CORVALLIS MANOR




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Corvallis Manor has a Trust Grade of F, indicating significant concerns about the quality of care provided. Ranking #111 out of 127 facilities in Oregon places it in the bottom half, while being the only option in Benton County means families have no local alternatives. The facility's trend is worsening, with a troubling increase in issues from 6 in 2024 to 27 in 2025. Staffing is average with a 3/5 star rating and a turnover rate of 58%, which is close to the state average of 49%, while RN coverage is also average. However, the facility has incurred $345,051 in fines, concerning as it is higher than 96% of Oregon facilities, suggesting ongoing compliance issues. Critical incidents include a resident who died after being administered 100 mg of oxycodone instead of the prescribed 5 mg, and another resident whose respiratory decline was not reported, leading to hospitalization and death. These findings highlight serious weaknesses in medication management and monitoring.
- Trust Score
- F
- In Oregon
- #111/127
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 58% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $345,051 in fines. Lower than most Oregon facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 38 minutes of Registered Nurse (RN) attention daily — about average for Oregon. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 81 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Below Oregon average (3.0)
Significant quality concerns identified by CMS
12pts above Oregon avg (46%)
Frequent staff changes - ask about care continuity
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
10 points above Oregon average of 48%
The Ugly 81 deficiencies on record
Apr 2025
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to check the Hoyer (a mechanical lift device used to transfer residents) straps to prevent a fall and failed to ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to report injuries of unknown origin for 1 of 5 sampled residents (#10) reviewed for abuse reporting. This placed residents a...
Read full inspector narrative →
Mar 2025
23 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility failed to assess a resident for safe self-administration of medication for 1 of 1 sampled resident (#50) reviewed for anticoagulant medic...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to provide a clean environment as well as functioning phones and lights for 2 of 6 sampled residents (#s 33 and 174) reviewed...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure grievances were acted upon timely for 1 of 5 sampled residents (#14) reviewed for dignity and missing property. Thi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to incorporate PASARR (Preadmission Screening and Resident Review) Level II recommendations for 1 of 1 sampled r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
2. Resident 124 was admitted to the facility in 3/2025 with a diagnosis of diabetes.
A 3/5/25 nursing Admission/readmission Evaluation form revealed Resident 124 was cognitively intact and required e...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to follow physician orders for treatment of a resident's pressure ulcer for 1 of 5 sampled residents (#20) reviewed for medic...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0687
(Tag F0687)
Could have caused harm · This affected 1 resident
Based on interview, and record review it was determined the facility failed to provide appropriate foot care for 1 of 2 sampled residents (#s 22) reviewed for skin. This placed residents at risk for i...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review it was determined the facility failed to ensure resident water temperatures were safe for 3 of 6 sampled residents (#s 2, 10, and 17) and 1 of 1 ther...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review it was determined the facility failed to assess a resident's ability to self-catheterize (sterile tube inserted into the bladder through the urethra ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to ensure accurate communication occurred between the...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0699
(Tag F0699)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure a resident who was a history of trauma received trauma-informed care for 1 of 1 sampled resident (#22)...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review it was determined the facility failed to ensure a resident's use of bed rails was assessed for 1 of 1 sampled resident (#124) reviewed for side rails...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0742
(Tag F0742)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure recommended mental health services were provided for 1 of 5 sampled residents (#18) reviewed for unnecessary medica...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to provide timely pharmaceutical services for 1 of 1 ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to provide appropriate monitoring and dosing of medic...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to complete a GDR (gradual dose reduction) and appropriately monitor a resident on psychotropic medications for 2 of 5 sample...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0773
(Tag F0773)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to promptly notify the ordering physician of laboratory results for 1 of 1 sampled residents (#37) reviewed for ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0775
(Tag F0775)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure lab results were in the resident record for 1 of 5 sampled residents (#10) reviewed for medications. This placed re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review it was determined the facility failed to make reasonable efforts to deliver a menu based on resident requests and preferences for 2 of 2 residents (#...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review it was determined the facility failed to follow infection control standards for contact and Enhanced Barrier Precautions for 3 of 7 sampled residents...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to provide antibiotic stewardship for 1 of 1 sampled resident (#25) reviewed for UTIs. This placed residents at risk for drug...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident 14 was admitted to the facility in 2/2025 with a diagnosis of diabetes.
Per epocrates (online pharmacy resource) re...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Resident 61 was admitted to the facility in 12/2024 with diagnoses including diabetes and protein-calorie malnutrition.
On 3/...
Read full inspector narrative →
Jan 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to provide modified textured diets as ordered for 2 of 3 sampled residents (#s 1 and 2 ) reviewed for food. This...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review it was determined the facility failed to maintain essential kitchen equipment for 1 of 1 kitchen reviewed for kitchen services. This placed residents...
Read full inspector narrative →
Nov 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview it was determined the facility failed to provide maintenance services to maintain a safe, com...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review it was determined the facility failed to ensure sufficient nursing staff to maintain the highest practicable physical and psychosocial well-being for ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review it was determined meals were not served at the proper temperature for 1 of 1 kitchens reviewed for meal service. This placed residents at risk for foo...
Read full inspector narrative →
Sept 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure the resident's right to be free from neglect for 1 of 3 sampled residents (#1) reviewed for abuse. This placed resi...
Read full inspector narrative →
Jun 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to obtain consent and review risks and benefits prior to administering a COVID-19 vaccination to 1 of 3 sampled residents (#9...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on interview and record review it was determined the facility failed to staff a RN for eight consecutive hours per day seven days per week for 22 out of 91 days reviewed for staffing. This place...
Read full inspector narrative →
Dec 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined Staff 5 (Agency RN) failed to follow standards of practice related to insulin administration and failed to be honest during an investigation for ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure a resident was free from a significant medication error for 1 of 3 sampled residents (#2) reviewed for medications....
Read full inspector narrative →
Dec 2023
28 deficiencies
3 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
2. Resident 20 was admitted to the facility in 2022 with diagnosis of Parkinson's disease (A progressive disorder which affects the nervous system).
A 11/2023 MAR instructed staff to administer carbid...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident 66 was admitted to the facility in 2023 with diagnosis of sepsis (infection in the blood).
A 11/14/23 admission MDS ...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0692
(Tag F0692)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review it was determined the facility failed to maintain acceptable parameters of nu...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review it was determined the facility failed to provide a comfortable shower chair for 1 of 9 sampled residents (#14) reviewed for ADLs. This placed residen...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review it was determined the facility failed to provide a homelike environment for 1 of 1 facility reviewed for environment. This placed residents at risk f...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure a resident grievance was resolved timely for 1 of 3 sampled residents (#375) reviewed for nutrition. This placed re...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure a resident or resident representative was provided a bed hold policy for 1 of 1 sampled resident (#63) reviewed for...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident 21 was admitted to the facility in 2023 with diagnoses including pneumonia, COPD (difficulty or discomfort with brea...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review it was determined the facility failed to develop care plans for 2 of 7 sampled residents (#s 6 and 375) reviewed for pain and accidents. This placed ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure care plans were updated for 2 of 2 sampled residents (#s 8 and 11) reviewed for dialysis (process to p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to obtain eye care services for 1 of 1 sampled resident (#8) reviewed for vision. This placed residents at risk ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review it was determined the facility failed to ensure a resident's environment remained free from accident hazards for 1 of 4 sampled residents (#20) revie...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review it was determined the facility failed to ensure resident's respiratory equipment was maintained for 2 of 3 sampled residents (#s 21 and 225) reviewed...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure a resident was offered pain medication when assessed to have pain for 1 of 3 sampled residents (#375) reviewed for ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0744
(Tag F0744)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to comprehensively assess dementia needs for 1 of 2 sampled residents (#23) reviewed for dementia. This placed residents at r...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0773
(Tag F0773)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure a resident's physician was notified of abnormal laboratory results for 1 of 5 sampled residents (#375) reviewed for...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0940
(Tag F0940)
Could have caused harm · This affected 1 resident
Based on interview, and record review it was determined the facility failed to have an effective new staff orientation program for 2 of 3 staff members (#s 12 and 13) reviewed for staffing and orienta...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to provide a response for Resident Council concerns for 1 of 1 Resident Council reviewed for grievances. This placed resident...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
4. Resident 14 was admitted to the facility in 2022 with diagnoses including stroke and heart failure.
The 8/4/22, 5/4/23, 8/17/23 and 10/24/23 IDT (Interdisciplinary Team) Care Plan Conference and W...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident 6 was admitted to the facility in 2023 with a diagnosis including depression.
A 11/2/23 admission MDS indicated Resi...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review it was determined the facility failed to provide sufficient staffing to meet the needs of 1 of 8 sampled residents (#36) and 1 of 1 facility reviewed...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to ensure CNA staff annual performance reviews were completed for 5 of 5 sampled CNA staff (#s 8, 21, 22, 23, and 24) reviewe...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
3. Resident 46 was admitted to the facility in 2020 with diagnoses including stroke and schizoaffective disorder (a mental health disorder with combination of schizophrenia symptoms, such as hallucina...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
4. Resident 20 was admitted to the facility in 2022 with diagnosis of Parkinson's disease (a progressive disorder which affects the nervous system).
A 9/21/23 signed physician orders instructed staff ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review it was determined the facility failed to ensure proper flavor and appealing food textures for 1 of 1 kitchen and 1 of 13 sampled residents (#8) obser...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to ensure resident records were accurate for 3 of 17 sampled residents (#s 8, 14, and 66) reviewed for ADLs, dialysis, nutrit...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 6. Resident 228 was admitted to the facility on [DATE] with diagnoses including kidney disease and dementia.
A 11/27/23 Skilled...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected multiple residents
Based on interview, and record review it was determined the facility failed to have a system in place to track annual nurse aide training for the required 12 hours of in-service training annually for ...
Read full inspector narrative →
Oct 2023
2 deficiencies
2 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0658
(Tag F0658)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to provide care and services in compliance with profe...
Read full inspector narrative →
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0760
(Tag F0760)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on Based on interview and record review it was determined the facility failed to ensure narcotic pain medication was admin...
Read full inspector narrative →
Sept 2023
1 deficiency
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Respiratory Care
(Tag F0695)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to recognize and respond to Resident 2's respiratory ...
Read full inspector narrative →
Jul 2023
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to identify and report a potential violation of mistreatment for 1 of 3 sampled residents (#204) reviewed for accidents. This...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure a thorough investigation was completed in a timely manner for an unwitnessed fall with serious injury for 1 of 1 sa...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to ensure Staff 7 (CNA) provided transfer assistance ...
Read full inspector narrative →
Nov 2022
12 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure resident grievances were addressed for 1 of 1 sampled resident (#35) reviewed for personal property. This placed re...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to develop a comprehensive care plan for 1 of 5 sampled residents (#30) reviewed for medication. This placed residents at ris...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
2. Resident 64 was admitted to the facility in 8/2022 with diagnoses including lung disease and dementia.
An 8/10/22 physician order indicated staff were to apply one nicotine patch in the morning an...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
3. Resident 5 admitted to the facility in 2/2022 with diagnoses including neurogenic bladder (lack of bladder control caused by nerve damage) and quadriplegia (paralysis of all four limbs).
A revised ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to provide dialysis services and medications for 1 of 1 sampled resident (#45) reviewed for dialysis. This place...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
3. Resident 10 was admitted to the facility in 6/2021 with diagnoses including diabetes.
On 11/1/22 at 10:29 AM a review of the resident's clinical record revealed no documentation related to advance ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to ensure the daily staff posting was accurate for 31 of 31 days reviewed for sufficient staffing. This placed residents at r...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to ensure narcotic drug records were reconciled for 4 of 4 narcotic books reviewed for medication administration. This placed...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review it was determined the facility failed to ensure the medication error rate was less than 5 percent. There were 25 medication administration opportuniti...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
Based on observation and interview it was determined the facility failed to provide meals with an appetizing appearance and temperature for 4 for 4 sampled residents (#s 10, 19, 23 and 68) reviewed fo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review it was determined the facility failed to follow infection control standards for COVID-19 for 1 of 1 facility reviewed for infection control. This plac...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
Based on observation and interview it was determined the facility failed to ensure flooring was in safe, sanitary and homelike conditions in resident rooms for three of three facility hallways reviewe...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 3 life-threatening violation(s), Special Focus Facility, 4 harm violation(s), $345,051 in fines, Payment denial on record. Review inspection reports carefully.
- • 81 deficiencies on record, including 3 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • $345,051 in fines. Extremely high, among the most fined facilities in Oregon. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Corvallis Manor's CMS Rating?
CMS assigns CORVALLIS MANOR an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Oregon, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Corvallis Manor Staffed?
CMS rates CORVALLIS MANOR's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 58%, which is 12 percentage points above the Oregon average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs. RN turnover specifically is 69%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Corvallis Manor?
State health inspectors documented 81 deficiencies at CORVALLIS MANOR during 2022 to 2025. These included: 3 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 4 that caused actual resident harm, and 74 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
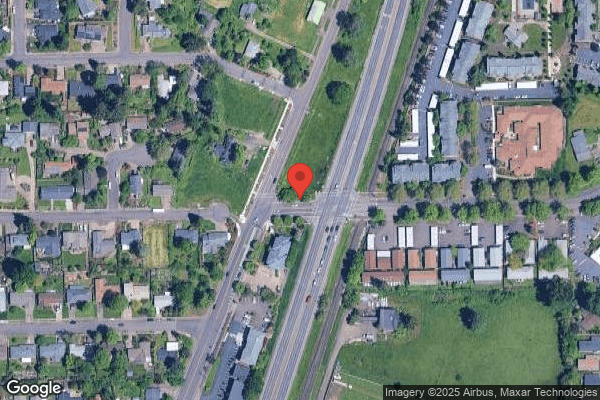
Who Owns and Operates Corvallis Manor?
CORVALLIS MANOR is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by VOLARE HEALTH, a chain that manages multiple nursing homes. With 135 certified beds and approximately 68 residents (about 50% occupancy), it is a mid-sized facility located in CORVALLIS, Oregon.
How Does Corvallis Manor Compare to Other Oregon Nursing Homes?
Compared to the 100 nursing homes in Oregon, CORVALLIS MANOR's overall rating (1 stars) is below the state average of 3.0, staff turnover (58%) is significantly higher than the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Corvallis Manor?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's Immediate Jeopardy citations and the facility's high staff turnover rate.
Is Corvallis Manor Safe?
Based on CMS inspection data, CORVALLIS MANOR has documented safety concerns. Inspectors have issued 3 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility is currently on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes nationwide). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Oregon. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Corvallis Manor Stick Around?
Staff turnover at CORVALLIS MANOR is high. At 58%, the facility is 12 percentage points above the Oregon average of 46%. Registered Nurse turnover is particularly concerning at 69%. RNs handle complex medical decisions and coordinate care — frequent RN changes can directly impact care quality. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Corvallis Manor Ever Fined?
CORVALLIS MANOR has been fined $345,051 across 5 penalty actions. This is 9.4x the Oregon average of $36,529. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Corvallis Manor on Any Federal Watch List?
CORVALLIS MANOR is currently an SFF Candidate, meaning CMS has identified it as potentially qualifying for the Special Focus Facility watch list. SFF Candidates have a history of serious deficiencies but haven't yet reached the threshold for full SFF designation. The facility is being monitored more closely — if problems continue, it may be added to the official watch list. Families should ask what the facility is doing to address the issues that led to this status.