and preferences for 1 (R #12) of 1 (R #12) residents. If the facility is not honoring r...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation and interviews the facility failed to provide a homelike environment for all 17 residents that ate their meals in the small dining room when staff failed to remove resident meals ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to complete a Minimum Data Set (MDS; a collection of health data that ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to create an accurate baseline care plan (minimum healthcare informati...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews, the facility failed to develop a comprehensive care plan for 3 (R #58, R ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to provide activities of daily living (ADL; activities r...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Fall Findings:
R #42:
K. Record review of R #42's medical record revealed R#42 was admitted on [DATE] with a diagnosis of unst...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to conduct a monthly Drug Regime Review for 1 (R #1) of 5 (R #1, R #29, R #37,R #45 and R #74) residents reviewed for unnecessary medications....
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to monitor for the use of psychotropic medications (any medication tha...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0802
(Tag F0802)
Could have caused harm · This affected most or all residents
Based on record review, interview, and observation, the facility failed to provide sufficient support staff to carry out the functions of food and nutrition services at the facility. This deficient pr...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0809
(Tag F0809)
Could have caused harm · This affected most or all residents
Based on observation, record review, and interview, the facility failed to deliver meals consistently and timely for all 80 residents in the facility. This deficient practice could potentially lead to...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to ensure food was stored, prepared, distributed, and served to resident...
Read full inspector narrative →
Apr 2023
16 deficiencies
1 IJ (1 affecting multiple)
CRITICAL
(K)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview the facility failed to ensure that 1 (R #1) of 3 (R #1, 26 and 42) residents ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0661
(Tag F0661)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure that a discharge summary was completed and provided to 1 (R ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure that there is an appropriate diagnosis for the use of psycho...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0807
(Tag F0807)
Could have caused harm · This affected 1 resident
Based on interview, observation, and record review, the facility failed to manage hydration for 1 (R #52) of 1 (R #52) resident reviewed for hydration. This deficient practice is likely to result in s...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0810
(Tag F0810)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to provide assistive devices (special eating equipment and utensils) for 1 (R #50) of 1 (R #50) resident reviewed for use of ass...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Findings related to R #40
L. Record review of nursing progress notes dated 03/06/23 at 3:22 pm revealed.Rsd (resident) states pa...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview the facility failed to revise the care plan for 3 (R #40, 46 and 70) of 3 (R #40, 46 and 70...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure that 1 (R #70) of 1 (R #70) resident reviewed for vision, received proper assistive devices to maintain her vision. If the facility ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to
1. Ensure that residents received a safe transfer(without injury) using a hoyer lift (mechanical device designed to lift patients safely) d...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected multiple residents
Based on record review, observation and interview, the facility failed to ensure that residents maintain acceptable parameters of body weight for 1(R #45) of 1(R #45) resident reviewed for weight loss...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected multiple residents
Based on observation, record review and interview the facility failed to ensure that food was prepared in a form to meet the residents needed for 2 (R #5 and #82) of 2 (R #5 and 82) resident observed ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected multiple residents
Based on observation, record review and interview, the facility failed to provide food that accommodates resident allergies intolerance's and preferences for 3 (R #40, 52 and 81) of 3 (R #40, 52 and 8...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0849
(Tag F0849)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to ensure that there was collaboration between the facility and hospice services for 1 (R #46) of 1 (R #46) residents reviewed for hospice ser...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Findings related to doors:
O. On 04/05/23 at 11:13 am during observation and interview, R #7's door was open. Interview with Medication Technician (MT) #2 confirmed that the door should have been clos...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation and interview, the facility failed to store foods under sanitary conditions by not:
1. Ensuring food items in the refrigerator and freezer were properly labeled and dated.
2. Ensu...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0574
(Tag F0574)
Minor procedural issue · This affected most or all residents
Based on observation and interview, the facility failed to ensure that residents receive information on how to contact the state survey agency to file a complaint or seek advocacy. This deficient prac...
Read full inspector narrative →
Mar 2022
17 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0697
(Tag F0697)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observation, and interview, the facility failed to provide the necessary care to effectively manage pain...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to ensure resident had access to call light for 1 (R #59...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to revise the care plan for 1 (R #67) of 1 (R #67) resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to provide ADL (Activities of Daily Living) assistance for baths/showe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to ensure that 1 (R #44) of 1 (R #44) resident received proper assistive devices to maintain his vision. If the facility is not ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure resident specific physician orders and ongoing communication...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0849
(Tag F0849)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure there was collaboration between the facility and hospice ser...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to provide a homelike environment, for 2 (R #'s 63 and 6...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to provide an incident or a follow-up report to the State Survey Agency, for 2 (R #33 and R #67) of 2 (R #33 and #67) residents reviewed for f...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview the facility failed to develop and implement a comprehensive person-centered care plan for ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0711
(Tag F0711)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure residents have a written, signed, and dated progress note fr...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure that PRN (as needed) orders psychotropic medications were li...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation and interview the facility failed to:
1. Ensure that medications in the medication cart were not expired.
2. Ensure that all medications were properly labeled and stored.
These ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to store and serve food under sanitary conditions by not:
1. Ensuring fo...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0841
(Tag F0841)
Could have caused harm · This affected most or all residents
Refer to F0684, F0697, and F0711 for findings pertinent to this citation.
A.
Record review of Medical Director Agreement Page 1 and 2 section 5 (duties) dated 07/20/19 and signed by the Facility Med...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observation and interview the facility failed to maintain proper infection prevention measures for 2 (R #67's and R #64) of 2 (R #67's and R #64) residents identified during random observatio...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected most or all residents
Based on record review, observation, and interview, the facility failed to:
1. Display nurse staffing information in a clear and visible place.
2. Maintain the posted information for a minimum of 18 m...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 29% annual turnover. Excellent stability, 19 points below New Mexico's 48% average. Staff who stay learn residents' needs.
- • Multiple safety concerns identified: 1 life-threatening violation(s), Special Focus Facility, 3 harm violation(s), $96,079 in fines, Payment denial on record. Review inspection reports carefully.
- • 72 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $96,079 in fines. Extremely high, among the most fined facilities in New Mexico. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is La Vida Buena Healthcare's CMS Rating?
CMS assigns La Vida Buena Healthcare an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within New Mexico, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is La Vida Buena Healthcare Staffed?
CMS rates La Vida Buena Healthcare's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 29%, compared to the New Mexico average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at La Vida Buena Healthcare?
State health inspectors documented 72 deficiencies at La Vida Buena Healthcare during 2022 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 3 that caused actual resident harm, 66 with potential for harm, and 2 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates La Vida Buena Healthcare?
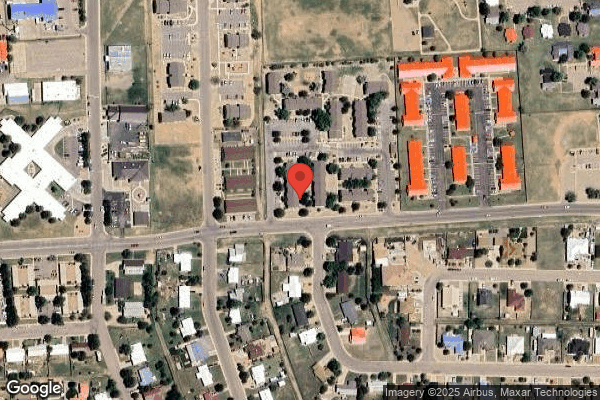
La Vida Buena Healthcare is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by OPCO SKILLED MANAGEMENT, a chain that manages multiple nursing homes. With 102 certified beds and approximately 90 residents (about 88% occupancy), it is a mid-sized facility located in Las Vegas, New Mexico.
How Does La Vida Buena Healthcare Compare to Other New Mexico Nursing Homes?
Compared to the 100 nursing homes in New Mexico, La Vida Buena Healthcare's overall rating (1 stars) is below the state average of 2.9, staff turnover (29%) is significantly lower than the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting La Vida Buena Healthcare?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's Immediate Jeopardy citations.
Is La Vida Buena Healthcare Safe?
Based on CMS inspection data, La Vida Buena Healthcare has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility is currently on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes nationwide). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in New Mexico. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at La Vida Buena Healthcare Stick Around?
Staff at La Vida Buena Healthcare tend to stick around. With a turnover rate of 29%, the facility is 17 percentage points below the New Mexico average of 46%. Low turnover is a positive sign. It means caregivers have time to learn each resident's needs, medications, and personal preferences. Consistent staff also notice subtle changes in a resident's condition more quickly. Registered Nurse turnover is also low at 29%, meaning experienced RNs are available to handle complex medical needs.
Was La Vida Buena Healthcare Ever Fined?
La Vida Buena Healthcare has been fined $96,079 across 8 penalty actions. This is above the New Mexico average of $34,040. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is La Vida Buena Healthcare on Any Federal Watch List?
La Vida Buena Healthcare is currently an SFF Candidate, meaning CMS has identified it as potentially qualifying for the Special Focus Facility watch list. SFF Candidates have a history of serious deficiencies but haven't yet reached the threshold for full SFF designation. The facility is being monitored more closely — if problems continue, it may be added to the official watch list. Families should ask what the facility is doing to address the issues that led to this status.