ALTERNATIVE HEALTHCARE SOLUTIONS LLC
Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Alternative Healthcare Solutions LLC in San Juan, Puerto Rico has a Trust Grade of C+, which indicates that the facility is slightly above average but not without its issues. It ranks #1 out of 6 nursing homes in Puerto Rico and #1 out of 2 in San Juan County, placing it in the top tier of local options. Unfortunately, the facility is experiencing a worsening trend in quality, with a slight increase in reported issues from 16 in 2023 to 17 in 2024. Staffing is a strong point, rated 5 out of 5 stars with a turnover rate of 32%, close to the state average, meaning staff are generally stable and familiar with residents. However, the facility has incurred $68,560 in fines, which is concerning and indicates ongoing compliance problems. Specific incidents that raise red flags include the use of Styrofoam trays for meals, leading to food served at unsafe temperatures, and a lack of proper food storage and safety practices, such as unmarked food items and spoiled produce being found in the kitchen. Despite these weaknesses, the high staffing rating suggests there are dedicated caregivers who can provide quality attention to residents. Families should weigh these strengths against the notable concerns when considering this facility for their loved ones.
- Trust Score
- C+
- In Puerto Rico
- #1/6
- Safety Record
- Moderate
- Inspections
- Getting Worse
- Staff Stability ○ Average
- 32% turnover. Near Puerto Rico's 48% average. Typical for the industry.
- Penalties ✓ Good
- $68,560 in fines. Lower than most Puerto Rico facilities. Relatively clean record.
- Skilled Nurses ✓ Good
- Each resident gets 376 minutes of Registered Nurse (RN) attention daily — more than 97% of Puerto Rico nursing homes. RNs are the most trained staff who catch health problems before they become serious.
- Violations ⚠ Watch
- 33 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Staffing Rating · Excellent nurse staffing levels
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (32%)
16 points below Puerto Rico average of 48%
Facility shows strength in staffing levels, fire safety.
The Bad
14pts below Puerto Rico avg (46%)
Typical for the industry
Well above median ($33,413)
Moderate penalties - review what triggered them
The Ugly 33 deficiencies on record
Dec 2024
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** d. The Diet department was visited on 12/02/2024 at 10:20 AM. Kitchen the manager (employee #6) was asked by the surveyor in rel...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on Physical enviroment observations, performed on 12/02/2024 through 12/03/2024 to from 8:30 AM through 3:30 PM, it was de...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0802
(Tag F0802)
Could have caused harm · This affected most or all residents
Findings include:
The following was identified during the dining services evaluation process:
1. Breakfast and lunch are served in Styrofoam disposable trays. The trays are assembled in a way that hot...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on dining observations, review of policies procedures and facility staff interview performed on 12/02/2024 through 12/03/2...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on flash tour and kitchen observations, performed on 12/02/2024 through 12/03/2024 from 8:30 AM through 4:30 PM, it was determined that the facility failed to ensure that facility failed to stor...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on announces recertification survey, during the observation procedure by the staff on 12/02/2024, it was determined that t...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations of the physical environment and facility staff interview performed on 12/02/2024 through 12/03/2024 from 8...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected most or all residents
Based on unannounced recertification survey, during the observation conducted at the nursing desk on 12/02/2024, it was determined that the facility failed did not ensure that the following informatio...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0883
(Tag F0883)
Minor procedural issue · This affected most or all residents
Based on records reviewed (RR) and observations on 12/02/2024, it was determined that the facility failed to ensure that education was provided to residents on the benefits and side effects of Covid-1...
Read full inspector narrative →
Apr 2024
8 deficiencies
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations of the physical environment, review of policies and procedures and facility staff interview performed on 0...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on eleven records reviewed (RR) resident interview, and interview with the Nursing Supervisor (employee #2) performed from...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0694
(Tag F0694)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. R. R #8 is a [AGE] year-old male resident admitted [DATE] with a diagnosis of Lumbar Discitis plus Osteomyelitis. Resident wa...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected most or all residents
4. Information related to the competence certification and skills of nursing personnel who are interacting with residents who had PICC lines was not provided or evidenced during survey procedures on 0...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0802
(Tag F0802)
Could have caused harm · This affected most or all residents
Based on observations and interview with the Dietitian (employee #1) performed from 04/17/2024 thru 04/18/2024, from 8:00 AM thru 4:00 PM, it was determined that the facility failed to provide suffici...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations of the Kitchen, review of policies procedures and facility staff interview performed on 04/17/2024 to from 8:00 AM through 4:00 PM, it was determined that the facility failed to ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0813
(Tag F0813)
Could have caused harm · This affected most or all residents
Based on review of policies, procedures and facility staff interview performed on 04/17/2024 to from 8:00 AM through 4:30 PM, it was determined that the facility failed to comply with the policy regar...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations performed from 04/17/2024 through 04/18/2024, from 8:20 AM through 4:30 PM, it was determined that the fac...
Read full inspector narrative →
May 2023
16 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on a recertification survey, review of eleven medical records, resident interview and interview with the Nursing Superviso...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on recertification survey, performed on 5/01/2023 to 5/2/2003 at 8:00 AM to 4:00 PM, observation and interview of resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on recertification survey, interview of eleven medical records, and interview conducted 5/01/2023 to 5/02/2023 from 8:00 A...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on a recertification survey, observations, review of 9 clinical records, two closed records ,3 random sample, and intervie...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on a recertification survey, observations of the physical environment, review of policies procedures and facility staff in...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Record review #65 is a [AGE] year-old male resident admitted [DATE] with a diagnosis of Left heel Infected Ulcer with Osteomy...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on a Recertification survey and review of Beneficiary Protection Notification of the past 6 month, it was determined that ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 6. Record review #5 is an [AGE] year-old male admitted on [DATE] with diagnosis of Descondition. The resident was admitted for r...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on a recertification survey, observational tour of the facility's kitchen performed from 05/01/2023 thru 05/02/2023, from 8:40 AM thru 4:30 PM and interview with administrative dietitian (employ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected most or all residents
Based on recertification survey, performed on 05/01/23 through 05/02/23 from 8:00 AM till 4:30 PM review of Quality Assessment Performance Improvement (QAPI) program documentation and interview with D...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0868
(Tag F0868)
Could have caused harm · This affected most or all residents
Based on recertification survey, performed on 05/01/23 through 05/02/23 from 8:00 AM till 4:30 PM review of Quality Assessment Performance Improvement (QAPI) program documentation and interview with D...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 6. Record review #65 is a [AGE] year-old male resident admitted [DATE] with a diagnosis of Left heel Infected Ulcer with Osteomy...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0882
(Tag F0882)
Could have caused harm · This affected most or all residents
Based on recertification survey, performed on 05/01/23 through 05/02/23 from 8:00 AM till 4:30 PM review of Infection Control program documentation and interview with Director of Nursing (DON) (employ...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected most or all residents
Based on recertification survey, performed on 05/01/23 through 05/02/23 from 8:00 AM till 4:30 PM observations and interview with Information Technician (employee #7) it was identified that facility f...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0740
(Tag F0740)
Minor procedural issue · This affected most or all residents
Based on recertification survey review of policies and procedures, record review, and interview, with Medical Director (employee #3), it was determined that the facility failed to have an organized be...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0741
(Tag F0741)
Minor procedural issue · This affected most or all residents
Based on recertification survey review of policies and procedures, record review, and interview, with Medical Director (employee #3), it was determined that the facility failed to have an organized pr...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 32% turnover. Below Puerto Rico's 48% average. Good staff retention means consistent care.
- • 33 deficiencies on record. Higher than average. Multiple issues found across inspections.
- • $68,560 in fines. Extremely high, among the most fined facilities in Puerto Rico. Major compliance failures.
About This Facility
What is Alternative Healthcare Solutions Llc's CMS Rating?
CMS assigns ALTERNATIVE HEALTHCARE SOLUTIONS LLC an overall rating of 4 out of 5 stars, which is considered above average nationally. Within Puerto Rico, this rating places the facility higher than 99% of the state's 100 nursing homes. This rating reflects solid performance across the metrics CMS uses to evaluate nursing home quality.
How is Alternative Healthcare Solutions Llc Staffed?
CMS rates ALTERNATIVE HEALTHCARE SOLUTIONS LLC's staffing level at 5 out of 5 stars, which is much above average compared to other nursing homes. Staff turnover is 32%, compared to the Puerto Rico average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Alternative Healthcare Solutions Llc?
State health inspectors documented 33 deficiencies at ALTERNATIVE HEALTHCARE SOLUTIONS LLC during 2023 to 2024. These included: 28 with potential for harm and 5 minor or isolated issues.
Who Owns and Operates Alternative Healthcare Solutions Llc?
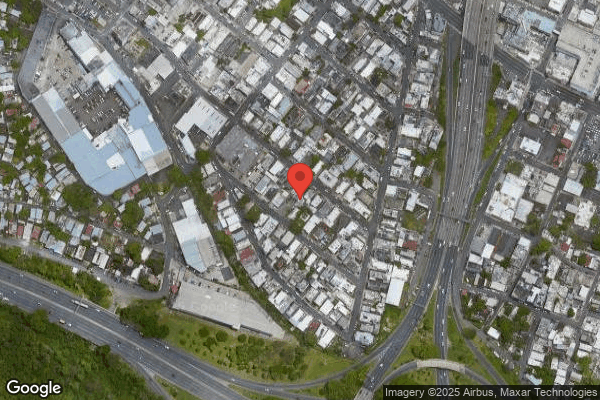
ALTERNATIVE HEALTHCARE SOLUTIONS LLC is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 22 certified beds and approximately 12 residents (about 55% occupancy), it is a smaller facility located in SAN JUAN, Puerto Rico.
How Does Alternative Healthcare Solutions Llc Compare to Other Puerto Rico Nursing Homes?
Compared to the 100 nursing homes in Puerto Rico, ALTERNATIVE HEALTHCARE SOLUTIONS LLC's overall rating (4 stars) is above the state average of 3.5, staff turnover (32%) is significantly lower than the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Alternative Healthcare Solutions Llc?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Alternative Healthcare Solutions Llc Safe?
Based on CMS inspection data, ALTERNATIVE HEALTHCARE SOLUTIONS LLC has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 4-star overall rating and ranks #1 of 100 nursing homes in Puerto Rico. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Alternative Healthcare Solutions Llc Stick Around?
ALTERNATIVE HEALTHCARE SOLUTIONS LLC has a staff turnover rate of 32%, which is about average for Puerto Rico nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Alternative Healthcare Solutions Llc Ever Fined?
ALTERNATIVE HEALTHCARE SOLUTIONS LLC has been fined $68,560 across 15 penalty actions. This is above the Puerto Rico average of $33,764. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Alternative Healthcare Solutions Llc on Any Federal Watch List?
ALTERNATIVE HEALTHCARE SOLUTIONS LLC is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.