MOUNTAIN LAUREL HEALTHCARE AND REHABILITATION CTR




Inspected within the last 6 months. Data reflects current conditions.
Mountain Laurel Healthcare and Rehabilitation Center has received a Trust Grade of F, indicating significant concerns about the quality of care provided. It ranks #609 out of 653 facilities in Pennsylvania, placing it in the bottom half, and #3 out of 4 in Clearfield County, meaning only one local option is worse. The facility is showing signs of improvement, with the number of issues decreasing from 18 in 2024 to 14 in 2025. Staffing is a relative strength, with a 4 out of 5 rating and a turnover rate of 35%, which is better than the state average. However, the facility has accumulated $98,690 in fines, which is concerning and indicates potential compliance issues. While staffing is a positive aspect, the facility has experienced serious incidents, such as failing to ensure a resident's safety in the bathroom, which led to a fall and a fracture. Additionally, the dining experience has not met residents' preferences, with some forced to eat in their rooms due to the main dining area being closed. The cleanliness and homelike environment of residents' rooms have also been criticized, with several rooms showing signs of neglect, such as torn and stained signs meant to prevent wandering. Overall, while there are some strengths, families should be aware of the significant weaknesses and past issues before making a decision.
- Trust Score
- F
- In Pennsylvania
- #609/653
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ○ Average
- 35% turnover. Near Pennsylvania's 48% average. Typical for the industry.
- Penalties ✓ Good
- $98,690 in fines. Lower than most Pennsylvania facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 25 minutes of Registered Nurse (RN) attention daily — below average for Pennsylvania. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 71 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (35%)
13 points below Pennsylvania average of 48%
Facility shows strength in staffing levels, quality measures, fire safety.
The Bad
Below Pennsylvania average (3.0)
Significant quality concerns identified by CMS
11pts below Pennsylvania avg (46%)
Typical for the industry
Well above median ($33,413)
Moderate penalties - review what triggered them
The Ugly 71 deficiencies on record
Aug 2025
14 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on review of policies and clinical records, as well as staff interviews, it was determined that the facility failed to ensure that the physician was notified timely about a change in condition f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0628
(Tag F0628)
Could have caused harm · This affected 1 resident
Based on clinical record review, as well as staff interviews, it was determined that the facility failed to notify the resident's representative in writing regarding the reason for transfer to the hos...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
Based on clinical record reviews and staff interviews, it was determined that the facility failed to ensure that physician's orders for enteral tube feedings (feeding through a tube inserted directly ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on a review of facility policies, clinical records, and staff interviews, it was determined that the facility failed to ensure that it was free from significant medication errors for one of 50 r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on review of policies, manufacturer's instructions and clinical records, as well as observations and staff interviews, it was determined that the facility failed to date an opened insulin pen in...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0807
(Tag F0807)
Could have caused harm · This affected 1 resident
Based on clinical record reviews and observations, as well as resident and staff interviews, it was determined that the facility failed to ensure that drink preferences were honored for 2 of 50 reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected 1 resident
Based on review of the facility's plans of correction for previous surveys, and the results of the current survey, it was determined that the facility's Quality Assurance Performance Improvement (QAPI...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected multiple residents
Based on observations and staff interviews, it was determined that the facility failed to provide a dining experience based upon resident's preference for 5 of 50 residents reviewed (Residents 46, 69,...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observations and staff interviews, it was determined that the facility failed to provide a clean and homelike environment in residents' rooms for six of 50 residents reviewed (Residents 23, 2...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected multiple residents
Based on review of clinical records and staff interviews, it was determined that the facility failed to ensure that proper care to prevent infection was provided for one of 50 residents reviewed (Resi...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on review of policies and clinical records, as well as staff interviews, it was determined that the facility failed to have sufficient nursing staff to provide showers as scheduled for 5 of 50 r...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
Based on clinical record reviews and staff interviews, it was determined that the facility failed to respond to a pharmacy recommendation for one of 50 residents reviewed (Resident 46) and failed to p...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on review of facility policies, as well as observations and staff interviews, it was determined that the facility failed to store and serve food in accordance with professional standards for foo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected multiple residents
Based on a review of a list of nurse aides currently employed by the facility, including their hire dates and training hours, as well as staff interviews, it was determined that the facility failed to...
Read full inspector narrative →
Sept 2024
15 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on a review of facility policies and clinical records, as well as observations and staff interviews, it was determined that the facility failed to protect the residents rights for one of 44 resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on review of facility policies, investigation reports, and clinical records, as well as staff interviews, it was determined that the facility failed to ensure that residents were free from abuse...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on review of clinical records, as well as staff interviews, it was determined that the facility failed to notify the state ombudsman and/or the resident and resident's responsible party in writi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on review of policies and clinical records, as well as staff interviews, it was determined that the facility failed to ensure that resident-centered care plans were developed and implemented for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on review of facility policy and clinical records, as well as staff interviews, it was determined that the facility failed to ensure that a resident's care plan was updated/revised to reflect th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on review of facility policy, clinical record reviews, and resident and staff interviews, it was determined that the facility failed to ensure a safe environment related to smoking for one of 44...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on review of manufacturer's instructions and clinical records, as well as observations and staff interviews, it was determined that the facility failed to maintain a medication administration er...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on review of facility policies and clinical records, as well as staff interviews, it was determined that the facility failed to ensure that each resident was offered and/or received the influenz...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
Based on clinical record reviews and staff interviews, it was determined that the facility failed to provide medications as ordered by the physician for two of 44 residents reviewed (Residents 55, 84)...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected multiple residents
Based on a review of facility policies and clinical records, as well as staff interviews, it was determined that the facility failed to provide appropriate care to prevent urinary tract infections for...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0699
(Tag F0699)
Could have caused harm · This affected multiple residents
Based on review of clinical records, as well as resident and staff interviews, it was determined that the facility failed to ensure that residents were assessed and received trauma-informed care to el...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0744
(Tag F0744)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of facility policies, clinical records, and investigation reports, as well as staff interviews, it was determine...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0802
(Tag F0802)
Could have caused harm · This affected multiple residents
Based on observations, as well as resident and staff interviews, it was determined that the facility failed to have sufficient dietary staff to enable the main dining room to be open for meal times.
F...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on review of faciliy policy, observations, and staff interviews, it was determined that the facility failed to prepare and store ice under sanitary conditions for one of three ice machines (seco...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected multiple residents
Based on review of the facility's plans of correction for previous surveys, and the results of the current survey, it was determined that the facility's Quality Assurance Performance Improvement (QAPI...
Read full inspector narrative →
May 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on review of policies and clinical records, as well as staff interviews, it was determined that the facility failed to ensure that the resident's responsible party was notified about the need to...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on review of clinical records and facility investigation reports, as well as staff interviews, it was determined that the facility failed to ensure that the resident environment remained free of...
Read full inspector narrative →
Feb 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on review of policies and clinical records, as well as staff interviews, it was determined that the facility failed to ensure that the residents' environment remained free of accident hazards fo...
Read full inspector narrative →
Oct 2023
21 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on a review of policies, as well as interviews with residents and staff, it was determined that the facility failed to ensure that residents and/or their representatives could file a grievance/c...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on review of clinical records and staff interviews, it was determined that the facility failed to develop a comprehensive care plan that included specific and individualized interventions to add...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on review of facility policy and clinical records, as well as staff interviews, it was determined that the facility failed to ensure that a resident's care plan was updated/revised to reflect th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on review of Pennsylvania's Nursing Practice Act, facility policies, and clinical records, as well as staff interviews, it was determined that the facility failed to ensure that an assessment wa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on review of policies and clinical records, as well as observations and staff interviews, it was determined that the facility failed to ensure that residents were provided proper nail care for o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on review of the clinical records and facility policies, as well as observations and staff interviews, it was determined that the facility failed to ensure that pressure ulcer prevention interve...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on review of clinical records, observations, and staff interviews, it was determined that the facility failed to ensure that physician-ordered contracture management services were provided as ca...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on clinical record reviews, observations, and staff interviews, it was determined that the facility failed to supervise a resident while eating resulting in a choking episode requiring back blow...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on clinical record reviews, observations, and staff interviews, it was determined that the facility failed to provide appropriate care for an indwelling urinary catheter for one of 46 residents ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on review of clinical records and facility policies, as well as observations and staff interviews, it was determined that the facility failed to ensure that a resident's respiratory status was p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on clinical record reviews, as well as observations and staff interviews, it was determined that the facility failed to ensure that a dialysis emergency kit containing appropriate equipment, suc...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0742
(Tag F0742)
Could have caused harm · This affected 1 resident
Based on review of policies and clinical records, as well as resident and staff interviews, it was determined that the facility failed to ensure that a resident who displayed problematic wandering beh...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on review of policies and clinical records, medication manufacture instructions, as well as observations and staff interviews, it was determined that the facility failed to ensure that medicatio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
Based on facility policy, clinical record reviews, observations, and staff and resident interviews, it was determined that the facility failed to honor food preferences for one of 46 residents reviewe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on review of clinical records, as well as staff interviews, it was determined that the facility failed to maintain clinical records that were complete and accurately documented for one of 46 res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0849
(Tag F0849)
Could have caused harm · This affected 1 resident
Based on review of hospice contracts and clinical records, as well as staff interviews, it was determined that the facility failed to ensure that the designated interdisciplinary team member obtained ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected 1 resident
Based on review of the facility's plans of correction for previous surveys, and the results of the current survey, it was determined that the facility's Quality Assurance Performance Improvement (QAPI...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on review of facility policies and clinical records, as well as observations and staff interviews, it was determined that the facility failed to follow CDC guidelines to reduce the spread of inf...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
Based on staff and resident interviews, it was determined that the facility failed to ensure that meals were served in a manner that maintained or enhanced each resident's dignity by serving meals on ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
Based on review of clinical records, as well as staff interviews, it was determined that the facility failed to ensure that physician's orders for medications were followed for two of 46 residents rev...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on review of policies, as well as observations and staff interviews, it was determined that the facility failed to ensure that food items in the walk-in freezer were properly secured, labeled an...
Read full inspector narrative →
Jul 2023
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on review of Pennsylvania laws, the facility's policies, and residents' clinical records, as well as staff interviews, it was determined that the facility failed to ensure that all alleged viola...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on review of policies and clinical records, as well as staff interviews, it was determined that the facility failed to thoroughly investigate potential abuse/misappropriation for one of six resi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0836
(Tag F0836)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the Older Adults Protective Services Act, facility policies, information provided by the facility, and reside...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record reviews and staff interviews, it was determined that the facility failed to ensure that clinical record...
Read full inspector narrative →
Jun 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on review of facility policies, clinical records, as well as staff interviews, it was determined that the facility failed to ensure that a resident's care plan was updated/revised to reflect the...
Read full inspector narrative →
Mar 2023
8 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on clinical record reviews and staff interviews, it was determined that the facility failed to ensure that a resident's responsible party was notified about a change in condition/care for one of...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on review of policies, clinical records, and facility grievance forms, as well as staff interviews, it was determined that the facility failed to make ongoing efforts to resolve grievances for o...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on review of facility policies and clinical records, as well as staff interviews, it was determined that the facility failed to follow physician's orders for labwork for one of 22 residents revi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on a review of clinical records and facility reports, as well as staff interviews, it was determined that the facility failed to ensure that a resident's environment remained as free of accident...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on review of clinical records and staff interviews, it was determined that the facility failed to ensure that there was timely notification and/or intervention for significant weight loss for on...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on clinical record reviews and staff interviews, it was determined that the facility failed to maintain clinical records that were complete and accurately documented for one of 22 residents revi...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observations and staff interviews, it was determined that the facility failed to provide a clean and homelike environment in the second floor dining room and in a residents' room for one of 2...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of policies and clinical records, as well as observations and staff interviews, it was determined that the facil...
Read full inspector narrative →
Feb 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of policies and clinical records, as well as staff interviews, it was determined that the facility failed to ens...
Read full inspector narrative →
Jan 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0576
(Tag F0576)
Could have caused harm · This affected 1 resident
Based on review of clinical records and facility grievance forms, as well as staff interviews, it was determined that the facility failed to maintain the privacy of residents' mail and failed to ensur...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on review of policies, clinical records, and facility grievance forms, as well as staff interviews, it was determined that the facility failed to include the steps taken to investigate the griev...
Read full inspector narrative →
Jan 2023
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on review of policies and clinical records, as well as observations and staff interviews, it was determined that the facility failed to ensure that the resident environment remained as free of a...
Read full inspector narrative →
Nov 2022
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on review of written and posted menus, as well as observations and staff interviews, it was determined that the facility failed to follow their planned menu, and it was determined that the porti...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 35% turnover. Below Pennsylvania's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: 1 harm violation(s), $98,690 in fines, Payment denial on record. Review inspection reports carefully.
- • 71 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • $98,690 in fines. Extremely high, among the most fined facilities in Pennsylvania. Major compliance failures.
- • Grade F (25/100). Below average facility with significant concerns.
About This Facility
What is Mountain Laurel Healthcare And Rehabilitation Ctr's CMS Rating?
CMS assigns MOUNTAIN LAUREL HEALTHCARE AND REHABILITATION CTR an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Pennsylvania, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Mountain Laurel Healthcare And Rehabilitation Ctr Staffed?
CMS rates MOUNTAIN LAUREL HEALTHCARE AND REHABILITATION CTR's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 35%, compared to the Pennsylvania average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Mountain Laurel Healthcare And Rehabilitation Ctr?
State health inspectors documented 71 deficiencies at MOUNTAIN LAUREL HEALTHCARE AND REHABILITATION CTR during 2022 to 2025. These included: 1 that caused actual resident harm and 70 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Mountain Laurel Healthcare And Rehabilitation Ctr?
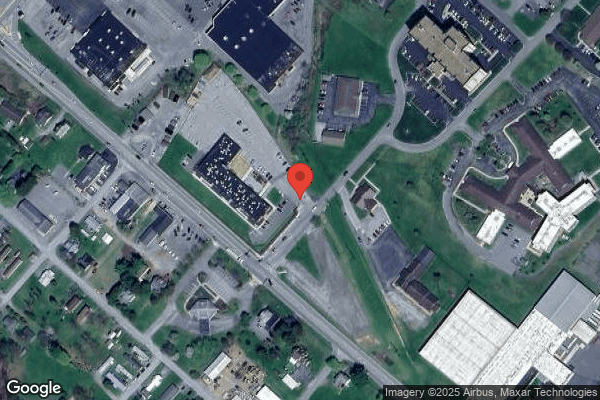
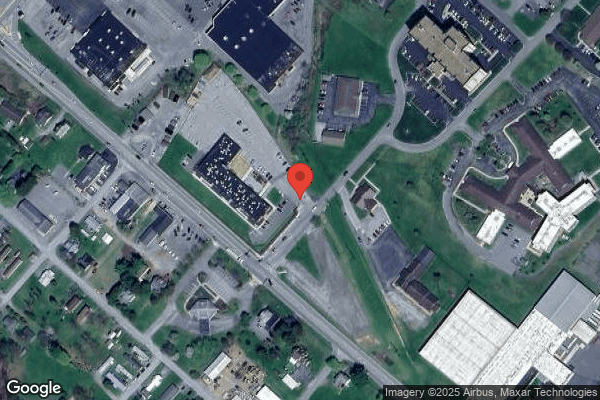
MOUNTAIN LAUREL HEALTHCARE AND REHABILITATION CTR is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 240 certified beds and approximately 103 residents (about 43% occupancy), it is a large facility located in CLEARFIELD, Pennsylvania.
How Does Mountain Laurel Healthcare And Rehabilitation Ctr Compare to Other Pennsylvania Nursing Homes?
Compared to the 100 nursing homes in Pennsylvania, MOUNTAIN LAUREL HEALTHCARE AND REHABILITATION CTR's overall rating (1 stars) is below the state average of 3.0, staff turnover (35%) is significantly lower than the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Mountain Laurel Healthcare And Rehabilitation Ctr?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Mountain Laurel Healthcare And Rehabilitation Ctr Safe?
Based on CMS inspection data, MOUNTAIN LAUREL HEALTHCARE AND REHABILITATION CTR has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Pennsylvania. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Mountain Laurel Healthcare And Rehabilitation Ctr Stick Around?
MOUNTAIN LAUREL HEALTHCARE AND REHABILITATION CTR has a staff turnover rate of 35%, which is about average for Pennsylvania nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Mountain Laurel Healthcare And Rehabilitation Ctr Ever Fined?
MOUNTAIN LAUREL HEALTHCARE AND REHABILITATION CTR has been fined $98,690 across 2 penalty actions. This is above the Pennsylvania average of $34,066. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Mountain Laurel Healthcare And Rehabilitation Ctr on Any Federal Watch List?
MOUNTAIN LAUREL HEALTHCARE AND REHABILITATION CTR is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.