HIGHLAND HOUSE NURSING & REHABILITATION CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Highland House Nursing & Rehabilitation Center has received a Trust Grade of F, indicating significant concerns about its quality of care. It ranks #89 out of 127 nursing homes in Oregon, placing it in the bottom half statewide, and #3 of 4 in Josephine County, meaning only one other local facility is rated lower. While the facility is improving, with issues decreasing from 31 in 2024 to just 4 in 2025, there are still serious concerns, including a critical incident of alleged sexual abuse involving a staff member. Staffing is a mixed bag; they have a below-average rating of 2 out of 5 stars and a staff turnover rate of 54%, which is around the state average. Additionally, the facility has concerning RN coverage, being below 89% of Oregon facilities, which may impact the quality of care, although they have good quality measures. Overall, families should weigh the facility's improvements against its serious past issues and current staffing challenges.
- Trust Score
- F
- In Oregon
- #89/127
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 54% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $36,852 in fines. Lower than most Oregon facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 20 minutes of Registered Nurse (RN) attention daily — below average for Oregon. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 65 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Below Oregon average (3.0)
Below average - review inspection findings carefully
Near Oregon avg (46%)
Higher turnover may affect care consistency
Above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 65 deficiencies on record
Apr 2025
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure residents were treated with respect and dignity for 1 of 6 sampled residents (#12) reviewed for abuse. This placed ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to accurately assess facility acquired pressure ulcers for 1 of 3 sampled residents (#11) reviewed for skin conditions. This ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to evaluate a potential unavoidable accident of a feeding tube being dislodged to prevent recurrence for 1 of 3 sampled resid...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure residents were free from significant medication errors for 1 of 4 sampled residents (#13) reviewed for medications....
Read full inspector narrative →
Aug 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure residents were free from sexual abuse for 2 of 3 sampled residents (#s 2 and 3) reviewed for abuse. This placed res...
Read full inspector narrative →
Jul 2024
1 deficiency
1 IJ (1 affecting multiple)
CRITICAL
(K)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected multiple residents
Based on interview and record review it was determined a facility employee sexually abused 6 of 10 sampled residents (#s 6, 7, 8, 9, 10 and 11) who were reviewed for sexual abuse. As a result of the p...
Read full inspector narrative →
Jun 2024
29 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
3. Resident 335 admitted to the facility on 6/2024 with diagnoses including dementia.
A 6/11/24 review of Resident 335's orders revealed a 6/7/24 order for quetiapine fumarate (an antipsychotic medica...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to notify a resident's representative of a fall for 1 of 2 sampled resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on observation and interview it was determined the facility failed to maintain privacy and confidentiality of resident records in 1 of 1 Social Services office. This placed residents at risk for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review it was determined the facility failed to assess the use of a physical restraint for 1 of 1 sampled resident (#57) reviewed for restraints. This place...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
2. Resident 91 was admitted to the facility in 8/2022 with diagnoses including intervertebral disc displacement of the spine.
An 8/19/22 MDS assessed Resident 91 as moderately cognitively impaired.
A ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to investigate for abuse for 1 of 6 sampled residents (#65) reviewed for dignity and respect. This placed residents at risk f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to comprehensively assess residents related to behaviors for 1 of 2 sampled residents (#25) reviewed for behavio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to document and conduct a Significant Change MDS assessment within the required timeframe for 1 of 2 sampled residents (#57) ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure residents were referred to the appropriate state-designated authority for a Level II PASARR (Pre-admission Screenin...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident 335 was admitted to the facility on [DATE] with diagnoses including left femur (thigh bone) fracture after a fall an...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility staff failed to follow professional standards of practice for a diagnosed mental disorder for 1 of 6 (#16) sampled residents reviewe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure a resident had glasses for 1 of 3 sampled residents (#20) reviewed for communication-sensory. This pla...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
3. Resident 63 was admitted to the facility in 2024 with diagnoses including falls and anxiety.
An 4/29/24 care plan indicated Resident 63 required a bedside commode for toileting.
The 5/13/24, 5/22/...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure nutritional supplements were provided for 1 of 3 sampled residents (#19) reviewed for nutrition. This placed reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, it was determined the facility failed to obtain orders for oxygen and clean a resident's oxygen equipment for 1 of 1 sampled resident (#51) reviewed...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident 339 admitted to the facility on [DATE] at 11:45 AM with diagnoses including left femur (thigh bone) fracture.
On 6/1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0699
(Tag F0699)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to ensure a resident who was a trauma survivor receiv...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0745
(Tag F0745)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure a resident was transported to dialysis for 1 of 1 sampled resident (#134) reviewed for dialysis. This placed reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review it was determined the facility failed to follow infection control standards for 1 of 5 halls (200 hall) reviewed for infection control. This placed r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure a resident was not administered an antibiotic without indication for 1 of 3 sampled residents (#86) reviewed for UT...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
4. Resident 95 admitted to the facility in 5/2023 with diagnoses including a femur (thigh) fracture.
Resident 95's 5/25/23 admission MDS assessed her/him as cognitively intact.
Review of an investigat...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
5. Resident 90 was admitted to the facility in 2023 with diagnosis of neck fracture.
A 7/5/23 at 1:27 AM Alert Note indicated Resident 90 was agitated and was kept up by the fireworks and one sounded ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to provide a written grievance resolution or communicate with a resident or resident's representative regarding the resolutio...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. Resident 21 was admitted to the facility on [DATE] with diagnoses including cervical vertebra (neck) fracture.
A 4/5/24 Compr...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
2. Resident 33 was admitted to the facility in 8/2021 with diagnoses including diabetes.
A physician order dated 1/16/24, indicated Resident 33 was to receive Senna (a laxative)two tablets two times d...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, it was determined the facility failed to post accurate and complete staffing information for 1 of 1 facility reviewed for staffing. This placed resi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
4. Resident 63 was admitted to the facility in 2024 with diagnoses including anxiety and asthma.
A pharmacy review dated 4/29/24 recommended following the use of Symbicort (inhaler medication) Residen...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on interview and record review it was it was determined the facility failed to ensure a medication error rate of less than 5%. The facility administration rate was 7.41% with two errors in 27 op...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to have a system in place to ensure CNA staff received 12 hours of in-service training annually for 3 of 5 randomly selected ...
Read full inspector narrative →
Mar 2023
20 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure residents were assessed for safe self-administration of medications for 1 of 1 sampled resident (#34) ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on interview and record review, it was determined the facility failed to protect the resident's right to be free from sexual abuse by Witness 3 (Alledged Perpetrator/Medical Transportation Drive...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to complete a thorough investigation of an allegation of abuse for 1 of 3 sampled residents (#54) reviewed for abuse. This pl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on interview and record review was determined the facility failed to ensure assessments accurately reflected the residents' status for 1 of 9 sampled residents (#30) reviewed for ADLs. This plac...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to ensure Staff 11 (Former Staff/RN) adhered to profe...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to provide bathing assistance to dependent residents for 2 of 7 sampled residents (#s 4 and 18) reviewed for ADLs. This place...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0687
(Tag F0687)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to provide routine diabetic foot care for 2 of 2 sampled residents (#s 10 and 34) reviewed for foot care. This p...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure respiratory equipment was properly maintained for 1 of 1 sampled resident (#30) reviewed for respirato...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure residents received dialysis services consistent with the care plan for 1 of 1 sampled residents (#18) reviewed for ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0745
(Tag F0745)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to identify potential trauma and monitor psychosocial...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to ensure residents were free from significant medica...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation and interview it was determined the facility failed to store treatment supplies in locked compartments for 1 of 1 treatment cart on 500 hall observed. This placed residents at ris...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview it was determined the facility failed to ensure staff wore and used PPE correctly for 1 of 1 ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to obtain copies and provide assistance to residents who expressed interest in formulating an advance directive for 3 of 7 sa...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. On 3/6/23 at 1:53 PM Resident 32's windowsill was observed to have four nails sticking up along the length of the windowsill ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Resident 34 was admitted to the facility in 9/2021 with diagnoses including diabetes and mild cognitive impairment.
A 10/5/21...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to ensure sufficient staffing to meet resident care needs for 4 of 5 halls (100, 200, 300 and 400) reviewed for staffing. Thi...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to ensure CNA staff annual performance reviews were completed for 4 of 4 sampled CNA staff (#s 7, 8, 9 and 10) reviewed for s...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to ensure the Direct Care Staff Daily Reports were complete for 10 of 33 days reviewed for staffing. This placed residents at...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review it was determined the facility failed to store food in accordance with professional standards for food service safety for 1 of 1 kitchen refrigerator ...
Read full inspector narrative →
Feb 2022
10 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to update care plans related to smoking status and resident preferences for 1 of 5 sampled residents (#29) reviewed for medic...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to follow orders related to insulin for 1 of 5 sampled residents (#47) reviewed for medications. This placed residents at ris...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure there was a signed agreement and ongoing communication and collaboration with the dialysis provider fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed adequately monitor resident medications for 1 of 5 sampled residents (#107) reviewed for medications. This placed residents a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure residents received adequate psychotropic medication monitoring for 1 of 5 sampled residents (#47) reviewed for medi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
On 1/28/22 at 7:58 AM Staff 18 (LPN) documented she administered Resident 52 artificial tears and fluticasone nasal spray, however she was not observed to administer the medications. Resident 52 refus...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0563
(Tag F0563)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review it was determined the facility failed to allow residents to have visitors for 5 of 10 sampled residents (#s 1, 23, 25, 26 and 41) reviewed for advance...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review it was determined the facility failed to provide activities on a routine basis for 1 of 1 sampled resident (#1) reviewed for choices and 1 of 1 facili...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to ensure accurate records and documentation related to medications, behaviors and smoking for 4 of 6 sampled residents (#s 6...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation and interview it was determined the facility failed to ensure 1 of 1 ice machine was plumbed correctly to prevent the backflow of contaminated matter into the ice machine. This pl...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 1 life-threatening violation(s), $36,852 in fines, Payment denial on record. Review inspection reports carefully.
- • 65 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $36,852 in fines. Higher than 94% of Oregon facilities, suggesting repeated compliance issues.
- • Grade F (33/100). Below average facility with significant concerns.
About This Facility
What is Highland House Nursing & Rehabilitation Center's CMS Rating?
CMS assigns HIGHLAND HOUSE NURSING & REHABILITATION CENTER an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Oregon, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Highland House Nursing & Rehabilitation Center Staffed?
CMS rates HIGHLAND HOUSE NURSING & REHABILITATION CENTER's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 54%, compared to the Oregon average of 46%. RN turnover specifically is 67%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Highland House Nursing & Rehabilitation Center?
State health inspectors documented 65 deficiencies at HIGHLAND HOUSE NURSING & REHABILITATION CENTER during 2022 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death) and 64 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Highland House Nursing & Rehabilitation Center?
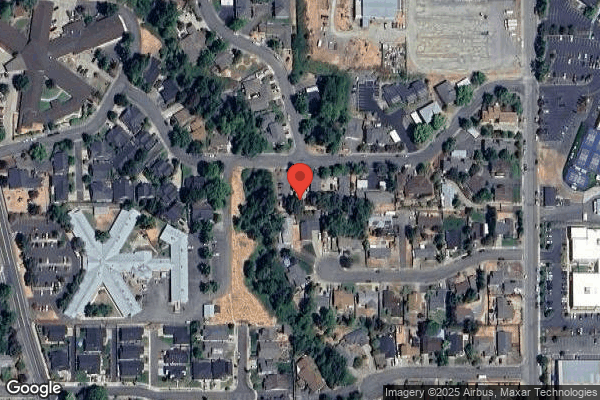
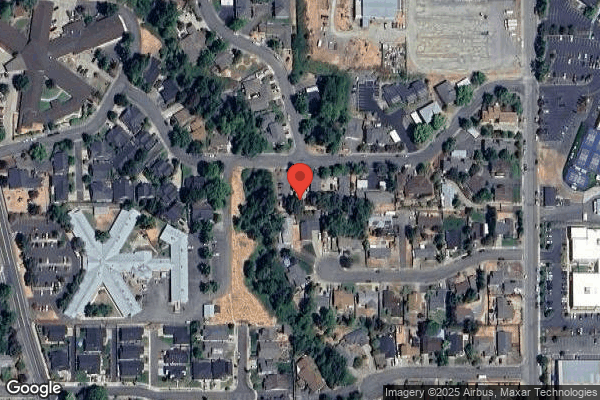
HIGHLAND HOUSE NURSING & REHABILITATION CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by VOLARE HEALTH, a chain that manages multiple nursing homes. With 119 certified beds and approximately 87 residents (about 73% occupancy), it is a mid-sized facility located in GRANTS PASS, Oregon.
How Does Highland House Nursing & Rehabilitation Center Compare to Other Oregon Nursing Homes?
Compared to the 100 nursing homes in Oregon, HIGHLAND HOUSE NURSING & REHABILITATION CENTER's overall rating (2 stars) is below the state average of 3.0, staff turnover (54%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Highland House Nursing & Rehabilitation Center?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's Immediate Jeopardy citations and the below-average staffing rating.
Is Highland House Nursing & Rehabilitation Center Safe?
Based on CMS inspection data, HIGHLAND HOUSE NURSING & REHABILITATION CENTER has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Oregon. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Highland House Nursing & Rehabilitation Center Stick Around?
HIGHLAND HOUSE NURSING & REHABILITATION CENTER has a staff turnover rate of 54%, which is 8 percentage points above the Oregon average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Highland House Nursing & Rehabilitation Center Ever Fined?
HIGHLAND HOUSE NURSING & REHABILITATION CENTER has been fined $36,852 across 1 penalty action. The Oregon average is $33,447. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Highland House Nursing & Rehabilitation Center on Any Federal Watch List?
HIGHLAND HOUSE NURSING & REHABILITATION CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.