CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, and interviews during the recertification, abbreviated (NY00359628), and extended surveys ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, and interviews during the recertification, abbreviated (NY00359628), and extended surveys conducted 3/4/2025 - 3/14/2025, the facility failed to ensure adequate supervision to prevent accidents for one (1) of six (6) residents (Resident #85) reviewed. Specifically, Resident #85 was cognitively impaired, was at risk for elopement, and did not have a care plan in place addressing their elopement risk. Subsequently, Resident #85 eloped from the facility on 11/5/2024 through an unsecured window and was located at a skilled nursing facility approximately 1/4 mile away and across the street from a river. This resulted in the likelihood of serious harm, serious injury, serious impairment, or death that is Immediate Jeopardy and Substandard Quality of Care to Resident #85 and 2 additional residents (Residents #73 and #131) residing on the A and B units identified as risk for elopement.
Findings include:
The facility policy, Elopement Assessment, revised 8/28/2024, documented elopement occurred when a resident successfully left the facility undetected and unsupervised and entered into harm's way. The elopement assessment was completed within 24 hours of admission, readmission, quarterly, with a significant change, and as needed. Based on the results of the elopement assessment, and if the resident was at risk, an individualized plan of care was developed based on the resident's behavior. If the resident was deemed an elopement risk, a wander device was placed on the resident's person or their wheelchair if they were non-ambulatory. Once a resident's wander device was placed, nursing placed an order in the medication administration record for the resident's wander device, and included the location of placement, the expiration date, and the tag number.
Resident #85 had diagnoses including dementia, schizophrenia, and delusional disorder. The 6/23/2024 Minimum Data Set assessment (an assessment tool) documented the resident had severely impaired cognition, was independent with walking and stairs, did not exhibit wandering behaviors, used a wander/elopement alarm daily, and received antipsychotics on a routine basis.
The Comprehensive Care Plan documented:
- on 6/17/2024 the resident had dementia which impaired decision-making abilities, memory/recall, participation in the Brief Interview for Mental Status assessment (an assessment of cognitive function), and participation in activities of daily living. Interventions included the resident would engage in conversation meaningful to them; resident areas were free of hazards; exit seeking behaviors were monitored such as wandering into unsafe areas and entering other resident rooms; and if the resident showed signs of distress, staff attempted to calm the resident.
The 6/17/2024 and 9/11/2024 elopement assessments documented the resident was at risk for elopement and a care plan was initiated. The assessments documented the resident was cognitively impaired and had made statements of wanting to leave the facility.
There was no documented evidence of an individualized care plan addressing the resident's risk for elopement.
Nursing progress notes documented:
- on 11/1/2024 by Licensed Practical Nurse #21 the resident was started on risperidone (an antipsychotic) for increased anxiety.
- on 11/3/2024 by Licensed Practical Nurse #21 the resident kept stating they feared the touchy feely man and that they were not looking for a new spouse.
- on 11/3/2024 by Licensed Practical Nurse #23 on the evening shift the resident was looking to go home.
The 11/4/2024 Nurse Practitioner #45 documented the resident was seen due to increased anxiety and multiple anxious episodes where their anxiety was higher. The resident also had fearfulness of a male resident they did not interact with anymore. The resident required supportive care and reassurance. The resident had long standing dementia that alters their memory, executive functioning, and long-term decision making.
The 11/5/2024 facility investigation completed by Registered Nurse #66 documented:
- at 4:30 PM, the facility received a call from a nearby skilled nursing facility informing them that Resident #85 was in their lobby. The resident was stating their facility was holding them hostage.
- staff statements documented no staff were aware the resident had left the facility. The last time the resident was seen by staff was at 2:30 PM on 11/5/2024 by Licensed Practical Nurse #22 and Certified Nurse Aide #11.
- a staff statement by Licensed Practical Nurse #22 documented around 2:30 PM, they spoke with the resident in their room about the resident's anxiousness regarding their family leaving.
- it was determined the resident left the facility through their unsecured room window. The resident pushed out their screen and crawled through the window.
- the resident was returned to the facility by Registered Nurse Supervisor #12 and a police escort.
- the resident was assessed when they returned to the facility. The resident had small bruises to their left flank, right hip, and lower back, and had a large bruise extending the length of their left posterior (back) calf.
- the resident had a wander alert device placed on 11/5/2024 after they returned to the facility.
The investigator signature was blank. The Administrator signed the investigation on 11/7/2024.
During an observation on 3/4/2025 at 11:25 AM, the windows in the room Resident #85 eloped from had screws in the frame of the window to stop the window from opening more than a few inches. The screen to the narrow window was not fully fitted to the window frame and had visible spacing with some tears in it.
Resident #85 was observed and interviewed:
- on 3/4/2025 at 2:43 PM, in their room and stated they were having a bad day. They stated they did not remember attempting to exit the facility.
- on 3/7/2025 at 3:21 PM, sitting in the stationary chair in their room. They stated it was not a good day and their nerves were shot. Their speech was jumbled, and they stated the facility was going to let them live there and give them food, but they were not on the list anymore. They spoke in circles and was worried about remaining at the facility.
- on 3/11/2025 at 3:56 PM, they stated they wanted to go home.
During an interview on 03/10/2025 at 3:35 PM Certified Nurse Aide #11 stated they checked the resident care record if the resident had behaviors or wandering. The behaviors would be listed on the resident care record and the interventions.
During an interview on 3/7/2025 at 11:14 AM, Registered Nurse Unit Manager #17 stated prior to the resident's elopement on 11/5/2024, there were no limiters (devices to keep the window from opening too far) on the windows on the A and B units and the windows opened all the way. The resident was not on increased monitoring prior to their elopement and was just monitored as needed for their behaviors. There was nothing care planned, or interventions implemented for the resident's increased behaviors because there was no pattern or specific trigger. If the resident was upset, staff gave them more redirection away from the current cause of the upset or attempted to distract them.
During an interview on 3/7/2025 at 11:38 AM, Maintenance Worker #3 stated they only checked the windows when a resident moved out of the room to get it ready for a new resident. They stated a previous maintenance worker put L-shaped brackets in place on half the unit. They ran out of brackets on 11/6/2024, after the elopement, so they put screws in the window frame The maintenance department put L-shaped brackets on the rest of the windows on B unit on 3/5/2025 because the screws that were placed were not in the correct spot and with force, the windows opened all the way.
During an interview on 3/7/2025 at 12:00 PM, Administrative Assistant #4 stated the facility, and surveyors were simultaneously checking windows on the windows on B unit on 3/4/2025. Administrative Assistant #4 stated they found a window that was able to be opened all the way which prompted the maintenance department to check the windows on the unit and the rest of the L-shaped brackets were placed. They informed Registered Nurse Unit Manager #17.
During an interview on 3/10/2025 at 11:03 AM, Cook/Former Facilities Worker #5 stated when Resident #85 eloped in 11/2024 the windows in the resident rooms on the A and B units did not have limiters. They were called back to the facility on [DATE] after the elopement to find a way to secure the resident's window. They put dry wall screws in the resident's window frame to limit the window from opening. The following day on 11/6/2024, they secured the remainder of the windows on the A and B units so they could not open past 4 inches.
During an interview on 3/11/2025 at 11:00 AM, Maintenance Worker #13 stated they put limiters on the windows after the elopement occurred to stop the windows from opening all the way. On 3/4/2025, they were made aware one of the windows opened past where the limiter would have been and when they checked that window there was a screw in place to limit it. They reinforced the window with the L-shaped brackets. The screws were found in the windows of at least half of the B unit windows, so they replaced all the screws with the L-shaped brackets. At the time the windows were limited, they had run out of L-shaped brackets and some of the windows only had screws placed. It was not a priority to replace the screws as they seemed to be working.
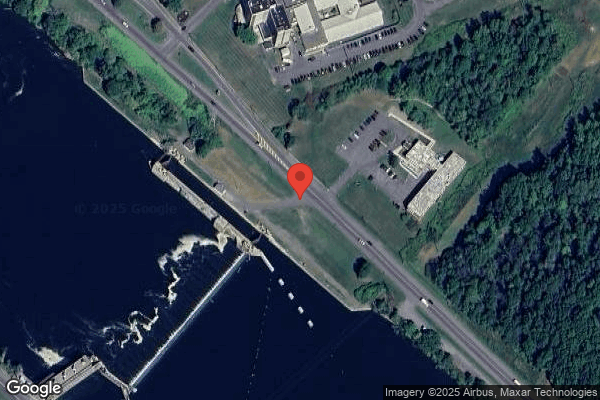
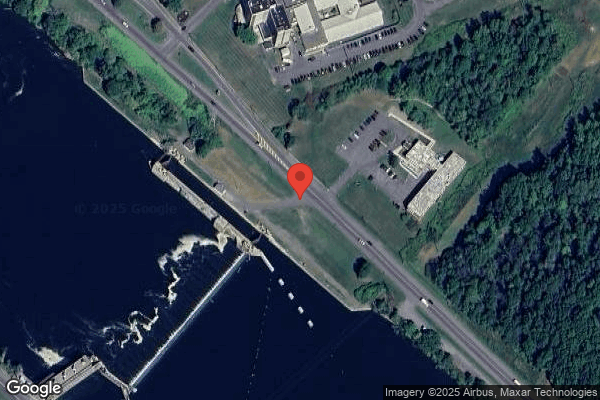
During an interview on 3/11/2025 at 1:12 PM, the Administrator stated the elopement assessment determined if residents were at risk. If a resident was deemed to be an elopement risk, they had a wander device placed, had a care plan initiated, and the Health Information Manager was updated so the resident could be added to the wander device book that listed what residents were wander risks with their picture. Resident #85 was deemed a risk for elopement upon admission on [DATE]. They did not have an elopement care plan until 11/5/2024 after their elopement and should have had one when they were identified as an elopement risk. A resident who eloped from the facility was at risk for harm due to the surrounding area that had a main road, hills, and a river.
During a telephone phone interview on 3/11/2025 at 2:00 PM, the Medical Director stated residents who were elopement risks should be on elopement precautions and have a care plan in place. They stated they knew Resident #85 well as they had followed them as their primary care doctor prior to the facility admission. The resident had paranoid behaviors with strange men and male caregivers. The facility was located on a main road with a river across the street. A resident who eloped from the facility was at risk for accidents and the geographic location could pose safety risks.
10 NYCRR 415.12(h)(1)(2)
___________________________________________________
An Immediate Jeopardy in F-689 was issued to the Administrator and Corporate Administrator on 3/11/2025 at 5:00 PM.
The facility performed the following steps to lift the Immediate Jeopardy in F-689, issued 3/11/2025 at 5:00 PM:
- As of 3/11/2025 at 6:50 PM the facility's immediate plan was reviewed and accepted.
- As of 3/12/2025 at 4:16 PM 100% of all staff currently working have been educated on elopement risk and window securement.
-As of 3/13/2025 at 7:45 AM, 85% of staff had been educated on elopement risk and window securement.
-The remaining staff will be educated prior to the start of their next shift or upon return from their leave.
-Staff education was verified onsite during interviews on 3/13/2025. Multiple staff including nursing, maintenance, housekeeping, and activities were interviewed.
-Staff were able to report content of education, confirmed the day they received the education, and the facility staff who presented the education
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, and interviews during the recertification and abbreviated (NY00330552) surveys conducted 3...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, and interviews during the recertification and abbreviated (NY00330552) surveys conducted 3/4/2025 - 3/14/2025, the facility failed to ensure residents received treatment and care in accordance with professional standards of practice for one (1) of two (2) residents (Resident #136) reviewed.
Specifically, Resident #136:
- physician's order for gastrostomy (a tube placed in the stomach) tube feeding was not administered as ordered and when administered was the incorrect volume;
- had an order to receive nothing by mouth and medications were ordered to be given orally;
- was improperly positioned prior to having a tube feeding administered;
- had an indwelling catheter collection bag in a permeable pillowcase laying on the floor;
- did not receive their weekly shower or hair washing;
- was left in their room with the door closed, their call bell on the floor and out of reach, and the resident was unable to use a traditional call bell and no alternative was given
- did not have preferred activities provided for sensory stimulation;
- was not provided with timely activities of daily living care;
- was visible from the hallway wearing only a brief with their gastrostomy tube insertion site in plain view;
- was observed in bed for consecutive days without being dressed.
This resulted in physical and psychosocial harm to Resident #136 that was not Immediate Jeopardy.
Findings include:
The facility policy Activities of Daily Living, revised 9/2024, documented care and services would be provided for transfers, ambulation, bathing, dressing, and grooming; residents who were unable to carry out activities of daily living would receive the necessary services to maintain good nutrition, grooming, personal and oral hygiene; and a resident's abilities and activities of daily living would not deteriorate unless deterioration was unavoidable.
The facility policy Bathing Techniques-Tub Bath or Shower, revised10/2024, documented all residents were bathed as often as necessary to maintain cleanliness, refresh and stimulate circulation, and residents would be assisted with showering hair and rest of body as needed, moving from head to toe.
The facility policy Fall Prevention, revised 10/2024, documented general safety precaution and fall prevention measures that applied to all residents that included easy access to call light, increased observation and surveillance, and observation during walking or safety rounds.
The facility policy Resident Care Record, last reviewed 2/21/202, documented the Unit Manager initiated the resident care record on all residents by checking which areas applied to the resident; staff were responsible to do all care as indicated by check marks in each category of care; if care was not given as indicated on the resident care record, the certified nurse aide would notify the charge nurse of what care was not given and why; the charge nurse would intervene with the resident and document the outcome; and at the completion of each shift, the certified nurse aide would initial on the back of the resident care record for the appropriate date and shift indicating care was given.
The facility policy, Tube Feeding-Gastrostomy, Percutaneous Gastrostomy (PEG) or Jejunostomy Tube Feeding with Use of Pump, revised 5/2024, documented obtain physician order for type and amount of formula, and frequency of administration. Place resident in semi-Fowler's position (sitting at 45-degree angle) to avoid aspiration (inhaling contents into lungs).
The facility policy Call Bell Accessibility, reviewed 9/2024, documented the facility would be adequately equipped with a call light at each residents' bedside, toilet, and bathing facility to allow residents to call for assistance; each resident would be evaluated for unique needs and preferences to determine any special accommodations that may be needed in order for the resident to utilize the call system; special accommodations would be identified on the resident's person-centered plan of care, and provided accordingly (examples include touch pads, larger buttons, bright colors, etc.); and staff would ensure the call light was within reach of the resident and secured, as needed.
The facility policy, Purpose, Goals, and Methods of Programs, revised 3/24/2024,
documented the facility would identify each resident's interests and needs and involve the resident in an on-going program of activities that were designed to appeal to their interests and to enhance their highest practicable level of physical, mental and psychosocial well-being.
Resident #136 had diagnoses including depression, obstructive uropathy (obstructed urine flow), cerebral infarction (stroke) with left hemiplegia (inability to move the left side of the body), and dysphagia (difficulty swallowing). The 1/30/2025 Minimum Data Set assessment (an assessment tool) documented the resident had intact cognition, had unclear speech, was sometimes able to express ideas and wants, was dependent for most activities of daily living, had an indwelling urinary catheter, was always incontinent of bowel, had a feeding tube, received 51% or more of total calories through a tube feeding, and was at risk for developing pressure ulcers. The 11/7/2024 Annual Minimum Data Set assessment (an assessment tool) documented the resident felt it was very important to choose what clothes to wear, it was somewhat important to choose between a tub bath, shower, bed bath or sponge bath, listen to music they liked, do things with groups of people, do favorite activities, and participate in religious services or practices.
Gastrostomy Tube Feedings and Oral Medications:
The comprehensive care plan, initiated 11/4/2024 and revised 3/1/2025, documented a nutritional and hydration risk related to dysphagia and nothing by mouth status. Interventions included diet and tube feeding as ordered, head of bed to always be at 45 degrees, and nothing by mouth.
The 12/26/2024 speech language pathology discharge summary documented the resident should be in upright position during and after tube feedings to decrease the risk of aspiration.
Physician orders documented the following:
-on 11/1/2024 aspirin 81 milligrams by mouth once a day; fluoxetine (an anti-depressant) 20 milligrams by mouth once a day; and senna (a stool softener) two 8.6 milligram tablets by mouth at bedtime.
-on 12/19/2024 nothing by mouth, bolus tube feeding by gastrostomy tube.
-on 1/22/2025 1.2 calorie high fiber tube feeding formula give 280 milliliters bolus (formula delivered by gravity or syringe) every 4 hours to equal 1680 milliliters and give 50 milliliters water before and after each feeding every 4 hours, give 30 milliliters water before and after medications four times a day
The December 2024, January 2025, February 2025, and March 2025 Medication Administration Records documented:
- aspirin 81 milligrams chewable tablet 1 tablet orally at 6:00 AM.
- fluoxetine 20 milligrams 1 tablet orally at 6:00 AM
- senna 8.6 milligrams 2 tablets orally at 9:00 PM
The medications were signed as administered daily from 12/19/2024 - 3/14/2025.
The March 2025 Medication Administration Record documented
- on 3/7/2025 the 10:00 PM 1.2 calorie high fiber tube feeding formula, and water flush was not administered
- on 3/8/2025 the 2:00 AM and 6:00 AM 1.2 calorie high fiber tube feeding formula, and water flush were not administered.
On 3/6/2025 from 8:20 AM through 2:16 PM a continuous observation of Resident #136 was made. No one entered the resident's room from 10:32 AM to 2:16 PM. Licensed Practical Nurse #36 was not observed administering the resident's tube feeding from 8:46 AM-2:16 PM.
At 11:36 AM Licensed Practical Nurse #36 signed for 10:00 AM tube feeding and water flush. At 12:24 PM the resident's mouth was very dry, and their lips were dry and flaking. At 2:16 PM, Licensed Practical Nurse #36 entered the resident's room. The resident was in bed with the head of the bed at approximately 20 degrees. Licensed Practical Nurse #36 flushed the feeding tube with 50 milliliters of water, mixed medications with 20 milliliters of water and administered via the tube, instilled one 237 milliliter carton of 1.2 calorie high fiber tube feeding formula into the tube using a syringe (physician order was for 280 milliliters), then flushed with 50 milliliters of water. Licensed Practical Nurse #36 stated the angle of the head of the bed was maybe 20 degrees and they boosted the resident up in bed.
On 3/7/2025 from 8:42 AM through 12:55 PM, a continuous observation of Resident #136 was made. No nursing staff entered the resident's room since 8:42 AM. At 11:03 AM Licensed Practical Nurse #36 passed the resident's room and placed the medication cart at the nursing station. At 11:57 AM Licensed Practical Nurse #36 opened the resident's door, peeked in, shut the door and walked away. At 1:35 PM the tube-feeding formula and water were not signed for on the medication administration record. Licensed Practical Nurse #36 was not observed administering the resident's tube feeding from 9:14 AM-1:44 PM. At 1:44 PM Certified Nurse Aide #22 and Licensed Practical Nurse #36 entered the resident's room. Licensed Practical Nurse #36 elevated the resident's head of bed to about 45 degrees, flushed the resident's tube with 50 milliliters of water, mixed medications with 30 milliliters of water, administered medications, poured one 237 milliliters carton of tube-feeding formula 1.2 into the tube using a syringe (physician order was for 280 milliliters), then flushed with 50 milliliters of water. At 1:57 PM both the 10:00 AM and 2:00 PM tube-feeding formula feedings and water flushes were signed as administered by Licensed Practical Nurse #36 on the medication administration record.
During an interview on 3/7/2025 at 3:02 PM, Licensed Practical Nurse #36 stated if something was signed for in the medication administration record then it was given. Any missed treatments or medications should be reported to the physician and documented. Resident #136 could not have anything by mouth and relied on tube-feeding formula and water flushes via their gastrostomy tube to sustain them. The tube-feeding formula and water flushes should be signed for right after they were administered. They stated they did not know who was responsible for the 10:00 AM administration. The Registered Nurse Unit Manager #36 took over for the night nurse at 8:45 AM and then they took over for the Registered Nurse Unit Manager #36. After reviewing the medication administration record, they stated they had signed for the tube-feeding formula and water, but they should have checked not given. The resident did not receive that, and they did not call anyone to get an order to make up for that missed dose. They were not sure who administered the tube-feeding formula and water flushes on 3/6/2025 at 10:00 AM, and thought they did. They signed for it and if they did not give it, it was probably because they had two floors, and it was hard to keep track of everything. After reviewing the medication administration record, they stated they documented it was not administered and the water flush was documented as administered late but they should have clicked not administered. They stated they should have reported it because they did not do anything to make up for that lost feeding. They stated the resident should receive one whole bottle of tube-feeding formula for the feedings and that was how they were shown and how other nurses did it. After reviewing the order, they stated a bottle was 8 ounces or 237 milliliters and the resident was supposed to get 280 milliliters. The resident did not receive the ordered amount. It was important the resident received what was ordered because they depended on the feeding and could become malnourished.
During an interview on 3/12/2025 at 2:02 PM, Licensed Practical Nurse #22 stated Resident #136 had an order for nothing by mouth and relied entirely on their tube feedings for nutrition. It was important they received the feedings as ordered or they could lose weight. If the tube feeding was not administered within an hour of the scheduled time, they should contact the Unit Manager or the provider for directives. When administering medications, the nurse should check to make sure it was administered by the right route (by mouth, by tube) the right route and if there was any confusion they would clarify before administering. After referring to their orders, they stated the resident had some medications that were ordered to be given by mouth. The orders should have been clarified, as it was possible someone might try to give them by mouth, which could result in aspiration. They stated when they administered the resident's tube feeding, they flushed with 60 milliliters of water, then administered one carton of tube-feeding. After looking at the order and the carton they stated that they had been giving the wrong amount and should have had a carton plus another 40 milliliters. Elevating the head of the bed to 45 degrees was important to prevent reflux and aspiration.
During an interview on 3/14/2025 at 9:31 AM, Physician #8 stated they did not recall being informed by nursing that Resident #136 missed any recent tube feedings.
During an interview on 3/14/2025 at 11:05 AM, Registered Nurse Manager #12 stated nurses should check the route in which medications were ordered. If a resident had an order to get nothing by mouth and there were orders for medications to be given by mouth, it needed to be addressed. It was possible someone might give those medications orally and cause the resident to choke. Bolus feedings (tube feeding formula is delivered quickly using a syringe) given at should be given as ordered. If a resident did not receive their feeding within the time scheduled, they expected it be reported to them so they could call the doctor and see if the feeding could still be given, or the next feeding could be bumped out. Nurses should not sign for something they did not give. They administered Resident #136's tube feeding in the past and the resident received one carton of tube-feeding formula 1.2. After referring to the order and the registered dietitian's note they stated the resident should receive more than one carton of tube-feeding formula. The resident was being monitored because they had a couple pound weight loss and Registered Nurse Manager #12 thought that giving the wrong amount may have contributed to that.
During an interview on 3/14/2025 at 11:30 AM, Registered Dietitian #49 stated Resident #136 received enteral (through a tube) feedings. The resident should receive tube-feeding formula 1.2 280 milliliters 6 times a day for a total of 1680 milliliters. They should be made aware if the feeding or the water flushes were not provided as ordered as the resident was a high nutrition risk. If the resident was not receiving their feeding as ordered it could lead to weight loss. They were not aware the resident's feeding was not provided or not administered as ordered.
During an interview on 3/14/2025 at 1:36 PM, the Director of Nursing stated they expected feeding orders were followed, and the physician was notified of any missed feedings. A bolus should not be skipped or signed for if not given. Missed feedings could cause harmful effects such as weight loss, a pressure ulcer and not feeling well. Resident #136's weights were discussed, and they waxed and waned, which made it even more important the resident received the right amount of formula. The resident was to receive nothing by mouth and their medications and tube-feeding formula should not say give orally. They expected contradictory information to be clarified, as it was possible it could have been given by mouth, which could lead to aspiration.
Activities of Daily Living/Dignity/Urinary Catheter/Activities
The undated resident care instructions documented the resident required assistance with positioning and turning; total assistance for dressing, grooming, and bathing; bathing was scheduled for Thursdays during the 6:00 AM to 2:00 PM shift; mechanical lift for transfers; assist of two for bed mobility; use of a reclining chair and tilt back wheelchair; and call bell-does not use.
The Comprehensive Care Plan documented:
- initiated 11/1/2024, the resident was at risk for pain related to increased muscle strengthening and mobility during rehabilitation. Interventions included assist in positioning for comfort.
- initiated 11/18/2024, the resident was at risk for pressure ulcers due to friction and shear. Interventions included two (2) or more to lift resident while in bed, consider postural alignment, weight distribution, and pressure relief when position in chair or wheelchair.
- initiated 11/1/2024, at risk for infection secondary to urinary catheter. Interventions included provide privacy bag for urine collection bag.
- initiated 11/1/2024, at risk for falls. Interventions included increased staff supervision with intensity based on resident need; provide individualized incontinence care based on needs/patterns; and encourage daily activity.
- initiated 11/1/2024, at risk for constipation related to decreased mobility. Interventions included encourage to get out of bed daily with exercise and activities as tolerated. Restlessness and confusion due to stroke. Interventions included provide and encourage participation in meaningful activities while awake, provide regular periods of exercise and attempt to reduce daytime napping.
The Comprehensive Care Plan did not include activities of daily living requirements.
The following observations of Resident #136 were made:
- on 3/4/2025 at 10:43 AM, lying in bed with only a brief on, their hair was greasy and flaky, and their gastrostomy tube, including the insertion site, was visible from the hall.
- on 3/5/2025 at 12:05 PM, the door to the resident's room was closed. The resident was lying in bed wearing only a brief, their hair was unkempt with flakes, their gastrostomy tube was exposed, and their catheter bag was in a permeable pillowcase resting directly on the floor. The resident was awake and making grunting, indiscernible noises.
- on 3/5/2025 at 2:00 PM, lying on their back in bed, their catheter bag was in a permeable pillowcase resting directly on the floor
The 3/6/2025 Master Assignment Sheet documented Licensed Practical Nurse #36 and Certified Nurse Aide #44 were assigned to the resident, and the resident was scheduled for a shower that day
Resident #136 was observed continuously on 3/6/2025 from 8:20 AM - 2:16 PM:
- at 8:20 AM, the resident was lying flat on their back in bed with flaky, unkempt hair.
- at 8:37 AM, Certified Nurse Aide #44 briefly entered the resident's room then left, shutting the door behind them. The resident was lying on their back wearing only a brief; their catheter bag was in a permeable pillowcase resting directly on the floor.
- at 10:32 AM, Certified Nurse Aide #44 and Licensed Practical Nurse #36 entered the resident's room. The resident had a large amount of dried stool on their buttocks; their skin was red and superficially peeling where the stool was. Certified Nurse Aide #44 cleansed the buttocks and applied skin protectant to the resident's buttocks while Licensed Practical Nurse #36 held the resident on their side. The resident was placed on their back, both staff exited the room and shut the door behind them. There was no television or music provided for stimulation.
- no additional care or activities were observed from 10:32 AM - 2:16 PM. There was no documented evidence the resident received their weekly shower during the 6:00 AM- 2:00 PM shift as scheduled.
During an interview and observation on 3/7/2025 at 8:42 AM, Resident #136 stated yes when asked if they wanted to get out of bed and dressed; yes when asked if they got bored being in their room all the time; and no when asked if anyone from activities came to see them. They also stated they preferred wearing a light shirt and shorts. The resident's dresser and closet had many articles of clean clothing.
Resident #136 was observed continuously on 3/7/2025 from 8:42 AM - 12:55 PM:
- at 8:42 AM, the door to the resident's room was closed, the resident was lying flat on their back, not dressed, their hair was unkempt with flakes, their catheter bag was in a permeable pillowcase resting directly on the floor
- from 11:32 AM - 1:35 PM, the resident's door was cracked open, the resident was lying on their back in bed, and their catheter bag was in a permeable pillowcase resting directly on the floor.
No one entered the resident's room to perform care from 8:42 AM - 1:44 PM.
- at 1:44 PM, Licensed Practical Nurse #36 and Certified Nurse Aide #44 entered the resident's room and boosted the resident up in bed. No other care or repositioning was provided.
During an interview on 3/7/2025 at 2:02 PM, Certified Nurse Aide #44 stated residents should be turned and repositioned every two hours; showers were listed on the assignment sheets and included hair washing; and if the resident care record did not say what kind of bathing to give, they gave a shower. If giving a bed bath, the resident's hair should be washed with the use of a basin and a cup. Resident #136 was dependent for showers and repositioning and should be repositioned every couple of hours if they could get to it. The resident was at risk for skin breakdown and infection. The resident used to get up to a chair, but now laid in bed all day every day and they were unsure why. The resident was scheduled for a shower that day but was given a partial bed bath and they did not wash the resident's hair because they were very busy. They did not report the shower was not given. They did not reposition the resident but did peek in at them to make sure they were safe. They did not dress the resident as they were told the resident did not like to get dressed but recalled the resident used to get up, got dressed, and liked to wear a tee shirt.
During an interview on 3/12/2025 at 12:52 PM Certified Nurse Aide #33 stated catheter bags should be in a privacy bag and not on the floor. If it was on the floor, bacteria could contaminate the tubing and enter the resident, causing an infection. Every resident should be dressed in some capacity each day as it was a privacy and dignity issue, especially if parts of their body were exposed. Doors should be shut only if a resident preferred. Residents at risk for falling should not have their door shut, as they could be unknowingly on the floor or up and walking around. A shut door could also make the resident feel trapped.
During an interview on 3/7/2025 at 3:02 PM, Licensed Practical Nurse #36 stated turning and repositioning should be done every 2 hours, and weekly showers should be provided. If a certified nurse aide could not complete a shower, they expected it to be reported at that time and not at the end of the shift. Showers and repositioning were important because it was a resident's right. Lack of showers could make them feel undignified, and lack of repositioning could lead to bed sores. Resident #136 was dependent for repositioning, showers, and dressing. The resident did not get dressed but they had never asked why. They stated Certified Nurse Aide #44 told them at 2:00 PM on 3/6/2025 that the resident did not get their shower. They noticed the resident's hair was flaky.
During an interview on 3/12/2025 at 2:02 PM, Licensed Practical Nurse #22 stated catheter collection bags should be hung from a chair or bed, not lying on the floor. Catheter bags on the floor was an infection control issue. Doors could be shut if a resident preferred, but if a resident was a fall risk it should be open to better monitor. If a resident was unable to speak, unable to use their call bell, and was a fall risk, their door should not be shut. All residents should be up and dressed each day. Getting out of bed was important for skin integrity, for stimulation provided by activities, and to experience a change of environment. Resident #136 did not really speak; remained in bed the last few times they had worked that unit; their door was shut quite a bit; they were never dressed; and they liked to crawl out of bed. They were not aware of any reason the resident could not get up, get dressed, or have their door open. They thought their door should be open because they tried to crawl out of bed.
During an interview on 3/14/2025 at 11:05 AM, Registered Nurse Unit Manager #12 stated they expected residents to be up and dressed in regular clothing unless they refused. Showers should be done and include shampooing on the assigned days. Turning and repositioning should occur every two hours; catheter bags should not be on the floor; and it was unsafe to have doors shut. If a resident missed their shower, they tried to fit them in on another day and/or time, otherwise that resident would go another week without that shower. It was important residents got out of bed to prevent respiratory and skin issues. Catheter bags should not be on the floor as the floors were dirty and could result in an infection. The resident should be turned and repositioned every two (2) hours to prevent skin breakdown.
During an interview on 3/14/2025 at 12:52 PM, the Infection Control Nurse stated catheter bags should be hung on the bed, the chair, or the walker, and not on the floor. That was an infection control issue because the floors were dirty and exposed the outlet tube to whatever germ was on the floor.
During an interview on 3/14/2025 at 1:04 PM, the Director of Nurses stated they wanted residents up and about and dressed each day. They expected residents were turned and repositioned every 2 - 4 hours; weekly showers be given; and catheter bags in an impermeable dignity bag and hung from the bed or the chair and not lying on the floor.
Call Bell:
The following observations of Resident #136's call bell were made:
- on 3/4/2025 at 10:43 AM and 12:36 PM on the nightstand out of reach.
- on 3/6/2025 at 8:37 AM tucked under the pillow their head was resting on, out of reach.
- on 3/7/2025 at 8:42 AM and 1:35 PM on the floor out of reach.
During an interview on 3/7/2025 at 2:02 PM, Certified Nurse Aide #44 stated all residents should always have their call bell in reach even if they were unable to use it. The facility had hand bells and tap bells for those who could not use push button bells. They stated Resident #136 had a push button call bell, but they did not think the resident could use it.
During an interview on 3/12/2025 at 2:02 PM, Licensed Practical Nurse #22 stated the facility had circular touch bells for those who could not use a regular push button bell. They had never seen Resident #136 use their push button call bell and had never seen an alternative bell tried.
During an interview on 3/14/2025 at 11:05 AM, Registered Nurse Manager #36 stated everyone should have a call bell. If a resident could not use the regular push button call bell they should be evaluated for an alternative. The facility had flat touch bells and hand bells as alternatives to the push button. Having a call bell was important so that a resident could get the staff's attention, otherwise they could fall.
During an interview on 3/14/2025 at 1:36 PM, the Director of Nursing stated if a resident was unable to use a regular call bell, they should have an alternative like a tap or hand bell. If they did have a call bell, it should not be on the floor. It was important residents had a call bell so they could let staff know if they needed assistance. They thought call bell use assessments were completed, but after referencing the electronic medical record they could not see that one was performed for Resident #136.
Activities/Psychosocial Stimulation:
The Comprehensive Care Plan documented:
- initiated 11/1/2024, the resident needed assistance and reminders to participate in activities. The resident enjoyed playing the drums, watching sports and game shows on TV, going outside, gardening, and talking with others. Interventions were to include the resident in one to one activities on unit; provide activities calendar; provide materials as needed for independent leisure pursuits, i.e., books, magazines, newspaper and puzzles. Remind of programs and encourage involvement;
- initiated 11/1/2024, was at risk for miscommunication related to dysphasia (difficulty speaking). Interventions included attempt to anticipate needs; use simple phrases and words; and the resident was able to nod yes or no.
- revised 1/30/2025, the resident enjoyed game shows, Catholic services, drums, sports, outside, gardening, and talking with others. Interventions included invite to mass, be sure they had a picture board, provide materials for independent pursuits, include in one-to-one activities such as games, exercise and trivia; transport to events; and use pictures to communicate.
The March 2025 activities calendar listed the following categories of activities that were documented as being important to the resident:
-on 3/4/2025 visits with Pastor [NAME]
-on 3/5/2025 mass and distribution of ashes and rosary
-on 3/6/2025 bingo
-on 3/7/2025 bible study and theater production of Cinderella
-on 3/10/2025 communion and musical melodies
-on 3/11/2025 visits with Pastor [NAME]
-on 3/12/2025 mass and rosary
-on 3/13/2025 bingo
-on 3/14/2025 bible study, [NAME] orchestra and moving from the music
The undated activities attendance report documented the resident attended the following activities from 3/1/2025-3/14/2025:
- on 3/3/2025 1:1 sensory visit, calendar delivery, traveling performer, and trivia.
- on 3/5/2025 television
- on 3/7/2025 1:1 visit to reminisce
- on 3/10/2025 traveling performer
- on 3/11/2025 a family visit
The 1/31/2025 Social Worker #42's progress note documented the resident sometimes felt lonely and isolated.
The following observations were made of Resident #136 in their room:
- on 3/4/2025 at 10:43 AM and 12:36 PM: staring at the ceiling with no television or music playing.
- on 3/5/2025 at 12:05 PM: in their room in bed with the door closed. At 2:00 PM, awake and lying in bed makes grunting and indiscernible noises with no television or music playing.
- on 3/6/2025 at 8:37 AM: Certified Nurse Aide #44 entered the resident's room, left the room a moment later shutting the door behind them. The television was off, and no music was playing. At 10:32 AM, Certified Nurse Aide #44 entered the resident's room to empty the catheter bag and shut the door when leaving. The resident was lying in bed with no television or music provided.
- on 3/7/2025 at 8:42 AM: in their room with the door closed. At 9:15 AM, an unidentified activities staff stopped in the resident's room, told them the date and the weather, turned on the television, talked about current events, and exited the room two minutes later at 9:17 AM, shutting the door behind them. At 11:12 AM, they were in bed with the door closed.
- on 3/7/2025 at 1:35 PM: lying in bed looking at the wall and ceiling. The television was off, and the door was closed.
- on 3/12/2025 at 12:49 PM: in bed with their legs partially over the side of the bed, the television was off, and the door was closed.
During an interview on 3/7/2025 at 8:42 AM, Resident #136 stated yes when asked if they wanted to get out of bed and dressed; yes when asked if they got bored being in their room all the time; and no when asked if anyone from activities had come to see them.
During an interview on 3/7/2025 at 2:02 PM, Certified Nurse Aide # 44 stated they had not seen activities staff spend much time with Resident #136. Their door should not be shut, as it could make the resident feel isolated which could make them depressed.
During an interview on 3/12/2025 at 12:49 PM, Resident #136 stated no wh[TRUNCATED]
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
Based on record review, observations, and interviews during the recertification and abbreviated (NY00332457) surveys conducted 3/4/2025 - 3/14/2025, the facility failed to ensure a resident with press...
Read full inspector narrative →
Based on record review, observations, and interviews during the recertification and abbreviated (NY00332457) surveys conducted 3/4/2025 - 3/14/2025, the facility failed to ensure a resident with pressure ulcers received the necessary treatment and services, consistent with professional standards of practice, to promote wound healing, prevent infection and prevent new ulcers from developing for three (3) of four (4) residents (Residents #60, #67, and #113) reviewed. Specifically, Resident #60 developed a stage 4 (full-thickness skin loss with exposed bone, tendon or muscle) pressure ulcer to their right hip. Care plan interventions were not consistently followed to prevent pressure ulcers from developing and when the pressure ulcer developed it was not adequately treated to prevent infection. Resident #67 developed a stage 4 pressure ulcer to their left heel while in the facility and there was no evidence the pressure ulcer was treated for 11 days after it was discovered. When the pressure ulcer was assessed by the wound physician consultant there was no evidence the facility evaluated and implemented their recommendations to promote healing. Additionally, on multiple days during survey the resident was observed not wearing their pressure relief booties as planned. Resident #113 had a stage 3 (full-thickness skin loss extending into fatty tissue) pressure ulcer to their right heel and was observed without a dressing on their wound. This resulted in actual harm to Residents #60 and #67 that was not immediate jeopardy.
Findings include:
The facility policy, Standards of Care - Pressure Injury (Ulcers), dated 12/11/2014, documented the registered nurse should regularly inspect skin for changes, such as redness and discoloration and palpate the skin for changes in temperature (warmth), edema (swelling), or hardness. The assessment documentation should be done on admission, quarterly and with a significant change in resident condition. Pressure prevention recommendations included assess skin regularly, protect high-risk areas such as elbows, heels, sacrum, and back of head from friction injury, and reposition schedules individualized based on the resident's condition.
The facility policy, Consults, last reviewed 11/2024, did not document how consultant recommendations were followed up and ordered.
The facility policy, Wound and Skin Care, revised 2020, documented the treatment plan would be tailored to meet individual needs. For any applicable treatment, a physician's order would be written. The policy did not address outside wound care consultants.
1) Resident #60 had diagnosis including dysphagia (difficulty swallowing), and stroke with left sided weakness and paralysis. The 2/2/2025 Minimum Data Set (an assessment tool) assessment documented the resident had severely impaired cognition, did not reject care, and was dependent on staff for all activities of daily living including toileting and bed mobility. The resident was frequently incontinent of bowel and bladder. The resident had a stage 3 and stage 4 pressure ulcer. Pressure ulcer care included a pressure reducing device for their bed, nutritional and hydration support, nonsurgical dressings, and applications of ointments/medications.
The 8/10/2022 Comprehensive Care Plan documented the resident was at risk for skin breakdown related to urinary incontinence and left-sided weakness and paralysis. Interventions included to instruct the resident to reposition self every two (2) to four (4) hours when in bed, keep linens and skin clean and dry, and report any signs of skin breakdown. On 3/4/2025, the care plan was reviewed and updated to include resident's skin to remain intact. No new interventions related to skin break down were documented.
The undated Resident Care Record (certified nurse aide care instructions) documented the resident was at risk for skin breakdown and required assistance with turning every two (2) hours. Use one (1) - two (2) person assist for bed mobility and two (2) person assist for transfers.
The activity of daily living care documentation revealed there was no documented evidence the resident was turned and repositioned on all shifts for 12/15/2024, 12/26/24, and 12/27/24, during the night shift on 12/28/2024, and on both day and night shifts on 12/29/2024.
The handwritten 24-hour report on 1/3/2025 by Licensed Practical Nurse #32 documented the Unit Manager and Assistant Director of Nursing saw the resident for an area on right buttock. There were no progress notes, assessments, or treatment orders associated with the area on the right buttock.
On 1/6/2025 at 3:12 PM, Nurse Practitioner #45 documented the resident was seen for increased pain. The resident had a wound on their right hip measuring 4.4 x 2.6 centimeters. There was no further description of the wound documented or a treatment plan.
On 1/7/2025 Physician Wound Consultant #30 documented the resident was seen for a seven (7) day old pressure ulcer on the right hip. The pressure ulcer measured 3.5 x 2.5 x 0.2 centimeters, and the wound bed contained 100% of necrotic (dead) tissue. The wound was debrided (removal of dead tissue). The treatment plan was to apply alginate honey (wound dressing containing honey and calcium alginate) to the pressure ulcer, cover with gauze and island border dressing daily, off-load the wound, reposition, and use an alternating pressure mattress.
On 1/8/2025 at 2:34 PM, the Assistant Director of Nursing documented the resident was seen on 1/7/2025 for weekly wound rounds. The resident had an unstageable wound on the right hip. The wound physician recommendations were to apply alginate honey , off load the wound, reposition the resident as able and add an alternate pressure mattress.
There was no documented evidence the wound physician's recommendations were discussed or ordered by a provider. There was no documented evidence of any treatment being done to the resident's pressure ulcer.
The 24-hour report on 01/12/2025 documented the wound was foul smelling with a large amount of drainage, and pain medication was given.
On 1/13/2025 at 4:20 PM, Nurse Practitioner #45 documented the resident was seen for a wound to the buttocks. It was extremely foul smelling with drainage and the Wound Physician Consultant was following the resident. The resident complained of pain regardless of positioning. The resident's right hip wound measured 4.4 x 2.6 centimeters. The Nurse Practitioner did not document any further description of the wound or what the treatment plan was, other than the resident was being followed by the Wound Physician.
On 1/14/2025 Physician Wound Consultant #30 documented the right hip pressure ulcer measured 3 x 3 x 0.2 centimeters, and the wound bed contained 100% necrotic tissue. The physician recommended to cleanse the pressure ulcer with wound cleanser at time of dressing change; off-load and reposition and utilize an alternate pressure mattress. This plan was discussed with nursing staff.
There was no documented evidence the wound physician's recommendations were discussed or ordered by a facility provider. There was no documented evidence of any treatment being done to the resident's pressure ulcer.
On 1/21/2025 Physician Wound Consultant #30 documented the wound to the resident's right hip was a stage 4 pressure ulcer. The wound measured 3 x 2.5 x 0.7 centimeters, and the wound bed contained 60% thick adherent devitalized necrotic tissue with 40% slough. The physician surgically excised 3.75 centimeters of devitalized tissue that extended into the muscle. The plan of care was discussed with nursing staff.
There was no documented evidence the wound physician's recommendations were discussed or ordered by a facility provider. There was no documented evidence of any treatment being done to the resident's pressure ulcer.
On 1/22/2025 at 11:48 AM, Registered Nurse Unit Manager #31 documented they received a call from the resident's family, who were with the resident at a doctor's appointment. The family asked Registered Nurse Unit Manager #31 questions related to the wound on the resident's right hip. They told the family the resident was seen on 1/7/2025 and wound care was done by the wound physician. At 3:45 PM, the resident's family called back to report the resident was being admitted to the hospital for further work-up and possible infection. The progress note did not document what the further work-up or infection was in relation to.
The 1/22/2025-1/27/2025 hospital records documented Resident #60 was admitted to the hospital. The resident was found to have a necrotic (dead tissue) pressure ulcer on the right hip, with exposed bone and foul-smelling drainage. Wound cultures were positive for infectious bacteria requiring treatment with intravenous antibiotics. The hospital social worker documented a discussion with the family regarding their concerns for resident neglect at the nursing facility.
During observations on 3/6/2025 at 9:16 AM and 12:45 PM Resident #60 was observed lying in bed on their back.
During interviews on 3/6/2025 at 9:20 AM and 03/07/2025 at 10:38 AM, Certified Nurse Aide #52 stated the resident would only get up for a short time and then was put back to bed. The resident was always incontinent, and they should have been repositioned frequently. They tried to reposition the resident every two hours, but the resident did not stay in the position off their wound. The resident was paralyzed on the left side and would lean to their right side. The resident had contractures (shortening of muscle/tendon), so it was difficulty to reposition them. They were not sure how long the resident had a wound, but stated they went to an appointment and was admitted to the hospital because of the wound.
During an observation and interview on 3/7/2025 at 1:43 PM, with Licensed Practical Nurse #32 and Resident #60, the Licensed Practical Nurse gathered the supplies for the resident's wound care to the right hip. They stated the wound was on the right hip and was a stage 4 pressure ulcer. The resident was laying on their right side. The current treatment was enzymatic debriding ointment and dry dressing. Once the resident was positioned on their left side to change the dressing, there was no old dressing in place to remove. The pressure ulcer on the right hip was round surrounded by pink intact skin. The Licensed Practical Nurse packed the gauze in the undermining and tunnelling of the wound. They stated the resident sometimes pulled the dressing off and would put their fingers and hands on the wound. They thought the pressure ulcer on the hip started sometime in January 2025, when they reported the area to Registered Nurse Unit Manager #31. They did not always have time to follow up with the registered nurse because they were busy with two floors, they would document on the 24-hour report for the staff to review. Licensed Practical Nurse #32 reviewed the electronic medical record and stated there was no treatment order for the pressure ulcer until 1/27/2025, when the resident returned from the hospital.
During an interview on 3/11/2025 at 3:39 PM, Registered Nurse Unit Manager #31 stated the resident was high risk for skin breakdown. The skin assessment should have been completed every three (3) months and whenever they returned from hospital admission. They stated they thought the resident had a stage 2 pressure ulcer to the right hip in the beginning of January. When asked if there was a treatment for the stage 2 pressure ulcer on the right hip, they referred to the resident record. They reviewed the electronic record for notes and specifics. They stated there was nothing, no treatment, no nursing note, and they were responsible to document when there was a new wound area and an assessment of the area. The resident currently had a healing stage 4 pressure ulcer. They stated a stage 4 wound was preventable, but they did not have a turning and positioning schedule documented. They really do not know when the resident was repositioned, or if they refused. They had all the nutrition interventions in place, it was just turning and positioning and getting them out of bed that was missing. The resident was care planned for potential skin break down related to their hemiplegia.
During a telephone interview on 3/12/2025 at 2:16 PM, Licensed Practical Nurse #6 stated the resident had a pressure ulcer to the right hip and had been there for a couple of months. Prevention for pressure ulcers was important for this resident because they were contracted, and unable to reposition themselves. They were supposed to reposition and change the resident every two (2) hours and repositioning and protein were important interventions to prevent wounds.
During an interview on 3/13/2025 at 12:56 PM, the Assistant Director of Nursing stated they completed wound rounds on Tuesday with the wound consultant. The registered nurse Unit Manager should be seeing their residents weekly for their skin assessment and making notes about change in condition of their skin. Resident #60 was at risk for skin break down and pressure ulcer because they were thin and not eating well. The resident currently had a facility acquired Stage 4 pressure ulcer which was originally unstageable on 1/7/2025. They were informed about the wound on 1/3/2025 and at that time the wound was on the right hip and was 4.4 x 2.6 centimeters and the resident was not seen until 1/7/2025 by the wound doctor. They stated prior to 1/7/2025 there were no recommendations or interventions in place to prevent pressure ulcers. The Assistant Director of Nursing stated, the wound had grown large fast and felt the hospital was dramatic with their documentation and reaction. The licensed practical nurses were responsible for completing the dressing changes. The Assistant Director of Nursing reviewed the record and stated they did not see a treatment order for the pressure ulcer prior to the hospitalization, and staff had not been repositioning the resident.
During a telephone interview on 3/13/2025 at 1:54 PM, Physician Wound Consultant #30 stated the resident had a Stage 4 pressure ulcer on the right hip. The resident was at risk for pressure ulcers because they were contracted, and thin. Prior to the wound the resident was on every two (2) hours reposition and using a standard mattress. After their evaluation they added the alternating pressure mattress. The resident was at risk for pressure due to contractures, challenges with nutrition and the need to be assisted with turning and position. They stated an unstageable pressure ulcer could have developed very quickly. They were unaware the facility was not implementing their wound care treatments as recommended.
During a telephone interview on 3/14/2025 at 10:20 AM, Registered Dietitian #49 stated they were made aware of skin issues on the 24-hour report and during weekly wound reports from the doctor. They stated they were seeing the resident in October 2024 because they had impaired skin to the left buttock and the resident was at risk for skin breakdown. The resident was receiving additional nutritional supplement and then with the right hip wound they added the prescribed protein supplement with the medication administration. It was important to supplement the protein for the wound healing.
2) Resident #67 was admitted with diagnoses including stage 4 pressure ulcer to their left heel, osteoarthritis, and physical debility. The 12/22/2024 Minimum Data Set assessment documented the resident had severely impaired cognition; did not reject care; had impairments to both sides of their lower extremities; required maximum assist with dressing and personal hygiene; was at risk for developing pressure ulcers, had one or more unhealed pressure ulcers/injuries, and had a stage 4 pressure ulcer.
The 8/20/2024 physician orders documented to apply skin prep (protective barrier) to the right heel 3 times daily.
The revised 11/21/2024 Comprehensive Care Plan documented the resident exhibited signs and symptoms of a pressure ulcer on the left heel. Interventions included to apply treatment per provider order. No further interventions regarding the left heel were documented.
On 2/8/2025 at 11:06 AM, the Assistant Director of Nursing documented the resident was seen on wound rounds on 2/4/2025. They had a stage 4 wound to the left heel. Progress was exacerbated due to generalized decline in the resident, and resident noncompliance with offloading wound. The ordered treatment for skin prep would continue. Recommendations included reposition as often as resident allowed, offload wound, and use of pressure off-loading boot. Nursing would continue to monitor resident's skin integrity.
On 2/11/2025 Physician Wound Consultant #30 documented the resident had a stage 4 pressure ulcer to their left heel that measured 2 x 2.5 x 0.1 centimeters. There was moderate serous exudate (wound drainage), and the wound had improved by evidence in decreased surface size. Recommendations included to apply calcium alginate (a soft wound dressing) once daily and apply gauze once daily. Recommendations also included reposition the resident per facility protocol, off-load wound, turn side to side in bed every 1-2 hours if able, and pressure off-loading boot.
There was no documented evidence the wound physician's recommendations were discussed or ordered by a provider until 2/21/2025.
On 2/21/2025, the Assistant Director of Nursing documented a late progress note for 2/11/2025. The resident was seen on 2/11/2025 for weekly wound rounds. Resident #67 had a stage 4 pressure ulcer to their left heel. There was moderate drainage and had 100% devitalized necrotic (dead) tissue. The treatment plan included to apply calcium alginate covering with dressing, wrap with gauze.
On 02/21/2025, a physician order was placed for calcium alginate to left heel, cover with dressing, date, initial, and wrap dressing/ankle with gauze, secure with tape and change daily.
On 2/25/2025, Physician Wound Consultant #30 documented the stage 4 pressure ulcer on the left heel measured 3 x 2 x 0.1 centimeters, moderate drainage and 100% necrotic (dead) tissue. The wound was debrided of devitalized and necrotic tissue. The treatment plan was to apply calcium alginate and leptospermum honey, apply sterile gauze and skin prep daily. Additional recommendations included to reposition per facility protocol, off-load wound, turn side to side in bed every 1 to 2 hours if able, pressure off-loading boot.
There was no documented evidence the wound physician's recommendations were discussed or ordered by a provider.
On 3/1/2025, The Assistant Director of Nursing documented the resident was seen on 2/25/2025 for weekly wound rounds for their stage 4 pressure ulcer to the left heel. The wound had moderate drainage with 100% necrotic tissue. The treatment plan had changed to apply calcium alginate with honey (an absorbent dressing used to remove dead tissue and promote a moist wound environment), cover with gauze sponge and wrapping with gauze daily.
The undated resident care record documented the resident needed assistance with turning every 2- 4 hours, was at risk for skin breakdown, and had an off-loading pressure boot for left foot.
On 3/5/2025 at 1:48 PM, the resident was observed in the common area in their recliner chair. Their left heel was directly against the footrest. The resident did not have an off-loading pressure boot on.
On 3/7/2025 at 9:10 AM, 9:44 AM, and 3:17 PM, the resident was observed without an off-loading pressure boot while seated in their recliner chair.
On 3/13/2025 at 12:15 PM, the resident was observed lying in bed with no off-loading pressure boot on.
During a wound care observation on 3/13/2025 at 12:25 PM, Licensed Practical Nurse #36 brought the wound care supplies into the resident's room and left the room to get a towel. When they entered the resident's room they did not sanitize or wash their hands prior to putting on their gloves. After removing the resident's old dressing and placing their heel on the towel they went to the bathroom and washed their hands. When they came back to the resident, they raised the head of the bed with the bed remote, touched the resident's bedside table, and did not sanitize or wash their hands prior to putting on new gloves to apply the resident's dressing.
During an interview on 3/14/2025 at 9:10 AM with Registered Nurse Unit Manager #17, they stated the Wound Care Consultant Physician's treatment recommendations were entered by their themselves or the Assistant Director of Nursing. Generally, the Assistant Director of Nursing obtained the order from the medical providers. They stated the resident was seen on 2/11/2025 by the Wound Care Consultant Physician and it appeared no wound care treatments were entered to be completed until 2/21/2025, but they were certain staff were completing wound treatments during that time. It also appeared the Wound Care Consultant Physician treatment recommendations made on 2/25/2025 were not entered to be completed as well. The resident had behavior issues and would take off their off-loading boot. If staff observed the resident without their off-loading boot on, they should attempt to apply the boot or let a nurse know about the resident's refusals.
During a telephone interview with Consultant Wound Physician #30 on 3/13/2025 at 1:53 PM, they stated they were at the facility weekly and as far as they were aware their treatment recommendations were put into place. They stated the resident's wound had a decline and they changed their treatment. They were unaware the facility was not implementing their wound care treatments as recommended.
3) Resident #113 was admitted with diagnosis including stage 3 pressure ulcer (full-thickness skin loss extending into fatty tissue) to their right heel and protein-calorie malnutrition. The 2/18/2025 Minimum Data Set assessment documented the resident had severely impaired cognition; did not reject care; required partial/maximal assistance with most of their activities of daily living including putting on/taking off their footwear; and the resident used a manual wheelchair. They were at risk for pressure ulcers, had one (1) stage 4 pressure ulcer that was not present on admission and one (1) unstageable pressure ulcer that was not present on admission. They received nutrition/hydration interventions to manage skin problems and received applications of ointments/medication.
The 8/15/2024 physician orders documented to attempt to keep blue booties on to off-load heels while in bed.
The revised 2/27/2025 Comprehensive Care Plan documented the resident was at risk for pressure ulcers. Interventions included to encourage resident to remain off right foot and monitor as resident frequently removed dressing and walked barefoot.
On 03/04/2025, Physician Wound Consultant #30 documented the resident had a pressure ulcer on right heel and right lateral foot. The right heel was a healing stage 4, measuring 0.7 x 0.6 x 0.2 centimeters, moderate serous drainage, and wound bed covered with 100% slough (moist, dead tissue). Treatment was leptospermum honey and cover with gauze island dressing daily. The right lateral foot was a healing unstageable pressure ulcer, measuring 0.3 x 0.3 centimeters in diameter. Treatment was to apply skin prep daily.
The undated resident care record (certified nurse aide care instructions) documented the resident was at risk for skin breakdown and used anti-slip socks/shoes. There was no documentation related to the resident removing dressing and walking barefoot.
The following 3/6/2025 observations of Resident #113 were made:
-At 12:36 PM, the resident was observed in the television lounge on the unit. They did not have their nonslip socks on, there was no bandage on their right foot, and their bare foot was on the carpet.
-At 1:02 PM, Certified Nurse Aide #37 walked past the resident down the hallway and did not acknowledge the resident's foot was bare and on the carpet.
-At 1:04 PM, Registered Nurse Unit Manager #31 walked past the resident and asked the resident What were you doing with your socks?, but they did not stop and put the resident's socks on.
-At 1:18 PM, and 1:33 PM, Certified Nurse Aide #37 walked past the resident down the hallway and did not acknowledge the resident's foot was bare and on the carpet.
- At 1:45 PM, Certified Nurse Aide #37 was observed talking to another resident near Resident #113 and did not acknowledge the resident's foot was bare and on the carpet.
- At 2:33 PM, the resident was observed with no socks, no bandage on their right foot, and their bare foot was on the carpet in the television lounge area.
During an interview on 03/06/2025 at 4:25 PM Certified Nurse Aide #56 stated they put socks on the resident as they noticed they were not wearing any. The resident would frequently take their socks off. The Certified Nurse Aide did not see any dressing on the resident's foot and did not tell anyone that there was no dressing in place.
During an interview on 3/7/2025 at 10:23 AM, Licensed Practical Nurse #31 stated if a resident's wound dressing was observed not to be in place, staff should have let the nurse know so the dressing could have been replaced. They had worked the day shift and part of the evening shift on 3/6/2025. They were not aware Resident #113's wound dressing was not on. This was something they would expect staff to tell them as it could lead to the wound worsening or a potential for infection.
During a treatment observation with Resident #113 and Licensed Practical Nurse #32, the resident had a small wound on the bottom of the right heel. The wound bed contained dark tissue, and the surrounding skin was white and macerated(wrinkly skin due to prolonged moisture). The Licensed Practical Nurse placed leptospermum honey on the wound and covered with a dry dressing. The wound on the right lateral foot was small with a scabbed area and the surrounding skin was intact. Skin Prep was applied to the wound.
During an interview with Registered Nurse Unit Manager #31 on 3/7/2024 at 11:09 AM, they stated if a resident did not have their wound dressing on their foot the resident could develop a possible infection, their wound could worsen or be slow to heal. They stated Resident #113 did take their footwear, socks, and dressings off at times and they observed Resident #113 on 3/6/2025 without socks on, but did not address it or tell anyone.
During a telephone interview with Physician Wound Consultant #30 on 3/14/2025 at 2:15 PM, they stated if a resident had an order for a wound dressing it should have been in place and if it came off nursing staff should have replaced it.
10NYCRR 415.12(c)(1)
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observations, record review, and interviews during the recertification survey conducted 3/4/2024-3/14/2025, the facility did not ensure each resident had the right to a dignified existence fo...
Read full inspector narrative →
Based on observations, record review, and interviews during the recertification survey conducted 3/4/2024-3/14/2025, the facility did not ensure each resident had the right to a dignified existence for 1 of 4 residents (Resident #508) reviewed. Specifically, Resident #508's bedside commode was not emptied, and urine and feces were malodorous and visible in plain sight.
Findings include:
The facility policy, Resident Rights, revised 7/5/2024 documented the resident had the right to receive services with reasonable accommodation of needs and a safe, clean, comfortable, homelike environment.
Resident #508 had diagnoses including fracture of right tibia (broken leg) and need for assistance with personal care. The 2/26/2025 Minimum Data Set assessment documented the resident was cognitively intact, had lower extremity impairment on one side, and required partial to moderate assistance with toileting.
The Comprehensive Care Plan initiated 3/6/2025 documented the resident was at risk for falls related to a tibia fracture. Interventions included increased staff assistance with intensity based on resident need and individualized toileting interventions were provided based on needs/ patterns. There was a documentation of the use of a commode.
The undated resident care record (care instructions) did not document use of a commode.
The following observations of Resident #508 were made:
- on 3/4/2025 at 10:53 AM, sitting up on the side of their bed with a bedside commode next to the bed that contained urine and toilet tissue. The resident stated the commode smelled all the time because there were not enough staff to empty it. At 12:42 PM, sitting up on the side of the bed eating their lunch with a visitor sitting next to the bed. The bedside commode was directly next to the bed and contained urine and toilet tissue that filled approximately one third of the bucket receptacle.
- on 3/6/2025 at 9:06 AM, lying in bed. The bedside commode was directly next to the bed and was approximately half full of urine, feces, and toilet tissue. The commode was visible to anyone who entered the room.
During an interview on 3/7/2025 at 9:36 AM, Resident #502 stated they often smelled the contents of their commode. They put their call bell on after a bowel movement, but they could not expect the commode to be emptied every time they used it because there was not enough staff. The staff that delivered their meal trays were not allowed to empty their commode.
During an interview on 3/7/2025 at 12:01 PM, Certified Nurse Aide #16 stated Resident #508 had a bedside commode because they could not bear weight on their leg. The resident rang for assistance because they needed help transferring on and off the commode. When they came in for their shift, the commode usually had contents in it because it was not emptied by the overnight shift. It was not appropriate the commode was not emptied and had waste in it, especially when the resident was eating. There was no cover to the commode and urine and feces had an odor. The resident had frequent visitors, and it was not dignified that the visitors saw and smelled the contents of the commode. They worked on 3/4/2025 and 3/6/2025 but it was hectic, they were too busy, and they could not keep up with emptying the commode. The commode should be emptied after each use.
During an interview on 3/7/2025 at 2:59 PM, Licensed Practical Nurse #15 stated the bedside commodes were not always emptied. They often saw commodes with waste contents in them. They recalled a time when the toilet was clogged because a large volume of contents from the commode was flushed. Resident #502 usually asked to have the commode emptied. It was busy so it did not get emptied every time. If it was not emptied, this was unsanitary they had to eat meals next to a soiled commode. There had been times the resident's family had asked to have the commode emptied and it was embarrassing to the resident their family saw the contents of their commode.
During an interview on 3/13/2025 at 10:36 AM, Registered Nurse Unit Manager #14 stated Resident #508 had a bedside commode. They expected the commode to be emptied after each use. If the commode was one third or half full, it was not being emptied after each use. The commode should be emptied for cleanliness and infection control. There could be an odor, it was a dignity issue and was humiliating to the resident their visitors saw and smelled the contents of their commode. When eating, the resident should have enjoyed the smell of their food, not the commode and it simply should not have happened.
10NYCRR 415.5(b)(1-3)
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0800
(Tag F0800)
Could have caused harm · This affected 1 resident
Based on observations, record review, and interviews during the recertification survey conducted 3/4/2025- 3/14/2025, the facility failed to provide each resident with a nourishing, palatable, well-ba...
Read full inspector narrative →
Based on observations, record review, and interviews during the recertification survey conducted 3/4/2025- 3/14/2025, the facility failed to provide each resident with a nourishing, palatable, well-balanced diet that meets their daily nutritional and special dietary needs, taking into consideration the preferences of each resident for 2 of 2 meals observed. Specifically, Resident #25's lunch meal was not served at a palatable, flavorful, and at an appetizing temperature, and the 6th floor breakfast meal was delivered to the unit 30 minutes after the scheduled time with the last meal tray was passed at 9:07 AM, resulting in unappetizing food temperatures. Additionally, during the initial main kitchen tour multiple food items were not dated when opened; 1 cooler was not in working order, did not have signage to indicate it was not to be used, contained 1 oral nutrition supplement, and the temperature gauge read 57 degrees Fahrenheit.
Findings include:
The facility's revised 2/2024 Temperature/ Taste Test policy documented to take the temperature and taste all foods prior to service to ensure palatability and acceptable temperatures for service. Twenty minutes prior to service, the cook serving the meal was responsible to take the temperature of all food being served from the steam line or stove for that meal. Any potentially hazardous food not meeting the acceptable temperatures of 41 degrees Fahrenheit or below for cold food, and 160 degrees Fahrenheit or above for hot food must be cooled or re-heated before service.
The facility's 6/2021 Tray Cart Schedule Log documented the following times for Breakfast:
-4th Floor 7:10 AM.
-7th Floor 7:20 AM.
-Unit A-3 7:30 AM.
-Unit A-2 7:35 AM.
-Unit B and Gardenview 7:45 AM.
-3rd Floor 7:55 AM.
-5Th Floor 8:05 AM.
-6Th Floor 8:15 AM.
TEST TRAYS:
During an interview with Resident #25 on 3/4/2025 at 11:48 AM, they stated the mealtimes were not consistent, the food was cold, and hard. When they requested an alternative meal sometimes those items were cold as well.
On 3/6/2025 at 12:28 PM, Resident #25's lunch meal was tested for taste and temperature in the presence of Licensed Practical Nurse #15. The following temperatures were obtained:
- Cheeseburger measured 124.3 degrees Fahrenheit.
- Onion rings measured 104.2 degrees Fahrenheit.
- Macaroni salad measured 55.2 degrees Fahrenheit,
- Mandarin oranges measured 59.4 degrees Fahrenheit.
- Water measured 48.7 degrees Fahrenheit.
- Milk measured 47.5 degrees Fahrenheit.
The cheeseburger was hard and difficult to chew, the onion rings were soggy and greasy, and the macaroni
salad had a very strong dill flavor.
During an observation in the main kitchen on 3/7/2025 at 8:02 AM, Head cook #69 was observed to take the temperatures of food items on the tray line. The following temperatures were documented:
- Hashbrowns measured 140 degrees Fahrenheit.
- Scrambled eggs measured 146 degrees Fahrenheit.
- Oatmeal measured 176 degrees Fahrenheit.
On 3/7/2025 at 8:27 AM, the 6th Floor meal trays started to be plated and going down the tray line and 8:44 AM, the last meal tray was placed on the delivery cart and arrived on the 6th floor at 8:45 AM. The last meal tray was passed at 9:07 AM and was tested for taste and temperature in the presence of the Food Service Director using a facility thermometer. The following temperatures were obtained:
- Cream of wheat measured 137 degrees Fahrenheit.
- Scrambled eggs measured 119.3 degrees Fahrenheit.
- Toast measured 117.4 degrees Fahrenheit.
- 1% milk measured 53.1 degrees Fahrenheit and 2nd carton of 1% measured 52.2 degrees Fahrenheit.
- Orange Juice measured 58.8 degrees Fahrenheit and cranberry juice measured 57.1 degrees Fahrenheit.
During an interview with the Food Service Director on 3/7/2025 at 9:14 AM, they stated all hot items should be served at 130 degrees Fahrenheit or more and cold items should be served below 42 degrees Fahrenheit for palatability. They stated the 6th floor meal trays were late due to a staff member in the kitchen dropping a tray of drinks. The unit was made aware the meal was going to be late.
During a follow up interview with the Food Service Director on 3/7/2025 at 3:30 PM, they stated it was important for food items to be served at palatable and appetizing temperatures.
FOOD STORAGE:
During the initial main kitchen tour on 3/7/2025 at 9:55 AM, in the presence of the Food Service Director the walk-in cooler contained 1 plastic container of 2 cups of liquids eggs without a date on it. The sandwich cooler contained 2 pounds of sliced provolone cheese in plastic wrap undated, 1 and ¼ pounds of sliced Swiss cheese wrapped in plastic wrap undated, 3 pounds of sliced American cheese in plastic wrap undated, 1 pound of sliced deli turkey meat in plastic wrap undated, and 1.5 pounds of sliced deli ham in plastic wrap undated.
During an interview with the Food Service Director on 3/4/25 at 10:18 AM, they stated it was important for all food items to be labeled and dated once they were open or removed from the original package for food safety reason. Items were only good for 3 days unless they were in the original packs with a best used by date on the packaging.
EQUIPMENT:
During the initial main kitchen tour on 3/7/2025 at 9:55 AM, in the presence of the Food Service Director, 1 cooler was not in working order, did not have signage to indicate it was not to be used, contained 1 oral nutrition supplement, and the temperature gauge read 57 degrees Fahrenheit.
During an interview with the Food Service Director on 3/7/2025 at 8:13 AM, they stated if equipment was not in working order, a sign should be placed on the item to indicate it should not be used to ensure food safety. The cooler stopped working on 3/3/2025 and they placed an out of order sign on it. They were unsure where the sign went. They had let the facility's Administrator know the cooler was not working and work order was placed for it to be repaired.
On 3/14/2025 at 9:14 AM, the facility's Administrator provided an electronic message from the Food Service Director dated 3/3/2025 at 1:43 PM, alerting them to the issue.
10NYCRR 415.14
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Administration
(Tag F0835)
Could have caused harm · This affected multiple residents
Based on observations, record review, and interviews during the recertification and abbreviated survey (NY00330552 and NY00359628) conducted 3/4/2025- 3/10/2025, and the recertification extended surve...
Read full inspector narrative →
Based on observations, record review, and interviews during the recertification and abbreviated survey (NY00330552 and NY00359628) conducted 3/4/2025- 3/10/2025, and the recertification extended survey conducted 3/10/2025-3/14/2025, the facility did not ensure it was administered in a manner that enabled it to use its resources effectively and efficiently to attain or maintain the highest practicable physical, mental, and psychosocial well-being of each resident. Specifically, administration failed to ensure that residents received appropriate quality of care by allowing the following deficient practices to exist, placing residents at risk for serious injury, serious harm, serious impairment, or death, F 689 Accident Hazards; failed to ensure policies and procedures were properly identified, communicated, and consistently implemented. Administration failed to ensure sufficient nursing staff to ensure resident safety and attain or maintain the highest practicable physical, mental and psychosocial well-being F725, leading to several deficient practices in the areas of F684 Quality of Care, F686 Treatment and Services to Prevent Pressure Ulcers, and F692 Nutrition/Hydration Status Maintenance.
Findings include:
The facility job description, Administrator/CEO, dated 8/10/2004, documented the Administrator reported to the Board of Directors and responsible for all phases of the facility services. They direct all department heads/directors in their responsibilities of duties and supervises and executes duties and responsibilities.
The facility Quality Assurance Plan, dated 3/2/2025, documented the committee plan, function and purpose was to anticipate compliance and quality problems; to take meaningful action, and evaluate the effectiveness of the action plan. The committee incorporates the process of all disciplines to perform ongoing assessments and audits to detect both positive and negative outcomes. The goal was to continuously improve resident, staff and service outcomes.
Deficient Practice Information:
Resident's Free from Accident, Refer to the citation text under F689.
The facility failed to ensure the residents' environment remained free of accident hazards for 1 of 6 residents reviewed.
Quality of Care, Refer to the citation text under F684
The facility failed to ensure residents received treatment and care in accordance with professional standards of practice for 1 of 2 residents.
Treatment/Services to Prevent/Heal Pressure Ulcer, Refer to the citation text under F686
The facility failed to ensure a resident with pressure ulcers received the necessary treatment and services, consistent with professional standards of practice, to promote wound healing, prevent infection and prevent new ulcers from developing for 3 of 4 residents.
Nutrition/Hydration Status Maintenance, Refer to the citation under F692
The facility failed to ensure residents maintained acceptable parameters of nutritional status for 2 of 3 residents.
Sufficient Nursing Staff, Refer to the citation under F725
The facility failed to ensure sufficient nursing staff to ensure resident safety and attain or maintain the highest practicable physical, mental and psychosocial well-being for 12 of 12 anonymous residents.
During an interview on 3/11/2025 at 1:12 PM, the Administrator stated upon admission residents were assessed for elopement risk and this was done each quarter as well. Resident #85 was determined to be an elopement risk on admission 6/17/2024 and at that time a wander prevention device was place on the resident. The resident had removed the wander guard the evening they eloped. Prior to becoming Administrator at the facility, there were no orders placed in the residents record to check that wander prevention devices were in place and working on the resident each shift.
During an interview of the Administrator on 3/13/2025 at 1:50 PM, they stated they have an average census between 140-145 residents, unit 2 remains closed and there is a registered nurse on all three shifts. The minimum staffing for A and B wing is 2 certified nurse aides on each side and 1 licensed practical nurse; the high-rise staffing for each unit is one licensed practical nurse covers unit 4 and 5 and one licensed practical nurse covers 6 and 7, and there is one certified nurse aide on each unit. They stated to a certain extent staffing can affect the quality-of-care residents receive. It was challenging to give good quality of care if the facility was short staffed.
During an interview on 3/14/2025 at 1:54 PM, the Administrator stated they decided what issues needed a performance improvement plan based on their audit trends and whatever was discussed in the quality assurance meetings as reported in their quality measure reports. They were working on staffing and scheduling continuously. They were running weekly reports on their pressure ulcers and those reports were brought to the quality assurance team. They did not have any audits in place for residents with weight loss, or activity of daily living or quality of care issues.
10 NYCRR 483.70(i)
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record reviews, and interviews during the recertification survey and abbreviated (NY00330552) surveys con...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record reviews, and interviews during the recertification survey and abbreviated (NY00330552) surveys conducted 3/4/2025- 3/14/2025, the facility did not ensure sufficient nursing staff to ensure resident safety and attain or maintain the highest practicable physical, mental and psychosocial well-being for all 149 residents in the facility. Specifically, during a confidential resident group meeting residents stated staffing was not sufficient, and call bells were not answered timely especially during the night shift. Deficiencies related to staffing levels were identified in the areas of Activities of Daily Living (F677), Quality of Care (F684), Treatment/Services to Prevent and Heal Pressure Ulcer (F686), and Nutrition/Hydration Status Maintenance (F692).
Findings include:
The Facility assessment dated [DATE] documented the facility was licensed for 200 beds with an average daily census of 136. Residents of the facility had both chronic illness and post-acute conditions. The residents of the short-term transitional care unit typically entered the facility with dependence in activity of daily living care and mobility. The residents living in the long-term care units typically had several chronic diseases, 96% of these residents' required assistance with mobility, and 99% of the resident's required assistance with bathing, dressing, and grooming. Most residents (40%) could eat after staff set -up their meals. The staffing plan for nursing and nutrition services were evaluated at the beginning of each shift and adjusted as needed to meet the needs and acuity of the resident population.
The facility policy, Staffing Plan, revised 9/5/2024, documented consideration was given to residents need when the composition of nursing staff was determined. Sufficient personnel were assigned to assure safe, effective nursing care; and a staffing pattern was developed that considered the needs of the resident population.
The facility's 3/7/2025 list of resident's requiring assistance of two documented:
- A-Wing - 4 residents required assistance of two for personal care and toileting.
- B-Wing - 16 residents required assistance of two for toileting, bed positioning and transfers.
- Unit 3- 1 resident required assistance of two for transfers.
- Unit 4- 10 residents required assistance of two for personal care, toileting, and transfers.
- Unit 5- 6 residents required assistance of two for personal care, and transfers.
- Unit 6- 7 residents required assistance of two for transfers, toileting and personal care.
- Unit 7- 8 residents required assistance of two for transfers, toileting and personal care.
During the entrance conference interview on 3/4/2025 at 10:07 AM, the Administrator stated the facility's census was 149, with one 40 bed unit closed (Unit 2).
The facility posted staffing from 3/4/2025 through 3/13/2025 documented a census of 140- 149 residents. Actual staffing on the units documented:
Tuesday 3/4/2025, day shift staffing:
- A wing: 1 registered nurse Unit Manager, 1 licensed practical nurse, 2 certified nurse aides, and one unit helper for 23 residents.
- B wing: 1 registered nurse Unit Manager, 1 licensed practical nurse, 1 certified nurse aides, and 1 unit helper for 37 residents.
- Unit 3: 1 registered nurse Unit Manager (who also covered Unit 6 and 7), 1 licensed practical nurse, and 1 certified nurse aides for 18 residents. - Unit 4 and Unit 5: 1 registered nurse Unit Manager, 1 licensed practical nurse, 2 certified nurse aides, and 1 unit helper for 39 residents.
- Unit 6 and Unit 7: 1 registered nurse Unit Manager, 1 licensed practical nurse, 2 certified nurse aides and 1 unit helper for 35 residents.
Tuesday 3/4/2025, evening shift staffing:
- 1 registered nurse House Supervisor.
- A wing: 1 licensed practical nurse and 2 certified nurse aides for 23 residents.
- B wing: 1 licensed practical nurse and 2 certified nurse aides for 37 residents.
- Unit 3: 1 licensed practical nurse, 1 certified nurse aide for 18 residents.
- Unit 4 and Unit 5: 1 licensed practical nurse, 2 certified nurse aides for 39 residents. - Unit 6 and Unit 7: 1 licensed practical nurse, 2 certified nurse aides for 35 residents.
Tuesday 3/4/2025, night shift staffing:
- 1 registered nurse House Supervisor.
- A Wing: 1 licensed practical nurse until 4:30 AM, registered nurse House Supervisor from 4:30 AM- 7:00 AM, 3 certified nurse aides (2 working from 2:00 AM - 6:00 AM) for 23 residents
- B Wing: 1 licensed practical nurse, 3 certified nurse aides (1 working 2:00 AM- 7:00 AM) for 37 residents.
- Unit 3: 1 licensed practical nurse, 0 certified nurse aide for 18 residents. - Unit 4 and 5: 1 licensed practical nurse, 2 certified nurse aides for 39 residents. - Unit 6 and 7: 1 licensed practical nurse, 2 certified nurse aides for 35 residents.
Wednesday 3/5/2024 day shift:
- A wing: 1 registered nurse Unit Manager, 1 licensed practical nurse, 3 certified nurse aides (one aide working until 10:15 AM), and one unit helper for 23 residents.
- B wing: 1 registered nurse Unit Manager, 1 licensed practical nurse, 3 certified nurse aides, and 1 unit helper for 37 residents.
- Unit 3: 1 registered nurse Unit Manager (who covered Unit 6 and 7), 1 licensed practical nurse, and 1 certified nurse aides for 18 residents. - Unit 4 and Unit 5: 1 registered nurse Unit Manager, 1 licensed practical nurse, 2 certified nurse aides, and 1 unit helper for 39 residents.
- Unit 6 and Unit 7: 1 registered nurse Unit Manager, 1 licensed practical nurse, 2 certified nurse aides for 35 residents.
Wednesday 3/5/2025, evening shift staffing:
- 1 registered nurse House Supervisor (also worked day shift).
- A wing: 1 licensed practical nurse and 2 certified nurse aides for 23 residents.
- B wing: 1 licensed practical nurse and 2 certified nurse aides for 37 residents.
- Unit 3: 1 licensed practical nurse, 1 certified nurse aide for 18 residents.
- Unit 4 and Unit 5: 1 licensed practical nurse, 2 certified nurse aides for 39 residents. - Unit 6 and Unit 7: 1 licensed practical nurse, 2 certified nurse aides for 35 residents.
Wednesday 3/5/2025, night shift staffing:
- 1 registered nurse House Supervisor (also covered medication administration on Unit 3), 1 certified nurse aide to float from 10:00 PM- 2:00 AM.
- A Wing: 1 licensed practical nurse, 2 certified nurse aides for 23 residents
- B Wing: 1 licensed practical nurse, 2 certified nurse aides for 37 residents
- Unit 3: 1 licensed practical nurse, 1 certified nurse aide for 18 residents. - Unit 4 and 5: 1 licensed practical nurse, 2 certified nurse aides for 39 residents. - Unit 6 and 7: 1 licensed practical nurse, 2 certified nurse aides for 35 residents.
Thursday 3/6/2025 day shift:
- A wing: 1 registered nurse Unit Manager, 1 licensed practical nurse, 2 certified nurse aides, and 1 unit helper for 23 residents.
- B wing: 1 registered nurse Unit Manager, 1 licensed practical nurse, 3 certified nurse aides, and 1 unit helper for 37 residents.
- Unit 3: 1 registered nurse Unit Manager (also covered Units 6 and 7) passing 7:00 AM - 11:00 AM medications, 1 licensed practical nurse 11 AM- 3 PM, and 1 certified nurse aides for 18 residents. - Unit 4 and Unit 5: 1 registered nurse Unit Manager, 1 licensed practical nurse, 2 certified nurse aides, and 1 unit helper for 39 residents.
- Unit 6 and Unit 7: 1 registered nurse Unit Manager, 1 licensed practical nurse, 2 certified nurse aides for 35 residents.
Thursday 3/6/2025, evening shift staffing:
- 1 registered nurse House Supervisor (also worked day shift working until 7:45 PM) 1 licensed practical nurse house supervisor 7:45 PM- 11:00 PM.
- A wing: 1 licensed practical nurse and 2 certified nurse aides (one working 2:00 PM- 6:00 PM) for 23 residents.
- B wing: 1 licensed practical nurse and 2 certified nurse aides for 37 residents
- Unit 3: 1 licensed practical nurse until meds are done, 1 certified nurse aide for 18 residents.
- Unit 4 and Unit 5: 1 licensed practical nurse, 2 certified nurse aides for 39 residents. - Unit 6 and Unit 7: 1 licensed practical nurse, 2 certified nurse aides for 35 residents.
Thursday 3/6/2025, night shift staffing:
- 1 registered nurse House Supervisor (also covered medication pass on Unit 3
-A Wing: 1 licensed practical nurse, 1 certified nurse aides for 23 residents
-B Wing: 1 licensed practical nurse, 2 certified nurse aides (one working 10:00 PM- 2:00 AM) for 37 residents.
- Unit 3: 1 registered nurse house supervisor to pass medication, 1 certified nurse aide for 18 residents. - Unit 4 and 5: 1 licensed practical nurse, 2 certified nurse aides for 39 residents. - Unit 6 and 7: 1 licensed practical nurse, 2 certified nurse aides for 35 residents.
Friday 3/7/2025 day shift:
- A wing: 1 registered nurse Unit Manager, 1 licensed practical nurse, 2 certified nurse aides (one working 10 AM - 2 PM), and 1 unit helper for 23 residents.
- B wing: 1 registered nurse Unit Manager, 1 licensed practical nurse, 2 certified nurse aides, and 1 unit helper for 37 residents.
- Unit 3: 1 registered nurse Unit Manager (also covered Unit 6 and 7), 1 licensed practical nurse, and 1 certified nurse aides for 18 residents. - Unit 4 and Unit 5: 1 registered nurse Unit Manager, 1 licensed practical nurse, 2 certified nurse aides, and 1 unit helper for 39 residents.
- Unit 6 and Unit 7: 1 registered nurse Unit Manager, 1 licensed practical nurse, 2 certified nurse aides for 35 residents.
Friday 3/7/2025 evening shift staffing:
-1 registered nurse House Supervisor (also worked day shift working until 7:45 PM) and 1 licensed practical nurse house supervisor who worked 7:45 PM- 11:00 PM.
- A wing: 1 licensed practical nurse and 2 certified nurse aides (one working 2:00 PM - 6:00 PM) for 23 residents.
- B wing: 1 licensed practical nurse and 2 certified nurse aides for 37 residents.
- Unit 3: 1 licensed practical nurse until meds are done and 1 certified nurse aide for 18 residents.
- Unit 4 and Unit 5: 1 licensed practical nurse, 2 certified nurse aides for 39 residents. - Unit 6 and Unit 7: 1 licensed practical nurse, 2 certified nurse aides for 35 residents.
Friday 3/7/2025 night shift staffing:
- 1 registered nurse House Supervisor and 1 registered nurse Infection Preventionist to complete first medication pass on unit 3.
- A Wing: 1 licensed practical nurse and 1 certified nurse aides for 23 residents
- B Wing: 1 licensed practical nurse and 2 certified nurse aides for 37 residents
- Unit 3: 1 registered nurse infection preventionist to complete first medication pass and 1 certified nurse aide for 18 residents. - Unit 4 and 5: 1 licensed practical nurse and 2 certified nurse aides for 39 residents. - Unit 6 and 7: 1 licensed practical nurse and 2 certified nurse aides for 35 residents.
Saturday 3/8/2025 day shift:
- 1 registered nurse House Supervisor.
- A wing: 1 licensed practical nurse, 1 certified nurse aides, and 1 unit helper for 23 residents.
- B wing: 1 licensed practical nurse, 1 certified nurse aides, and 1 unit helper for 37 residents.
- Unit 3:1 licensed practical nurse and 1 certified nurse aides for 18 residents. - Unit 4 and Unit 5: 1 licensed practical nurse, 2 certified nurse aides, and 1 unit helper for 39 residents.
- Unit 6 and Unit 7:1 licensed practical nurse and 3 certified nurse aides (one working 6:00 AM- 10:30 AM) for 35 residents.
Saturday 3/8/2025 evening shift staffing:
- 1 registered nurse House Supervisor (also schedule to work night shift) and 1 licensed practical nurse house supervisor 7:45 PM- 11:00 PM.
- A wing: 1 licensed practical nurse and 1 certified nurse aides for 23 residents.
- B wing: 1 licensed practical nurse and 2 certified nurse aides for 37 residents
- Unit 3: 1 registered nurse and 1 certified nurse aide for 18 residents.
- Unit 4 and Unit 5: 1 licensed practical nurse and 2 certified nurse aides for 39 residents. - Unit 6 and Unit 7: 1 licensed practical nurse, and 3 certified nurse aides for 35 residents.
Saturday 3/8/2025 night shift staffing:
- 1 registered nurse House Supervisor.
- A Wing: 1 licensed practical nurse and 1 certified nurse aide at 2:00 AM for 23 residents.
- B Wing: 1 licensed practical nurse and 1 certified nurse aides for 37 residents.
- Unit 3: 1 registered nurse until 3 AM, 1 licensed practical nurse at 3:00 AM- 7:00 AM, and no certified nurse aides for 18 residents. - Unit 4 and 5: 1 licensed practical nurse and 2 certified nurse aides for 39 residents. - Unit 6 and 7: 1 licensed practical nurse and 2 certified nurse aides for 35 residents.
Sunday 3/9/2025 day shift:
- 1 registered nurse House Supervisor scheduled until 7:00 PM.
- A wing: 1 licensed practical nurse, 1 certified nurse aides, and 1 unit helper for 23 residents.
- B wing: 1 licensed practical nurse, 2 certified nurse aides, and 1 unit helper for 37 residents.
- Unit 3:1 licensed practical nurse and 1 certified nurse aides for 18 residents. - Unit 4 and Unit 5: 1 licensed practical nurse, 2 certified nurse aides (one not in until 10 AM), and 1 unit helper for 39 residents.
- Unit 6 and Unit 7:1 licensed practical nurse and 2 certified nurse aides for 35 residents.
Sunday 3/9/2025 evening shift staffing:
- 1 registered nurse House Supervisor
- A wing: 1 licensed practical nurse and 1 certified nurse aides for 23 residents.
- B wing: 1 licensed practical nurse and 2 certified nurse aides (one aide to float between A & B from 2:00 PM- 6:00 PM) for 37 residents.
- Unit 3: 1 licensed practical nurse and 1 certified nurse aide for 18 residents.
- Unit 4 and Unit 5: 1 licensed practical nurse and 2 certified nurse aides for 39 residents. - Unit 6 and Unit 7: 1 licensed practical nurse and 2 certified nurse aides for 35 residents.
Sunday 3/9/2025 night shift staffing:
- 1 registered nurse house supervisor.
- A Wing: 1 licensed practical nurse, 2 certified nurse aides (one from 2:00 AM- 6:00 AM) for 23 residents
- B Wing: 1 licensed practical nurse, 2 certified nurse aides (one from 2:00 AM- 6:00 AM) for 37 residents
- Unit 3: 1 registered nurse, 1 certified nurse aide for 18 residents. - Unit 4 and 5: 1 licensed practical nurse, 2 certified nurse aides for 39 residents. - Unit 6 and 7: 1 registered nurse House Supervisor (11:00 PM- 3:00 AM),1 licensed practical nurse (3:00 AM- 7:00 AM), 2 certified nurse aides for 35 residents.
Monday 3/10/2025 day shift:
- A wing: 1 registered nurse Unit Manager, 1 licensed practical nurse, 3 certified nurse aides, and 1 unit helper for 23 residents.
- B wing: 1 registered nurse Unit Manager, 1 licensed practical nurse, 3 certified nurse aides (one working 10 AM- 2 PM), and 2-unit helpers (one orienting) for 37 residents.
- Unit 3:1 registered nurse Unit Manager (covering medications on unit 3 and covering units 6 and 7), and 1 certified nurse aides for 18 residents. - Unit 4 and Unit 5: 1 licensed practical nurse, 2 certified nurse aides, and 1 unit helper for 39 residents.
- Unit 6 and Unit 7:1 licensed practical nurse, 2 certified nurse aides for 35 residents.
Monday 3/10/2025 evening shift staffing:
- 1 registered nurse House Supervisor
- A wing: 1 licensed practical nurse and 1 certified nurse aides for 23 residents.
- B wing: 1 licensed practical nurse and 2 certified nurse aides for 37 residents.
- Unit 3: 1 licensed practical nurse and 1 certified nurse aide for 18 residents.
- Unit 4 and Unit 5: 1 licensed practical nurse and 2 certified nurse aides for 39 residents. - Unit 6 and Unit 7: 1 licensed practical nurse and 2 certified nurse aides for 35 residents.
Monday 3/10/2025 night shift staffing:
- 1 registered nurse House Supervisor
- A Wing: 1 licensed practical nurse and 2 certified nurse aides for 23 residents.
- B Wing: 1 licensed practical nurse and 2 certified nurse aides for 37 residents.
- Unit 3: 1 licensed practical nurse and 1 certified nurse aide for 18 residents. - Unit 4 and 5: 1 licensed practical nurse and 2 certified nurse aides for 39 residents. - Unit 6 and 7: 1 licensed practical nurse and 2 certified nurse aides for 35 residents.
Activities of Daily Living (refer to F677)
Based on observations, record review, and interviews the facility did not ensure residents who were unable to carry out activities of daily living received the necessary services to maintain good nutrition, grooming, and personal and oral hygiene for Residents #41, #65, and #87. There was no documented evidence Resident #41 received showers as care planned; Resident #65 did not receive assistance at meals as care planned; Resident #87 was not toileted in a timely manner and did not receive toileting assistance as care planned; and Resident #87 missed an activity due to staff not getting them up.
Quality of Care (refer to F684)
Based on observations, interviews, and record review the facility failed to ensure residents received treatment and care in accordance with professional standards of practice, the comprehensive person-centered care plan, and the residents' choices for Resident #136. Resident #136 was not treated with dignity, was not assisted with activity of daily care, was isolated in their room without activities/stimulation, and their tube feeding was not administered as ordered.
Treatment/Services to Prevent/Heal Pressure (refer to F686)
Based on observations, record review, and interviews the facility failed to ensure a resident with pressure ulcers received the necessary treatment and services, consistent with professional standards of practice, to promote wound healing, prevent infection and prevent new ulcers from developing for Residents #60, #67, and #113.Specifically, Resident #60 developed a Stage 4 (full-thickness skin loss with exposed bone, tendon or muscle) pressure ulcer to their right hip and care planned interventions were not consistently followed to prevent pressure ulcers from developing and when the pressure ulcer developed it was not adequately treated to prevent infection; Resident #67 developed a Stage 4 pressure ulcer to their left heel while in the facility and there was no documented wound care for 11 days, the wound care physician recommendations were not followed for 2 weeks, the resident was observed without their pressure relieving boots on, and the nurse did not perform hand hygiene during a dressing change; Resident #113 had a Stage 3 (full-thickness skin loss extending into fatty tissue) pressure ulcer to their right heel and was observed without a dressing on their wound.
Nutrition/Hydration Status Maintenance (refer to F692)
Based on observations, record review, and interviews the facility failed to ensure residents maintained acceptable parameters of nutritional status for Residents #67 and #134. Residents #67 and #134 had significant weight changes, medical was not made aware of significant weight changes, and they did not receive their nutritional supplements as ordered. Resident #67 did not receive their ordered adaptive equipment or supervision at multiple meals during survey.
GENERAL STAFFING
During an interview on 3/4/2025 at 10:53 AM, Resident #508 stated on 2/20/2025, their first night at the facility, they waited 2 hours for their call bell to be answered. They almost called 911 because they thought their call bell did not work. It happened again last night, and they ended up soiling themself because they waited too long. They were embarrassed that Certified Nurse Aide #20 had to clean them up. There was usually only one certified nurse aide working on the overnight shift.
During an interview on 3/4/2025 at 3:52 PM, Certified Nurse Aide #33 stated they floated to all the units. Currently they were the only staff on Unit 5, the licensed practical nurse was on the 4th floor. There were 17 residents on the unit, and this was how staffing was during the day. They stated most of the residents required assistance of two.
During an interview on 3/4/2025 at 4:06 PM, Licensed Practical Nurse #6 stated they were scheduled to cover Units 4 and 5. They were working the evening and night shift and was the only nurse for the two units.
During an interview on 3/5/2025 at 11:53 PM, Licensed Practical Nurse #32 stated they covered units 4 and 5 and there was one certified nurse aide on each floor. That was the typical staffing pattern. After they finished their medication pass, they had to assist the certified nurse aide with getting residents toileted and up for meals.
During an interview on 3/5/2025 at 1:50 PM, Certified Nurse Aide #19 who was assigned to unit 3, stated they were upset because they were mandated to work the evening shift again. They were mandated to work overtime an average of three times per week. It was always the same few certified nurse aides that were mandated because there was no staff. When they came in for their shift in the morning there were call lights going off at the same time. There was no one to help. Sometimes the nurse helped with the residents that required assistance of two to get out of bed. It was important to have enough staff to ensure the residents got the care they deserve. The resident's safety was put at risk when there was not enough staff. They reported their concerns to the Supervisor or the Nurse Manager, but nothing changed.
During an interview on 3/06/2025 at 8:44 AM, Licensed Practical Nurse #36 stated they were overwhelmed working both Units 6 and 7. They stated they must be on the unit when residents were in the dining room but if something happened on the other unit, that became a problem of having to find another staff person to cover the dining room. They stated they were behind on their medication pass. Sometimes short cuts were taken, and things were not always done as they should be. They stated they felt it was dangerous sometimes when they rushed all the time.
During an interview on 3/06/2025 at 10:51 AM, Certified Nurse Aide #35 stated low staffing was a problem especially if they had a resident with behavior issues, which sometime could take 2 staff to intervene to calm the resident. They must wait for someone to come to help with care when the residents required 2 staff, and this delayed resident care which was frustrating for the staff and the resident.
During an interview on 3/07/2025 at 12:22 PM, Certified Nurse Aide #34 stated they were the only aide working Unit 4 today, and there was floating staff to help.
During an interview on 3/11/2025 at 3:37 PM, Registered Nurse Unit Manager #31 stated they were responsible to manage Units 4 and 5. They stated 16 - 24 staff members were let go 2 weeks ago and that included the unit helpers for the evening shift. They stated they were not always able to complete admission assessments and weekly skin checks because it was expected they were on the unit to assist the nurse aides with getting residents up and helping with personal care needs. They stated it was hard to keep track of all the residents, their assessments, care plans when they covered 2 units, and assisted with care of the residents. They said between Units 4 and 5 they had 16 residents who required mechanical lifts and assistance of 2 staff.
During an interview on 3/14/2025 at 9:07 AM, Resident #699's family member stated there was never staff on the floor (unit 6). There were times they kept ringing the call bell and nobody came. They stated Resident #699 wanted to call 911 and they called the front desk and told the front desk receptionist if they did not get someone to Resident #699's room they would call 911. There was not enough help for all the residents on this floor.
During an interview on 3/13/2025 at 12:31 PM, the Assistant Director of Nursing/Interim Staffing Coordinator stated the previous staffing coordinator recently resigned, and they currently were doing the scheduling with the assistance of the Director of Nursing. They stated they would like to have a licensed practical nurse and one certified nurse aide on each floor. In the high rise (units 3-7), there was one aide for 20 residents. If there were residents that need two staff for assistance, they would utilize the nurse on the unit or call someone from another unit. The A wing was the rehabilitation floor, and there were always 2 certified nurse aides, one licensed practical nurse, and a registered nurse Unit Manager because that unit had more acute residents. They also had unit helpers to assist with making beds, passing water, but they could not do hands on care. Weekend staffing was a big challenge, the current goal was to just fill in the staffing holes. On the weekends, the on call registered nurse may have to come in to assist with the medication administration. They stated they were the House supervisor in the evenings sometimes. They recently they had to pass medication on the A wing, while supervising all the units, and there were a few falls that evening.
During a telephone interview on 3/13/2025 at 1:31 PM, former Staffing Coordinator #23 stated staffing ratios were always a challenge at the facility. They maintained the minimum staffing for each shift, but evenings, nights, weekends, and Mondays were hard to staff adequately. They would staff 1 licensed practical nurse per 40 residents on the A and B wings;1 licensed practical nurse for two units (40 residents) in the high rise (units 3-7); and 1 certified nurse aide per 20 residents. If staff called in then the previous shift staff person was mandated to stay, or they would reach out to staffing agency to fill in the holes.
During an interview with the Administrator and the Director of Nursing on 3/13/2025 at 1:50 PM, they stated they had an average census between 140-145 residents, Unit 2 remained closed and there was a registered nurse on all three shifts. The minimum staffing for A and B wings was 2 certified nurse aides on each side and 1 licensed practical nurse; the high rise (Units 3-7) staffing for each unit was one licensed practical nurse who covered units 4 and 5 and one licensed practical nurse who covered 6 and 7, and there was one certified nurse aide on each unit. They stated to a certain extent staffing can affect the quality of care residents received. It was challenging to give good quality of care if the facility was short staffed.
During an interview on 3/14/2025 at 9:32 AM, the Medical Director stated staffing is a challenge. The staffing could be better. Currently, the units have one aide for 20 residents, and 1 licensed practical nurse for 40 residents. The registered nurses helped with medication administration and were resident centered. The staffing morale was low, and this could affect staffing. The lack of adequate staff could affect the care of the residents.
10 NYCRR 415.13(a)(1)(i-iii)