LAKEVIEW NURSING & REHAB


Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Lakeview Nursing & Rehab has a Trust Grade of C, which means it is average and ranks in the middle of the pack when compared to other facilities. It holds the #61 position out of 282 nursing homes in Oklahoma, placing it in the top half, and is the best option among the three facilities in McIntosh County. Unfortunately, the facility is worsening, with the number of identified issues increasing from 2 in 2023 to 3 in 2025. Staffing is a concern here, with a rating of 2 out of 5 stars and less RN coverage than 85% of other facilities, although the staff turnover rate is impressively low at 0%. While there have been no fines reported, and the overall health inspection score is good, specific incidents such as a resident falling from bed multiple times without adequate updates to their care plan and unsanitary food preparation practices raise significant concerns about the quality of care.
- Trust Score
- C
- In Oklahoma
- #61/282
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ○ Average
- Turnover data not reported for this facility.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Oklahoma facilities.
- Skilled Nurses ⚠ Watch
- Each resident gets only 10 minutes of Registered Nurse (RN) attention daily — below average for Oklahoma. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 22 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 22 deficiencies on record
Feb 2025
3 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure a referral to the LOCEU was made when a resident had a diagnosis of a serious mental illness for one (#30) of 2 sampled residents re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to ensure an insulin vial was cleaned prior to administration for 1 (#27) of 1 sampled resident observed for insulin administrat...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure the deep fryer was clean and free of food particles and the splash guard on side of stove was cleaned routinely.
The a...
Read full inspector narrative →
Oct 2023
2 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observation, and interview, the facility failed to assist a resident with ADLs for one (#18) of 12 resid...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on record review, observation, and interview, the facility failed to prepare and distribute food under sanitary conditions.
The Resident Census and Conditions of Residents report documented 38 r...
Read full inspector narrative →
Jul 2022
17 deficiencies
1 IJ (1 affecting multiple)
CRITICAL
(K)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Res #30 had diagnoses which included dementia with behavioral disturbance, bladder cancer, and diabetes.
A quarterly residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to complete a significant change assessment after a resident decline for one (#12) of 21 sampled residents whose assessments were reviewed.
T...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
MDS Data Transmission
(Tag F0640)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to transmit resident assessments to the CMS system within 14 days of c...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on record review, observation, and interview, the facility failed to ensure a resident with urinary incontinence did not continue to have a urinary catheter after a hospitalization without a cli...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on record review, observation, and interview, the facility failed to assess and monitor for pain every shift according to the plan of care for one (#26) of one resident reviewed for pain.
The R...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
Based on record review, observation, and interview, the facility failed to ensure an assessment for risk of entrapment was conducted and an informed consent and physician order was obtained prior to i...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on record review, observation, and interview, the facility failed to reduce a medication which had been identified by the pharmacist consultant as appropriate for reduction and the physician agr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure meals from the kitchen were prepared, served, and stored, in a sanitary manner for 50 of 50 residents who received their meals from th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0909
(Tag F0909)
Could have caused harm · This affected 1 resident
Based on record review, observation, and interview, the facility failed to conduct regular inspections of beds, side rails, and mattresses, to identify any areas of potential entrapment for one (#30) ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Res #42 was admitted to the facility with diagnoses which included diabetes mellitus and hypertension.
A history and physical...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected multiple residents
Based on record review and interview the facility failed to provide letters of NOMNC and/or ABN for two (#12 and #21) of three residents reviewed Beneficiary Notices.
The Beneficiary Notice - Resident...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Res #30 had diagnoses which included dementia with behavioral disturbance, anxiety, major depressive disorder, schizophrenia,...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
3. Res #35 had diagnoses which included recurrent major depressive disorder, borderline personality disorder, Parkinson's disease, hypertension, tremor, insomnia, and chronic pain.
The quarterly asses...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. Res #30 had diagnoses which included dementia with behavioral disturbance, bladder cancer, and diabetes.
A quarterly assessm...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
2. Res #40 had diagnoses which included insomnia, bipolar disorder, PTSD, and depression.
A MRR, dated 07/26/21, requested an end date or medical justification for as needed Vistaril (an antianxiety ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
Based on record review, observation, and interview, the facility failed to monitor for target behaviors and side effects and failed to act on a MRR request for reduction for one (#15) of five sampled ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation and interview, it was determined the facility failed to ensure the removal of expired medications and supplies from the medication storage room.
This had the potential to affect a...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most Oklahoma facilities.
- • Multiple safety concerns identified: 1 life-threatening violation(s). Review inspection reports carefully.
- • 22 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • Grade C (58/100). Below average facility with significant concerns.
About This Facility
What is Lakeview Nursing & Rehab's CMS Rating?
CMS assigns LAKEVIEW NURSING & REHAB an overall rating of 4 out of 5 stars, which is considered above average nationally. Within Oklahoma, this rating places the facility higher than 99% of the state's 100 nursing homes. This rating reflects solid performance across the metrics CMS uses to evaluate nursing home quality.
How is Lakeview Nursing & Rehab Staffed?
CMS rates LAKEVIEW NURSING & REHAB's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes.
What Have Inspectors Found at Lakeview Nursing & Rehab?
State health inspectors documented 22 deficiencies at LAKEVIEW NURSING & REHAB during 2022 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death) and 21 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Lakeview Nursing & Rehab?
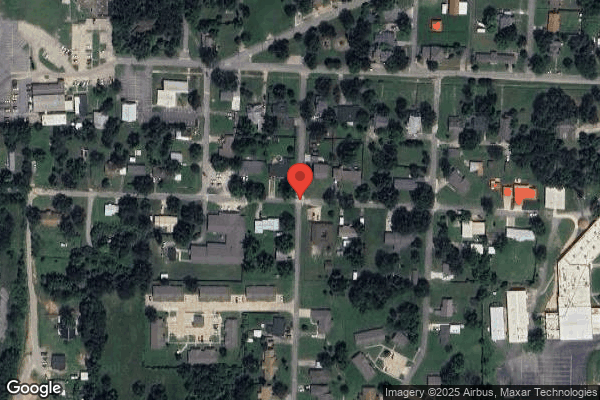
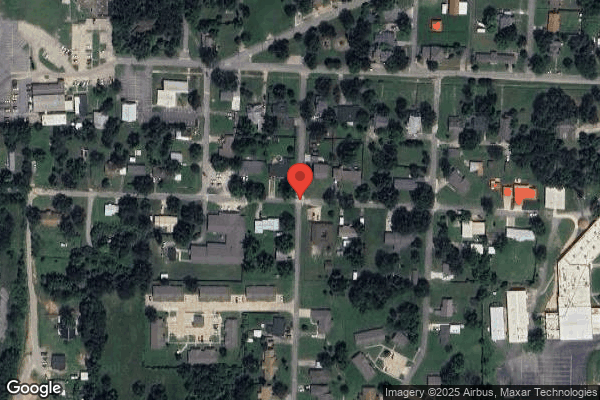
LAKEVIEW NURSING & REHAB is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by BRADFORD MONTGOMERY, a chain that manages multiple nursing homes. With 70 certified beds and approximately 57 residents (about 81% occupancy), it is a smaller facility located in EUFAULA, Oklahoma.
How Does Lakeview Nursing & Rehab Compare to Other Oklahoma Nursing Homes?
Compared to the 100 nursing homes in Oklahoma, LAKEVIEW NURSING & REHAB's overall rating (4 stars) is above the state average of 2.6 and health inspection rating (4 stars) is above the national benchmark.
What Should Families Ask When Visiting Lakeview Nursing & Rehab?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's Immediate Jeopardy citations and the below-average staffing rating.
Is Lakeview Nursing & Rehab Safe?
Based on CMS inspection data, LAKEVIEW NURSING & REHAB has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 4-star overall rating and ranks #1 of 100 nursing homes in Oklahoma. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Lakeview Nursing & Rehab Stick Around?
LAKEVIEW NURSING & REHAB has not reported staff turnover data to CMS. Staff turnover matters because consistent caregivers learn residents' individual needs, medications, and preferences. When staff frequently change, this institutional knowledge is lost. Families should ask the facility directly about their staff retention rates and average employee tenure.
Was Lakeview Nursing & Rehab Ever Fined?
LAKEVIEW NURSING & REHAB has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Lakeview Nursing & Rehab on Any Federal Watch List?
LAKEVIEW NURSING & REHAB is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.