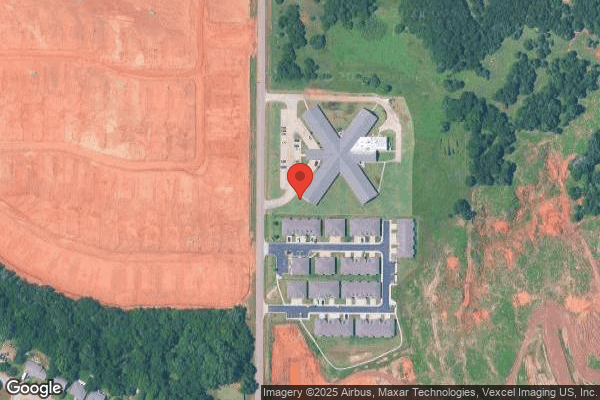
Noble Health Care Center
Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Noble Health Care Center has received a Trust Grade of F, indicating poor performance with significant concerns regarding care quality. Ranking #250 out of 282 facilities in Oklahoma places them in the bottom half of all nursing homes in the state, and #9 out of 10 in Cleveland County means there is only one local option that is better. While the facility is showing signs of improvement, having reduced issues from 14 in 2024 to 2 in 2025, their overall health inspection and staffing ratings are both at a concerning 1 out of 5 stars. Staffing turnover is average at 59%, which is close to the state average, but there have been serious and concerning incidents reported, such as failing to protect residents from abuse and maintaining cleanliness in the kitchen and living areas. On a positive note, the facility has not incurred any fines, which is a good sign, but families should weigh these strengths against the weaknesses highlighted in the inspector findings.
- Trust Score
- F
- In Oklahoma
- #250/282
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 59% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Oklahoma facilities.
- Skilled Nurses ⚠ Watch
- Each resident gets only 13 minutes of Registered Nurse (RN) attention daily — below average for Oklahoma. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 54 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Oklahoma average (2.6)
Significant quality concerns identified by CMS
13pts above Oklahoma avg (46%)
Frequent staff changes - ask about care continuity
Part of a multi-facility chain
Ask about local staffing decisions and management
11 points above Oklahoma average of 48%
The Ugly 54 deficiencies on record
Jun 2025
1 deficiency
1 Harm
SERIOUS
(H)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to ensure residents were free from abuse for 4 (#1, #2, ...
Read full inspector narrative →
Jan 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to perform weekly skin assessments for one (#4) of three sampled residents reviewed for skin assessment and monitoring.
The BOM identified 78 ...
Read full inspector narrative →
Dec 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure staff used infection control measures when getting ice for a resident (name unknown).
The DON reported 74 residents resided in the fac...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to ensure housekeeping services maintained a clean environment.
The DON ...
Read full inspector narrative →
Aug 2024
12 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to promote resident dignity by staff standing over residents while assisting them to eat.
The administrator identified 81 residents resided in t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure residents were offered the choice to formulate an advanced d...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure resident assessments were accurately coded on two of the MDS...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, and interview, the facility failed to complete neurological checks per protocol after an unwitnessed fal...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to obtain a physician order for the placement of a foley...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to supervise a resident while administering a breathing treatment for one (#49) of one sampled residents reviewed for respirator...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure psychotropic medications were monitored for target behaviors and side effects for one (#28) of five sampled residents reviewed for u...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to assess, monitor, and intervene for:
A. a resident who...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to ensure food was palatable and served at appetizing temperatures durin...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure food items were labeled, dated, and stored according to the facility policy.
The administrator identified 80 residents...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, and interviews the facility failed to follow their enhanced barrier precautions while prov...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to maintain an antibiotic stewardship program and infection surveillance to monitor antibiotic use for residents from April 2024 through June ...
Read full inspector narrative →
Jul 2023
15 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on record review, observation, and interview, the facility failed to ensure a resident did not self administer medications without a physician order for one (#59) of one sampled resident observe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to notify the Office of the State Long-Term Care Ombudsman of resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to refer a resident with a new diagnosis of possible serious mental il...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to update the care plan with fall interventions for one (#1) of one resident sampled for falls.
The Resident Census and Conditio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure residents were bathed as scheduled for one (#125) of one sampled resident reviewed for bathing.
The Resident Census and Conditions ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure timely physician response to monthly pharmacy medication regimen reviews for one (#38) of five residents sampled for unnecessary med...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to ensure staff were seated while providing feeding assi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to ensure resident electronic medical records were kept confidential during medication pass.
The Resident Census and Conditions of Residents for...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to:
a. change nebulizer tubing according to physician or...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure medications were administered according to physician orders for one (#20) of three residents sampled for medication pa...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure medication error rate was less than 5%. A total of 27 opportunities were observed with 11 errors. Total medication err...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to ensure:
a. expired supplies and medications were disposed of,
b. a medication label accurately documented the physician order for one (#20) o...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Laboratory Services
(Tag F0770)
Could have caused harm · This affected multiple residents
2. Res #38 had diagnoses which included hypothyroidism and hypertension.
A physician order, dated 03/25/21, documented to collect a thyroid cascade profile laboratory study every 12 months in January ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to ensure proper hand hygiene was performed during medication administration.
The Resident Census and Conditions of Residents form documented 30...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation and interview, the facility failed to ensure:
a. the kitchen was kept clean and maintained in good repair,
b. food products were properly thawed,
c. soiled/damp cloths were proper...
Read full inspector narrative →
May 2023
5 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure an allegation of abuse was reported to the state regulatory agency no later than two hours after the allegation was made for one (#2...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure an allegation of abuse had been thoroughly investigated for one (#2) of three sampled residents reviewed for abuse.
The Resident Cen...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure medication records were accurate for one (#1) of three sampled residents reviewed for accurate records.
The Resident Census and Cond...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to ensure:
a. orders for wound care were obtained for on...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
2. Res #3 had diagnoses which included hypertension.
A physician order, dated 04/27/23, documented to administer atenolol 75 mg one time per day, hold if systolic blood pressure less than 105 or diast...
Read full inspector narrative →
Dec 2022
5 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure a sink was securely affixed to the wall for two (#1 and #2) of seven residents sampled for environment.
The Resident Census and Condit...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to notify the physician of high blood sugar levels for two (#2 and #4) of three sampled residents reviewed for medications.
The DON identified...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Res #6 admitted to the facility on [DATE] and had diagnoses which included peripheral vascular disease and right below the kn...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based of record review and interview, the facility failed conduct regular weekly skin assessments, provide wound consults as ord...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to ensure medications were accurately administered for one (#1) of three residents sampled for medication administration.
The Resident Census ...
Read full inspector narrative →
Dec 2021
13 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a dependent resident was not transported and left at his hom...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to notify OSDH within two hours of an allegation of abuse for two (#13 and #79) of three resident sampled for abuse.
The Resident Census and ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected multiple residents
Based on record review and interviews, the facility failed to act upon grievances presented to staff during resident council meetings.
The Resident Census and Conditions of Residents report, dated 11...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. Res #47 had diagnoses that included COPD, fibromyalgia, obesity, and pain.
A bath list, revised 06/03/21, documented the resi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Res #12 had diagnoses to include unspecified dysphagia, GERD, and vitamin deficiency.
A physician order, dated 09/18/19, documen...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to provide supplements as ordered for one (#12) of two sampled residents reviewed for nutrition.
The Resident Census and Condit...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
2. Res #6 had diagnoses which chronic respiratory failure with hypoxia, chronic diastolic heart failure, dependence on supplemental oxygen and COPD.
A physician order, dated 03/21/20, documented the r...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected multiple residents
2. Res #24 had diagnoses which included articular cartilage disorders of right shoulder, pain, and post-polio syndrome,
A quarterly assessment, dated 09/12/21, documented the resident was cognitively...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
5. Resident council meeting minutes, dated 09/03/21, documented the residents stated the facility needed more CNAs and the weekends were bad.
Resident council meeting minutes, dated 10/01/21, documen...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5. Res #85 was admitted to the facility on [DATE] with diagnoses which included chronic pain, diabetes mellitus, intervertebral ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to provide food that accommodates residents' preferences for seven (#12,14, 33, 47, 61, 70, and #79) seven residents sampled for...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0809
(Tag F0809)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to provide meals in a timely manner.
The Resident Census and Conditions of Residents identified 95 residents who resided in the...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to maintain the kitchen in good repair and clean.
The RD identified 94 residents received services from the kitchen.
Findings:
On 11/30/21 at 8...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What safeguards are in place to prevent abuse and neglect?"
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most Oklahoma facilities.
- • Multiple safety concerns identified: Federal abuse finding, 1 harm violation(s). Review inspection reports carefully.
- • 54 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • Grade F (15/100). Below average facility with significant concerns.
- • 59% turnover. Above average. Higher turnover means staff may not know residents' routines.
About This Facility
What is Noble Health Care Center's CMS Rating?
CMS assigns Noble Health Care Center an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Oklahoma, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Noble Health Care Center Staffed?
CMS rates Noble Health Care Center's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 59%, which is 13 percentage points above the Oklahoma average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs. RN turnover specifically is 60%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Noble Health Care Center?
State health inspectors documented 54 deficiencies at Noble Health Care Center during 2021 to 2025. These included: 1 that caused actual resident harm and 53 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Noble Health Care Center?
Noble Health Care Center is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility is operated by STONEGATE SENIOR LIVING, a chain that manages multiple nursing homes. With 110 certified beds and approximately 80 residents (about 73% occupancy), it is a mid-sized facility located in Noble, Oklahoma.
How Does Noble Health Care Center Compare to Other Oklahoma Nursing Homes?
Compared to the 100 nursing homes in Oklahoma, Noble Health Care Center's overall rating (1 stars) is below the state average of 2.6, staff turnover (59%) is significantly higher than the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Noble Health Care Center?
Based on this facility's data, families visiting should ask: "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" These questions are particularly relevant given the substantiated abuse finding on record, the facility's high staff turnover rate, and the below-average staffing rating.
Is Noble Health Care Center Safe?
Based on CMS inspection data, Noble Health Care Center has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Oklahoma. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Noble Health Care Center Stick Around?
Staff turnover at Noble Health Care Center is high. At 59%, the facility is 13 percentage points above the Oklahoma average of 46%. Registered Nurse turnover is particularly concerning at 60%. RNs handle complex medical decisions and coordinate care — frequent RN changes can directly impact care quality. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Noble Health Care Center Ever Fined?
Noble Health Care Center has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Noble Health Care Center on Any Federal Watch List?
Noble Health Care Center is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.