Sunset Villa Healthcare




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Sunset Villa Healthcare has received a Trust Grade of F, indicating significant concerns about the facility's overall quality and care. With a state rank of #49 out of 67 in New Mexico, they are in the bottom half of facilities, but they are ranked #1 out of 3 in Chaves County, meaning they are the best option locally. The facility is improving, having reduced its number of issues from 31 in 2024 to 14 in 2025. However, staffing is a weakness with a rating of 2 out of 5 stars and a turnover rate of 56%, which is average for the state but still concerning. Additionally, the facility has incurred $79,204 in fines, which is higher than 95% of New Mexico facilities, signaling potential compliance problems. Specific incidents highlight serious concerns, such as a resident who fell and lay on the floor for approximately three hours because staff failed to perform timely rounds. Another resident with high fall risk was not properly monitored after a fall, which goes against the facility's own policies. While the facility does have some strengths, such as a trend toward improvement, these serious incidents and the high fines raise red flags for families considering this nursing home for their loved ones.
- Trust Score
- F
- In New Mexico
- #49/67
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 56% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ⚠ Watch
- $79,204 in fines. Higher than 75% of New Mexico facilities, suggesting repeated compliance issues.
- Skilled Nurses ⚠ Watch
- Each resident gets only 24 minutes of Registered Nurse (RN) attention daily — below average for New Mexico. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 58 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below New Mexico average (2.9)
Below average - review inspection findings carefully
Near New Mexico avg (46%)
Frequent staff changes - ask about care continuity
Well above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
8 points above New Mexico average of 48%
The Ugly 58 deficiencies on record
Sept 2025
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to provide activities of daily living (ADL; activities related to pers...
Read full inspector narrative →
Feb 2025
13 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Past Non-Compliance
Based on record review, and interview, the facility failed to prevent neglect for 1 (R #24) of 1 (R #24) re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and record review, the facility failed to ensure privacy was provided for 1 (R #1) of 1 (R #1) residents re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to provide a comfortable and homelike environment that was in good condition for 1 (R #5) of 1 (R #5) resident reviewed for a homelike environme...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to create an accurate baseline care plan (minimum healthcare informati...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and record review, the facility failed to provide activities of daily living (ADL; activities related to pe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed maintain adequate hydration for 1 (R #24) of 1 (R #24) resident review...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation and interview the facility failed to ensure medications were labeled with a proper open date or expiration date. These deficient practices are likely to negatively impact the heal...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to develop and implement an accurate, person-centered comprehensive ca...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure staff revised the care plan for 2 (R #5 and R #24) of 6 (R #...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to ensure residents who had completed and signed a consent form for influenza (flu, infection of the nose, throat and lungs caused by a virus)...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to offer COVID-19 (an acute respiratory disease in humans characterized mainly by fever and cough and capable of progressing to severe symptom...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observation, record review, and interview, the facility failed to develop and implement an ongoing infection prevention and control program (a program that is used to prevent, recognize, and ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected most or all residents
Based on record review and interview, the facility failed to ensure staff implemented a comprehensive antibiotic stewardship program (a set of commitments and actions designed to optimize the treatmen...
Read full inspector narrative →
Jun 2024
4 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R #6:
P. Record review of R #6's face sheet revealed R #6 was admitted into the facility on [DATE] with the following diagnoses:...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to update and implement a comprehensive person-centered care plan for ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R #3:
E. Record review of R #3's face sheet revealed she was admitted to the facility on [DATE].
F. Record review of R #3's base...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected most or all residents
Based on observation and interview, the facility failed to ensure all medication carts were locked while not in use. This deficient practice had the potential to affect all 19 people residing in rooms...
Read full inspector narrative →
Mar 2024
27 deficiencies
3 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure that 1(R #1) of 4 (R #1-4) residents reviewed received treat...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0697
(Tag F0697)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to effectively manage pain for 1 (R #3) of 2 (R #'s 3 and 57) resident...
Read full inspector narrative →
SERIOUS
(H)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0740
(Tag F0740)
A resident was harmed · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R #51:
GG. Record review of R #51's face sheet revealed R #51 was admitted to facility on 05/06/2023 with the following diagnose...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to allow 1 (R #51) of 1 (R #51) resident to return to the facility aft...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to meet professional standards of care for 1 (R #32) of ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This was cited as past non-compliance
Based on record review and interview, the facility failed to ensure 1 (R #5) of 1 (R #5-9)...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure residents obtained routine dental care for 1 (R #30) of 1 (R...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0810
(Tag F0810)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview, the facility failed to provide assistive devices for 1 (R #28) of 1 (R #28) residents reviewed during dining observation. If residents are not provid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure staff offered COVID-19 (a highly infectious viral disease) v...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to promote residents' choices for 2 (R #'s 5 and 32) of 2 (R #'s 5 and...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to assist or provide an opportunity for residents to organize a facility resident council for all 49 residents as listed on the Resident Censu...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to provide a safe, comfortable, and homelike environment. This deficient...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R #34:
K. Record review of R #34's face sheet revealed R #34 was admitted to the facility on [DATE].
L. Record review of the fa...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to meet professional standards of care for 1 (R #3) of 2...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to provide activities of daily living (ADL) assistance f...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to provide an on-going program of activities designed to meet the interests and well-being for 7 (R #'s 6, 9,16, 29, 30, 32, and...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to ensure a resident's hearing was maintained with funct...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, and interviews, the facility failed to ensure they had sufficient staff to meet the needs ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure the facility monitored for the use of psychotropic medicatio...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure medications and other medical supplies were no...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to maintain confidential records by leaving medical information visible to other residents, visitors, and unauthorized staff for 25 (R #'s 2, 7,...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected multiple residents
Based on record review, observation, and interview, the facility failed to ensure a functioning call light system for 1 (R #28) of 1 (R #28) residents reviewed for call lights. If the facility fails t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0943
(Tag F0943)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to provide training for 2 certified nurse aides (CNAs #6 and #7) of 5 CNAs ( #1, 2, 5, 6, and 7) on the facility's policies and procedures for...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to ensure Certified Nurse Aides (CNAs) received the required in-service training of no less than 12 hours per year for 1 (CNA #5) of 5 (CNA #1...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0680
(Tag F0680)
Could have caused harm · This affected most or all residents
Based on interview, the facility failed to have a qualified therapeutic recreation specialist or an activities professional direct the the activity program in the facility for all the residents who re...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation and interview, the facility failed to ensure food was stored, prepared, distributed, and served to residents in accordance with professional standards of food service safety when ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0949
(Tag F0949)
Could have caused harm · This affected most or all residents
Based on record review and interview, the facility failed to provide behavioral health (the emotions and behaviors that affect your overall well-being) care training for 31 Certified Nursing Assistant...
Read full inspector narrative →
Feb 2023
13 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to provide reasonable accommodations of resident needs and preferences for 1 (R #22) of 1 (R #22) residents reviewed by not having furniture pos...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on record review and interview the facility failed to develop a comprehensive care plan to include eye injections due to diabetic retinopathy (is a diabetes complication that affects eyes. It's ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure the accurate/correct diagnosis was applied for medication being administered for 1 (R #22) of 1 (R #22) residents reviewed for unnec...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
Based on interview and observation the facility failed to maintain equipment to adequately allow residents to call for staff assistance through a communication system which relays the call directly to...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to provide a homelike environment, for all 42 residents ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observation, and interview, the facility failed to ensure that 1 (R #5) of 3 (R #5, R #15, R #91) reside...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
Based on record review and interview the facility failed to ensure that the consultant pharmacist reviewed each resident's drug regime for irregularities on a monthly basis for three ( R # 5, 15, and ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observation, and interview, the facility failed to store and label food by not ensuring food in refriger...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0868
(Tag F0868)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to have the necessary minimum committee members (Medical Director, Administrator, Director of Nursing, Infection Preventionist, and two other ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected most or all residents
Based on record review and interview, the facility failed to provide a summary of a Baseline Care Plan for 6 (R #1, 15, 22, 29, 38, and 140) of 6 (R #1, 15, 22, 29, 38, and 140) residents and/or their...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on record review and interview the facility failed to provide services of a Registered Nurse (RN) for at least 8 consecutive hours a day, 7 days a week. This deficient practice could lead to res...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected most or all residents
Based on record review, observation, and interview the facility failed to:
1) Post the scheduled hours of nursing staff [Registered Nurses, Licensed Practical Nurses and Certified Nursing Assistants] ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure that medications were stored safely, which has...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What safeguards are in place to prevent abuse and neglect?"
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: Federal abuse finding, 5 harm violation(s), $79,204 in fines. Review inspection reports carefully.
- • 58 deficiencies on record, including 5 serious (caused harm) violations. Ask about corrective actions taken.
- • $79,204 in fines. Extremely high, among the most fined facilities in New Mexico. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Sunset Villa Healthcare's CMS Rating?
CMS assigns Sunset Villa Healthcare an overall rating of 2 out of 5 stars, which is considered below average nationally. Within New Mexico, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Sunset Villa Healthcare Staffed?
CMS rates Sunset Villa Healthcare's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 56%, which is 10 percentage points above the New Mexico average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs. RN turnover specifically is 62%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Sunset Villa Healthcare?
State health inspectors documented 58 deficiencies at Sunset Villa Healthcare during 2023 to 2025. These included: 5 that caused actual resident harm and 53 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Sunset Villa Healthcare?
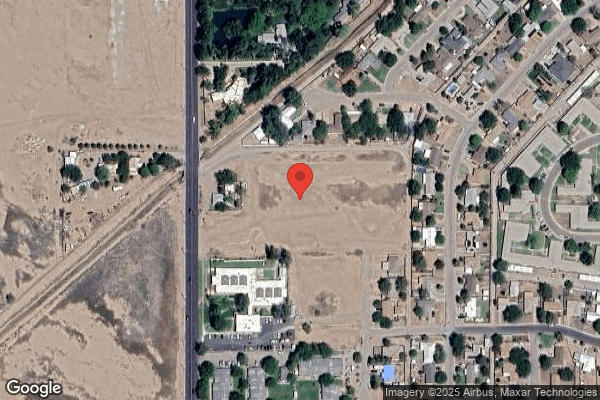
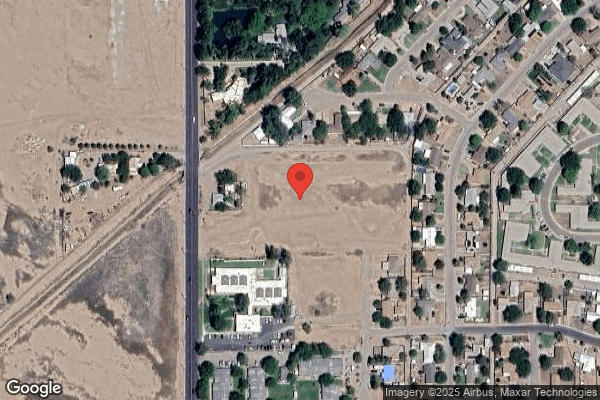
Sunset Villa Healthcare is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by OPCO SKILLED MANAGEMENT, a chain that manages multiple nursing homes. With 52 certified beds and approximately 50 residents (about 96% occupancy), it is a smaller facility located in Roswell, New Mexico.
How Does Sunset Villa Healthcare Compare to Other New Mexico Nursing Homes?
Compared to the 100 nursing homes in New Mexico, Sunset Villa Healthcare's overall rating (2 stars) is below the state average of 2.9, staff turnover (56%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Sunset Villa Healthcare?
Based on this facility's data, families visiting should ask: "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" These questions are particularly relevant given the substantiated abuse finding on record, the facility's high staff turnover rate, and the below-average staffing rating.
Is Sunset Villa Healthcare Safe?
Based on CMS inspection data, Sunset Villa Healthcare has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in New Mexico. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Sunset Villa Healthcare Stick Around?
Staff turnover at Sunset Villa Healthcare is high. At 56%, the facility is 10 percentage points above the New Mexico average of 46%. Registered Nurse turnover is particularly concerning at 62%. RNs handle complex medical decisions and coordinate care — frequent RN changes can directly impact care quality. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Sunset Villa Healthcare Ever Fined?
Sunset Villa Healthcare has been fined $79,204 across 2 penalty actions. This is above the New Mexico average of $33,871. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Sunset Villa Healthcare on Any Federal Watch List?
Sunset Villa Healthcare is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.