Guilford Health Care Center




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Guilford Health Care Center has a Trust Grade of F, indicating poor performance with significant concerns about care quality. It ranks #341 out of 417 facilities in North Carolina, placing it in the bottom half statewide, and #18 out of 20 in Guilford County, meaning there are only a couple of local facilities that perform better. The facility's situation is worsening, with the number of issues increasing from 7 in 2024 to 14 in 2025. Staffing is rated poorly at 1 out of 5 stars, and although turnover is around the state average at 54%, there is less RN coverage than 81% of North Carolina facilities, which is concerning as RNs are crucial for identifying potential health issues. Specific incidents include failing to provide snacks to residents who reported hunger and a lack of cleanliness in food preparation areas, which could affect the safety and satisfaction of meals served to residents. While the quality measures rating of 4 out of 5 suggests some positive aspects, the overall picture shows serious weaknesses that families should consider.
- Trust Score
- F
- In North Carolina
- #341/417
- Safety Record
- Low Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 54% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ⚠ Watch
- $8,203 in fines. Higher than 76% of North Carolina facilities, suggesting repeated compliance issues.
- Skilled Nurses ⚠ Watch
- Each resident gets only 21 minutes of Registered Nurse (RN) attention daily — below average for North Carolina. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 34 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Below North Carolina average (2.8)
Significant quality concerns identified by CMS
Near North Carolina avg (46%)
Higher turnover may affect care consistency
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 34 deficiencies on record
Apr 2025
14 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0567
(Tag F0567)
Could have caused harm · This affected 1 resident
Based on staff and resident interviews, the facility failed to provide residents with access to their personal fund accounts for 2 of 2 residents reviewed for management of personal funds (Resident #1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interviews and record review, the facility failed to maintain accurate advance directive information...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0624
(Tag F0624)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, and interim Guardian and staff interviews, the facility failed to provide a safe and orderly discharge. ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview the facility failed to complete the comprehensive Minimum Data Set (MDS) assessment w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident #36 was admitted to the facility on [DATE] with diagnoses that included severe protein-calorie malnutrition, adult f...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, resident, and staff interview, the facility failed to create a person-centered baseline care plan and pr...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and Responsible Party and staff interviews, the facility failed to complete a smoking asses...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observations, and staff interviews, the facility failed to secure an indwelling catheter tubing to preve...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and staff and Registered Dietitian interviews, the facility failed to administer tube feedi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observation, and interviews with residents and staff, the facility failed to provide fluids in accordanc...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected multiple residents
Based on record review, and staff and resident interviews, the facility failed to act upon grievances that were reported by the Resident Council, resolve repeat grievances, and communicate the facilit...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, staff interviews, and record reviews, the facility failed to have a medication error rate of less than 5%...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on a lunch meal tray line observation, staff interviews and record review the facility failed to follow the approved menu when pureed bread was not served to 11 of 11 residents on a pureed diet,...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0809
(Tag F0809)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, resident and staff interviews, the facility failed to provide snacks when requested for 4 of 4 residents ...
Read full inspector narrative →
Jan 2024
7 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview, the facility failed to obtain orders related to an indwelling urinary catheter for 1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observation and staff interviews, the facility failed to provide food in the form prescribed by the phys...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected multiple residents
Based on record review, and interviews with residents and staff, the facility failed to resolve group concerns (new and repeat concerns) reported during Resident Council meetings for 6 of 6 consecutiv...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observations and staff interviews, the facility failed to date opened multi-dose vials of insulin medication in 1 of 5 medication administration carts (100 hall), discard loose pills in the m...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, and staff interviews the facility failed to honor the food preferences for 4 of 10 residen...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations and staff interviews, the facility failed to keep food preparation areas, food service equipment clean, free from debris, grease buildup, and/or dried spills during two kitchen o...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected most or all residents
Based on observations, resident and staff interviews and record review, the facility's quality assurance (QA) process failed to implement, monitor, and revise as needed the action plan developed for t...
Read full inspector narrative →
Nov 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews, staff interviews, and interviews with the Nurse Practitioner, the facility failed to maintain complete ...
Read full inspector narrative →
Jun 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on record review and staff interviews the facility failed to report an allegation of abuse to the state agency within 2 hours for Resident #1. This was evident for 1 of 3 alleged abuse investiga...
Read full inspector narrative →
Mar 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observations, interviews with residents and staff, the facility failed to protect a resident's right to ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on resident interview, staff interviews and family interview, the facility failed to complete a thorough investigation and...
Read full inspector narrative →
Jan 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0687
(Tag F0687)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, resident interview, staff interview and record reviews, the facility failed to provide foot care and arra...
Read full inspector narrative →
Dec 2022
8 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews with staff and the Wound Care Nurse Practitioner (NP), the facility failed to schedule con...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, resident, staff interviews and record review, the facility failed to apply left hand splint for 2 of 2 re...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected 1 resident
Based on record review, staff and administration interviews the facility failed to have a Registered Nurse scheduled for 8 consecutive hours a day for 2 (11/26/22 and 11/27/22) of 30 days reviewed.
F...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, staff interviews, and record review, the facility failed to have a medication error rate of less than 5% ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff and dispensing pharmacist telephone interviews and record reviews, the facility failed to acquire a medication or...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observations, staff interviews and record reviews, the facility failed to: 1) Discard expired medications stored in 3 of 3 medication (med) carts observed (200 Middle Hall Med Cart; 200 High ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected multiple residents
Based on observations, resident and staff interview and record review, the facility's quality assurance and performance improvement (QAPI) process failed to implement, monitor, and revise as needed th...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations and staff interviews, the facility failed to keep food preparation areas, food storage areas and food service equipment clean, free from debris, grease buildup, and/or dried spil...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • 34 deficiencies on record. Higher than average. Multiple issues found across inspections.
- • Grade F (38/100). Below average facility with significant concerns.
About This Facility
What is Guilford Health Care Center's CMS Rating?
CMS assigns Guilford Health Care Center an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within North Carolina, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Guilford Health Care Center Staffed?
CMS rates Guilford Health Care Center's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 54%, compared to the North Carolina average of 46%.
What Have Inspectors Found at Guilford Health Care Center?
State health inspectors documented 34 deficiencies at Guilford Health Care Center during 2022 to 2025. These included: 34 with potential for harm.
Who Owns and Operates Guilford Health Care Center?
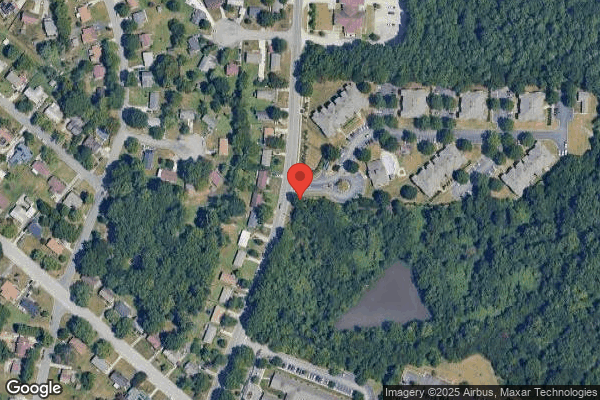
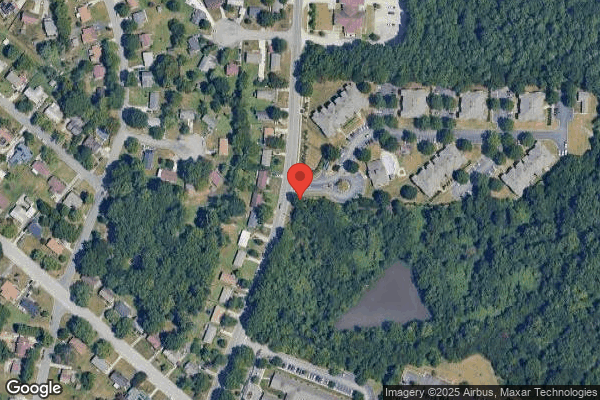
Guilford Health Care Center is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by LIFEWORKS REHAB, a chain that manages multiple nursing homes. With 110 certified beds and approximately 106 residents (about 96% occupancy), it is a mid-sized facility located in Greensboro, North Carolina.
How Does Guilford Health Care Center Compare to Other North Carolina Nursing Homes?
Compared to the 100 nursing homes in North Carolina, Guilford Health Care Center's overall rating (1 stars) is below the state average of 2.8, staff turnover (54%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Guilford Health Care Center?
Based on this facility's data, families visiting should ask: "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the below-average staffing rating.
Is Guilford Health Care Center Safe?
Based on CMS inspection data, Guilford Health Care Center has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in North Carolina. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Guilford Health Care Center Stick Around?
Guilford Health Care Center has a staff turnover rate of 54%, which is 8 percentage points above the North Carolina average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Guilford Health Care Center Ever Fined?
Guilford Health Care Center has been fined $8,203 across 2 penalty actions. This is below the North Carolina average of $33,161. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Guilford Health Care Center on Any Federal Watch List?
Guilford Health Care Center is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.