CRITICAL
(K)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Quality of Care
(Tag F0684)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, medical record review, and interview, the facility failed to ensure services were provided to m...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, medical record review, and interview, the facility failed to ensure services were provided to meet professional standards of quality and acceptable standards of clinical practice by not obtaining vital signs per physician orders for residents with an active COVID-19 infection diagnosis for 36 of 40 residents (Resident #96, #45, #31, #33, #11, #609, #64, #93, #15, #510, #612, #611, #80, #506, #613, #615, #54, #68, #27, #53, #12, #95, #74, #3, #30, #37, #617, #34, #618, #72, #103, #507, #102, #508, #619, and #509) reviewed with active COVID-19 infection and 1 of 8 residents (Resident #99) reviewed for medication administration when nursing staff administered oral medication with a 60 milliliter (ml) syringe to Resident #99 who was at high risk for aspiration. The facility's failure to obtain vital signs per physician orders for residents with an active COVID-19 diagnosis and failure to ensure care was provided within the professional scope of practice for medication administration resulted in an Immediate Jeopardy (IJ), (a situation in which the provider's noncompliance with one or more requirements of participation has caused, or is likely to cause, serious injury, harm, impairment, or death to a resident) which had the potential or likelihood to cause a serious adverse outcome for all 99 residents in the facility. The facility census was 99.
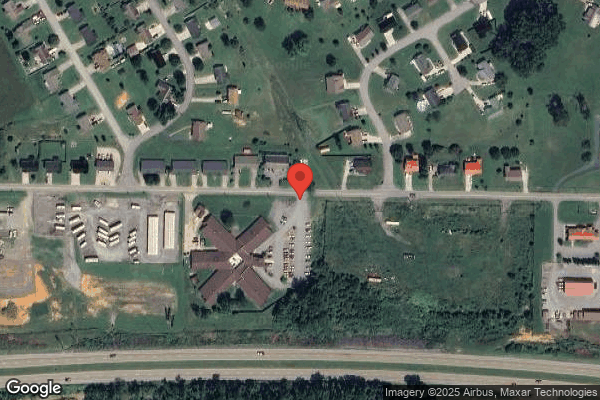
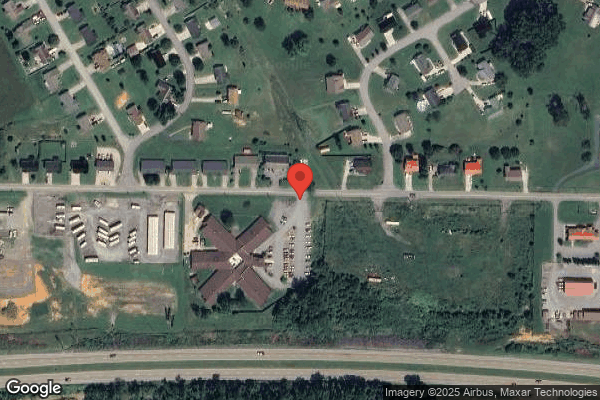
The Administrator, Director of Nursing (DON), [NAME] President of Operations (VPO), [NAME] President of Life Safety and Environmental Compliance (VPLSEC), and [NAME] President of Clinical Services (VPCS) (attended in person) and the [NAME] President of Regulatory Compliance (VPRC) and Chief Operating Officer (COO) with the Chief Regulatory Compliance Officer (CRCO) (attended by telephone) were notified of the IJs for F-684, F-726, F-835, F-837, F-867, and F-880, and on 11/13/2024 at 9:42 PM in the Common Area/Recreation Area.
The facility was cited Immediate Jeopardy at F-684 at a scope and severity of K, which is substandard quality of care.
An Extended survey was conducted onsite from 11/14/2024 through 11/15/2024.
The IJ began on 8/9/2024 and is ongoing.
The facility is required to submit a Plan of Correction (POC).
The findings include:
Review of the facility's policy titled, Physician Orders, undated, revealed .A physician .nurse practitioner [NP] .must provide written .verbal orders for the residents' care and needs .order should allow facility staff .provide essential care .to .residents .orders .provide information .maintain or improve .resident's functional abilities .
Review of the facility's policy titled, COVID-19 Management of Residents, undated, which referenced the 5/25/2023 Centers for Disease Control (CDC) guidelines revealed .The facility will not have a dedicated COVID-19 unit unless the number of positive residents warrant .the facility will place a COVID-19 positive resident in a single room with appropriate isolation signage and staff wearing N95 respirator [face mask], eye protection, gown, and gloves upon entry to the room .dedicated staff, to care for residents with COVID-19 .resident will be monitored every four hours for .symptoms, vital signs, oxygen saturation [O2 sat] .and respiratory exam [examination] .residents will .wear source control until symptoms resolve .
Review of the facility's policy titled, Documentation in the Residents' Records Guidelines, undated, revealed .documentation shall be completed at the time of service, but no later than the shift the assessment .occurred .documentation .shall be .accurate .containing .details about the resident's care .and/or response to care .
1. The facility failed to obtain vital signs as ordered by the physician for 36 of 40 residents with an active COVID-19 infection.
1a. Review of the medical record revealed Resident #96 was admitted to the facility on [DATE] with diagnoses including Pulmonary Disease, Heart Failure, Depression, and Hypertension. The diagnosis of COVID-19 was added on 8/14/2024.
Review of the laboratory result for Resident #96 dated 8/14/2024, revealed a positive COVID-19 test result.
Review of a Physician's Order for Resident #96 dated 8/14/2024, revealed . Vital Signs monitoring for Covid [COVID-19] Positive every 4 hours throughout covid positive Isolation precautions . the isolation and vital signs continued until 8/24/2024.
Review of the comprehensive care plan for Resident #96 dated 8/14/2024, revealed .Observe vital signs. Notify physician if abnormal .
Review of an admission Minimum Data Set (MDS) assessment dated [DATE], revealed Resident #96 scored a 15 on the Brief Interview for Mental Status (BIMS) assessment, which indicated the resident was cognitively intact.
Review of the Weights and Vitals Summary for Resident #96 dated 8/14/2024-8/24/2024, revealed the following lapses in obtaining the every 4-hour vital signs:
On 8/14/2024, the facility obtained vital signs (VS), temperature, respirations, pulse, oxygen saturation (O2 sat), and blood pressure only 2 of 6 times as ordered.
On 8/15/2024, the facility obtained VS only 3 of 6 times as ordered.
On 8/16/2024, the facility obtained VS only 1 of 6 times as ordered.
On 8/19/2024, the facility obtained the pulse and blood pressure only 1 of 6 times as ordered and no other VS were documented.
On 8/20/2024, the facility obtained VS only 1 of 6 times as ordered.
On 8/23/2024, the facility obtained the pulse and blood pressure only 1 of 6 times as ordered and no other VS were documented.
The facility failed to obtain any VS on Resident #96 on 8/17/2024, 8/18/2024, 8/21/2024, 8/22/2024, and 8/24/2024.
1b. Review of the medical record revealed Resident #45 was admitted to the facility on [DATE] with diagnoses including Cerebral Infarction, Hypertension, Fibromyalgia, and Chronic Pain Syndrome. The diagnosis of COVID-19 was added on 8/21/2024.
Review of the medical record for Resident #45 revealed no documentation of a positive COVID-19 test conducted from 8/20/2024-8/26/2024.
Review of the NP Progress Notes for Resident #45 dated 8/21/2024, revealed .Resident was seen today due to positive result of COVID [COVID-19] swab in facility .
Review of a Physician's Order for Resident #45 dated 8/23/2024, (2 days after positive test), revealed .Vital Signs monitoring for Covid Positive every 4 hours throughout covid positive Isolation precautions . the isolation and vital sign monitoring continued until 8/31/2024.
Review of a comprehensive care plan for Resident #45 dated 8/26/2024, revealed the resident had tested positive for COVID-19 with interventions including .Observe vital signs. Notify physician if abnormal .Resident under droplet precautions .
Review of the Weights and Vitals Summary, for Resident #45 dated 8/23/2024-8/31/2024, revealed the following lapses in obtaining the every 4-hour vital signs:
On 8/23/2024, the facility obtained the pulse and blood pressure only 2 of 6 times as ordered and no other vital signs were documented.
On 8/24/2024, 8/25/2024, and 8/26/2024, the facility obtained the pulse and blood pressure only 1 of 6 times as ordered and no other VS were documented.
On 8/25/2024, the facility obtained the pulse and blood pressure only 1 of 6 times as ordered and no other VS were documented.
On 8/26/2024, the facility obtained the pulse and blood pressure only 1 of 6 times as ordered and no other VS were documented.
On 8/27/2024, the facility obtained VS only 1 of 6 times as ordered.
On 8/29/2024, the facility obtained the pulse only 2 of 6 times as ordered, the blood pressure was obtained only 1 of 6 times as ordered, and no other VS were documented.
On 8/30/2024, the facility obtained the pulse and blood pressure only 2 of 6 times as ordered and no other VS were documented.
On 8/31/2024, the facility obtained the pulse and blood pressure only 1 of 6 times as ordered and no other VS were documented.
The facility failed to obtain any VS on Resident #45 on 8/28/2024.
Review of a significant change in status MDS assessment dated [DATE], revealed Resident #45 scored a 12 on the BIMS assessment, which indicated moderate cognitive impairment.
1c. Review of the medical record revealed Resident #31 was admitted to the facility on [DATE] with diagnoses including Dementia, Type 2 Diabetes, Hypertension, and Anemia. The diagnosis of COVID-19 was added on 8/21/2024.
Review of a quarterly MDS assessment dated [DATE], revealed Resident #31 scored a 99 on the BIMS assessment, which indicated the resident was unable to complete the interview.
Review of the laboratory result for Resident #31 dated 8/21/2024, revealed a positive COVID-19 test result.
Review of a Physician's Order for Resident #31 dated 8/23/2024 (2 days after the positive test), revealed .Vital Signs monitoring for Covid Positive every 4 hours throughout covid positive Isolation precautions . the isolation and vital sign monitoring continued until 8/31/2024.
Review of a comprehensive care plan for Resident #31 dated 8/26/2024 (5 days after the positive test), revealed the resident had tested positive for COVID-19.
Review of the Weights and Vitals Summary, for Resident #31 dated 8/21/2024-8/31/2024, revealed the following lapses in obtaining the every 4-hour vital signs:
On 8/21/2024, the facility obtained the temperature, pulse, and blood pressure only 1 of 6 times as ordered and no other VS were documented.
On 8/22/2024, 8/23/2024, 8/25/2024, 8/26/2024, 8/27/2024, and 8/29/2024, the facility obtained the pulse and blood pressure only 1 of 6 times as ordered and no other VS were documented.
The facility failed to obtain VS on Resident #31 on 8/24/2024, 8/28/2024, 8/30/2024, and 8/31/2024.
1d. Review of the medical record revealed Resident #33 was admitted to the facility on [DATE] with diagnoses including Generalized Arthritis, Hypertension, Chronic Pain, Heart Failure, and Difficulty Walking. The diagnosis of COVID-19 was added on 8/22/2024.
Review of an admission MDS assessment dated [DATE], revealed Resident #33 scored a 7 on the BIMS assessment, which indicated severe cognitive impairment.
Review of the laboratory result for Resident #33 dated 8/23/2024, revealed the COVID-19 test result was flagged as abnormal, which indicated the test was positive. Continued review of the laboratory result revealed the nursing staff had documented NEG [negative] in the notes field of the document, resulting in a conflicting result that indicated a negative COVID-19 test result.
Review of a Physician's Order for Resident #33 dated 8/23/2024, revealed .Vital Signs monitoring for Covid Positive every 4 hours throughout covid positive Isolation precautions . the isolation and vital signs continued until 8/31/2024.
Review of the comprehensive care plan for Resident #33 dated 8/23/2024, revealed the resident tested positive for COVID-19 and was placed under droplet precautions. Continued review revealed .Observe vital signs. Notify physician if abnormal .Observe/document breath sounds, document rate, rhythm, and the use of any accessory muscles .Notify MD if resident has low oxygen saturation or goes into respiratory distress .
During an interview on 11/12/2024 at 3:48 PM, the [NAME] President (VP) of Clinical Services stated according to the NP visit note for Resident #33 dated 8/26/2024, the resident was evaluated for a positive COVID-19 diagnosis after testing positive for COVID-19 on 8/23/2024. Continued interview confirmed the COVID-19 test result documentation dated 8/23/2024 was inaccurately documented as NEG when the resident had an active COVID-19 diagnosis and positive test result.
Review of the Weights and Vitals Summary, for Resident #33 dated 8/23/2024 through 9/1/2024, revealed the following lapses in obtaining the every 4-hour vital signs:
On 8/23/2024, the temperature was only obtained 1 of 6 times as ordered, the respirations and O2 Sat were only obtained 2 of times as ordered, the pulse and blood pressure were only obtained 3 of 6 times as ordered, and no other VS were documented.
On 8/26/2024 and 8/27/2024, the facility only obtained the VS 1 of 6 times as ordered and no other VS were documented.
On 8/29/2024 and 8/30/2024, the facility obtained the pulse and blood pressure only 1 of 6 times as ordered and no other VS were documented.
On 9/1/2024, the facility obtained the respirations, pulse, O2 Sat, and blood pressure only 1 of 6 times as ordered and no other VS were documented.
The facility failed to obtain any VS on Resident #33 on 8/24/2024, 8/25/2024, 8/28/2024, and 8/31/2024.
1e. Review of the medical record revealed Resident #11 was admitted to the facility on [DATE] with diagnoses including Hypertension, Diabetes, and Depression. The diagnosis of COVID-19 was added on 8/22/2024.
Review of a quarterly MDS assessment dated [DATE], revealed Resident #11 scored a 15, which indicated the resident was cognitively intact.
Review of the laboratory result for Resident #11 dated 8/23/2024, revealed a positive COVID-19 test result.
Review of a Physician's Order for Resident #11 dated 8/23/2024, revealed .Vital Signs monitoring for Covid Positive every 4 hours throughout covid positive Isolation precautions . the isolation and vital signs continued until 9/1/2024.
Review of a comprehensive care plan for Resident #11 dated 8/23/2024, revealed the resident had tested positive for COVID-19 with interventions including .Observe vital signs. Notify physician if abnormal .
Review of the Weights and Vitals Summary, for Resident #11 dated 8/23/2024-9/1/2024, revealed the following lapses in obtaining the every 4-hour vital signs:
On 8/23/2024, the facility obtained the pulse and blood pressure only 2 of 6 times as ordered and no other VS were documented.
On 8/25/2024, 8/26/2024, 8/27/2024, and 8/28/2024, the facility obtained the pulse and blood pressure only 1 of 6 times as ordered and no other VS were documented.
On 8/29/2024 and 8/30/2024, the facility obtained the pulse and blood pressure only 2 of 6 times as ordered and no other VS were documented.
On 8/31/2024, the facility obtained the pulse and blood pressure only 1 of 6 times as ordered and no other VS were documented.
On 9/1/2024, the facility obtained the respirations and O2 Sat only 1 of 6 times as ordered, pulse and blood pressure only 2 of 6 times as ordered, and no other VS were documented.
The facility failed to obtain any VS on Resident #11 on 8/24/2024.
1f. Review of the medical record revealed Resident #609 was admitted to the facility on [DATE] and readmitted [DATE] with diagnoses including Thyroid Cancer, Chronic Pain, Pneumonia, Diabetes, Anxiety, and History of Lung Blood Clots. The diagnosis of COVID-19 was added on 9/4/2024.
Review of the laboratory result for Resident #609 dated 8/23/2024, revealed a positive COVID-19 test result.
Review of a Physician's Order for Resident #609 dated 8/23/2024, revealed .Isolation Droplet precautions @ all times due to positive covid 19 test . The isolation continued until 9/2/2024. Continued review revealed no order for vital sign monitoring.
Review of the admission MDS assessment dated [DATE], revealed Resident #609 scored a 7 on the BIMS assessment, which indicated severe cognitive impairment.
Review of a Physician's Order for Resident #609 dated 8/26/2024 (3 days after positive COVID-19 test), revealed .Vital Signs monitoring for Covid Positive every 4 hours throughout covid positive Isolation precautions . the isolation and vital sign monitoring continued until 9/2/2024.
Review of a comprehensive care plan for Resident #609 dated 8/26/2024, revealed the resident had tested positive for COVID-19 with interventions including .Observe vital signs. Notify physician if abnormal .
Review of theWeights and Vitals Summary, for Resident #609 dated 8/23/2024-9/2/2024, revealed the following lapses in obtaining the every 4-hour vital signs:
On 8/26/2024, the facility obtained the temperature, respirations, pulse, and blood pressure only 2 of 6 times as ordered, the O2 Sat only 3 of 6 times as ordered, and no other VS were documented.
On 8/28/2024, the facility obtained the O2 Sat only 1 of 6 times as ordered and no other VS were documented.
On 8/31/2024, the facility obtained the O2 Sat only 3 of 6 times as ordered and no other VS were documented.
On 9/2/2024, the facility obtained the temperature 1 of 6 times as ordered and no other VS were documented.
The facility to obtain any VS on Resident #609 on 8/27/2024, 8/29/2024, 8/30/2024, and 9/1/2024.
1g. Review of the medical record revealed Resident #64 was admitted to the facility on [DATE] with diagnoses including Diabetes, Heart Failure, and Hypertension. The diagnosis of COVID-19 was added on 8/25/2024.
Review of an admission MDS assessment dated [DATE], revealed Resident #64 scored a 15 on the BIMS assessment, which indicated the resident was cognitively intact.
Review of a Physician's Order for Resident #64 dated 8/23/2024 (2 days prior to the COVID-19 test), revealed .Vital Signs monitoring for Covid Positive every 4 hours throughout covid positive Isolation precautions . The isolation and vitals signs continued until 9/2/2024.
Review of the laboratory result for Resident #64 dated 8/25/2024, revealed a positive COVID-19 test result.
Review of a comprehensive care plan for Resident #64 dated 8/26/2024, revealed the resident had tested positive for COVID-19 with interventions including .Observe vital signs. Notify physician if abnormal .Resident under droplet precautions .
Review of the Weights and Vitals Summary, for Resident #64 dated 8/23/2024-9/2/2024, revealed the following lapses in obtaining the every 4-hour vital signs:
On 8/26/2024 and 8/27/2024, the facility obtained the VS only 1 of 6 times as ordered and no other VS were documented.
The facility failed to obtain any VS for Resident #64 on 8/23/2024, 8/24/2024, 8/25/2024, 8/28/2024, 8/29/2024, 8/30/2024, 8/31/2024, 9/1/2024, and 9/2/2024.
1h. Review of the medical record revealed Resident #93 was admitted to the facility on [DATE] with diagnoses including Encephalopathy, Hypothyroidism, Hypertension, and Difficulty in Walking. The diagnosis of COVID-19 was added on 8/26/2024.
Review of an admission MDS assessment dated [DATE], revealed Resident #93 scored an 8 on the BIMS assessment, which indicated moderate cognitive impairment.
Review of the medical record revealed a positive COVID-19 test for Resident #93 was not available for review.
Review of a NP Progress Notes for Resident #93 dated 8/23/2024, revealed .Resident was seen today due to testing positive for COVID-19 in the facility via nasal swab .
Review of a Physician's Order for Resident #93 dated 8/23/2024, revealed .Vital Signs monitoring for Covid Positive every 4 hours throughout covid positive Isolation precautions . the isolation and vital sign monitoring continued until 9/2/2024.
Review of a comprehensive care plan for Resident #93 dated 8/26/2024, revealed the resident tested positive for COVID-19 with interventions including .Observe vital signs. Notify physician if abnormal .
Review of the Weights and Vitals Summary, for Resident #93 dated 8/23/2024-9/2/2024, revealed the following lapses in obtaining the every 4-hour vital signs:
On 8/26/2024, the facility obtained the temperature only 2 of 6 times as ordered, obtained the respirations, pulse, O2 Sat, and blood pressure only 1 of 6 times as ordered, and no other VS were documented.
On 8/27/2024, the facility obtained the VS only 1 of 6 times as ordered and no other VS were documented.
On 8/28/2024, the facility obtained the temperature and blood pressure only 1 of 6 times as ordered and no other VS were documented.
The facility failed to obtain any VS for Resident #93 on 8/23/2024, 8/24/2024, 8/25/2024, 8/29/2024, 8/30/2024, 8/31/2024, 9/1/2024, and 9/2/2024.
1i. Review of the medical record revealed Resident #15 was admitted to the facility on [DATE], was discharged to the hospital, and readmitted to the facility on [DATE] with diagnoses including Mood Disorder, Vascular Dementia, Acute Kidney Failure, Pseudomonas, Non-Pressure Chronic Ulcer of Skin, Dysphagia, Venous Insufficiency, Anxiety Disorder, and Gastrointestinal Hemorrhage. The diagnosis of COVID-19 was added on 8/26/2024.
Review of a quarterly MDS assessment dated [DATE], revealed Resident #15 scored a 9 on the BIMS assessment, which indicated moderate cognitive impairment.
Review of the laboratory result for Resident #15 dated 8/23/2024, revealed a positive COVID-19 test result.
Review of a Physician's Order for Resident #15 dated 8/26/2024 (3 days after the positive test result), revealed .Vital Signs monitoring for Covid Positive every 4 hours throughout covid positive Isolation precautions . the isolation and vital signs continued until 9/1/2024.
Review of a comprehensive care plan for Resident #15 dated 8/26/2024, revealed the resident had tested positive for COVID-19 with interventions including .Observe vital signs. Notify physician if abnormal .
Review of the Weights and Vitals Summary, for Resident #15 dated 8/26/2024-9/1/2024, revealed the following lapses in obtaining the every 4-hour vital signs:
On 8/26/2024 and 8/27/2024, the facility obtained the VS only 1 of 6 times as ordered and no other VS were documented.
On 8/29/2024, the facility obtained the respirations, pulse, and blood pressure only 1 of 6 times as ordered and no other VS were documented.
On 9/1/2024, the facility obtained the respirations, pulse, O2 Sat, and blood pressure only 1 of 6 times as ordered and no other VS were obtained.
The facility failed to obtain any VS for Resident #15 on 8/28/2024, 8/30/2024, and 8/31/2024.
1j. Review of the medical record revealed Resident #510 was admitted to the facility on [DATE], was discharged to the hospital, and readmitted to the facility on [DATE] with diagnoses including Heart Failure, Atrial Fibrillation, Hypertension, and Difficulty in Walking. The diagnosis of COVID-19 was added on 8/26/2024.
Review of an admission MDS assessment dated [DATE], revealed Resident #510 scored a 13 on the BIMS assessment, which indicated the resident was cognitively intact.
Review of the laboratory result for Resident #510 dated 8/24/2024, revealed a positive COVID-19 test result.
Review of a Physician's Order for Resident #510 dated 8/26/2024 (2 days after the positive COVID-19 test result), revealed .Vital Signs monitoring for Covid Positive every 4 hours throughout covid positive Isolation precautions . the isolation and vital sign monitoring continued until 9/2/2024.
Review of a comprehensive care plan for Resident #510 dated 8/26/2024, revealed the resident had tested positive for COVID-19 with interventions including .Observe vital signs. Notify physician if abnormal .
Review of the Weights and Vitals Summary, for Resident #510 dated 8/26/2024-9/2/2024, revealed the following lapses in obtaining the every 4-hour vital signs:
On 8/26/2024, the facility obtained the respirations, pulse, O2 Sat and blood pressure only 1 of 6 times as ordered and no other VS were documented.
On 8/27/2024, the facility obtained the pulse, O2 Sat, and blood pressure only 1 of 6 times as ordered and no other VS were documented.
On 8/28/2024, the facility obtained the blood pressure only 1 of 6 times as ordered and no other VS were documented.
On 8/29/2024, the facility obtained the respirations, pulse and blood pressure only 1 of 6 times as ordered and no other VS were documented.
On 8/30/2024, the facility obtained the pulse and blood pressure only 1 of 6 times as ordered and no other VS were documented.
On 8/31/2024, the facility obtained the pulse only 1 of 6 times as ordered and no other VS were documented.
On 9/1/2024, the facility obtained the respirations, pulse, O2 Sat, and blood pressure only 1 of 6 times as ordered and no other VS were documented.
On 9/2/2024, the facility obtained the pulse and blood pressure only 1 of times as ordered, the O2 Sat only 2 of 6 times as ordered, and no other VS were documented.
1k. Review of the medical record revealed Resident #612 was admitted to the facility on [DATE] with diagnoses including Diabetes Mellitus, Asthma, Heart Failure, and Depression. The diagnosis of COVID-19 was added on 8/26/2024.
Review of the laboratory result for Resident #612 dated 8/24/2024, revealed a positive COVID-19 test result.
Review of a Physician's Order for Resident #612 dated 8/26/2024 (2 days after the positive COVID-19 test result), revealed .Vital Signs monitoring for Covid Positive every 4 hours throughout covid positive Isolation precautions . the isolation and vital sign monitoring continued until 9/3/2024.
Review of a comprehensive care plan for Resident #612 dated 8/26/2024, revealed the resident had tested positive for COVID-19 with interventions including .Observe vital signs. Notify physician if abnormal .
Review of an admission MDS assessment dated [DATE], revealed Resident #612 scored a 14 on the BIMS assessment, which indicated the resident was cognitively intact.
Review of the Weights and Vitals Summary, for Resident #612 dated 8/26/2024-9/3/2024, revealed the following lapses in obtaining the every 4-hour vital signs:
On 8/26/2024 and 8/27/2024, the facility obtained the VS only 1 of 6 times as ordered and no other VS were documented.
On 9/1/2024, the facility obtained the pulse only 1 of 6 times as ordered and no other VS were documented.
The facility failed to obtain any VS for Resident #612 on 8/28/2024, 8/29/2024, 8/30/2024, 8/31/2024, 9/2/2024, and 9/3/2024.
1l. Review of the medical record revealed Resident #611 was admitted to the facility on [DATE] and readmitted on [DATE] with diagnoses including Atrial Fibrillation, Hypertension, Heart Failure, and Difficulty in Walking. The diagnosis of COVID-19 was added on 8/26/2024.
Review of an admission MDS assessment dated [DATE], revealed Resident #611 scored a 15 on the BIMS assessment, which indicated the resident was cognitively intact.
Review of a Physician's Order for Resident #611 dated 8/26/2024, revealed .Vital Signs monitoring for Covid Positive every 4 hours throughout covid positive Isolation precautions . the isolation and vital sign monitoring continued until 9/3/2024.
Review of a comprehensive care plan for Resident #611 dated 8/26/2024, revealed the resident had tested positive for COVID-19 with interventions including .Observe vital signs. Notify physician if abnormal .
Review of the Weights and Vitals Summary, for Resident #611 dated 8/26/2024-9/3/2024, revealed the following lapses in obtaining every 4-hour vital signs:
On 8/26/2024, the facility obtained the temperature, respirations, pulse and O2 Sat only 1 of 6 times as ordered, obtained the blood pressure only 2 of times as ordered, and no other VS were documented.
On 8/27/2024, the facility obtained the temperature, respirations, pulse, and blood pressure only 1 of 6 times as ordered, the O2 Sat was obtained only 2 of 6 times as ordered, and no other VS were documented.
On 8/28/2024, the facility obtained the blood pressure only 1 of 6 times as ordered, obtained the temperature, respirations, pulse, and O2 Sat only 2 of 6 times as ordered and no other VS were documented.
On 8/29/2024, the facility obtained the O2 Sat only 1 of 6 times as ordered, temperature and respirations only 2 of 6 times as ordered, the blood pressure only 3 of 6 times as ordered, pulse only 4 of 6 times as ordered, and no other VS were documented.
On 8/30/2024, the facility obtained the O2 Sat only 1 of 6 times as ordered, the pulse and blood pressure only 2 of 6 times as ordered, and no other VS were documented.
On 8/31/2024, the facility obtained the pulse, O2 Sat and blood pressure only 1 of 6 times as ordered and no other VS were documented.
On 9/1/2024, the facility obtained the respirations, pulse, O2 Sat, and blood pressure only 1 of 6 times as ordered and no other VS were documented.
On 9/2/2024, the facility obtained the pulse, O2 Sat, and blood pressure only 2 of 6 times as ordered and no other VS were documented.
On 9/3/2024, the facility obtained the pulse, O2 Sat, and blood pressure only 1 of 6 times as ordered and no other VS were documented.
1m. Review of the medical record revealed Resident #80 was admitted to the facility on [DATE], was discharged to the hospital, and readmitted to the facility on [DATE] with diagnoses including Chronic Kidney Disease, Diabetes Mellitus, Hypertension, and Heart Failure. The diagnosis of COVID-19 was added on 8/26/2024.
Review of an admission MDS assessment dated [DATE], revealed Resident #80 scored a 10 on the BIMS assessment, which indicated moderate cognitive impairment.
Review of the medical record for Resident #80 revealed no documentation of a positive COVID-19 laboratory test result.
Review of the NP Progress note for Resident #80 dated 8/26/2024, revealed .Resident was seen today for a follow-up after recent positive COVID-19 swab .
Review of a Physician's Order for Resident #80 dated 8/26/2024, revealed .Vital Signs monitoring for Covid Positive every 4 hours throughout covid positive Isolation precautions . the isolation and vital sign monitoring continued until 9/3/2024.
Review of a comprehensive care plan for Resident #80 dated 8/26/2024, revealed the resident tested positive for COVID-19 with interventions including .Observe vital signs. Notify physician if abnormal .
Review of the Weights and Vitals Summary, for Resident #80 dated 8/26/2024-9/3/2024, revealed the following lapses in obtaining the every 4-hour vital signs:
On 8/26/2024, the facility obtained the respirations, pulse, O2 Sat, and blood pressure only 1 of 6 times as ordered, temperature only 2 of 6 times as ordered, and no other VS were documented.
On 8/27/2024, the VS were only obtained 1 of 6 times as ordered and no other VS were documented.
On 8/28/2024, the facility obtained the temperature only 1 of 6 times as ordered and no other VS were documented.
On 9/3/2024, the facility obtained the VS only 1 of 6 times as ordered and no other VS were documented.
The failed to obtain any VS for Resident #80 on 8/29/2024, 8/30/2024, 8/31/2024, 9/1/2024, and 9/2/2024.
1n. Review of the medical record revealed Resident #506 was admitted to the facility on [DATE], was discharged to the hospital, and readmitted to the facility on [DATE] with diagnoses including Cerebral Infarction, Chronic Pain Syndrome, and Muscle Weakness. The diagnosis of COVID-19 was added on 8/27/2024.
Review of a quarterly MDS assessment dated [DATE], revealed Resident #506 scored a 14 on the BIMS assessment, which indicated the resident was cognitively intact.
Review of the laboratory result for Resident #506 dated 8/26/20[TRUNCATED]
CRITICAL
(L)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0726
(Tag F0726)
Someone could have died · This affected most or all residents
⚠️ Facility-wide issue
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, job description reviews, review of the Centers for Disease (CDC) website for recommendations an...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, job description reviews, review of the Centers for Disease (CDC) website for recommendations and guidance for Enhanced Barrier Precautions (EBP) and Coronavirus Disease 2019 (COVID-19), medical record reviews, observations, and interviews, the facility failed to ensure the nursing staff were knowledgeable and fully understood of 6 residents (Residents # 13, #24, #25, #52, #56, and #83) in EBP on 3 of 4 hallways (200, 300, and 400 hallways), of 4 residents (Residents #102, #507, #508, and #509) with active COVID-19 infection on 1 of 4 hallways (100 hallway), and implemented the appropriate use of Personal Protective Equipment (PPE) for isolation rooms to prevent and control the spread of COVID-19, and other infectious organisms. The facility's non-compliance placed the residents in Immediate Jeopardy (IJ) (A situation in which the providers noncompliance with one or more requirements of participation has caused or is likely to cause serious injury, harm, impairment, or death to a resident).
The Administrator, Director of Nursing (DON), [NAME] President of Operations (VPO), [NAME] President of Life Safety and Environmental Compliance (VPLSEC), and [NAME] President of Clinical Services (VPCS) (attended in person) and the [NAME] President of Regulatory Compliance (VPRC) and Chief Operating Officer (COO) with the Chief Regulatory Compliance Officer (CRCO) (attended by telephone) were notified of the IJs for F-880, F-835, F-837, F-867, F-684, and F-726 on 11/13/2024 at 9:42 PM in the Common Area/Recreation Area.
The facility was cited Immediate Jeopardy at F-726 at a scope and severity of L.
An extended survey was conducted on 11/14/2024-11/15/2024.
The Immediate Jeopardy began on 8/9/2024 and is ongoing.
The facility is required to submit a Plan of Correction.
The findings include:
Review of the undated facility policy titled, Competent & [and] Sufficient Staff, revealed .to provide sufficient staff with appropriate competencies .skill sets to assure resident safety .attain or maintain the highest practicable physical, mental and psychosocial well-being of each resident .Providing care includes, but is not limited to, assessing, evaluating, planning and implementing resident care plans and responding to resident's needs .The facility must ensure .nurse aides are able to demonstrate competency in skills .techniques necessary to care for residents' needs .The facility must ensure .licensed nurses have the specific competencies .skill sets necessary to care for resident's needs .
Review of the undated facility policy titled, COVID-19 Management of Residents, which referenced the 5/25/2023 CDC guidelines revealed .The facility will not have a dedicated COVID-19 unit unless the number of positive residents warrant .the facility will place a COVID-19 positive resident in a single room with appropriate isolation signage and staff wearing N95 respirator, eye protection, gown, and gloves upon entry to the room .dedicated staff, to care for residents with COVID-19 .the door will be kept closed .resident will be monitored every four hours for .symptoms, vital signs, oxygen saturation .and respiratory exam .residents will .wear source control until symptoms resolve .
Review of the facility's Director of Nursing job description revealed .The Director of Nursing manages and directs the day-to-day functions of the Nursing Department in accordance with established policies, procedures, and practices that comply with federal, state, and local regulations .ensures .that staff are qualified and trained .
Review of the facility's ADON (Assistant Director of Nursing) Staff Development Coordinator job description revealed .Assisting DON in all aspects of resident care, nursing services, and directing personnel within the facility .Initiates the development of policies .procedures that govern nursing services .Responsible for staff performance .Designs, plans, and provides educational programs on all shifts .for all departments .Participates in the staff evaluation process .observation of employee performance .Provides general facility orientation to all new employees and ongoing in-service education .Audit documentation for errors or inconsistencies .Inventory, identify .monitor .supplies .
Review of the facility's RN (Registered Nurse) Supervisor job description revealed .over-see .nurses and CNAs [Certified Nursing Assistant] are providing proper care to .residents .
Review of the facility's Licensed Practical Nurse (LPN) Supervisor job description revealed .provides nursing services following the patient's treatment plan .physician's directions .supervises .nursing assistants on duty .Ensures quality .safe delivery of nursing services to patients .Uses equipment .supplies effectively .efficiently .Assist patients with personal hygiene .Provides nursing care following established nursing service objectives and standards. Ensures .all safety .infection control practices are followed .
Review of the facility's Registered Nurse (RN) job description revealed .Ensures quality .safe delivery of nursing services to patients .Implements plan of care formulated by physicians .Uses equipment .supplies .effectively .efficiently .Ensuring all work areas .resident's rooms are maintained in accordance with safety and sanitation standards .Administering professional nursing practice services .
Review of the facility's Certified Nursing Assistant (CNA) job description revealed .Assists .in provision of basic care for residents .Demonstrate performance .Demonstrate knowledge of disease entities .Ensure .asepsis is carried out during treatments .procedures .
Review of the facility's Personal Care Aide job description revealed .has complete personal care training .competent to perform assigned functions of personal care to the client .Assists clients with personal hygiene .Assist clients in the use of toilet facilities .Meal preparation .feeding .
Review of the facility's Facility Administrator job description revealed .plans, coordinates and manages all services and employees of facility .is responsible for the overall direction, coordination and evaluation of all care and services provided .Ensures .each employee working at the .facility has a Job Description, has read it, understands it, and complies with it in full .Assists with hiring .providing orientation/training .of sufficient .qualified staff to carry out all programs .services .Holds department leaders accountable .Oversees . helps develop education, in-services training .program development .
Review of the Medical Director Services Agreement and Description of Services dated 6/1/2021, revealed .Review resident cases .for quality of care .quality of life concerns .take steps to resolve situations .Participate in Facility staff meetings concerning infection control, pharmacy services .Review, approve, implement, and assist in the development of clinical, nursing .resident care policies .procedures .Review, consider .act upon consultant recommendations pertaining to .resident care .Attend Quality Assessment and Assurance meetings .Advise .direct quality improvement plans .Assist in identification .implementation of .staff educational needs .provide information to staff .
Review of the CDC guidance titled, Implementation of Personal Protective Equipment (PPE) Use in Nursing Homes to Prevent Spread of Multidrug-resistant Organisms (MDROs), dated 4/2/2024, revealed .Enhanced Barrier Precautions (EBP) are an infection control intervention designed to reduce transmission of resistant organisms that employs targeted gown and glove use during high contact resident care activities .Effective implementation of EBP requires staff training on the proper use of personal protective equipment (PPE) and the availability of PPE and hand hygiene supplies at the point of care .Examples of high-contact resident care activities requiring gown and glove use for Enhanced Barrier Precautions include: Dressing .Bathing/showering .Transferring .Providing hygiene .Changing linens .Changing briefs or assisting with toileting .Device care or use: central line, urinary catheter, feeding tube, tracheostomy/ventilator .Wound care: any skin opening requiring a dressing .When implementing .Enhanced Barrier Precautions, it is critical to ensure that staff have awareness of the facility's expectations about hand hygiene and gown/glove use, initial and refresher training, and access to appropriate supplies. To accomplish this .Post clear signage on the door or wall outside of the resident room indicating the type of Precautions and required PPE (e.g., gown and gloves) .Enhanced Barrier Precautions, signage should also clearly indicate the high-contact resident care activities that require the use of gown and gloves .Incorporate periodic monitoring .assessment of adherence to determine the need for additional training and education .
Review of the CDC guidance titled, Viral Respiratory Pathogens Toolkit for Nursing Homes, dated 10/28/2024, revealed .HCP [Healthcare Personnel] who enter the room of a resident with sign and symptoms of SARS-CoC-2 [Covid-19] infection should use a NIOSH [National Institute for Occupational Safety and Health]-approved particulate respirator with N95 filters or higher, gown, gloves, and eye protection .
Review of an undated and untitled document provided by the Infection Preventionist (IP) on 11/3/2024 revealed a list of residents in the facility who were in droplet isolation for COVID-19 included Residents #102, #507, #508, and #509.
Review of the medical record revealed Resident #102 was admitted to the 100 Hallway on 10/2/2024 with diagnoses including Cerebral Infarction, Chronic Obstructive Pulmonary Disease, Hemiplegia and Hemiparesis Affecting Right Dominant Side, and Hypertension.
Review of the Physician's Order for Resident #102 dated 10/28/2024, revealed .Isolation Droplet precautions .due to positive covid 19 [COVID-19] test. Mask, googles [goggles], gloves, gown, face shield .
Review of the medical record revealed Resident #507 was admitted to the 100 Hallway on 10/11/2024 with diagnoses including Wedge Compression Fracture of the First Lumbar Vertebra, Osteoporosis, Dementia, Anxiety, and Hypothyroidism.
Review of the Physician's Order for Resident #507 dated 10/25/2024, revealed .Isolation Droplet precautions .due to positive covid 19 test. Mask, googles, gloves, gown, face shield .
Review of the medical record revealed Resident #508 was admitted to the 100 Hallway on 10/15/2024 with diagnoses including Cerebral Infarction, Congestive Heart Failure, and Major Depressive Disorder.
Review of a Physician's Order for Resident #508 dated 10/28/2024, revealed .Isolation Droplet precautions .due to positive covid 19 test. Mask, googles, gloves, gown, face shield .
Review of the medical record revealed Resident #509 was admitted to the 100 Hallway on 10/30/2024 with diagnoses including Fracture of Right Humerus, COVID 19, Anxiety, Pressure Ulcer of Sacral Region Stage 4, Chronic Respiratory Failure, and Adult Failure to Thrive.
Review of the Physician's Order for Resident #509 dated 10/31/2024, revealed .Isolation Droplet precautions .due to positive covid 19 test. Mask, googles, gloves, gown, face shield .
Review of a list of all residents on EBP provided by the facility during the survey dates 11/3/2024-11/15/2024, revealed 4 residents on the 100 Hallway, 12 residents on the 200 Hallway, 9 residents on the 300 Hallway, and 10 residents on the 400 Hallway.
Review of an undated and untitled document provided by the IP on 11/3/2024 revealed a list of residents in the facility who were EBP:
Resident #13- EBP for wound
Resident #24- EBP for ESBL (Extended-Spectrum Beta-Lactamase- a type of bacterial infection that's resistant to many antibiotics)
Resident #25- EBP for ESBL
Resident #52- EBP for wound and ESBL
Resident #56-EBP for indwelling urinary device
Resident #83- EBP for wound, indwelling urinary device, and ESBL
Review of the medical record revealed Resident #13 was admitted to facility on 5/13/2024 with diagnoses including Depression, Restless Leg Syndrome, and Anxiety.??
?
Review of a Physician's Order for Resident #13 dated 5/17/2024, revealed .resident in enhanced barrier precautions . for a wound.?
Review of the comprehensive care plan for Resident #13 dated 5/17/2024, revealed .enhanced barrier precautions . for a wound.
Review of the medical record revealed Resident #24 was admitted to the facility on [DATE] with diagnoses including Unsteadiness on Feet, Epilepsy, and Dementia.
Review of a Physician's Order for Resident #24 dated 8/19/2024, revealed resident inenhanced [in enhanced] barrier precautions . for ESBL of the urine.
Review of the comprehensive care plan for Resident #24 dated 9/17/2024, revealed .enhanced barrier precautions . for ESBL of the urine.
Review of the medical record revealed Resident #25 was admitted to the facility on [DATE] with diagnoses including Difficulty Walking, Breast Cancer, and Hypertension.
Review of a Physician's Order for Resident #25 dated 4/5/2024, revealed .Resident in Enhanced Barrier precautions . for ESBL in the urine.
Review of the comprehensive care plan for Resident #25 revised 11/4/2024, revealed .enhanced barrier precautions .ESBL .
Review of the medical record revealed Resident #52 was admitted to the facility on [DATE] and readmitted on [DATE] with diagnoses including Intellectual Disabilities, Autistic Disorder, and Pain.
Review of a Physician's Order for Resident #52 dated 7/12/2024, revealed .resident in enhanced barrier precautions . for a wound and ESBL of the urine.
Review of the comprehensive care plan for Resident #52 dated 9/17/2024, revealed .enhanced barrier precautions . for a wound and ESBL of the urine.
Review of the medical record revealed Resident #56 was admitted to the facility on [DATE] with diagnoses including Sepsis, Difficulty Walking, Arthritis, Gout, Cough, and Depression.
Review of a Physician's Order for Resident #56 dated 7/12/2024, revealed .resident in enhanced barrier precautions . for an indwelling urinary catheter.
Review of the medical record revealed Resident #83 was admitted to the facility on [DATE] with diagnoses including Parkinson's Disease, Lack of Coordination, Depression, Pain, and Anxiety.
Review of a Physician's Order for Resident #83 dated 5/24/2024, revealed .Resident in Enhanced Barrier precautions . for a wound, an indwelling urinary catheter, and ESBL in the urine.
Review of the comprehensive care plan for Resident #83 dated 11/10/2024, revealed .Enhanced barrier precautions . for a wound, an indwelling urinary catheter, and ESBL.
During an observation on 11/3/2024 at 11:30 AM, Residents #13, #25, #56 and #83 had an 8 and half inch by 11-inch sign on their door which read ENHANCED BARRIER PRECAUTIONS (EBP) .EVERYONE MUST .Clean their hands, including before entering and leaving the room .PROVIDERS AND STAFF MUST ALSO .Wear gloves and gown for the following .Transferring .Changing Linens .Providing Hygiene .Do not wear the same gown and gloves for the care of more than one person .
During a meal observation on 11/3/2024 at 12:10 PM, Patient Care Assistant (PCA) O removed a meal tray from a tray cart, entered Resident #13's room, adjusted the resident's belongings, delivered the meal tray, exited the room, returned to the tray cart, and removed an additional meal tray without performing hand hygiene. PCA O entered Resident #25's room, adjusted the resident's belongings on the bedside table, delivered the meal tray, exited the room, returned to the tray cart, and removed an additional meal tray without performing hand hygiene. PCA O entered Resident #56's room, adjusted the resident's belongings, delivered the meal tray, exited the room, returned to the tray cart and removed an additional meal tray without performing hand hygiene. PCA O entered Resident #83's room, adjusted the resident's belongings, delivered the meal tray, exited the room, and returned to the tray cart. PCA O did not perform hand hygiene prior to entering and prior to exiting the 4 residents' rooms.
During an interview on 11/3/2024 at 12:32 PM, Resident #25 stated her hands were washed by PCA O with a washcloth prior to receiving her lunch tray. Resident #25 stated PCA O was not wearing a gown or gloves during hand hygiene.
During an interview on 11/3/2024 at 12:35 PM, Resident #56 stated his hands were washed by PCA O with a washcloth prior to receiving his lunch tray. Resident #56 stated PCA O was not wearing a gown or gloves during hand hygiene.
During an interview on 11/3/2024 at 12:40 PM, Resident #83 stated her hands were washed by PCA O with a washcloth prior to receiving her lunch tray. Resident #83 stated PCA O was not wearing a gown or gloves during hand hygiene.
During a meal observation on 11/3/2024 at 12:42 PM, revealed Paid Feeding Assistant (PFA) DD delivered a meal tray to Resident #508 on the 100 Hallway, who was in droplet isolation precautions. PFA DD did not wear the appropriate PPE (N95 mask, gown, gloves, and eye/face shield protection) prior to entering the droplet isolation room.
During an observation on 11/3/2024 at 12:45 PM, Risk Manager LPN M entered Resident #509's room on the 100 Hallway, who was in droplet isolation precautions, without wearing PPE prior to entering the room, adjusted the bedside table and spoke with the resident with the door open. Then Risk Manger LPN M exited the room, accessed the clean PPE supplies from the over the door PPE storage bin, donned (applied) an N95 mask, disposable shoe covers, and an isolation gown, reentered the room, and closed the door.
During an interview on 11/3/2024 at 12:56 PM, PCA O stated the EBP sign was only for the CNAs. PCA O stated she did not have to wash her hands before entering and exiting rooms with EBP signage because she did not provide any care. PCA O confirmed she did not wear a gown or gloves when she provided hand hygiene to residents and restated the EBP signage is for CNAs. PCA O stated she did not have to wear a gown in any EBP rooms for any of her job duties which included meal tray deliveries and bed linen changes. PCA O also stated, .I would not know how to tell . which resident the EBP signage is for when a room has more than 1 resident.
During an observation on 11/4/2024 at 7:52 AM, CNA Z entered Resident #509's (COVID-19 positive on admission [DATE]) room without wearing PPE and performed hand hygiene on the resident before the breakfast meal, then exited the room.
During an observation on 11/4/2024 at 7:53 AM, CNA Z entered Resident #508's (COVID-19 positive 10/28/2024) room without wearing PPE and performed hand hygiene on the resident before the breakfast meal, then exited the room.
During an interview on 11/4/2024 at 9:00 AM, LPN PP and CNA Z referred to the 100 Hallway as the facility's COVID-19 unit. LPN PP and CNA Z stated they looked for isolation barrels and signage on the resident's doors to identify residents on transmission-based precautions. LPN PP and CNA Z stated they were unaware residents in droplet isolation precautions required closed doors to prevent the transmission of respiratory infections and stated they had not been educated to keep the COVID-19 resident doors closed during a COVID outbreak. CNA Z stated they are required to complete education courses on the facility's computer-based learning system, they have meetings at the nurses' station where the nurses will hand staff a piece of paper and tell us to sign. LPN PP stated she was hired sometime in January 2024 and did not know how to log onto the computer-based learning system and had not completed any online education.
During an interview on 11/4/2024 at 3:45 PM, the IP, with the ADON present, confirmed they were responsible for staff education, which was provided with new employee orientation, annual skills fair (last conducted 11/2023), re-education with updates, and an in-service book located at the nurses' station. The IP and ADON expressed staff are informed of which residents are in transmission-based precautions by department heads after daily huddle meetings. Continued interview with the IP revealed she stated the facility's policies for infection control were more stringent than the CDC guidelines, but she was unable to provide an example of how the facility's policies were more stringent than the CDC guidelines and acknowledged no changes to the facility's current policy had occurred. The IP stated the facility's infection control policies were provided to her through the corporate office and she had received updates from the local health department. The IP verified and confirmed the infection control policies the facility followed were dated 5/2023. The IP confirmed she was unaware of what the current CDC guidelines were and had not been to the CDC website. The IP stated staff are required to wear a gown, gloves, goggles, and N95 mask when entering a droplet isolation room with COVID-19 positive residents. The IP also stated staff are required to wear the appropriate PPE based on the type of isolation and signage posted on the door and she expected staff to change PPE and perform hand hygiene between resident care. The IP was informed of multiple observations and interviews with staff which revealed staff had no knowledge of transmission-based precautions, PPE, types of isolation, COVID-19 precautions, and how to identify residents in isolation. The IP confirmed that was deficient practice and stated employees of the facility should have knowledge of infection control practices prior to providing resident care.
During an interview on 11/4/2024 at 5:45 PM, on the 300 hallway, LPN JJ was asked how she knew residents were in EBP. LPN JJ stated EBP was a sign on the resident's door used to alert staff that the resident needed barrier cream. When LPN JJ was asked if she knew what EBP was and what it meant to her she stated that is when a resident needs barrier cream applied to their peri area (an area of the pelvic cavity between the genitals and the anus). LPN JJ stated, .I would .look for a tube of barrier cream in the room .if the resident had a sign for EBP with no barrier cream in the room .then the resident did not need any barrier cream . The LPN stated EBP signage was not a communication tool used to alert staff for required PPE usage in the room for resident care.
During an interview on 11/5/2024 at 10:43 AM, on the 300 hallway, PFA Q stated the EBP signage was only for nurses and CNAs. PFA Q stated she did not have to wear a gown in any EBP rooms for any of her job duties which included meal tray deliveries, assisting residents with their meals in their rooms, performing hand hygiene on residents, changing bed linens, and removing soiled linens and trash from rooms.
During an interview on 11/5/2024 at 10:45 AM, on the 300 hallway, LPN R stated 11/5/2024 was her second day at the facility. LPN R stated she received education on infection control prior to starting and stated, .I can't remember what all they [Administration] said .they did not have a class .they gave me a bunch of papers to read .and I signed a paper saying that I received training . LPN R also stated she did not know what the requirements were for residents on EBP, stated both residents in a room were on EBP if an EBP sign was on the door and stated .since EBP is not really true isolation you could wear the same gown and gloves for both residents .
During an interview on 11/5/2024 at 10:55 AM, on the 300 hallway, PFA S stated EBP signage was only for the CNAs, and she did not have to wear a gown or do hand hygiene before entering an EBP room. PFA S stated she did not have to wear a gown in any EBP rooms for any of her job duties which included meal tray deliveries, assisting residents with their meals in their rooms, performing hand hygiene on residents, changing bed linens, and removing soiled linens and trash from rooms. PFA S also stated she occasionally would help nurses bathe residents, empty urinals, and assist in turning residents. PFA S stated she could not remember a specific time but stated she routinely provided resident care for Resident #13, Resident #25, Resident #52, Resident #56, and Resident #53 without wearing a gown.
During an interview and observation on 11/5/2024 at 2:52 PM, on the 300 hallway, CNA T stated she was trained on infection control recently and stated, .Enhance Barrier Precautions is a new word for me .I have not heard this before . CNA T observed an EBP sign at the 300-hall nurses' station and stated this signage meant CNAs and Nurses had to wash their hands, wear gloves, wear a gown when going in rooms and stated it [PPE] had to be discarded and hands washed before leaving the room. CNA T stated she had the entire 300-Hall and did not have any rooms on EBP. Further observation of the 300-Hallway revealed 7 rooms with EBP signage in place.
During an interview on 11/6/2024 at 9:02 AM, Risk Manager LPN M confirmed he failed to follow infection control practices and don the appropriate PPE for droplet isolation when he entered Resident #509's room on the 100 Hallway on 11/3/2024.
During an observation on 11/6/2024 at 2:10 PM, Housekeeper GG was in Resident #102's (COVID-19 positive 10/28/2024) room sweeping the floor. Housekeeper GG was observed wearing a surgical face mask only and did not wear any additional PPE. Continued observation revealed signage for Droplet Precautions posted to the wall beside the resident's door.
During an interview on 11/6/2024 at 3:15 PM, the MD stated he had previously voiced concerns to the facility's administration regarding the staff's non-compliance with PPE usage on the 100 Hallway and stated the staff were .undermining their own safety . The MD stated the facility's response to his concern was to increase the supply of PPE to multiple resident rooms (including non-COVID positive rooms) which contributed to the staff confusion regarding the identification of residents on transmission- based precautions. The MD stated due to the incorrect and inconsistent transmission-based precaution signage posted outside resident rooms, he stated he was also confused and had to seek clarification from the staff prior to entering the rooms on the 100 Hallway. The MD stated, .one day I came to see a resident and he had 3 different signs on the door, and I thought to myself .what do I wear .and if I am a doctor and I don't know what to wear .how do the staff know what to wear . The MD also stated he had historically instructed the nurses to keep the doors closed for residents with COVID-19 infections to help mitigate the spread of the infection unless there was a safety concern.
During an interview on 11/7/2024 at 10:00 AM, on the 400 hallway, PFA RR was unaware of what EBPs were and stated she had never been educated. PFA RR stated she would wear gloves and gown with those residents.
During an interview and facility policy review on 11/12/2024 at 10:12 AM, in the conference room, with the VPCS, VPRC, DON, and the Administrator, revealed the facility identified they were not following the current CDC guidelines to prevent and control the spread of COVID-19. The Administrator stated the facility had allowed COVID-19 positive employees to work in accordance with the CDC guidelines for contingency staffing and did not realize the emergency staffing waiver had ended. The Administrator stated the facility had re-educated all the managers on 11/11/2024 on the current CDC guidelines. Review of the education material used to re-educate the staff referenced the outdated 2023 CDC guidelines.
During an interview and CDC guidelines review on 11/13/2024 at 3:32 PM, with the Administrator and VPCS, revealed the CRCO is responsible for updating the facility's COVID-19 policies and confirmed these outdated policies were used to re-educate staff. Further interview revealed the facility's new COVID-19 policies were revised (date unknown) and referenced the outdated 2023 CDC guidelines.
During an interview on 11/13/2024 at 7:55 PM, the Administrator confirmed the facility had some areas of improvement to address regarding infection prevention and control practices (to include the prevention and control of COVID-19 and adherence to isolation with PPE usage for the employees) and competent staffing.
Refer to F-684, F-835, F-837, F-867, and F-880
CRITICAL
(L)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Administration
(Tag F0835)
Someone could have died · This affected most or all residents
⚠️ Facility-wide issue
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, Centers for Disease Control and Prevention (CDC) recommendations and guidance review, job descr...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, Centers for Disease Control and Prevention (CDC) recommendations and guidance review, job description review, facility assessment review, and interviews, the facility's Administration failed to ensure current CDC guidelines were utilized to prevent and control the spread of COVID-19 to the residents and employees. The facility's Administration failed to ensure the staff were competent and knowledgeable on Enhanced Barrier Precautions (EBP) and COVID-19 isolation practices which included use of appropriate Personal Protective Equipment (PPE) for potentially contagious residents. The facility's Administration failed to accurately identify residents with an active diagnosis of COVID-19. The facility's Administration failed to ensure the completion of COVID-19 testing of the staff during the COVID-19 outbreaks from 8/2024-11/2024. The facility's Administration failed to ensure COVID-19 positive employees and residents were quarantined for the required isolation time frame recommended by the CDC, and the facility's Administration allowed COVID-19 positive employees to provide care for COVID-19 negative residents. The facility's Administration failed to ensure an effective QAPI program which reviewed systems and processes with ongoing tracking and monitoring of active COVID-19 infections in the facility. The facility's Administration failed to recognize, in QAPI, repeated systemic failures to assess, identify, and implement the residents' need for isolation precautions related to COVID-19 that resulted in multiple COVID-19 outbreaks in the facility. The facility's Administration failed to ensure the facility carried out physician orders related to vital sign monitoring for 36 of 40 COVID-19 positive residents during a COVID-19 outbreak to ensure any acute clinical changes were addressed and monitored. The facility's Administration failed to ensure treatment, care, and services related to medication administration for a resident at risk for aspiration were implemented in accordance with professional standards of practice.
These failures by the facility's Administration resulted in an Immediate Jeopardy (a situation in which the provider's noncompliance with one or more requirements of participation has caused, or is likely to cause, serious injury, harm, impairment, or death to a resident), which had had the likelihood to affect all 99 residents in the facility.
The Administrator, Director of Nursing (DON), [NAME] President of Operations (VPO), [NAME] President of Life Safety and Environmental Compliance (VPLSEC), and [NAME] President of Clinical Services (VPCS) (attended in person) and the [NAME] President of Regulatory Compliance (VPRC) and Chief Operating Officer (COO) with the Chief Regulatory Compliance Officer (CRCO) (attended by telephone) were notified of the IJs for F-684, F-726, F-835, F-837, F-867, and F-880, on 11/13/2024 at 9:42 PM in the Common Area/Recreation Area.
The facility was cited Immediate Jeopardy at F-835 at a scope and severity of L.
The facility was cited Immediate Jeopardy at F684 at a scope and severity of K which is substandard quality of care
The facility was cited Immediate Jeopardy at F726, F-837, F867, F-880 at a scope and severity of L.
An Extended survey was conducted onsite from 11/14/2024-11/15/2024.
The IJ began on 8/9/2024 and is ongoing.
The facility is required to submit a Plan of Correction (POC).
The findings include:
Review of the facility's policy titled, COVID-19 GENERAL TESTING POLICY,undated, revealed .Staff with symptoms or signs of COVID-19 .will be tested as soon as possible and will be restricted from the facility pending the results of COVID-19 testing .Residents who have signs and symptoms of COVID-19 .will be tested .be placed on transmission-based precautions (TBP) .DURING COVID-19 OUTBREAK .Facilities will investigate an outbreak using contact tracing or a broad-based approach .Broad-based approach .used if the facility is unable to conduct contract tracing .Broad-based approach includes testing every 3-[to] 7 days until no more positive cases identified for 14 days .if additional cases are identified after testing a unit, floor, or specific area .the facility will expand testing to facility-wide . Further review revealed the policy referenced the CDC guidance dated 5/25/2023.
Review of the facility's policy titled, COVID-19 Management of Residents, undated, revealed .The facility will not have a dedicated COVID-19 unit unless the number of positive residents warrant .the facility will place a COVID-19 positive resident in a single room with appropriate isolation signage and staff wearing N95 respirator, eye protection, gown, and gloves upon entry to the room .dedicated staff, to care for residents with COVID-19 .the door will be kept closed .resident will be monitored every four hours for .symptoms, vital signs, oxygen saturation .and respiratory exam .residents will .wear source control until symptoms resolve . Further review revealed the policy referenced the CDC guidance dated 5/25/2023.
Review of the CDC's guidance titled, Infection Control Guidance: SARS-CoV-2, dated 6/24/2024, revealed, .The recommendations in this guidance continue to apply after the expiration of the federal COVID-19 Public Health Emergency [5/11/2023] .To provide the greatest assurance that someone does not have SARS-CoV-2 infection .Establish a Process to Identify and Manage Individuals with Suspected or Confirmed SARS-CoV-2 Infection .Ensure everyone is aware of recommended IPC [infection prevention and control] practices in the facility . (The CDC published this recommendation on 6/24/2024 and was the guidance the facility should have followed from 6/24/2024 to present).
Review of the CDC guidance titled, Viral Respiratory Pathogens Toolkit for Nursing Homes, dated 10/28/2024, revealed .Educate .Ensure everyone .including HCP [healthcare providers], are aware of recommended IPC [infection prevention and control] practices in the facility .When an acute respiratory infection is identified in a resident or HCP .take rapid action to prevent the spread to others in the facility .Apply appropriate Transmission-Based Precautions for symptomatic residents .HCP who enter the room of a resident with signs or symptoms of an unknown respiratory viral infection that is consistent with SARS-CoV-2 [COVID-19] infection should adhere to Standard Precautions .use a NIOSH-approved particulate respirator with N95 filters or higher, gown, gloves, and eye protection (i.e. [example], goggles or a face shield that covers the front and sides of the face) .Develop sick leave policies for HCP .with public health guidance to discourage presenteeism .allow HCP with respiratory infection to stay home for the recommended duration of work restriction .Test anyone with respiratory illness signs or symptoms .Investigate for potential respiratory virus spread among residents and HCP .Perform active surveillance to identify any additional ill residents or HCP using symptom screening .evaluating potential exposures .testing of exposed individuals is recommended, even if they are asymptomatic .Make initial attempts to control limited spread .If SARS-CoV-2 transmission is occurring .Consider implementing broad-based testing as opposed to only testing close contacts to identify asymptomatic infection .
Review of the Administrator's Job Description signed and dated by the Administrator on 10/3/2022, revealed .plans, coordinates and manages all services and employees of [the] facility .responsible for .coordination and evaluation of all care and services provided .manages compliance with all policies and procedures .oversees and help develop education .ensure .outcomes .policies and procedures of Nursing services meet .regulations .services are provided in accordance with [the] resident's plan of care .drives .ongoing activities of the Quality Improvement Committee (QAPI) .
Review of the DON's Job Description signed and dated by the DON on 7/10/2024, revealed .manages and directs the day-to-day functions of the Nursing Department in accordance with policies .that comply with federal, state, and local regulations .ensures .staff are qualified and trained .ensures that each patient's needs are assessed and .treatment plan is developed for nursing care .ensures that required documentation is complete .
Review of the facility's assessment dated [DATE], revealed .purpose of the assessment is to determine what resources are necessary to care for residents competently .use this assessment to make decisions about your direct care staff needs .capabilities to provide services to the residents .list the types of care that your resident population requires and that you provide for your resident population .infection prevention and control .identification and containment of infections .prevention of infections .staff training .infection control .isolation .use of personal protective equipment [PPE] .policies and procedures are established in compliance with state and federal regulations as well as CDC guidelines .issues identified facility or resident specific are made [as a multidimensional approach in] QAPI [Quality Assurance and Performance Improvement] .
Investigation revealed the facility experienced two COVID-19 outbreaks. Documentation revealed during the first outbreak on 8/9/2024-10/11/2024 that 28 residents (Residents #96, #31, #45, #33, #11, #64, #609, #93, #15, #510, #611, #80, #612, #506, #615, #613, #614, #54, #68, #27, #53, #12, #95, #74, #30, #37, #3, and #89) and 15 employees tested positive for COVID-19. During the second outbreak which began on 10/19/2024 through present, revealed 10 residents (Residents #99, #617, #103, #72, #34, #618, #507, #508, #102, and #94) and 5 employees tested positive for COVID-19. The facility allowed 17 of the 20 total COVID-19 positive employees to return to work before the required isolation time frame recommended by CDC guidance, which increased the likelihood that contagious employees could spread the COVID-19 infection to all residents in the facility. The facility failed to accurately identify COVID-19 positive residents and residents who required EBP with appropriate signage and tracking of potentially infectious diseases. Further investigation revealed employees were non-compliant with PPE usage in the provisions of care for residents in Enhanced Barrier Precautions (EBP) rooms for 6 of 26 residents (Resident #13, #25, #56, #83, #24, #52).
During an interview and facility policy review on 11/12/2024 at 10:12 AM, in the conference room, with the VPCS, VPRC, DON, and the Administrator, the facility identified they were not following the current CDC guidelines to prevent and control the spread of COVID-19. The ADM stated the facility had allowed COVID-19 positive employees to work in accordance with the CDC guidelines for contingency staffing and did not realize the emergency staffing waiver had ended. The Administrator stated the facility had re-educated all the managers on 11/11/2024 on the current CDC guidelines. Review of the education material used to re-educate the staff referenced the outdated 2023 CDC guidelines.
During an interview and CDC guidelines review on 11/13/2024 at 3:32 PM, with the Administrator and VPCS, revealed the CRCO was responsible for updating the facility's COVID-19 policies and confirmed these outdated policies were used to re-educate staff. Further interview revealed the facility's new COVID-19 policies were revised (date unknown) referenced the outdated 2023 CDC guidelines.
During an interview on 11/15/2024 at 3:00 PM, the Corporate Human Resources and VPRC verified and confirmed Licensed Practical Nurse (LPN) D, Registered Nurse (RN) B, LPN MM, Laundry NN, and LPN OO worked after testing positive for COVID-19 and were not quarantined for the recommend CDC guidance, which had the potential to cause or increase the 2 COVID-19 outbreaks.
During an interview on 11/16/2024 at 7:56 PM, the DON confirmed the facility failed to perform facility wide employee testing and adhere to the recommended quarantine time during the COVID-19 outbreaks, failed to track and trend all facility COVID-19 cases, and confirmed the facility failed to ensure COVID-19 positive residents were quarantined according to CDC guidance.
Refer to F-880
Investigation revealed the facility failed to ensure the nursing staff were knowledgeable and had a full understanding on the identification of residents on 3 of 4 hallways (200, 300, and 400 hallways) on EBP, active COVID-19 residents on 1 of 4 hallways (100 hallway) and implemented EBP, the appropriate use of (PPE) for isolation rooms to prevent and control the spread of COVID-19, and other infectious organisms. The facility failed to wear appropriate PPE for residents in EBP rooms for 6 of 26 residents (Resident #13, #25, #56, #83, #24, #52) reviewed for EBP.
Refer to F-726
The facility failed to ensure that services provided met professional standards of quality and acceptable standards of clinical practice for not obtaining vital signs per physician orders for residents with an active COVID-19 diagnosis for 36 of 40 residents (Resident #96, #45, #31, #33, #11, #609, #64, #93, #15, #510, #612, #611, #80, #506, #613, #615, #54, #68, #27, #53, #12, #95, #74, #3, #30, #37, #617, #34, #618 #72, #103, #507, #102, #508, #619, and #509) of 40 residents reviewed and 1 of 6 residents (Resident #99) reviewed for medication administration.
Refer to F-684
Review of the QAPI meeting minutes dated 11/2023-10/2024, revealed the QAPI committee and the Governing Body failed to identify infection control deficiencies related to unsafe infection control practices with accurate identification of COVID-19 positive residents to prevent the spread of COVID-19 which resulted in multiple COVID-19 outbreaks, non-compliance with isolation procedures, and the practice of allowing COVID-19 positive employees to provide care to Non-COVID-19 positive residents. The facility's Administration failed to recognize the need to address staff competency related to infection control practices to address non-compliance with PPE usage for care provisions to residents who were potentially contagious and failed to implement corrective actions to address the deficient practice with physician's orders compliance related to vital sign monitoring and ensuring professional standards of care were followed for an unsafe practice of medication administration for a resident at risk for aspiration.
Refer to F-837 and F-867
During an interview on 11/6/2024 at 3:15 PM, the Medical Director stated he had voiced previous concerns to the facility administration regarding staff PPE usage and infection control practices. The Medical Director stated he was confused and would seek clarification from the staff prior to entering resident rooms because of the facility's inconsistent use and incorrect signage use for residents with transmissions-based precautions. The Medical Director stated he expected the facility to follow the CDC guidelines (current and updated) for the management of COVID-19 outbreaks. The Medical Director stated he had instructed the nurses to keep the doors closed for residents with COVID-19 infections and stated keeping the resident's door closed would mitigate the spread and control of COVID-19. The Medical Director stated the facility did not implement his professional recommendations in QAPI meetings for infection control practices and guidance during the outbreaks.
During an interview on 11/13/2024 at 7:55 PM, the Administrator stated the facility had some areas of improvement to address in QAPI regarding infection prevention and control practices (to include the prevention and control of COVID-19 and adherence to isolation with PPE usage for the employees), competent staffing, and ensuring professional standards of care are met related to safety with medication administration and compliance with physician orders.
CRITICAL
(L)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0837
(Tag F0837)
Someone could have died · This affected most or all residents
⚠️ Facility-wide issue
Based on facility policy review, review of the Centers for Disease Control and Prevention (CDC) recommendations and guidance, job description review, facility assessment review, and interviews, the Go...
Read full inspector narrative →
Based on facility policy review, review of the Centers for Disease Control and Prevention (CDC) recommendations and guidance, job description review, facility assessment review, and interviews, the Governing Body failed to provide oversight to Administration to ensure current CDC guidelines were utilized to prevent and control the spread of COVID-19 to the residents and employees. The Governing Body failed to provide oversight to Administration to ensure the staff were competent and knowledgeable on Enhanced Barrier Precautions (EBP) and COVID-19 isolation practices which included use of appropriate Personal Protective Equipment (PPE) for potentially contagious residents. The Governing Body failed to provide oversight to Administration to accurately identify residents with an active COVID-19 infection. The Governing Body failed to provide oversight to Administration to ensure COVID-19 testing of the staff was completed per CDC guidelines during the COVID-19 outbreaks from 8/2024-11/2024. The Governing Body failed to provide oversight to Administration to ensure COVID-19 positive employees and residents were quarantined for the required isolation time frame recommended by the CDC which resulted in COVID-19 positive employees provided care to COVID-19 negative residents. The Governing Body failed to provide oversight to Administration to ensure an effective, date-driven Quality Assurance and Performance Improvement (QAPI) program which reviewed systems and processes and failed to ensure the facility conducted ongoing tracking with monitoring of active COVID-19 infections in the facility. The Governing Body failed to provide oversight to Administration to ensure the QAPI Committee recognized repeated systemic failures to assess, identify, and implement the residents' need for isolation precautions related to COVID-19 that resulted in multiple COVID-19 outbreaks in the facility. The Governing Body failed to provide oversight to Administration to ensure the facility followed physician orders related to vital sign monitoring for 36 of 40 COVID-19 positive residents during a COVID-19 outbreak to ensure any acute clinical changes were addressed and monitored. The Governing Body failed to provide oversight to Administration to ensure treatment, care, and services related to medication administration for a resident at risk for aspiration were implemented in accordance with professional standards of practice.
The failure of the Governing Body to provide oversight to the facility's Administration resulted in an Immediate Jeopardy (a situation in which the provider's noncompliance with one or more requirements of participation has caused, or is likely to cause, serious injury, harm, impairment, or death to a resident), which had had the likelihood to affect all 99 residents in the facility.
The Administrator, Director of Nursing (DON), [NAME] President of Operations (VPO), [NAME] President of Life Safety and Environmental Compliance (VPLSEC), [NAME] President of Clinical Services (VPCS) (attended in person) and the [NAME] President of Regulatory Compliance (VPRC) and Chief Operating Officer (COO) with the Chief Regulatory Compliance Officer (CRCO) (attended by telephone) were notified of the IJs for F-880, F-835, F-837, F-867, F-684, and F-726 on 11/13/2024 at 9:42 PM in the Common Area/Recreation Area.
The facility was cited Immediate Jeopardy at F-837 at a scope and severity of L.
The facility was cited Immediate Jeopardy at F-684 at a scope and severity of K which is substandard quality of care.
The facility was cited Immediate Jeopardy at F-726, F-835, F867, and F-880 at a scope and severity of L.
An Extended survey was conducted onsite from 11/14/2024 through 11/15/2024.
The IJ began on 8/9/2024 and is ongoing.
The facility is required to submit a Plan of Correction (POC).
The findings include:
Review of the facility's undated policy titled, Quality Assurance and Performance Improvement (QAPI) Program, revealed .the facility shall develop, implement, and maintain an ongoing .data-driven QAPI program that is focused on indicators of the outcomes of care .objectives .provide a means to measure current and potential indicators for outcomes of care .establish and implement performance improvement projects to correct identified negative or problematic indicators .governing board (body) .is .responsible for the QAPI program .governing board [body] evaluates the effectiveness of its QAPI program at least annually .
Review of the facility's undated policy titled, Governing Body, revealed .the facility will have designated persons functioning as a governing body, that is .responsible for establishing and implementing policies .the governing body is responsible and accountable for the QAPI program .the governing body will have a process in place by which the administrator .reports .communication .how the governing body responds back to the administrator .
Review of a facility's undated document titled, Governing Body Organizational Structure, revealed the governing body members were designated as the Medical Director, VPRC, VPCS, and the VPO.
Review of a facility document titled, Regulatory Compliance and QAPI Program, dated 8/15/2023, revealed .infection prevention program expectations .surveillance .infection tracking and log .COVID [COVID-19] tracking staff and residents .testing .reporting .appropriate use of source control and PPE use during care .appropriate use of precautions .droplet .contact .enhanced barrier .QAPI participation .schedule monthly infection control meeting .separate from QAPI meetings .reporting of infection control meeting minutes during QAPI meetings .Ad-Hoc [as necessary] infection control meetings during outbreaks to discuss root cause analysis and facility actions .
Review of the Administrator's Job Description signed and dated by the Administrator on 10/3/2022, revealed .plans, coordinates and manages all services and employees of [the] facility .responsible for .coordination and evaluation of all care and services provided .manages compliance with all policies and procedures .oversees and help develop education .ensure .outcomes .policies and procedures of Nursing services meet .regulations .services are provided in accordance with [the] resident's plan of care .drives .ongoing activities of the Quality Improvement Committee (QAPI) .
Review of the Medical Director Services Agreement and Description of Services dated 6/1/2021, revealed .Review resident cases .for quality of care .quality of life concerns .take steps to resolve situations .Participate in Facility staff meetings concerning infection control, pharmacy services .Review, approve, implement, and assist in the development of clinical, nursing .resident care policies .procedures .Review, consider .act upon consultant recommendations pertaining to .resident care .Attend Quality Assessment and Assurance meetings .Advise .direct quality improvement plans .Assist in identification .implementation of .staff educational needs .provide information to staff . Further review revealed the Medical Director was not listed as a governing body designee in this contract.
Review of a facility document (undated and untitled) revealed the QAPI committee meets one time monthly, and the Administrator was the committee contact.
Investigation revealed the facility experienced two COVID-19 outbreaks. Documentation revealed during the first outbreak on 8/9/2024 through 10/11/2024, 28 residents and 15 employees tested positive for COVID-19. During the second outbreak on 10/19/2024 through present, revealed 10 residents and 5 employees tested positive for COVID-19. The facility allowed 17 of the 20 total COVID-19 positive employees to return to work before the required isolation time frame recommended by CDC guidance, which increased the likelihood that contagious employees could spread the COVID-19 infection to all residents in the facility. The facility failed to accurately identify COVID-19 positive residents and residents who required EBP with appropriate signage and tracking of potentially infectious diseases. Further investigation revealed employees were non-compliant with PPE usage in the provisions of care for residents in EBP rooms.
Refer to F-880
The facility failed to ensure the nursing staff were knowledgeable and fully understood what EBP were, how to identify residents in EBP, and what PPE was required for residents in EBP and active COVID-19 rooms. The facility failed to ensure nursing staff implemented appropriate PPE usage for residents in EBP and droplet (for COVID-19) isolation to prevent and control the spread of COVID-19 and other infectious organisms.
Refer to F-726
The facility failed to ensure that services provided met professional standards of quality and acceptable standards of clinical practice when staff failed to follow physician orders for obtaining vital signs on residents who tested positive for COVID-19 and failed to follow professional standards of practice for medication administration.
Refer to F-684
The facility Administration failed to address in QAPI the facility's widespread problem of ensuring COVID-19 positive employees were excluded from work, failed to complete COVID-19 testing and tracking for employees, failed to accurately identify which residents were positive for COVID-19, and failed to ensure the residents and employees with an active COVID-19 infection had completed the required isolation time frame recommended by the Centers of Disease Control (CDC) to control the exposure and spread of COVID-19. The facility Administration failed to recognize the need to address staff competency related to infection control practices to address non-compliance with PPE usage for care provisions to residents that were potentially contagious. The facility Administration failed to recognize and address deficient practice related to following physician's orders and failed to ensure professional standards of care were followed related to medication administration.
Refer to F-835
Review of the QAPI meeting minutes dated 11/2023 through 10/2024, revealed the QAPI committee and the Governing Body failed to identify infection control deficiencies related to unsafe infection control practices with accurate identification of COVID-19 positive residents to prevent the spread of COVID-19 which resulted in multiple COVID-19 outbreaks, non-compliance with isolation procedures, and the practice of allowing COVID-19 positive employees to provide care to Non-COVID-19 positive residents. The QAPI committee and the Governing Body failed to recognize the need to address staff competency related to infection control practices to address non-compliance with PPE usage for care provisions to residents that were potentially contagious. The QAPI committee and the Governing Body failed to implement corrective action to address the deficient practice with physician's orders compliance related to vital sign monitoring and ensuring professional standards of care were followed for an unsafe practice of medication administration for a resident at risk for aspiration.
Refer to F-837 and F-867
During an interview on 11/6/2024 at 3:34 PM, the Administrator stated QAPI meetings are held monthly, and the required members are the Administrator, Medical Director, DON, and the Infection Preventionist. The Administrator stated the Governing Body members can attend the monthly QAPI meetings if desired, but it is not required for the Governing Body members to attend. The Administrator stated the primary mode of communication with the Governing Body designees was by email and there was no formal report or information required to send to the Governing Body members. The Administrator stated she did not know if the Governing Body had separate meeting to discuss facility problems or concerns. The Administrator could not identify the Governing Body members upon request.
During an interview on 11/7/2024 at 10:03 AM, the Administrator stated at least one member of the Governing Body attended the monthly QAPI meetings and confirmed the Governing Body did not have a separate meeting to address facility problems or concerns. The Administrator stated she sent the Governing Body designees an invitation to attend the monthly QAPI meetings via (by way of) video teleconference.
During an observation and interview on 11/7/2024 at 10:09 AM, revealed the Administrator entered the conference room and asked the surveyor to review the QAPI meeting signature logs provided to the surveyor on 11/5/2024. The Administrator skimmed through the monthly QAPI signature logs and proceeded to sign the signature of the VPRC on multiple signature logs (witnessed by the survey team). The Administrator stated the facility needed to review the QAPI meeting minutes and signature logs previously provided to the surveyor and stated the signature logs for the monthly QAPI meetings had been given in error. The Administrator took the monthly QAPI signature logs out of the conference room to review with the corporate team.
During an observation and interview on 11/7/2024 at 10:45 AM, the Administrator returned to the conference room with the monthly QAPI meeting signature logs (11/2023 through 10/2024). Observation revealed the QAPI meeting signature logs had new signatures added from a member of the Governing Body on each of the QAPI meeting signature logs. The Administrator stated she had the Governing Body members to sign the QAPI meeting signature logs to verify their attendance to the meetings. The Administrator stated the Governing Body members failed to sign the signature logs of the QAPI meetings and stated the Governing Body members attended these meetings via video conference. (The Administrator failed to provide documentation of the video conference invitations with attendance to verify the presence of the Governing Body members in comparison to the addition of the new signatures.)
Review of the QAPI meeting signature logs on 11/7/2024 at 10:50 AM, revealed the following discrepancies:
11/30/2023: addition of the name and signature of VPRC (name misspelled)
12/29/2023: addition of the name and signature of VPCS
1/25/2024: addition of the name and signature of VPO and VPRC (both names were misspelled)
2/22/2024: addition of the name and signature of VP of Administrator Leadership Education and QAPI (VPALEQ)
3/21/2024: addition of the name and signature of VPALEQ
4/18/2024: addition of the name and signature of VPCS
5/24/2024: addition of the name and signature of VPCS
6/27/2024: addition of the name and signature of VPCS
7/18/2024: addition of the name and signature of VPRC
8/30/2024: addition of the name and signature of VPCS
9/26/2024: addition of the name and signature of VPRC (name misspelled)
10/24/2024: addition of the name and signature of VPRC (name misspelled)
During an interview in the recreation/ family visitation room on 11/8/2024 at 12:00 PM, with the VPRC and VPCS (Governing Body members), the VPRC stated she attended the monthly QAPI meetings via video teleconference or in-person. The VPRC and the VPCS stated they received the invitation for the QAPI meeting schedule via email (from the Administrator) and will attend. The VPRC stated the Governing Body designees did not conduct a separate meeting from the QAPI meetings to discuss facility problems or areas of concern. The VPRC stated the Governing Body communicated with each other via email or phone calls to discuss any action items recognized. The VPRC could not recall any specific conversation to the Governing Body designees regarding COVID-19 infection control issues, COVID-19 outbreaks, or CDC guideline updates. The VPCS stated the Governing Body had input and made suggestions during the QAPI meetings. The VPCS could not recall any specific suggestions or action plans during the QAPI meetings to address COVID-19 infection control issues, COVID-19 outbreaks, and CDC guideline updates.
CRITICAL
(L)
Immediate Jeopardy (IJ) - the most serious Medicare violation
QAPI Program
(Tag F0867)
Someone could have died · This affected most or all residents
⚠️ Facility-wide issue
Based on facility policy review, job description review, facility assessment review, Quality Assurance and Performance Improvement (QAPI) Plan review, QAPI Meeting Minutes review, facility documentati...
Read full inspector narrative →
Based on facility policy review, job description review, facility assessment review, Quality Assurance and Performance Improvement (QAPI) Plan review, QAPI Meeting Minutes review, facility documentation review, medical record review, observations, and interviews, the facility's QAPI program failed to ensure an effective, data-driven QAPI program that identified quality deficiencies, implement performance improvement activities to address quality concerns, and perform a root cause analysis related to infection control practices. The facility ' s QAPI committee failed to develop and implement effective processes or initiate action plans for performance improvement when the committee failed to recognize poor infection control practices of the facility and to ensure an effective infection control program to mitigate the spread of disease. The facility ' s QAPI program failed to recognize and provide to the staff the updated Centers for Disease Control Guidelines for the isolation and quarantine time of COVID-19 residents and employees, which allowed COVID-19 positive employees to work and provide care for vulnerable and COVID-19 negative residents of the facility, exposing the residents to the COVID-19 infection. The facility census was 99.
The facility's failure to ensure an effective QAPI program, implement proper infection control practices, ensure physician ' s orders were followed related to vital sign monitoring for COVID-19 positive residents, and ensure medication administrations adhered to professional standard of practice resulted in an Immediate Jeopardy (IJ), (a situation in which the provider's noncompliance with one or more requirements of participation has caused, or is likely to cause, serious injury, harm, impairment, or death to a resident) which had likelihood to impact all 99 residents of the facility.
The Administrator, Director of Nursing (DON), [NAME] President of Operations (VPO), [NAME] President of Life Safety and Environmental Compliance (VPLSEC), and [NAME] President of Clinical Services (VPCS) (attended in person) and the [NAME] President of Regulatory Compliance (VPRC) and Chief Operating Officer (COO) with the Chief Regulatory Compliance Officer (CRCO) (attended by telephone) were notified of the IJs for F-880, F-835, F-837, F-867, F-684, and F-726 on 11/13/2024 at 9:42 PM in the Common Area/Recreation Area.
The facility was cited Immediate Jeopardy at F-867 at a scope and severity of L.
The facility was cited Immediate Jeopardy at F-684 at a scope and severity of K which is substandard quality of care.
The facility was cited Immediate Jeopardy at F-726, F-835, F-837, F-880 at a scope and severity of L.
An Extended survey was conducted onsite from 11/14/2024 through 11/15/2024.
The IJ began on 8/9/2024 and is ongoing.
The facility is required to submit a Plan of Correction (POC).
The findings include:
Review of the facility's undated policy titled, Quality Assurance and Performance Improvement (QAPI) Program, revealed .the facility shall develop, implement, and maintain an ongoing .data-driven QAPI program that is focused on indicators of the outcomes of care .objectives .provide a means to measure current and potential indicators for outcomes of care .establish and implement performance improvement projects to correct identified negative or problematic indicators .governing board (body) .is .responsible for the QAPI program .governing board [body] evaluates the effectiveness of its QAPI program at least annually .
Review of a facility document titled, Regulatory Compliance and QAPI Program, dated 8/15/2023, revealed .infection prevention program expectations .surveillance .infection tracking and log .COVID [COVID-19] tracking staff and residents .testing .reporting .appropriate use of source control and PPE use during care .appropriate use of precautions .droplet .contact .enhanced barrier .QAPI participation .schedule monthly infection control meeting .separate from QAPI meetings .reporting of infection control meeting minutes during QAPI meetings .Ad-Hoc [as necessary] infection control meetings during outbreaks to discuss root cause analysis and facility actions .
Review of a facility document (undated and untitled) revealed the QAPI committee meets one time monthly, and the Administrator is the committee contact.
Review of the Administrator's Job Description signed and dated by the Administrator on 10/3/2022, revealed .plans, coordinates and manages all services and employees of [the] facility .responsible for .coordination and evaluation of all care and services provided .manages compliance with all policies and procedures .oversees and help develop education .ensure .outcomes .policies and procedures of Nursing services meet .regulations .services are provided in accordance with [the] resident ' s plan of care .drives .ongoing activities of the Quality Improvement Committee (QAPI) .
Review of the DON ' s Job Description signed and dated by the DON on 7/10/2024, revealed .manages and directs the day-to-day functions of the Nursing Department in accordance with policies .that comply with federal, state, and local regulations .ensures .staff are qualified and trained .ensures that each patient ' s needs are assessed and .treatment plan is developed for nursing care .ensures that required documentation is complete .
Review of the Medical Director Services Agreement and Description of Services dated 6/1/2021, revealed .Review resident cases .for quality of care .quality of life concerns .take steps to resolve situations .Participate in Facility staff meetings concerning infection control, pharmacy services .Review, approve, implement, and assist in the development of clinical, nursing .resident care policies .procedures .Review, consider .act upon consultant recommendations pertaining to .resident care .Attend Quality Assessment and Assurance meetings .Advise .direct quality improvement plans .Assist in identification .implementation of .staff educational needs .provide information to staff .
Investigation revealed the facility had two COVID-19 outbreaks. Documentation revealed during the first outbreak on 8/9/2024 through 10/11/2024, revealed 28 residents and 15 employees tested positive for COVID-19. During the second outbreak on 10/19/202 through present, revealed 10 residents and 5 employees tested positive for COVID-19. The facility allowed 17 of the 20 total COVID-19 positive employees to return to work before the required isolation time frame recommended by CDC guidance, which increased the likelihood that contagious employees could spread the COVID-19 infection to all residents in the facility. The facility failed to accurately identify COVID-19 positive residents and residents who required EBP with appropriate signage and tracking of potentially infectious diseases. Further investigation revealed employees were non-compliant with PPE usage in the provisions of care for residents in Enhanced Barrier Precautions (EBP) rooms for 6 of 26 residents.
Refer to F-880
Investigation revealed the facility failed to ensure the nursing staff were competent and fully understood isolation guidelines for EBP and COVID-19 and implemented appropriate use of PPE (Personal Protective Equipment) for residents in isolation to prevent and control the spread of COVID-19 and other infectious organisms.
Refer to F-726
The facility failed to ensure that treatment and care provided met professional standards of quality and acceptable clinical practice for following physician ' s orders and administering medications.
Refer to F-684
The facility Administration failed to administer the facility in a manner that enabled it to use its resources effectively and efficiently to attain or maintain the highest practicable physical, mental, and psychosocial well-being of each resident. The facility Administration failed to ensure an effective QAPI Committee that identified noncompliance timely and used quality data to track and trend noncompliance. The facility Administration failed to ensure COVID-19 positive employees were excluded from work, failed to complete COVID-19 testing and tracking for residents and employees, failed to identify COVID-19 positive residents accurately, and failed to ensure the residents and employees with an active COVID-19 infection had completed the required isolation time frame recommended by the Centers of Disease Control (CDC) to control the exposure and spread of COVID-19. The facility Administration failed to ensure competent nursing staff who correctly identified all types of isolation precautions and implemented the correct PPE usage for those precautions. The facility Administration failed to identify deficient practice related to failure of staff to follow physician's orders and provide care according to professional standards of practice.
Refer to F-835
The Governing Body failed to provide oversight to Administration to address in QAPI the facility ' s failure to identify all areas of non-compliance related to infection control, isolation and quarantine guidelines, PPE usage, competent staff, and acceptable standards of practice. The Governing Body failed to ensure Administration implement updated policies and procedures which aligned with the CDC guidelines and requirements for infection control.
Refer to F-837
Review of the QAPI meeting minutes dated 11/2023-10/2024, revealed the QAPI committee and the Governing Body failed to identify infection control deficiencies related to unsafe infection control practices with accurate identification of COVID-19 positive residents to prevent the spread of COVID-19 which resulted in multiple COVID-19 outbreaks, non-compliance with isolation procedures, and the practice of allowing COVID-19 positive employees to provide care to Non-COVID-19 positive residents. The QAPI committee and the Governing Body failed to recognize the need to address staff competency related to infection control practices to address non-compliance with PPE usage for care provisions to residents who were potentially contagious. The QAPI committee and the Governing Body failed to implement corrective action to address the deficient practice of noncompliance with physician ' s orders related to vital sign monitoring and ensuring professional standards of care were followed for an unsafe practice of medication administration for a resident at risk for aspiration.
During an interview on 11/6/2024 at 3:15 PM, the Medical Director stated he had voiced previous concerns to the facility administration in QAPI regarding staff PPE usage and infection control practices. The Medical Director stated the facility did not implement his professional recommendations in QAPI meetings for infection control practices and guidance during the outbreaks.
During an interview on 11/13/2024 at 7:55 PM, the Administrator stated the facility had .some areas of improvement to address in QAPI to improve infection prevention and control practices . Further interview revealed the Administrator wanted to address in QAPI competent staffing and professional standards of care are met.
Refer to F-684, F-726, F835, F837, F867, and F880
CRITICAL
(L)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Infection Control
(Tag F0880)
Someone could have died · This affected most or all residents
⚠️ Facility-wide issue
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, Centers for Disease Control and Prevention (CDC) recommendations and guidance review, medical r...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, Centers for Disease Control and Prevention (CDC) recommendations and guidance review, medical record review, observations, and interviews, the facility failed to ensure current CDC guidelines dated 6/24/2024 and 10/28/2024 were followed to prevent and control the spread of COVID-19 to residents and staff, failed to identify and track residents with an active COVID-19 infection, failed to wear appropriate Personal Protective Equipment (PPE) in COVID-19 isolation rooms, and failed to perform facility wide employee testing and recommended quarantine time during the COVID-19 outbreaks. The facility failed to ensure COVID-19 positive residents were quarantined according to CDC guidance when Residents #608, #619, and #509 were admitted with COVID-19. The facility's first COVID-19 outbreak started 8/9/2024 through 10/11/2024, which resulted in 28 residents (Residents #96, #31, #45, #33, #11, #64, #609, #93, #15, #510, #611, #80, #612, #506, #615, #613, #614, #54, #68, #27, #53, #12, #95, #74, #30, #37, #3, and #89) and 15 employees testing positive. The facility's second COVID-19 outbreak started 10/19/2024 and was on going which resulted in 10 residents (Residents #99, #617, #103, #72, #34, #618, #507, #508, #102, and #94) and 5 employees testing positive. The facility failed to identify and track residents and staff with COVID-19 for 2 of 2 outbreaks. The facility failed to ensure staff wore the appropriate PPE and identified residents in Enhanced Barrier Precautions (EBP) for 6 of 26 residents (Resident #13, #25, #56, #83, #24, #52). The facility's noncompliance resulted in an Immediate Jeopardy (IJ) (a situation in which the provider's noncompliance with one or more requirements of participation has caused, or is likely to cause, serious injury, harm, impairment, or death to a resident). The facility failed to follow infection control procedures during medication administration for 2 residents (Resident #52 and #99) of 6 residents observed for medication administration. The facility census was 99.
The Administrator, Director of Nursing (DON), [NAME] President of Operations (VPO), [NAME] President of Life Safety and Environmental Compliance (VPLSEC), [NAME] President of Clinical Services (VPCS) (attended in person) and the [NAME] President of Regulatory Compliance (VPRC) and Chief Operating Officer (COO) with the Chief Regulatory Compliance Officer (CRCO) (attended by telephone) were notified of the IJs for F-880, F-835, F-837, F-867, F-684, and F-726 on 11/13/2024 at 9:42 PM in the Common Area/Recreation Area.
The facility was cited Immediate Jeopardy at F-880 at a scope and severity of L.
The facility was cited Immediate Jeopardy at F-684 at a scope and severity of K, which is substandard quality of care.
The facility was cited Immediate Jeopardy at F-726, F-835, F-837, F-867 at a scope and severity of L.
An Extended survey was conducted onsite from 11/14/2024 through 11/15/2024.
The IJ began on 8/9/2024 and is ongoing.
The facility is required to submit a Plan of Correction (POC).
The findings include:
1) Review of the facility's undated policy titled, COVID-19 GENERAL TESTING POLICY, which referenced the 5/25/2023 CDC guidelines revealed .Staff with symptoms or signs of COVID-19 .will be tested as soon as possible and will be restricted from the facility pending the results of COVID-19 testing .Residents who have signs and symptoms of COVID-19 .will be tested .be placed on transmission-based precautions (TBP) .DURING COVID-19 OUTBREAK .Facilities will investigate an outbreak using contact tracing or a broad-based approach .testing every 3-[to] 7 days until no more positive cases identified for 14 days .if additional cases are identified after testing .the facility will expand testing to facility-wide if testing .implementation of infection control measures have failed .PCR [Polymerase chain reaction] [accurate and reliable test for diagnosing COVID-19] will be used .testing will occur on day 1, day 3, and day 5 .
Review of the facility's undated policy titled, COVID-19 ADMISSIONS AND READMISSIONS, which referenced the 5/25/2023 CDC guidelines revealed .Due to risk of unrecognized COVID-19 infections among residents, facilities must conduct testing at the time of admission to the facility based on COVID-19 Hospital Admissions Levels .Empiric use of Transmission-Based Precautions is not necessary .unless .Resident is placed on a unit experiencing ongoing SARS-CoV-2 [COVID-19] transmission .
Review of the facility's undated policy, COVID-19 Management of Residents, undated, which referenced the 5/25/2023 CDC guidelines revealed .The facility will not have a dedicated COVID-19 unit unless the number of positive residents warrant .the facility will place a COVID-19 positive resident in a single room with appropriate isolation signage and staff wearing N95 respirator, eye protection, gown, and gloves upon entry to the room .dedicated staff, to care for residents with COVID-19 .the door will be kept closed if safe to do so .resident will be monitored every four hours for .symptoms, vital signs, oxygen saturation .and respiratory exam .staff will wear full PPE (N95 respirator, gown, gloves, eye protection) when providing care .
Review of the facility's undated policy titled, COVID-19 Positive Staff Member Work Restriction, which referenced the 5/25/2023 CDC guidelines revealed .HCP [Health Care Providers] should self-monitor for symptoms and seek re-evaluation .if symptoms recur .these HCP will be restricted form work .until they again meet the healthcare criteria .Staff who were ASYMPTOMSTATIC .will return to work .at least .7 .days have passed since the date of their first positive viral test if a negative viral test .is obtained .48 hours prior to returning to work or 10 days if testing is not performed .if using an antigen [rapid diagnostic test] test, staff should have a negative test obtained on day 5 and 48 hours later .Staff who are SYMPTOMATCIC can return to work .at least .7 .days have passed since symptoms first appeared, if a negative viral test .is obtained within 48 hours prior to returning to work, or 10 days if testing is not performed .at least 24 hours have passed since last fever without the use of fever-reducing medications .When Contingency staffing strategies are used, staff with SARS-CoV-2 infection will be well enough and willing to return to work .at least .5 .days have passed since symptoms first appeared (day 0) .at least 24 hours have passed since last fever without the use of fever-reducing medications .Symptoms .have improved .facility may choose to confirm resolution of infection with a PCR or a series of .2 .negative antigen tests taken 48 hours apart .Antigen tests typically have a more rapid turnaround time .are often less sensitive than PCR .Antigen testing is preferred .
Review of the facility's undated policy titled, COVID-19 Transmission Based Precautions, which referenced the 5/25/2023 CDC guidelines revealed .Transmission-Based Precautions .If residents are placed in Transmission-Based Precautions .will be removed .after day 7 .and all viral testing .is negative .If viral testing is not performed, residents will be removed from Transmission-Based Precautions after day 10 .Duration of Transmission-Based Precautions for residents with COVID-19 .a minimum of 10 days since symptoms first appeared .fever free for 24 hours .
Review of the facility's undated policy titled, COVID-19 GUIDELINES UNIVERSAL SCREENING, which referenced the 5/25/2023 CDC guidelines revealed .if the facility is in outbreak, all residents .will be evaluated at least daily for signs and symptoms of COVID-19 .if residents have a fever or symptoms .monitoring will be increased to every four hours .vital signs (temperature, pulse, respirations) .Oxygen saturation .Blood pressure .
Review of the CDC's guidance titled, Infection Control Guidance: SARS-CoV-2, dated 6/24/2024, revealed, .The recommendations in this guidance continue to apply after the expiration of the federal COVID-19 Public Health Emergency [3/11/2023] .Establish a Process to Identify and Manage Individuals with Suspected or Confirmed SARS-CoV-2 Infection .Ensure everyone is aware of recommended IPC [infection prevention and control] practices in the facility .Source control is recommended for individuals in healthcare settings who: Have suspected or confirmed SARS-CoV-2 infection or other respiratory infection (e.g., those with runny nose, cough, sneeze); or Had close contact (patients and visitors) or a higher-risk exposure HCP with someone with SARS-CoV-2 infection, for 10 days after their exposure .Anyone with even mild symptoms of COVID-19, regardless of vaccination status, should receive a viral test for SARS-CoV-2 as soon as possible .To provide the greatest assurance that someone does not have SARS-CoV-2 infection, if using an antigen test .facilities should use 3 tests, spaced 48 hours apart .testing should be repeated every 3-7 days until no new cases are identified for at least 14 days .HCP who enter the room of a patient with suspected or confirmed SARS-CoV-2 infection should adhere to Standard Precautions .use a NIOSH [National Institute for Occupational Safety and Health] Approved particulate respirator with N95 filter .gown, gloves .eye protection .A single new case of SARS-CoV-2 infection in any HCP or resident should be evaluated to determine if others in the facility could have been exposed .Perform testing for all residents and HCP identified as close contacts or on the affected unit(s) if using a broad-based approach, regardless of vaccination status. Testing is recommended immediately (but not earlier than 24 hours after the exposure) and, if negative, again 48 hours after the first negative test and, if negative, again 48 hours after the second negative test. This will typically be at day 1 (where day of exposure is day 0), day 3, and day 5 .
Review of the CDC guidance titled, Viral Respiratory Pathogens Toolkit for Nursing Homes, dated 10/28/2024, revealed .Educate .Ensure everyone .including HCP, are aware of recommended IPC [infection prevention and control] practices in the facility .When an acute respiratory infection is identified in a resident or HCP .take rapid action to prevent the spread to others in the facility .Apply appropriate Transmission-Based Precautions for symptomatic residents .HCP who enter the room of a resident with signs or symptoms of an unknown respiratory viral infection that is consistent with SARS-CoV-2 [COVID-19] infection should adhere to Standard Precautions .use a NIOSH-approved particulate respirator with N95 filters or higher, gown, gloves, and eye protection (i.e. [example], goggles or a face shield that covers the front and sides of the face) .Develop sick leave policies for HCP .with public health guidance to discourage presenteeism [lost productivity that occurs when employees are not fully functioning in the workplace because of an illness, injury, or other condition] .allow HCP with respiratory infection to stay home for the recommended 10 day duration of work restriction .Test anyone with respiratory illness signs or symptoms .Investigate for potential respiratory virus spread among residents and HCP .Perform active surveillance to identify any additional ill residents or HCP using symptom screening .evaluating potential exposures .testing of exposed individuals is recommended, even if they are asymptomatic .Make initial attempts to control limited spread .If SARS-CoV-2 transmission is occurring .Consider implementing broad-based testing as opposed to only testing close contacts to identify asymptomatic infection .
The following 29 residents resided on the 100, 200, and 400 hallways. Resident #608 was admitted to the facility COVID-19 positive on 8/9/2024 and was identified as the start of the outbreak. An additional 28 residents tested positive for COVID-19 during the COVID-19 outbreak in the facility from 8/9/2024-10/11/2024 (Residents #96, #31, #45, #33, #11, #64, #609, #93, #15, #51, #611, #80, #612, #506, #615, #613, #614, #54, #68, #27, #53, #12, #95, #74, #30, #37, #3, and #89).
The following COVID-19 positive employees were not excluded from work for the required isolation time frame recommended by the CDC guidance to prevent the exposure and spread of COVID-19 (Licensed Practical Nurse (LPN) Y, Physical Therapist (PT) CC, LPN BB, Housekeeper GG, Laundry HH, Physical Therapist Assistant (PTA) II, LPN JJ, Certified Nursing Assistant (CNA) KK, CNA Z, CNA AA, LPN C, and CNA LL) .
1a) Review of the medical record revealed Resident #608 was admitted to the facility on [DATE] with diagnoses including Myopathy, Hypertension, GERD (Gastroesophageal Reflux Disease), Osteoarthritis, Dementia, and COVID-19 (added on 8/9/2024).
Review of the medical record revealed Resident #608 tested positive for COVID-19 on 8/7/2024 at the hospital and was admitted to the facility's 100 Hallway with an active COVID-19 infection on 8/9/2024. Further review revealed Resident #608 was identified as the start of the first COVID-19 outbreak.
Review of a Physician's Order for Resident #608 dated 8/9/2024, revealed .isolation droplet precautions .[at] .all times due to positive covid 19 [COVID-19] test .mask .goggle [goggles] gloves, gown, face shield . The isolation order continued until 8/12/2024. (discontinued 5 days before the CDC recommended guidance)
Review of the comprehensive care plan for Resident #608 dated 8/13/2024 (4 days after admission), revealed .Resident is positive for COVID-19 .
Review of a 5-day Minimum Data Set (MDS) assessment dated [DATE], revealed Resident #608 scored a 3 on the Brief Interview for Mental Status (BIMS) assessment which indicated the resident had severe cognitive impairment.
1b) Review of the medical record revealed Resident #96 was admitted to the facility on [DATE] and re-admitted to the facility on [DATE] on the 100 Hallway with diagnoses including Lung Disease, Heart Failure, COVID-19 (added on 8/14/2024), and Obstructive Sleep Apnea.
Review of the laboratory result for Resident #96 dated 8/14/2024, revealed a COVID-19 test was flagged as an abnormal result which indicated the COVID-19 test was positive. Resident #96 tested positive for COVID-19 within 24 hours of admission.
Review of the comprehensive care plan for Resident #96 initiated 8/14/2024, revealed no revisions made to care plan goals and interventions related to the new COVID-19 infection.
Review of a Physician's Order for Resident #96 dated 8/14/2024, revealed .Isolation Droplet precautions @ [at] all times due to positive COVID-19 test. Mask, googles [goggles], gloves, gown, face shield . The isolation order continued until 8/24/2024.
Review of an admission MDS assessment dated [DATE], revealed Resident #96 scored a 15 on the BIMS assessment which indicated the resident was cognitively intact.
1c) Review of the Medical record revealed Resident #31 was admitted to the facility on the 100 Hallway on 5/10/2024 with diagnoses including Dementia, Anemia, Diabetes, and COVID-19 (added on 8/21/2024).
Review of a quarterly MDS assessment dated [DATE], revealed Resident #31 scored a 00 on the BIMS assessment which indicated the resident had severe cognitive impairment. Further review revealed staff were unable to complete the assessment.
Review of the laboratory result for Resident #31 dated 8/21/2024, revealed a positive COVID-19 test.
Review of a Physician's Order for Resident #31 dated 8/21/2024, revealed .Isolation Droplet precautions @ all times due to positive covid 19 test. Mask, googles, gloves, gown, face shield . The isolation continued until 8/31/2024.
Review of the comprehensive care plan for Resident #31 dated 8/26/2024, revealed .Resident is positive for COVID-19 .
1d) Review of the medical record revealed Resident #45 was admitted to the facility on the 100 Hallway on 6/20/2024 with diagnoses including Cerebral Infarction (Stroke), Anxiety Disorder, Hypertension, Chronic Kidney Disease, and COVID-19 (added on 8/21/2024).
Review of a Physician's Order for Resident #45 dated 8/21/2024, revealed .Isolation Droplet precautions @ all times due to positive covid 19 test. Mask, googles, gloves, gown, face shield . The isolation order continued until 8/31/2024.
Review of the comprehensive care plan for Resident #45 dated 8/26/2024, revealed .Droplet precautions .Resident is positive for COVID-19 infection .Droplet isolation sign in place .
Review of a significant change in status MDS assessment dated [DATE], revealed Resident #45 scored a 12 on the BIMS assessment which indicated the resident had moderate cognitive impairment.
1e) Review of the medical record revealed Resident #33 was admitted to the facility on the 100 Hallway on 8/13/2024 with diagnoses including COVID-19 (added on 8/22/2024), Congestive Heart Failure, Chronic Obstructive Pulmonary Disease (COPD), and Adult Failure to Thrive.
Review of a 5-day admission MDS assessment dated [DATE], revealed Resident #33 scored a 7 on the BIMS assessment which indicated the resident had severe cognitive impairment.
Review of the laboratory result for Resident #33 dated 8/23/2024, revealed the COVID-19 test result was positive.
Review of a Physician's Order for Resident #33 dated 8/23/2024, revealed .Isolation Droplet precautions @ all times due to positive covid 19 test. Mask, googles, gloves, gown, face shield . The isolation order continued until 8/31/2024.
Review of the comprehensive care plan for Resident #33 dated 8/23/2024, revealed the resident tested positive for COVID-19 and was placed under droplet precautions.
During an interview on 11/12/2024 at 3:48 PM, the [NAME] President (VP) of Clinical Services stated according to the Nurse Practitioner (NP) note dated 8/26/2024 for Resident #33 the resident was evaluated for a positive COVID-19 diagnosis. Continued interview confirmed the COVID-19 test result was positive.
1f) Review of the medical record revealed Resident #11 was admitted to the facility on the 100 Hallway on 5/28/2024 with diagnoses including Hypertension, Diabetes, Depression, and COVID-19 (added on 8/22/2024).
Review of the quarterly MDS assessment dated [DATE], revealed Resident #11 scored a 15 on the BIMS assessment which indicated the resident was cognitively intact.
Review of the laboratory result for Resident #11 dated 8/23/2024, revealed a positive COVID-19 test result.
Review of a Physician's Order for Resident #11 dated 8/23/2024, revealed .Isolation Droplet precautions @ all times due to positive COVID-19 test. Mask, googles, gloves, gown, face shield . The isolation order continued until 9/1/2024.
Review of the comprehensive care plan for Resident #11 dated 8/23/2024, revealed the resident had tested positive for COVID-19 and required droplet precautions.
1g) Review of the medical revealed Resident #64 was admitted to the facility on the 100 Hallway on 7/16/2024 with diagnoses including Diabetes, Primary Pulmonary Hypertension, and History of Lung Blood Clots. Further review revealed the diagnosis of COVID-19 was not added.
Review of an admission MDS assessment dated [DATE], revealed Resident #64 scored a 7 on the BIMS assessment which indicated the resident had severe cognitive impairment.
Review of a Physician's Order for Resident #64 dated 8/23/2024 (2 days prior to the COVID-19 test), revealed .Isolation Droplet precautions @ all times due to positive covid 19 test. Mask, googles, gloves, gown, face shield . The isolation order continued until 9/2/2024.
Review of the laboratory result for Resident #64 dated 8/25/2024, revealed a positive COVID-19 test.
Review of the comprehensive care plan for Resident #64 dated 8/26/2024, revealed .Droplet precautions .COVID-19 .
1h) Review of the medical record revealed Resident #609 was admitted to the facility on [DATE] and readmitted to the facility on the 100 Hallway on 9/25/2024 with diagnoses including Thyroid Cancer, Lung Cancer, Pneumonia, History of Lung Blood Clots, and COVID-19 (added on 9/4/2024).
Review of the laboratory result for Resident #609 dated 8/23/2024, revealed a positive COVID-19 test.
Review of a Physician's Order for Resident #609 dated 8/23/2024, revealed .Resident has an active infection on droplet precautions .COVID-19 . The isolation order continued until 9/2/2024. (discontinued 1 day before the CDC recommended guidance)
Review of the comprehensive care plan for Resident #609 dated 8/26/2024, revealed .Resident is positive for COVID-19 .
Review of an admission MDS assessment dated [DATE], revealed Resident #609 scored a 7 on the BIMS assessment which indicated the resident had severe cognitive impairment.
1i) Review of the medical record revealed Resident #93 was admitted to the facility on the 100 Hallway on 7/26/2024 with diagnoses including Pneumonia, Hypothyroidism, Difficulty Walking, and COVID-19 (added on 8/26/2024).
Review of an admission MDS assessment dated [DATE], revealed Resident #93 scored an 8 on the BIMS assessment which indicated the resident had moderate cognitive impairment.
Review of the medical record for Resident #93 revealed no laboratory test for COVID-19 was available for review.
Review of a Physician's Order for Resident #93 dated 8/23/2024, revealed .Isolation Droplet precautions @ all times due to positive COVID-19 test .Mask, googles, gloves, gown, face shield . The isolation order continued until 9/2/2024.
Review of the comprehensive care plan for Resident #93 dated 8/26/2024, revealed .Droplet precautions .covid [COVID-19] .
1j) Review of the medical record revealed Resident #15 was admitted to the facility on the 100 Hallway on 7/30/2024 and was readmitted to the facility on [DATE] with diagnoses including Dementia, Acute Kidney Failure, Anxiety, and COVID-19 (added on 8/26/2024).
Review of a quarterly MDS assessment dated [DATE], revealed Resident #15 scored a 9 on the BIMS assessment which indicated the resident had moderate cognitive impairment.
Review of the laboratory result for Resident #15 dated 8/23/2024, revealed a positive COVID-19 test result.
Review of a NP's Progress Note for Resident #15 dated 8/23/2024, revealed the resident was evaluated due to the chief complaint of nausea and positive COVID-19 test result.Plan .Isolation precautions .
Review of the comprehensive care plan for Resident #15 dated 8/26/2024, revealed .Resident is positive for COVID-19 .
Review of a Physician's Order for Resident #15 dated 8/26/2024, revealed .Isolation Droplet precautions @ all times due to positive covid 19 test. Mask, googles, gloves, gown, face shield . The resident received the order for isolation 2 days after the positive COVID-19 test result. The isolation was discontinued on 9/1/2024 (discontinued 5 days before the CDC recommended guidance).
1k) Review of the medical record revealed Resident #510 was admitted to the facility on [DATE] and readmitted to the 100 hallway on 6/27/2024 with diagnoses including Heart Failure, Atrial Fibrillation, Chronic Kidney Disease, and COVID-19 (added on 8/26/2024).
Review of a quarterly MDS assessment dated [DATE], revealed Resident #510 scored a 13 on the BIMS assessment which indicated the resident was cognitively intact.
Review of a laboratory result for Resident #510 dated 8/24/2024, revealed the resident was positive for COVID-19.
Review of a Physician's Order for Resident #510 dated 8/26/2024 (2 days after COVID-19 positive test), revealed .Isolation Droplet precautions @ all times due to positive COVID-19 test .Mask, googles, gloves, gown, face shield . The isolation orders continued until 9/2/2024.
Review of the comprehensive care plan for Resident #510 dated 8/26/2024, revealed .Droplet precautions .COVID-19 .
1l) Review of the medical record revealed Resident #611 was admitted to the facility on [DATE] and readmitted to facility on the 100 Hallway on 8/15/2024 with diagnoses including Atrial Fibrillation, Congestive Heart Failure, and COVID-19 (added on 8/26/2024).
Review of an admission MDS assessment dated [DATE], revealed Resident #611 scored a 15 on the BIMS assessment which indicated the resident was cognitively intact.
Review of the medical record for Resident #611, revealed no laboratory data for a positive COVID-19 test was available for review
Review of a Physician's Order for Resident #611 dated 8/26/2024, revealed .Isolation Droplet precautions @ all times due to positive covid 19 test. Mask, googles, gloves, gown, face shield . The isolation order continued until 9/3/2024.
Review of the comprehensive care plan for Resident #611 revised on 8/26/2024, revealed .positive for COVID-19 .
Review of a NP's Progress Note for Resident #611 dated 8/28/2024, revealed the resident was evaluated due to follow up of positive COVID-19 test result .Plan . Isolation precautions .
1m) Review of the medical record revealed Resident #80 was admitted to the facility on [DATE] and readmitted to the 100 Hallway on 9/3/2024 with diagnoses including Fracture of the Right Femur, Diabetes, Heart Failure, and COVID-19 (added 8/26/2024).
Review of an admission MDS assessment dated [DATE], revealed Resident #80 scored a 10 on the BIMS assessment which indicated the resident had moderate cognitive impairment.
Review of a NP's Progress note for Resident #80 dated 8/26/2024, revealed .Resident was seen today for a follow-up after recent positive COVID-19 swab .
Review of a Physician's Order for Resident #80 dated 8/26/2024, revealed .Isolation Droplet precautions @ all times due to positive covid 19 test. Mask, googles, gloves, gown, face shield . The isolation order continued until 9/3/2024.
Review of the comprehensive care plan for Resident #80 dated 8/26/2024, revealed .Droplet precautions .Baseline care plan .COVID-19 .
1n) Review of the medical record revealed Resident #612 was admitted to the facility on the 100 Hallway on 8/20/2024 with diagnoses including Chronic Respiratory Failure, Chronic Pulmonary Edema, Morbid Obesity, Emphysema, and COVID-19 (added 8/26/2024).
Review of an admission MDS assessment dated [DATE], revealed Resident #612 scored a 14 on the BIMS assessment which indicated the resident was cognitively intact.
Review of the laboratory result for Resident #612 dated 8/24/2024, revealed a positive COVID-19 test result.
Review of a Physician's Order for Resident #612 dated 8/26/2024 (2 days after the positive COVID- 19 test result), revealed .Isolation Droplet precautions @ all times due to positive covid 19 test. Mask, googles, gloves, gown, face shield . The isolation order continued until 9/3/2024.
Review of the comprehensive care plan for Resident #612, dated 8/26/2024, revealed .Resident is positive for COVID-19 .
1o) Review of the medical record revealed Resident #506 was admitted to the facility on the 100 Hallway on 7/10/2024 with diagnoses including Human Immunodeficiency Virus (HIV), Acute Respiratory Failure, and COVID-19 (added 8/27/2024).
Review of the quarterly MDS assessment dated [DATE], revealed Resident #506 scored a 14 on the BIMS assessment which indicated the resident was cognitively intact.
Review of the laboratory test for Resident #506 dated 8/26/2024, revealed a positive COVID-19 test result.
Review of a NP's Progress Note for Resident #506 dated 8/27/2024, revealed .Chief Complaint .Follow-up COVID-19 .Isolation precautions .
Review of a Physician's Order for Resident #506 dated 8/27/2024 (1 day after the positive COVID-19 test result), revealed .Isolation Droplet precautions @ all times due to positive covid 19 test. Mask, googles, gloves, gown, face shield . The isolation order continued until 9/5/2024.
Review of the Comprehensive Care Plan for Resident #506 dated 9/5/2024, revealed the resident had a positive COVID-19 diagnosis and required isolation.
1p) Review of the Medical Record revealed Resident #615 was admitted to the facility on [DATE] with diagnoses including Cirrhosis of the Liver, Chronic Kidney Disease, and COVID-19 (added on 8/30/2024).
Review of the medical record revealed Resident #615 tested positive for COVID-19 on 8/27/2024 at the hospital and was admitted to the facility's 100 Hallway with an active COVID-19 infection on 8/30/2024.
Review of a Physician's Order for Resident #615 dated 8/30/2024, revealed .Isolation Droplet precautions @ all times due to positive COVID-19 test .Mask, googgles, gloves, gown, face shield. The isolation order continued until 9/6/2024.
Review of an admission MDS assessment dated [DATE], revealed Resident #615 scored a 10 on the BIMS assessment which indicated the resident had moderate cognitive impairment.
Review of the comprehensive care plan for Resident #615 dated 9/4/2024, revealed .Droplet precautions .COVID-19 .Respiratory .follow facility infection control P&P [policy and procedures] for isolation .Check for proper PPE [personal protective equipment] .Droplet isolation sign in place . (baseline care plan was not developed within 48 hours of admission and the comprehensive care plan did not reflect the active COVID-19 diagnosis until 5 days after admission to capture COVID-19).
1q) Review of the medical record revealed Resident #613 was admitted to the facility on [DATE] and readmitted on the 100 Hallway on 8/14/2024 with diagnoses including Muscle Weakness, Diabetes, Heart Failure, and COVID-19 (added 8/28/2024).
Review of a NP's Progress Note dated 8/28/2024 for Resident #613 revealed .Chief Complaint .COVID-19 positive .seen today due to testing positive for COVID-19 via nasal swab in the facility .
Review of the comprehensive care plan for Resident #613 dated 8/28/2024, revealed .Resident is positive for COVID-19 .
Review of a Physician's Order for Resident #613 dated 8/30/2024 (2 days after the positive COVID-19 test result), revealed .Isolation Droplet precautions @ all times due to positive COVID-19 test. Mask, googles, gloves, gown, face shield . The isolation order continued until 9/7/2024. (discontinued 2 days before the CDC recommended guidance)
Review of a quarterly MDS assessment dated [DATE], revealed Resident #613 scored a 12 on the BIMS assessment which indicated the resident had moderate cognitive impairment.
1r) Review of the medical record revealed Resident #614 was admitted to the facility on the 100 Hallway on 8/19/2024 with diagnoses including Anxiety, Low Oxygen Blood Saturation, and COVID-19 (added 8/28/2024).
Review of a discharge MDS dated [DATE], Resident #614 scored a 9 on the BIMS assessment which indicated the resident had moderate cognitive impairment.
Review of the laboratory result for Resident #614 dated 8/28/2024, revealed a positive COVID-19 test result. (9 days after admission into the facility)
Review of the comprehensive care plan for Resident #614 dated 8/28/2024, revealed .Resident is positive [TRUNCATED]
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observations, and interview, the facility failed to protect the resident's right to dignity when...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observations, and interview, the facility failed to protect the resident's right to dignity when an indwelling catheter drainage bag was left uncovered and visible to the public for 1 resident (Resident #90) of 99 residents observed for dignity.
The findings include:
Review of the medical record revealed Resident #90 was admitted to the facility on [DATE] and readmitted on [DATE] with diagnoses including Neuromuscular Dysfunction of the Bladder, Malignant Neoplasm of the Urethra, and Acute Kidney Failure.
Review of a significant change Minimum Data Set (MDS) assessment dated [DATE], revealed Resident #90 scored an 11 on the Brief Interview for Mental Status (BIMS) assessment which indicated the resident had moderate cognitive impairment. Further review revealed the resident had an indwelling urinary catheter.
Review of an Order Summary report for Resident #90 dated 10/24/2024, revealed .[indwelling urinary catheter] dx [diagnosis] neurogenic bladder.
Review of a comprehensive care plan for Resident #90 revised 11/5/2024, revealed, .[indwelling urinary catheter] .dx: Neurogenic bladder .provide privacy bag to drainage bag at all times .
During an observation on 11/3/2024 at 11:45 AM, revealed Resident #90 had no privacy dignity cover present to the bedside urinary drainage bag and the uncovered drainage bag was visible to the outside of the resident's room, into the hallway.
During an interview on 11/3/2024 at 12:15 PM, Registered Nurse B confirmed Resident #90 did not have a privacy dignity cover present to the urinary bedside drainage bag which resulted in the direct visibility of the urinary drainage bag from the hallway.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on facility policy review, medical record review, observations, and interviews, the facility failed to ensure the residents' protected health information remained private and confidential on 2 (...
Read full inspector narrative →
Based on facility policy review, medical record review, observations, and interviews, the facility failed to ensure the residents' protected health information remained private and confidential on 2 (D-Wing and C-Wing) of 4 hallways, which had the potential to allow unauthorized individuals access to the residents' private health information.
The findings include:
Review of the facility's policy titled, Electronic Health Records Guidelines, undated, revealed .the staff shall maintain confidentiality of the residents' information .only authorized persons are permitted to review records .
Review of the facility's policy titled, HIPAA [Health Insurance Portability and Accountability Act] Guidelines, undated, revealed .the facility will implement reasonable and appropriate measures to protect and maintain the confidentiality .of the resident's identifiable information .
During an observation and interview on 11/8/2024 at 12:19 PM, on the D-Wing, revealed the residents' protected health information was present on the computer screen on the medication cart and was left unattended. Registered Nurse B revealed the computer screen was not locked and covered prior to leaving the medication cart. RN B confirmed the residents' personal health information was not protected and was available for the public to see.
During an observation on 11/4/2024 at 7:59 AM, on the C-Wing, revealed Licensed Practical Nurse (LPN) A left the resident roster for all the residents present on the C-Wing, visible on the top of the medication cart. Further observation revealed the resident roster had sensitive resident health information present and was not covered to maintain confidential resident information.
During an interview on 11/4/2024 at 8:01 AM, LPN A confirmed the residents' sensitive and protected health information was not properly maintained to ensure resident information was not visible to the public. LPN A stated she forgot to cover it prior to leaving the medication cart.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, medical record review, observations and interviews, the facility failed to develop a person-cen...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, medical record review, observations and interviews, the facility failed to develop a person-centered comprehensive care plan related to a stomach drain for 1 resident (Resident #36) and for a COVID-19 infection for 1 resident (Resident #506); the facility failed to implement care plan interventions related to sexual behaviors for 1 resident (Resident #606), and related to meal assistance for 1 resident (Resident #93) of 40 residents reviewed for care plans.
The findings include:
Review of the facility's policy titled, Comprehensive Care Plans, undated, revealed it is the policy of this facility to develop and implement a comprehensive person-centered care plan consistent with .timeframes to meet a resident's .needs .services provided or arranged by the facility .resident specific interventions .qualified staff responsible for carrying out interventions specified in the care plan will be notified of their roles .initially and when changes are made .
Review of the facility's policy titled, Meal Serving guidelines, undated, revealed .The facility will utilize a tray ticket system to ensure diets are served per physician's orders .validating . information in the diet card is correct .special instructions in the diet card will be followed .
Review of the medical record revealed Resident #36 was admitted to the facility on [DATE] with diagnoses including Cerebral Infarction, Peripheral Vascular Diseases, Absence of Right Leg Above Knee, Absence of Left Leg Below Knee, and Gastrointestinal Prosthetic Devices.
Review of a medical provider's progress note for Resident #36 dated 7/17/2024, revealed .MRCP [a non-invasive imaging technique that uses MRI [Magnetic Resonance Imaging, a non-invasive medical imaging technique that uses radio waves and a strong magnetic field to create detailed pictures of the inside of the body] to create detailed pictures of the biliary and pancreatic systems] .completed showing dilated gallbladder with stones, no common bile duct dilation or obstruction. CT [computed tomography] of abdomen showed .gallstones .wall thickening. Surgery was consulted .was not a good surgery candidate. Cystostomy tube placed on 7/8/2024 .HIDA [a nuclear medicine imaging procedure that evaluates the function of the liver, gallbladder, and bile ducts] scan showed cystic duct obstruction and acute cholecystitis .
Review of the Physician's Order Summary Report for Resident #36 dated 7/17/2024, revealed .Chart chole [cholecystostomy-a gallbladder drain] drain output two times a day .
Review of a significant change MDS (Minimum Data Set) assessment for Resident #36 dated 9/9/2024, revealed the resident had a BIMS (Brief Interview of Mental Status) assessment of 00, which indicated severe cognitive impairment.
Review of the comprehensive care plan for Resident #36 dated 10/1/2024, showed the resident's gallbladder drain (a tube with a soft plastic bulb on the end that uses suction to pull fluid out of the body) to the right upper quadrant of the abdomen was not included in the care plan.
During an interview on 11/5/2024 at 2:50 PM, the MDS Care Plan Coordinator stated she was responsible for updating resident care plans. During a review of Resident #36's comprehensive care plan the MDS Care Plan Coordinator confirmed the care plan did not include the resident's gallbladder drain.
Review of the medical record revealed Resident #506 was admitted to the facility on [DATE], was discharged to the hospital and readmitted to the facility on [DATE] with diagnoses including Cerebral Infarction, Chronic Pain Syndrome and Muscle Weakness. The diagnosis of COVID-19 was added on 8/27/2024.
Review of a quarterly MDS assessment dated [DATE], revealed Resident #506 scored a 14 on the BIMS assessment, which indicated the resident was cognitively intact.
Review of the laboratory result for Resident #506 dated 8/26/2024, revealed a positive COVID-19 test result.
Review of the comprehensive care plan for Resident #506 revised 8/23/2024, revealed no care plan interventions for a COVID-19 infection.
Review of a Physician's order for Resident #506 dated 8/27/2024, revealed .Isolation Droplet precautions @ [at] all times due to positive covid 19 test. Mask, googles [goggles], gloves, gown, face shield . The isolation continued until 9/5/2024.
During an interview and record review on 11/8/2024 at 5:00 PM, the Director of Nursing (DON) verified Resident #506 had a COVID-19 infection and confirmed the facility failed to develop a person-centered care plan related to COVID-19.
Review of the medical record revealed Resident #606 was admitted to the facility on [DATE], with diagnoses including Parkinson's Disease, Failure to Thrive, Depression, Cognitive Disorder, and Anxiety.
Review of Resident #606's comprehensive care plan dated 11/1/2024, revealed .Resident is currently under investigation for inappropriate sexual contact .Behavior was unbeknownst to facility prior to admitting .Interventions .supervision of resident .1:1[one on one supervision] .
During an observation on 11/3/2024 at 11:48 AM, Resident #606 was in his room alone sitting in his wheelchair awake. No staff member was observed in residents' room or in the hallway by the resident's room for 1:1 supervision. Continued observation revealed one Patient Care Assistant (PCA) O on the hallway, delivering lunch trays to the residents on the 300-hallway.
During a record review and interview on 11/4/2024 at 9:44 AM, the Admissions Director (AD) verified Resident #606 was not on the Sexual Abuse Registry and stated she had no knowledge of the resident's sexual behaviors prior to admission. The AD stated she was informed by the [NAME] President (VP) of Clinical Services and other regional team members the resident had sexual behaviors towards another person while at a sister facility. The AD stated she was not informed if the alleged victim was a resident and was not informed if the behavior was determined consensual. The AD stated Resident #606 required one-on-one (1:1) supervision and required to always have a staff member with him for the duration of his stay.
During an interview on 11/5/2024 at 2:30 PM, Certified nursing Aide (CNA) U stated she was not told Resident #606 required 1:1 supervision. CNA U also stated the resident did have sexual behaviors towards staff and stated .he would pretend to be asleep and then grab you when you when you got close to him . CNA U further stated Resident #606 was not capable of self propelling the wheelchair out of his room.
During a telephone interview on 11/5/2024 at 9:50 PM, CNA W stated she was not told Resident #606 required 1:1 supervision for sexual behaviors and stated she was only told in report to take an additional staff member with her when she entered Resident #606's room.
During a record review and interview on 11/6/2024 at 3:27 PM, the MDS Care Plan Coordinator reviewed Resident #606's care plan and stated the resident was care planned for sexual behaviors with the 1:1 supervision at all times. The MDS Care Plan Coordinator stated a staff member should have been present at the resident's side at all times and confirmed the facility failed to implement the 1:1 behavior intervention for Resident #606.
Review of the medical record revealed Resident #93 was admitted to the facility on [DATE] with diagnoses including Dementia, Bilateral Macular Degeneration, and Muscle Weakness.
Review of a 5-day MDS assessment dated [DATE], revealed Resident #93 scored an 8 on the BIMS assessment, indicating moderate cognitive impairment.
Review of a comprehensive care plan dated 8/20/2024, revealed Resident #93 had a nutrition care plan with interventions including staff assistance with meals.
Review of the Physician's Orders for Resident #93 dated 9/19/2024, revealed . assist with meals .
During an observation on 11/3/2024 at 11:28 AM, Resident #93 was sitting in a wheelchair in the resident's room. Further observation revealed a breakfast meal tray in the resident's room and 100% of a pureed breakfast meal remained on the meal tray. Continued observation revealed no assistance was being provided.
Review of Resident #93's meal ticket (communication tool used to alert staff of dietary needs) dated 11/3/2024, revealed the resident required meal set up.
Review of the Dietician's Note dated 10/31/2024, revealed staff was to assist the resident with meals.
During an interview on 11/3/2024 at 11:30 AM, Feeding Assistant L stated Resident #93 did not require assist with meals and stated residents who required assist with meals had a yellow meal ticket labeled to assist with meals.
During an interview on 11/3/2024 at 11:35 AM, CNA G stated Resident #93 was not assisted with meals but was given cues or encouraged to eat her meals. CNA G was unaware to assist Resident #93 with meals.
During an observation and interview on 11/4/2024 at 7:56 AM, Activity Assistant H delivered the breakfast meal tray to Resident #93 and exited the resident's room. The resident's meal ticket revealed .set up . Activity Assistant H stated she was not aware the resident required assistance with meals.
During an interview on 11/4/2024 at 8:21 AM, LPN I stated Resident #93 was not assisted with meals, but was to have her meal tray set up and encouraged to eat with cues. LPN I reviewed the resident's care plan and stated .assist with meals .would need a yellow sheet from dietary . LPN I further reviewed the resident's meal ticket and confirmed the meal ticket was not labeled to assist the resident with meals.
During an interview on 11/6/2024 at 8:50 AM, the Speech Therapist (ST) stated she had Resident #93 listed as an Assist/Set Up with meals. The ST reviewed the meal ticket for Resident #93 and confirmed it did not indicate to assist the resident with meals and was inaccurate.
During an interview on 11/7/2024 at 9:56 AM, the MDS Care Plan Coordinator, reviewed the care plan dated 10/3/2024, and stated Resident #93's care plan was to be assisted with meals. The MDS Care Plan Coordinator confirmed the resident's care plan was not implemented.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, medical record review, observation, and interview, the facility failed to administer a feeding ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, medical record review, observation, and interview, the facility failed to administer a feeding tube formula (liquid nutrition delivered through a tube inserted into the stomach) as ordered by the physician for 1 resident (Resident #1) of 2 residents reviewed for tube feeding nutrition.
The findings include:
Review of the facility's undated policy titled, Feeding Tube guidelines, revealed .Ensuring that the administration of enteral nutrition is consistent with and follows the practitioner's orders .
Review of the medical record revealed, Resident #1 was admitted to the facility on [DATE] with diagnoses including Stroke, Epilepsy, Type 2 Diabetes, Gastrointestinal (GI) Bleed, Dysphagia (difficulty swallowing), and Aphasia.
Review of the Physicians Order for Resident #1 dated 10/16/2024, revealed .Glucerna [tube feeding liquid nutrition] 1.5 at 70ML/HR [milliliters per hour] Water Flush 45ML/HR x [times] 22 hrs [hours] .Pleasure pureed [pudding like consistency], thin liquid tray as requested .
Review of a quarterly Minimum Data Set (MDS) assessment dated [DATE], revealed Resident #1 had a Brief Interview for Mental Status (BIMS) score of 00, which indicated the resident was not able to complete the test due to cognitive impairment. Continued review revealed the resident had a Gastrostomy feeding tube (surgically placed device to give direct access to the stomach for feeding, hydration, and medication) for nutrition.
Review of a comprehensive care plan dated 12/11/2024, revealed Resident #1 received tube feeding as his primary source of nutrition and hydration and was at risk for complications including malnutrition, aspiration and dehydration. Continued review revealed Resident #1 received a mechanically altered texture pleasure diet.
Review of a Medication Administration Record (MAR) for Resident #1 dated 1/1/2025, revealed .Diet .Tube Feeding .Glucerna 1.5 at 70 ML/HR .x 22 hours . Continued review revealed .Enteral Feed Order at bedtime. Change tubing, formula and syringe every 24 hours. The MAR revealed a check mark with Licensed Practical Nurse (LPN) A's initials in the 8:00 PM time box which indicated the task was completed.
Review of a Nurse's Note (authored by LPN A) for Resident #1 dated 1/2/2025 at 6:32 AM, revealed .WENT INTO ROOM TO CHECK ON RESIDENT'S TUBE FEEDING .OSMOLITE 1.2 CAL [calorie] [tube feeding liquid nutrition] WAS NOTED TO BE HANGING [being administered through the tube feeding] .GLUCERNA 1.5 CAL PER MD [Medical Doctor] ORDERS .NO S/S [signs and symptoms] OF DISTRESS OR DISCOMFORT .NO N/V [nausea and vomiting] OR DIARRHEA .GLUCERNA 1.5 CAL IMMEDIATELY HUNG [administered]. DON [Director of Nursing] AND .[the Provider] WAS NOTIFIED .
During an observation on 1/21/2025 at 1:00 PM, revealed Resident #1 had Glucerna 1.5 tube feeding formula infusing at 70 ML/HR.
During an interview on 1/22/2025 at 11:45 AM, the Medical Director stated he was notified by the facility's nursing staff, the incorrect tube feeding formula was administered on 1/1/2025 (approximately 10 hours) to Resident #1. The Medical Director stated Resident #1 was monitored several days after the incident and did not exhibit any complications from being administered the incorrect tube feeding formula for the approximately 10 hours.
Review of a Nutrition Progress Note for Resident #1 dated 1/22/2025 at 3:01 PM, revealed .On 1/ 2 [1/2/2025] [administration started on 1/1/2025 at 8:00 PM and ended on 1/2/2025 at 6:32 AM] .he [Resident #1] was given [administered] Osmalite [Osmolite] 1.5 .Error was discovered [by LPN A on 1/2/2025 at 6:32 AM] and feeding was changed to Glucerna 1.5 and resumed without incident .did not have signs .symptoms .distress .discomfort .GI side effects .Osmalite is a general tube feeding formula and does not contain components that would harm [Resident #1] upon administration .
During an interview on 1/23/2025 at 10:30 AM, the Executive Director of Nursing stated it was her expectation the nurses administer the tube feeding formula as ordered by the physician.
Multiple attempts for telephone interview of LPN A from 1/21/2025 - 1/23/2025 were unsuccessful.
Refer to CTFC12 for Plan of Correction
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, observations and interviews, the facility failed to maintain and store oxygen equipment in a cl...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, observations and interviews, the facility failed to maintain and store oxygen equipment in a clean and sanitary condition for 2 residents (Resident #39 and Resident #59) of 8 residents reviewed for oxygen equipment storage.
The findings include:
Review of the facility policy titled, Respiratory Equipment Cleaning GUIDELINES, undated, revealed .weekly cleaning activities includes .tubing and air dry .Replace equipment immediately when it is .visible soiling .Cover respiratory items with plastic bag when not in use .
Medical record review revealed Resident #39 was admitted to the facility on [DATE], with diagnoses including Dementia, Skin Cancer, Depression and Low Back Pain.
During an observation on 11/6/2024 at 9:25 AM, a nebulizer mask [oxygen mask used to deliver medications] was lying on Resident #39's nightstand and was not covered or stored in a bag. Licensed Practical Nurse (LPN) C confirmed Resident #39's nebulizer mask was not stored in a sanitary condition and was available for resident use.
During an observation on 11/7/2024 at 9:50 AM, a nebulizer mask was lying on Resident #39's nightstand and was not covered or stored in a bag. LPN C confirmed Resident #39's nebulizer mask was not stored in a sanitary condition and was available for resident use.
Medical record review revealed Resident #59 was admitted to the facility on [DATE], with diagnoses including Chronic Obstructive Pulmonary Disease (COPD), Pneumonia, Kidney Disease and Shortness of Breath.
During an observation on 11/3/2024 at 11:45 AM, Resident #59 had multiple nebulizer masks in the room, stored in bags with various dates written on the bag. A nebulizer mask was bagged and dated 9/8/2024, another mask was bagged and dated 11/3/2024, and 1 nebulizer mask, with a cloudy substance on the surface of the mask, was dated 9/22/2024, was attached to the nebulizer machine, lying on the resident's nightstand, and was not labeled or stored in a bag.
During an observation and interview on 11/4/2024 at 1:30 PM, LPN A observed Resident #59's multiple nebulizer masks and stated nebulizer masks were changed by night shift weekly on Sundays. LPN A stated she did not know who changed the nebulizer masks and stated she was unsure when nebulizer masks were cleaned. LPN A stated the mask dated 9/8/2024 and the mask dated 9/22/2024 were considered out of date and should have been discarded. LPN A confirmed the nebulizer mask dated 9/22/2023 was soiled, connected to the nebulizer machine, was not stored in a sanitary condition, and was available for resident use.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, medical record review, observation, and interview, the facility failed to ensure a physician or...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, medical record review, observation, and interview, the facility failed to ensure a physician order for bed rail usage was obtained prior to use for 1 resident (Resident #99) of 3 residents reviewed for bed rails.
The findings include:
Review of the facility's policy titled, Physician Orders, undated, revealed .A physician .nurse practitioner .must provide written .verbal orders for the residents' care and needs .
Review of the facility's policy titled, Bed Rails Use guidelines, undated, revealed .It is the policy of this facility to utilize a person-centered approach when determining the use of bed rails .ongoing .supervision .including documentation .
Review of the medical record revealed Resident #99 was admitted to the facility on [DATE] and readmitted on [DATE] with diagnoses including Epilepsy, Dehydration, Cerebral Palsy, and Protein-Calorie Malnutrition.
Review of a Bed Rail Evaluation assessment for Resident #99 dated 9/18/2024, revealed the resident had a signed consent for bed rail use.
Review of a comprehensive care plan for Resident #99 dated 9/20/2024, revealed the resident had a care plan for Cerebral Palsy and interventions included full side rails with padding for protection against rocking behaviors and seizure activity, padded/pillows for positioning of bed rails. Further review revealed the care plan was not revised until 11/4/2024 to include padded bed rails with padding and pillows.
Review of a quarterly Minimum Data Set (MDS) assessment dated [DATE], revealed Resident #99 was rarely/never understood.
During an observation on 11/3/2024 at 5:00 PM, Resident #99 was observed lying in bed with padded bed rails in place.
During an observation on 11/5/2024 at 5:15 PM, revealed Resident #99's bed had padded full bed rails in place to the bed.
Review of the physician orders for Resident #99 revealed the resident did not have a physician order for bed rails prior to 11/5/2024.
During an interview on 11/6/2024 at 3:30 PM, the Assistant Director of Nursing (ADON) confirmed there was no physician's order for padded full bed rails prior to 11/5/2024.
During an interview on 11/7/2024 11:00 AM, the Director of Nursing (DON) confirmed a physician's order for bed rails was not obtained prior to use for Resident #99.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, facility documents, medical record review and interviews, the facility failed to maintain compl...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, facility documents, medical record review and interviews, the facility failed to maintain complete records of pharmacy reviews and a record of the provider's responses to irregularities identified by the pharmacist for 2 residents (Resident #37 and Resident #71) of 5 residents reviewed for pharmacy services.
The findings include:
Review of the facility policy titled, Pharmacy Services, revealed .The licensed pharmacist will collaborate with facility leadership and staff to coordinate pharmaceutical services within the facility, guide development and evaluation of pharmaceutical services procedures and help the facility identify, evaluate and resolve pharmaceutical concerns .The facility in coordination with the licensed pharmacist will provide .A system of medication records that enables periodic accurate reconciliation .
Review of the medical record revealed Resident #37 was admitted to the facility on [DATE], with diagnoses including Rheumatoid Arthritis, Chronic Respiratory Failure, Heart Failure, Fibromyalgia, Anxiety Disorder, Bipolar Disorder, Chronic Pain and Depression.
Review of the annual Minimum Data Set (MDS) assessment dated [DATE], revealed Resident #37 scored a 15 on the Brief Interview for Mental Status (BIMS) assessment, which indicated the resident was cognitively intact. Further review revealed the resident was taking antipsychotic, antianxiety, and antidepressant medications.
Review of the documents titled, Record of Drug Regimen Review Report-Consultant Notes, for Resident #37, dated 3/20/2024, 5/14/2024, and 8/19/2024, revealed medication irregularities and recommendations identified by the pharmacist.
Review of Resident #37's medical record did not include separate documents of the pharmacist's identified irregularities with the provider's response to the identified irregularities.
Review of the medical record revealed Resident #71 was admitted to the facility on [DATE] with diagnoses including Delusional Disorder, Psychosis, Anxiety, Dementia, Altered Mental Status and Stroke.
Review of the documents titled, Record of Drug Regimen Review Report-Consultant [Pharmacist] Notes, for Resident #71, revealed medication irregularities and recommendations identified by the pharmacist on 12/20/2023, 6/18/2024, 7/17/2024, 8/19/2024, and 9/16/2024.
Review of Resident #71's medical record did not include separate documents of the pharmacist's identified irregularities with the provider's response to the identified irregularities.
During medical record review and interview on 11/6/2024 10:30 AM, the Medical Record Clerk confirmed the facility had not maintained the pharmacist's recommendations with a physician response for Resident #37 and Resident #71.
During an interview on 11/6/2024 at 10:44 AM, the Administrator confirmed the facility had not maintained records of the pharmacist's recommendations with a physician response for Resident #71 from 12/20/2023 to 6/18/2024.
During an interview on 11/6/2024 at 10:47 AM, the [NAME] President (VP) of Clinical Services confirmed the facility had not maintained a complete monthly pharmacist review with recommendations for Resident #37 and Resident #71. The VP of Clinical Services confirmed the facility did not have records to indicate the provider was notified and did not have records of the provider's responses.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility documentation review, medical record review, and interview, the facility failed to complete the facility asses...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility documentation review, medical record review, and interview, the facility failed to complete the facility assessment to accurately reflect the needs and services provided by the facility, which had the potential to affect 2 of 99 residents (Residents #52 and #86).
The findings include:
Review of the Facility Assessment Tool dated 7/18/2024, revealed .Ethnic, cultural .factors .Describe ethnic, cultural .or personal resident preferences that may potentially affect the care provided to residents by .facility. Examples .include .languages .Presently, no resident falls outside the homogenous local culture, language .
Review of the medical record revealed Resident #52 was admitted to the facility on [DATE] with diagnoses including Major Depressive Disorder, Anxiety, Intellectual Disability, and Autism.
Review of a quarterly Minimum Data Set (MDS) assessment dated [DATE], revealed Resident #52 scored an 11 on the Brief Interview for Mental Status (BIMS) assessment which indicated the resident had moderate cognitive impairment.
Review of a comprehensive care plan for Resident #52 dated 11/8/2022 revealed .has preference in how she identifies and would like the care team to be aware . Interventions included . identifies as a female and wants the pronouns of 'her', 'she' used when addressing her .likes to dress in female clothing .
Review of the medical record revealed Resident #86 was admitted to the facility on [DATE] with diagnoses of Cerebral Infarction and Dementia.
Review of a provider progress note for Resident #86 dated 1/25/2024, revealed .Speaks only Russian .Communication performed with translator. Resident hesitant to answer but does answer yes and no questions .Translator app used for communication with limited results due to the underlying dementia .
Review of Resident #86's comprehensive care plan dated 8/31/2024, revealed .Communication .native language is Russian .
Review of the annual MDS assessment dated [DATE], revealed Resident #86 preferred language is Russian. Cognitive skills for daily decision-making revealed Resident #86 had severe cognitive impairment.
During an interview on 11/7/2024 at 2:00 PM, the Administrator confirmed the facility assessment updated 7/18/2024 was not accurate and did not reflect Resident #52 as being transgender and identifying as a female and Resident #86's native language barrier.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Review of the medical record revealed Resident #79 was admitted to the facility on [DATE] with diagnoses including Hemiplegia, C...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Review of the medical record revealed Resident #79 was admitted to the facility on [DATE] with diagnoses including Hemiplegia, Cerebral Infarct, Gastrostomy Status and Dysphagia.
Review of a Physician's Order Summary Report for Resident #79 dated 12/17/2022, revealed Lexapro (anti-depressant medication) 20 milligram (mg) daily.
Review of the comprehensive care plan dated 12/19/2022 and revised on 3/1/2023, revealed Resident #79 was at risk for adverse side effect related to use of antidepressant medications with interventions which included to administer antidepressant medications as ordered.
Review of a facility document for Resident #79 dated 6/2023, revealed the medication Lexapro was recommended by the pharmacist to be decreased from 20 mg to 15 mg daily. The physician agreed to the reduction and decreased the Lexapro to 10 mg daily on 6/27/2023.
Review of a quarterly Minimum Data Set (MDS) assessment dated [DATE], revealed Resident #79 was never/rarely understood. Further review revealed the resident had a feeding tube.
During a medication administration observation on 11/4/2024 at 9:15 AM, revealed LPN I administered Lexapro 10 mg to Resident #79. The medication (Lexapro) was packaged as 1 tablet and labeled as 10 mg.
Review of the medication administration record (MAR) for Resident #79 dated 11/1/2024-11/4/2024, revealed the Lexapro 20 mg order had been signed as given by the nursing staff.
Review of the MAR for Resident #79 dated 5/1/2024 through 11/4/2024, revealed the order for Lexapro 20 mg was documented as administered by the nursing staff every month for the 6 month time frame reviewed.
During an interview on 11/6/2024 at 11:51 AM, the [NAME] President (VP) of Clinical Services confirmed the facility failed to transcribe the order for Lexapro 10 mg accurately on 6/27/2023 into the electronic medical record (EMR) which resulted in a transcription error from 6/27/2023 through 11/4/2024 (over 1 year and 4 months, the correct dose of medication (10 mg) was administered however the correct order for Lexapro 10 mg was not documented in the medication administration record.
During a telephone interview on 11/6/2024 at 4:40 PM, the Pharmacist stated the pharmacy received and processed the order to decrease the Lexapro to 10 mg on 6/27/2023. The Pharmacist further stated Lexapro 10 mg had been delivered to the facility since 6/27/2023.
During an interview on 11/7/2024 at 10:17 AM, the DON confirmed the nursing staff failed to accurately transcribe the Lexapro prescription order for Resident #79 since 6/2023.
Based on facility policy review, medical record review, observations, and interviews, the facility failed to ensure a COVID-19 test result was accurately documented for 5 residents (Resident #37, #45, #33, #80, and #94) of 40 residents reviewed for COVID-19 testing documentation. The facility failed to ensure an order for a urinalysis was obtained timely for 1 resident (Resident #30) of 3 resident reviewed for laboratory services. The facility failed to transcribe a physician's order accurately and timely for 1 resident (Resident #79) of 5 residents reviewed for medication administration.
The findings include:
Review of the facility's policy titled, Laboratory Services Guidelines, undated, revealed .the facility must provide or obtain laboratory services when ordered by a physician .the facility is responsible for the timeliness of the services .
Review of the facility's policy titled, Physician Orders, undated, revealed .A physician, physician assistant, nurse practitioner [NP] or clinical specialist must provide written and/or verbal orders for the residents' care and needs .The written and/or verbal orders should include at a minimum .Medication orders if indicated .
Review of the facility's policy titled, Medication Administration via Enteral Tube, undated, revealed .It is the policy of this facility to ensure the safe and effective administration of medications via enteral feeding tubes by utilizing best practice guideline .Verify physician orders for medication and enteral tube flush amount .
Review of the facility's policy titled, Physician Orders Transcription, undated, revealed .The attending physician shall authenticate orders for the care and treatment of assigned residents .For physician/practitioner orders received in writing or via fax, the nurse in a timely manner will .Call the attending physician to verify the order .Document the verification order by entering the order and the time, date, and signature on the physician order sheet .Follow facility procedures for verbal or telephone orders including: noting the order, submitting to pharmacy, and transcribing to medication or treatment administration record .
Review of the medical record revealed Resident #37 was admitted to the facility on [DATE] with diagnoses including Rheumatoid Arthritis, Heart Failure, and Fibromyalgia. The diagnosis of COVID-19 was added on 9/4/2024.
Review of an annual Minimum Data Set (MDS) assessment dated [DATE], revealed Resident #37 scored a 15 on the Brief Interview for Mental Status (BIMS) assessment which indicated the resident was cognitively intact.
Review of a NP Progress Note for Resident #37 dated 9/4/2024, revealed .being seen due to testing positive for COVID this morning via nasal swab in the facility .
Review of a physician's order for Resident #37 dated 9/4/2024, revealed .Isolation Droplet precautions @ [at] all times due to positive covid 19 test. Mask, googles [goggles], gloves, gown, face shield .Vital Signs monitoring for Covid Positive every 4 hours throughout covid positive Isolation precautions . the isolation and vital sign monitoring continued until 9/15/2024.
Review of a comprehensive care plan for Resident #37 dated 9/5/2024, revealed the resident had tested positive for COVID-19 with interventions including .Observe vital signs. Notify physician if abnormal .Resident under droplet precautions .
Review of the medical record for Resident #37 revealed no documentation of a positive COVID-19 test available for review.
Medical record review revealed Resident #45 was admitted to the facility on [DATE] with diagnoses including Cerebral Infarction, Hypertension, and Chronic Pain Syndrome. The diagnosis of COVID-19 was added on 8/21/2024.
Review of the NP Progress Note revealed for Resident #45 dated 8/21/2024, revealed .Resident was seen today due to positive result of COVID [COVID-19] swab in facility .
Review of a physician's order for Resident #45 dated 8/21/2024, revealed .Isolation Droplet precautions @ all times due to positive covid 19 test. Mask, googles, gloves, gown, face shield . The isolation continued until 8/31/2024.
Review of a physician's order for Resident #45 dated 8/23/2024, revealed .Vital Signs monitoring for Covid Positive every 4 hours throughout covid positive Isolation precautions . and continued until 8/31/2024.
Review of a comprehensive care plan for Resident #45 dated 8/26/2024, revealed the resident had tested positive for COVID-19 with interventions including .Observe vital signs. Notify physician if abnormal .Resident under droplet precautions .
Medical record review for Resident #45 revealed no documentation of a positive COVID 19 test conducted from 8/20/2024-8/26/2024.
Review of a significant change MDS assessment dated [DATE], revealed Resident #45 scored a 12 on the BIMS assessment which indicated the resident had moderate cognitive impairment.
Review of the medical record revealed Resident #33 was admitted to the facility on [DATE] with diagnoses including Hypertension, Chronic Pain, Heart Failure, and Difficulty Walking. The diagnosis of COVID-19 was added on 8/22/2024.
Review of an admission MDS assessment dated [DATE], revealed Resident #33 scored a 7 on the BIMS assessment which indicated the resident had severe cognitive impairment.
Review of the laboratory results for Resident #33 dated 8/16/2024, 8/18/2024, and 8/21/2024, revealed negative COVID-19 test results.
Review of the laboratory results for Resident #33 dated 8/23/2024, revealed the COVID-19 test result was flagged as abnormal which indicated the test was positive. Continued review of the laboratory result revealed the nurse had documented NEG in the notes field of the document which indicated a negative COVID-19 test result. The laboratory results form contained conflicting results.
Review of a physician's order for Resident #33 dated 8/23/2024, revealed .Isolation Droplet precautions @ all times due to positive covid 19 test. Mask, googles, gloves, gown, face shield . The isolation continued until 8/31/2024.
Review of a physician's order for Resident #33 dated 8/23/2024, revealed .Vital Signs monitoring for Covid Positive every 4 hours throughout covid positive Isolation precautions . and continued until 8/31/2024.
Review of a comprehensive care plan for Resident #33 dated 8/23/2024, revealed the resident had tested positive for COVID-19 with interventions including .Observe vital signs. Notify physician if abnormal .Resident under droplet precautions .
During an interview on 11/12/2024 at 3:48 PM, the [NAME] President of Clinical Services stated according to the Nurse Practitioner vist note for Resident #33 dated 8/26/2024, revealed the resident was evaluated for a positive COVID-19 diagnosis after testing positive for COVID-19 on 8/23/2024. Continued interview confirmed the COVID-19 test result documentation dated 8/23/2024 was inaccurately documented as NEG when the resident had an active COVID-19 diagnosis and positive test result.
Medical record review revealed Resident #80 was admitted to the facility on [DATE], was discharged to the hospital, and readmitted to the facility on [DATE] with diagnoses including Chronic Kidney Disease, Diabetes, Hypertension, and Heart Failure. The diagnosis of COVID-19 was added on 8/26/2024.
Review of an admission MDS assessment dated [DATE], revealed Resident #80 scored a 10 on the BIMS assessment which indicated the resident had moderate cognitive impairment.
Review of the NP Progress note for Resident #80 dated 8/26/2024, revealed .Resident was seen today for a follow-up after recent positive COVID-19 swab .
Review of a physician's order for Resident #80 dated 8/26/2024, revealed .Isolation Droplet precautions @ all times due to positive covid 19 test. Mask, googles, gloves, gown, face shield .Vital Signs monitoring for Covid Positive every 4 hours throughout covid positive Isolation precautions . The isolation and vital sign monitoring continued until 9/3/2024.
Review of a comprehensive care plan for Resident #80 dated 8/26/2024, revealed the resident had tested positive for COVID-19 with interventions including .Observe vital signs. Notify physician if abnormal .Resident under droplet precautions .
Review of the medical record for Resident #80 revealed no documentation of a positive COVID 19 test result.
Review of the medical record revealed Resident #94 was admitted to the facility on [DATE], discharged to home on [DATE], and readmitted to the facility on [DATE] with diagnoses including Dementia, Asthma, Chronic Obstructive Pulmonary Disease, Atrial Fibrillation, and Wheezing.
Review of the admission MDS assessment dated [DATE], revealed Resident #94 scored a 1 on the BIMS assessment which indicated severe cognitive impairment.
Review of the laboratory results for Resident #94 dated 10/23/2024, 10/25/2024, and 10/28/2024, revealed a negative COVID 19 test.
Review of the laboratory results for Resident #94 dated 10/30/2024, 11/1/2024, or 11/4/2024, revealed the COVID 19 test result did not indicate a positive or negative result.
Review of a NP Progress Note for Resident #94 dated 10/31/2024, revealed .Chief Complaint/Nature of Presenting Problem: COVID .intermittent cough .tested positive for COVID-19. Symptomatic management .
Review of a NP Progress Note for Resident #94 dated 11/1/2024, revealed .Chief Complaint/Nature of Presenting Problem: f/up [follow up] covid .continues to experience an intermittent cough .tested positive for COVID-19 3 days ago [10/29/2024] .monitor closely for effectiveness of medication .Nursing and staff to continue to monitor for any acute changes or concerns .
Review of a NP Progress Note for Resident #94 dated 11/8/2024, revealed .Resident reportedly tested positive by nursing staff, today is day 10 .improving .
During an interview and review of Resident #94's electronic medical record (EMR) on 11/8/2024 at 12:05 PM, the Director of Nursing (DON) stated she was unable to view the results of Resident #94's COVID 19 testing results for 10/30/2024, 11/1/2024, or 11/4/2024 under the results tab of the EMR and was unable to specify the results of the testing. The DON stated she was not sure why the results were not listed under the results tab and it may be related to a computer system issue.
During an interview and review of Resident #94 EMR on 11/8/2024 at 12:07 PM, the Licensed Practical Nurse (LPN) Risk Manager stated after he obtained COVID 19 test of residents, he entered the results under the results tab of the electronic medical record. The LPN Risk Manager stated he was unable to verify the COVID 19 test results for Resident #94 on 10/30/2024, 11/1/2024, or 11/4/2024 as it had not been documented under the results tab of the EMR.
During an interview on 11/8/2024 at 3:15 PM, the Director of Nursing (DON) stated she had researched the COVID results on the electronic medical record for Resident #94 and stated after the test results were received, the nurse may opt to write in a negative result or click abnormal or normal. If the abnormal box was checked, the system flags the test result to show there was a positive test result. If the normal box was checked there was no flag which indicated the test was negative. Results of the COVID-19 test was inconsistenly documented on the results form.
Review of the medical record revealed Resident #30 was admitted to the facility on [DATE] and readmitted on [DATE] with diagnoses including Chronic Kidney Disease, Dementia, and Muscle Weakness.
Review of an Acute Visit Progress Note dated 10/9/2024, revealed NP L evaluated Resident #30 and ordered a urinalysis.
Review of a Physician's Order for Resident #30 on 10/9/2024, revealed an order to obtain UA (urinalysis) to culture. Further review revealed the order to obtain the UA to culture was discontinued on 10/13/2024 (4 days later) by Licensed Practical Nurse (LPN) D.
Review of a Follow-Up Visit Note dated 10/12/2024, revealed NP X evaluated Resident #30 and re-ordered the urinalysis. Further review revealed there were no UA results as previously ordered for the provider to review.
Review of a Physician's Order for Resident #30 on 10/13/2024, revealed an order to obtain a UA C&S (culture and sensitivity) (after the previous order dated 10/9/2024 was discontinued on 10/13/2024).
Review of the Medication Administration Record (MAR) for Resident #30 dated 10/2024, revealed the order for UA C&S dated 10/13/2024 was signed off as completed on 10/14/2024 at 7:52 AM by LPN E.
Review of an Acute Visit Progress Note dated 10/16/2024, revealed NP L evaluated Resident #30 for altered mental status (AMS) and again re-ordered the UA. Further review revealed there were no UA results as previously ordered for the provider to review.
Review of a Physician's Order for Resident #30 on 10/16/2024, revealed an order to obtain a UA Culture and Sensitivity for increased confusion.
Review of a quarterly MDS assessment dated [DATE], revealed Resident #30 scored a 5 on the Brief Interview for Mental Status (BIMS) assessment which indicated the resident had severe cognitive impairment. Further review revealed the resident required partial/ moderate assistance with toileting and had falls after admission into the facility.
Review of a Follow-Up Visit Note dated 10/17/2024, revealed NP L evaluated Resident #30 for a possible urinary tract infection and again re-ordered the UA. Further review revealed there were no UA results as previously ordered for the provider to review.
Review of a UA test result for Resident #30 dated 10/17/2024, revealed no abnormalities present in the urine. Further review revealed the urine specimen was obtained on 10/17/2024 at 4:00 PM.
Review of a UA C&S result for Resident #30 dated 10/21/2024, revealed the presence of bacteria in Resident #30's urine after the culture was performed.
Review of a Follow-Up Visit Note dated 10/21/2024, revealed NP L evaluated Resident #30 for review of UA results with altered mental status. NP L ordered an antibiotic for a urinary tract infection for Resident #30.
Review of a comprehensive care plan revised 11/4/2024, revealed Resident #30 required assistance of 1 staff member for toileting and was at risk for altered bladder elimination.
During a telephone interview on 11/6/2024 at 4:19 PM, LPN D stated she discontinued the UA ordered on 10/9/2024 and reordered the UA sample to be completed on 10/14/2024. LPN D stated she cannot recall why she discontinued the original order but does recall speaking to the NP (unknown) about rescheduling the UA for the nightshift nurse to obtain. LPN D stated she tried to obtain the urine sample on Resident #30 multiple times by clean catch method however due to the resident's cognition, she was unable to obtain the urine sample. LPN D stated she did not document the failed attempts to collect the urine specimen on Resident #30 in the medical record.
During a telephone interview on 11/6/2024 at 4:27 PM, LPN E stated she signed off the UA order on 10/14/2024 as completed in the medical record. LPN E stated she signed off the order as completed however she was unable to collect the specimen. LPN E stated she had tried to obtain the urine sample on Resident #30 multiple times by clean catch method however due to the resident's cognition she was unable to obtain. LPN E stated she also attempted to obtain the urine sample via straight cath (catheter) method however due to the resident's cognition and behaviors she was unable to collect. LPN E stated she did not document the attempts to collect the urine specimen on Resident #30 in the medical record and did not notify the provider of the failed attempts to collect the urine sample. LPN E stated she could not recall if she had collected the urine specimen on Resident #30 as ordered on 10/16/2024.
During a telephone interview on 11/6/2024 at 4:46 PM, NP L stated she initially ordered a UA for altered mental status for Resident #30 on 10/9/2024. NP L stated she could not recall when the UA was obtained by the nursing staff. NP L stated between her intermittent follow-up visits (10/9/2024-10/17/2024) with Resident #30 there were no UA results to review. NP L stated the expected time frame for a UA order to be carried out and obtained was within 24 hours. NP L stated it was also the expectation if the nursing staff could not obtain or carry out an order (UA sample) the medical provider should be notified for further guidance. NP L stated she was not notified by the nursing staff of any issues with obtaining the UA sample for Resident #30.
During an interview on 11/7/2024 at 8:50 AM, LPN N stated she oversaw the laboratory process at the facility and stated she recalled the order on 10/9/2024 to obtain the UA on Resident #30. LPN N stated the staff had attempted to get the urine for Resident #30 and was unsuccessful. LPN N confirmed there was no documentation in the medical record regarding the physician notification or the failed attempts to collect the urine specimen. LPN N stated the nurses should have documented any procedure conducted for Resident #30 in the medical record.
During an interview on 11/7/2024 at 9:00 AM, LPN C stated she worked day shift on 10/17/2024 and was pretty sure she collected the urine specimen on Resident #30. LPN C confirmed she failed to document the urinalysis collection for Resident #30 in the medical record.
During an interview on 11/7/2024 at 9:15 AM, the Director of Nursing (DON) reviewed the medical record for Resident #30 and confirmed the urinalysis test ordered originally for 10/9/2024 was not completed timely. DON stated any medical procedure, change in resident status, and assessment should be documented in the medical record. The DON confirmed the procedure of obtaining urinalysis test with the failed attempts was not documented in the medical record.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, medical record review and interview, the facility failed to develop and implement the base line...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, medical record review and interview, the facility failed to develop and implement the base line care plan for active COVID-19 infections for 4 of 6 (Resident #608, #615, #617, and #509) residents admitted with an active COVID-19 infection.
The findings include:
Review of the facility's policy titled, Baseline Care Plan Guidelines, undated, revealed .it is the policy of the facility to develop and implement a baseline care plan for each resident that includes the instructions needed to provide effective and person-centered care .the baseline care plan will .be developed within 48 hours of a resident ' s admission .
Review of the medical record revealed Resident #608 was admitted to the facility on [DATE] with diagnoses including COVID-19, Shortness of Breath, and Fatigue.
Review of a baseline care plan for Resident #608 dated 8/9/2024, revealed the resident did not require isolation or quarantine for active infectious disease.
Review of a Physician's Order for Resident #608 dated 8/9/2024, revealed .isolation droplet precautions .[at] .all times due to positive covid 19 [COVID-19] test .mask .goggle [goggles] gloves, gown, face shield .vital signs monitoring for Covid [COVID-19] Positive every 4 hours throughout covid [COVID-19] isolation precautions .
Review of a 5-day Minimum Data Set (MDS) assessment dated [DATE], revealed Resident #608 scored a 3 on the Brief Interview for Mental Status (BIMS) assessment which indicated the resident had severe cognitive impairment. Further review revealed the resident had an active COVID-19 infection and required isolation or quarantine for an active infectious disease.
Review of the medical record revealed Resident #615 was admitted to the facility on [DATE] with diagnoses including COVID-19, Shortness of Breath, and Muscle Weakness.
Review of a baseline care plan for Resident #615 dated 8/30/2024, revealed the resident did not require isolation or quarantine for active infectious disease.
Review of a Physician's Order for Resident #615 dated 8/30/2024, revealed .isolation droplet precautions .[at] .all times due to positive covid 19 [COVID-19] test .mask .googles [goggles] gloves, gown, face shield .vital signs monitoring for Covid [COVID-19] Positive every 4 hours throughout covid [COVID-19] isolation precautions .
Review of a 5-day Minimum Data Set (MDS) assessment dated [DATE], revealed Resident #615 scored a 10 on the BIMS assessment which indicated the resident had moderate cognitive impairment. Further review revealed the resident had an active COVID-19 infection and required isolation or quarantine for an active infectious disease.
Review of the medical record revealed Resident #617 was admitted to the facility on [DATE] with diagnoses including COVID-19, Hypertension, and Difficulty Walking.
Review of the medical record revealed Resident #617 did not have a baseline care plan initiated or developed to for isolation or quarantine for an active COVID-19 infection.
Review of a Physician s Order for Resident #617 dated 10/21/2024, revealed .isolation droplet precautions .[at] .all times due to positive covid 19 [COVID-19] test .mask .googles [goggles] gloves, gown, face shield .vital signs monitoring for Covid [COVID-19] Positive every 4 hours throughout covid [COVID-19] isolation precautions .
Review of a 5-day Minimum Data Set (MDS) assessment dated [DATE], revealed Resident #617 scored a 14 on the BIMS assessment which indicated the resident was cognitively intact. Further review revealed the resident had an active COVID-19 infection and required isolation or quarantine for an active infectious disease.
Review of the medical record revealed Resident #509 was admitted to the facility on [DATE] with diagnoses including COVID-19, Hypertension, and Seizures.
Review of the medical record revealed Resident #509 did not have a baseline care plan initiated or developed for isolation or quarantine for an active COVID-19 infection.
Review of a Physician's Order for Resident #509 dated 10/31/2024, revealed .isolation droplet precautions .[at] .all times due to positive covid 19 [COVID-19] test .mask .googles [goggles] gloves, gown, face shield .vital signs monitoring for Covid [COVID-19] Positive every 4 hours throughout covid [COVID-19] isolation precautions [started 10/30/2024] .
Review of a 5-day Minimum Data Set (MDS) assessment dated [DATE], revealed Resident #509 scored a 13 on the BIMS assessment which indicated the resident was cognitively intact. Further review revealed the resident had an active COVID-19 infection and required isolation or quarantine for an active infectious disease.
During an interview on 11/12/2024 at 6:15 PM, the MDS/Care Plan Coordinator confirmed the baseline care plans for Resident #608, Resident #615, Resident #617, and Resident #509 were not developed and implemented regarding the need for isolation or quarantine for an active Covid-19 infection to alert employees of the need to wear PPE to prevent and control the spread of COVID-19 to the residents and the employees.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, Centers for Disease (CDC) recommendations and guidance review, facility documents review, medic...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, Centers for Disease (CDC) recommendations and guidance review, facility documents review, medical record review, and interview, the facility failed to ensure COVID-19 positive residents had care plans timely revised to include COVID-19 isolation requirements and personal protective equipment (PPE) usage by employees, recommended by the CDC, to control the exposure and spread of the COVID-19 virus during the facility's COVID-19 outbreak from 8/9/2024 through 11/16/2024, for 10 residents (Residents #53, #609, #510, #68, #93, #15, #615, #507, #619 and #509) of 40 residents reviewed for care plans. The facility failed to ensure fall interventions were revised on the care plan for 1 resident (Resident #43) of 3 residents reviewed for falls and failed to revise the code status for 1 resident (Resident #95) of 24 residents reviewed for advance directives.
The findings include:
Review of the CDC's guidance titled, Infection Control Guidance: SARS-CoV-2, dated 6/24/2024, revealed .Ensure everyone is aware of recommended IPC [infection prevention and control] practices in the facility .Source control is recommended for individuals in healthcare settings who: Have suspected or confirmed SARS-CoV-2 infection or other respiratory infection (e.g., those with runny nose, cough, sneeze); or had close contact (patients and visitors) or a higher-risk exposure (HCP) with someone with SARS-CoV-2 infection, for 10 days after their exposure . Perform testing for all residents and HCP identified as close contacts or on the affected unit(s) if using a broad-based approach, regardless of vaccination status.
Review of the facility's policy titled, Care Plans, Comprehensive Person-Centered, undated, revealed Each resident's comprehensive person-centered care plan is consistent with the resident's [needs] .revisions to the plan of care .includes measurable objectives and timeframes .describes the services that are to be furnished .reflects currently recognized standards of practice .care plans are revised as information about the residents and the residents' condition change .The interdisciplinary team reviews and updates the care plan .when there has been .change in the resident's condition .when the desired outcome is not met .
Medical record review revealed Resident #53 was admitted to the facility on [DATE] with diagnoses including Arthritis, Hepatitis C, Type 2 Diabetes, Obstructive Uropathy and Benign Prostatic Hyperplasia (BPH).
Review of a quarterly Minimum Data Set (MDS) assessment dated [DATE], revealed Resident #53 scored a 15 on the Brief Interview for Mental Status (BIMS) assessment, which indicated the resident was cognitively intact.
Review of the Physician's Orders for Resident #53 dated 9/3/2024, revealed .Isolation Droplet precautions @ [at] all times due to positive covid 19 test .Mask, googles [goggles], gloves, gown, face shield .All services provided in resident room .every shift until 9/14/2024 .
Review of Resident #53's comprehensive care plan dated 9/5/2024, revealed the care plan was not revised to include an active COVID-19 infection or COVID-19 isolation requirements.
Medical record review revealed Resident #609 was admitted to the facility on [DATE] with diagnoses including Thyroid Cancer, Chronic Pain, Pneumonia, COVID-19 (added 9/4/2024), Diabetes, and Anxiety.
Review of the Physician's Orders for Resident #609 dated 8/23/2024, revealed .Resident has an active infection on droplet precautions .Covid 19 .
Review of the admission MDS assessment dated [DATE], revealed Resident #609 scored a 7 on the BIMS assessment, which indicated severe cognitive impairment.
Review of the comprehensive care plan for Resident #609 dated 8/26/2024, revealed .Resident is positive for Covid 19 .Observe/document breath sounds . the use of any accessory muscle .Monitor .respiratory distress .shortness of breath . Further review revealed the care plan was not revised to include COVID-19 isolation requirements until 3 days after the positive COVID-19 test.
Medical record review revealed Resident #510 was admitted to the facility on [DATE] with diagnoses including Heart Failure, Atrial Fibrillation, Chronic Kidney Disease, and Stenosis of Carotid Artery.
Review of a quarterly MDS assessment dated [DATE], revealed Resident #510 scored a 13 on the BIMS assessment, which indicated the resident was cognitively intact.
Review of a laboratory result for Resident #510 dated 8/24/2024, revealed .positive rapid covid test .
Review of the Physician's Orders for Resident #510 dated 8/26/2024 revealed .Isolation Droplet precautions @ all times due to positive covid 19 test .Mask, googles, gloves, gown, face shield .All services provided in resident room .every shift until 9/2/2024 .
Review of Resident #510's comprehensive care plan dated 8/26/2024 revealed .Droplet precautions .Covid 19 .interventions .Check for proper PPE, hand washing, and Droplet isolation sign in place . Further review revealed the care plan was not revised to include COVID-19 isolation requirements until 2 days after the positive COVID-19 test.
Medical record review revealed Resident #68 was admitted to the facility on [DATE] and readmitted on [DATE] with diagnoses including Type 2 Diabetes, Morbid Obesity, Heart Failure, and Hypertension.
Review of a quarterly MDS assessment dated [DATE], revealed Resident #68 scored a 15 on the BIMS assessment, which indicated the resident was cognitively intact.
Review of the Physician's Orders for Resident #68 dated 9/3/2024, revealed . Droplet precautions .All services provided in resident room .Covid positive Precautions .every shift for 3 days .
Review of Resident #68's comprehensive care plan dated 9/5/2024, revealed .Resident is positive for Covid 19 .interventions .Emphasize good hand washing techniques . Further review revealed the care plan was not revised with interventions to include COVID-19 isolation requirements.
Medical record review revealed Resident #93 was admitted to the facility on [DATE] with diagnoses including Pneumonia, Hypothyroidism, Goiter, and Difficulty Walking.
Review of an admission MDS assessment dated [DATE], revealed Resident #93 scored an 8 on the BIMS assessment, which indicated moderate cognitive impairment.
Review of the Physician's Orders for Resident #93 dated 8/23/2024, revealed .Isolation Droplet precautions @ all times due to positive covid 19 test .Mask, googles, gloves, gown, face shield .All services provided in resident room .every shift until 9/2/2024 .
Review of Resident #93's comprehensive care plan dated 8/26/2024, revealed .Droplet precautions .interventions .Check for proper PPE, hand washing, and Droplet Isolation sign in place . Further review revealed the care plan was not revised to include COVID-19 isolation requirements until 3 days after the positive COVID-19 test.
Medical record review revealed Resident #15 was admitted to the facility on [DATE] and readmitted on [DATE] with diagnoses including Myocardial Infarction, Congestive Heart Failure, Gastrointestinal Hemorrhage and Chronic Kidney Disease.
Review of a laboratory result for Resident #15 dated 8/23/2024, revealed the resident had a positive COVID-19 test.
Review of a quarterly MDS assessment dated [DATE], revealed Resident #15 scored a 9 on the BIMS assessment, which indicated moderate cognitive impairment.
Review of the Physician's Orders for Resident #15 dated 8/26/2024, revealed .Isolation Droplet precautions @ all times due to positive covid 19 test .Mask, googles, gloves, gown, face shield .All services provided in resident room .every shift until 9/1/2024 .
Review of Resident #15's comprehensive care plan dated 8/26/2024, revealed .Droplet precautions .Covid-19 .interventions .Check for proper PPE, hand washing, and Droplet isolation sign in place . Further review revealed the care plan was not revised to include COVID-19 isolation requirements until 3 days after the positive COVID-19 test.
Medical record review revealed Resident #615 was admitted to the facility on [DATE] with diagnoses including Cirrhosis of the Liver, Esophageal Varices, Type 2 Diabetes, and Chronic Kidney Disease.
Review of a quarterly MDS assessment dated [DATE], revealed Resident #615 scored a 10 on the BIMS assessment, which indicated moderate cognitive impairment.
Review of the Physician's Orders for Resident #615 dated 8/30/2024, revealed .Isolation Droplet precautions @ all times due to positive covid 19 test .Mask, googles, gloves, gown, face shield .All services provided in resident room .every shift until 9/6/2024 .
Review of Resident #615's comprehensive care plan dated 9/4/2024 revealed .Droplet precautions .covid 19 .Transmission based droplet isolation .Respiratory .until discontinued by the physician .follow facility infection control P&P [policy and procedures] for isolation .Check for proper PPE, hand washing, and Droplet isolation sign in place . Further review revealed the care plan was not revised with interventions to include COVID-19 isolation requirements until 5 days after the positive COVID-19 diagnosis.
Medical record review revealed Resident #507 was admitted to the facility on [DATE], with diagnoses including Wedge Compression Fracture of the First Lumbar Vertebra, Osteoporosis, Dementia, Hypertension and Hypothyroidism.
Review of the admission MDS assessment dated [DATE], revealed Resident #507 scored a 14 on the BIMS assessment which indicated the resident was cognitively intact.
Review of the laboratory results for Resident #507 dated 10/25/2024, revealed a positive COVID-19 test result.
Review of the Physician's Orders for Resident #507 dated 10/25/2024, revealed .Isolation Droplet precautions @ all times due to positive covid 19 test. Mask, googles, gloves, gown, face shield . Further review revealed isolation was to continue through 11/4/2024.
Review of the comprehensive care plan for Resident #507 dated 11/4/2024, revealed a diagnosis of COVID 19 and droplet precautions with interventions including .Check for proper PPE, hand washing, and Droplet isolation sign in place . Further review revealed the care plan was not revised to include COVID-19 isolation requirements until 10 days after the positive COVID-19 test.
Medical record review revealed Resident #619 was admitted to the facility on [DATE] with diagnoses including Sepsis, Obstructive Sleep Apnea, COVID-19, Contact with and Exposure to Other Viral Communicable Disease and Pneumonia.
Review of the hospital's History and Physical for Resident #619 dated 10/24/2024, revealed .Assessment .Principal Problem: COVID . Continued review revealed .Isolation Enhanced Droplet .
Review of the nurse's note for Resident #619 dated 10/25/2024, revealed the resident was admitted to the facility with the diagnosis of COVID 19.
Review of the facility document titled, INTERDISCIPLINARY TEAM CARE CONFERENCE NOTE/CARE PLANNING PROCESS, for Resident #619 dated 10/27/2024, revealed .Resident has no issues so far at this time .Discharge plans are to go back home . Continued review revealed no documentation of the positive COVID 19 test result or isolation precautions.
Review of the Physician's Order for Resident #619 dated 10/28/2024, revealed .Isolation Droplet precautions @ all times due to positive covid 19 test. Mask, googles, gloves, gown, face shield .
Review of the comprehensive care plan for Resident #619 dated 10/29/2024, revealed the resident had a diagnosis of COVID 19. Further review revealed no documentation of COVID-19 isolation precautions.
During an interview on 11/13/2024 at 3:22 PM, the MDS-Care Plan Coordinator confirmed a comprehensive care plan was not revised to include Resident #619 positive COVID-19 test result and isolation precautions.
Medical record review revealed Resident #509 was admitted to the facility on [DATE] with diagnoses including Fracture of Right Humerus, COVID 19, Congestive Heart Failure, Chronic Respiratory Failure and Adult Failure to Thrive.
Review of hospital documentation for Resident #509 dated 10/28/2024, revealed a positive COVID-19 test result.
Review of the Physician's Order Summary Report for Resident #509 dated 10/31/2024, revealed .Isolation Droplet precautions @ all times due to positive covid 19 test. Mask, googles, gloves, gown, face shield . Further review revealed isolation was to continue until 11/7/2024. The care plan was not revised until 3 days after the positive COVID-19 diagnosis.
Review of the admission MDS assessment dated [DATE], revealed Resident #509 scored a 13 on the BIMS assessment, which indicated the resident was cognitively intact.
Review of the comprehensive care plan for Resident #509 revised date 11/4/2024, revealed the resident had a positive COVID-19 test result and was in droplet isolation precautions with interventions including checking for proper PPE, hand washing, and droplet isolation sign in place.
During an interview on 11/12/2024 at 6:39 PM, the Administrator, Director of Nursing (DON), and [NAME] President (VP) of Clinical services confirmed CDC guidance was not followed related to COVID-19 PPE usage by employees and COVID-19 isolation requirements.
Medical record review revealed Resident #43 was admitted to the facility on [DATE] with diagnoses including Yeast Infection, Obesity, Cancer of Rectum, Anxiety, Insomnia, Pain, Muscle Weakness and Need for Assistance.
Review of Resident #43's comprehensive care plan related to falls initiated 7/1/2024, revealed the care plan identified the resident as a falls risk, and revealed the care plan had not been revised since the care plan was initiated.
Review of a quarterly MDS assessment dated [DATE], revealed Resident #43 scored a 15 on the BIMS assessment, which indicated the resident was cognitively intact.
Review of the facility's incident investigation document dated 10/30/2024, revealed Resident #43 had an unobserved fall and documented .ask for assistance when transferring . for the new fall intervention implemented.
During an interview and observation on 11/3/2024 at 11:21 AM, Resident #43 stated she had a fall the last week of October 2024, and stated the facility did not educate her to ask for staff assistance after the fall and stated .all they did was put this sign on my wall . and indicated a 8 by 11-inch sign posted on the wall which revealed .call before your fall .
During an observation on 11/5/2024 at 10:20 AM, Resident #43 continued to have the same sign posted on her wall which read .call before your fall .
During an interview and record review on 11/5/2024 at 10:40 AM, Certified Nursing Assistant (CNA) T stated Resident #43 was not a falls risk and had never fallen. CNA T stated the resident's [NAME] notified CNAs if the resident had ever fallen and of the required fall interventions for the residents. Review of Resident #43's [NAME] with CNA T revealed the resident was not identified as a falls risk and did not have interventions listed for falls.
During an interview on 11/5/24 at 10:45 AM, CNA U stated Resident #43 had a fall recently but was not a falls risk. CNA U stated the intervention was to put non-skid socks on the resident and stated Resident #43 was not a falls risk if she wore non-skid socks. CNA U confirmed Resident #43 did not have falls risk identified or fall interventions on the [NAME] to alert CNAs the resident was at risk for falls.
During an interview on 11/5/2024 at 10:55 AM, Licensed Practical Nurse (LPN) A stated Resident #43 had a fall on 10/30/2024, and stated she told the resident to ask for assistance when transferring from the bed and stated later that day she was instructed to place the call before you fall sign in the resident's room. LPN A stated she did not know what was on Resident #43's care plan and [NAME], stated she did not know how to access resident care plans and stated .I don't think falls is something that would be on a care plan or [NAME] .
During a record review and interview on 11/6/2024 at 3:27 PM, the MDS-Care Plan Coordinator reviewed Resident #43's [NAME] and care plan. The MDS-Care Plan Coordinator confirmed the [NAME] did not identify Resident #43 as a falls risk and did not include fall interventions. The MDS-Care Plan Coordinator also confirmed Resident #43's falls care plan was not revised with any intervention to include non-skid footwear, signage in the resident's room, or resident education.
Medical record review revealed Resident #95 was admitted to the facility on [DATE] with diagnoses including Vascular Dementia, Mood Disorder, Delusional Disorders, Adult Failure to Thrive, Type 2 Diabetes, Malignant Neoplasm of Upper Lobe (Left Bronchus or Lung), Hydronephrosis with Renal and Ureteral Calculous Obstruction, Hypertension, Depression and Anxiety.
Review of Resident #95's comprehensive care plan dated 7/30/2024, revealed .FULL CODE status [cardiopulmonary resuscitation] .Interventions .If code status changes update medical record .
Review of the POST (Physician Orders for Scope of Treatment) document signed by Resident #95's family on 7/30/2024, revealed .Do Not Attempt Resuscitation (DNR) .Limited Additional Interventions .Long-Term artificial Nutrition per tube .
Review of a quarterly MDS assessment dated [DATE], revealed Resident #95 scored a 12 on the BIMS assessment, indicating moderate cognitive impairment.
During an interview on 11/6/2024 at 10:15 AM, the MDS-Care Plan Coordinator stated Resident #95's code status changed from a full code to a DNR and stated Resident #95's advance directive care plan was incorrect. The MDS Care Plan Coordinator confirmed the facility failed to revise Resident #95's comprehensive care plan.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, medical record review, observations, and interviews, the facility failed to ensure medications ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, medical record review, observations, and interviews, the facility failed to ensure medications were properly stored in 2 medication carts (A-Wing and C-Wing) of 4 medication carts reviewed for medication storage.
The findings include:
Review of the facility's policy titled, Medication Storage Guidelines, undated, revealed .the facility will ensure all medications will be stored in the medication rooms/ carts .to ensure proper sanitization, temperature .moisture control .all medications requiring refrigeration are stored in refrigerators located in .each medication room .routinely inspected .for .missing labels .these medication are destroyed .
Review of the medical record revealed Resident #103 was admitted to the facility on [DATE] with diagnoses including Lupus, Alzheimer's Disease, and Atrial Fibrillation.
Review of the admission Minimum Data Set (MDS) assessment dated [DATE], revealed Resident #103 scored a 0 on the Brief Interview for Mental Status (BIMS) which indicated the resident had severe cognitive impairment.
During an observation and interview on 11/3/2024 at 5:10 PM, on the A-Wing medication cart, revealed an unopened box of Lorazepam [anti-anxiety medication] 30 milliliter (ml) liquid for Resident #103 was stored in the medication cart. The medication label indicated the medication required refrigeration storage. Licensed Practical Nurse (LPN)/ Risk Manager M confirmed the medication had been stored on the medication cart since delivery on 10/31/2024, was not opened, and was not stored in the refrigerator.
During an interview on 11/4/2024 at 4:00 PM, the Pharmacist stated liquid Lorazepam would gradually lose the effectiveness of the medication if not stored in refrigerator and if the medication was stored on the medication cart for 3 days at room temperature, the medication should be discarded.
During an interview on 11/4/2024 at 5:41 PM, the Administrator and Director of Nursing (DON) stated it was the facility's expectation for the Lorazepam for Resident #103 to be stored per pharmacy/manufacturer guidelines. The DON confirmed Resident #556's liquid Lorazepam was not stored properly and should be discarded and replaced.
During a medication administration observation on 11/4/2024 at 7:30 AM, on the C-Wing medication cart, revealed the following medication storage:
(one) 16-ounce (oz) bottle (house stock) of Lactulose (medication used to treat constipation) 10 gm/mL (gram/milliliter) 3/4 full (opened and undated)
(one) 17.9 oz bottle (house stock) of Polyethylene Glycol (medication used to treat constipation) 1/4 full (opened and undated)
During an interview on 11/4/2024 at 7:45 AM, LPN A confirmed the medications observed in the medication cart had not been stored properly.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, observations and interviews, the facility failed to maintain a clean, comfortable, and home lik...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, observations and interviews, the facility failed to maintain a clean, comfortable, and home like environment for 5 hallways of 5 hallways observed for comfortable and home like environments.
The findings include:
Review of the facility policy titled, Resident Environmental Quality, undated, revealed The facility will be .maintained to provide a safe, functional .and comfortable environment for residents .Resident rooms must be designed and equipped for adequate nursing care, comfort, and privacy .Preventive maintenance .should be followed .
During an observation on 11/3/2024 at 11:40 AM, revealed the 100-hallway carpet had multiple large stains in various places from unidentified substances, which included various shades of brown stains and bright red stains.
During an observation on 11/3/2024 at 11:42 AM, revealed the 200-hallway carpet had multiple large stains in various places from unidentified substances, which included various shades of brown stains and bright red stains.
During an observation on 11/3/2024 at 11:45 AM, revealed room [ROOM NUMBER] had a bed with a broken foot board, which included large missing pieces of the foot board and the trim missing from the footboard. Further observation of room [ROOM NUMBER] revealed a yellow 2-sided adhesive ribbon hanging from the ceiling with multiple unidentified small black bugs with wings attached to both sides of the adhesive ribbon.
During an observation on 11/3/2024 at 11:47 AM, revealed the 300-hallway carpet had multiple large stains in various places from unidentified substances, which included various shades of brown stains and bright red stains.
During an observation on 11/3/2024 at 11:50 AM, revealed room [ROOM NUMBER] had multiple walls with multiple large stains in various shades of brown and black from unidentified substances. The multiple walls had several large areas of paint missing from the walls with exposed drywall. Further observation of room [ROOM NUMBER] revealed multiple stains in various shades of brown on the window curtains and a large area of missing wallpaper.
During an observation on 11/3/2024 at 11:55 AM, revealed room [ROOM NUMBER] had a sink in the room with running water. The sink faucet handles were turned backwards (in the shut off position) which indicated the sink's water should not have been flowing from faucet.
During an observation on 11/3/2024 at 11:57 AM, revealed the 300-hallway carpet had multiple large stains in various places from unidentified substances, which included various shades of brown stains and bright red stains.
During an observation on 11/3/2024 at 12:00 PM, revealed room [ROOM NUMBER] had multiple walls with multiple large stains in various shades of brown and black from unidentified substances. The multiple walls had several large areas of paint missing from the walls with exposed drywall. Further observation of room [ROOM NUMBER] revealed the trim on the wall was missing in multiple places and large areas of paint was peeling from the walls, which exposed drywall.
During an interview on 11/3/2024 at 2:03 PM, the Administrator stated the facility started taking quotes to repair rooms and change the carpet in September 2022, and stated the facility did not start repairing rooms until October 2024. The Administrator stated she was aware there was multiple rooms on every unit in need of repair.
During observations and interview on 11/6/2024 at 3:40 PM, the [NAME] President (VP) of Life Safety and Environmental Compliance observed the carpet with multiple hallway carpet stains and stated the bright red stain was from spilled red-colored punch beverages and stated he could not identify the source of the brown stains. The VP of Life Safety and Environmental Compliance observed Rooms 211, 307, 312, and 415 and confirmed the resident rooms and the respective hallways were not serviced to maintain a clean, comfortable, and home like environment.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on facility policy review, observations, and interviews, the facility failed to discard expired food in 1 of 1 kitches which had the potential to affect 99 of 99 residents.
The findings include:...
Read full inspector narrative →
Based on facility policy review, observations, and interviews, the facility failed to discard expired food in 1 of 1 kitches which had the potential to affect 99 of 99 residents.
The findings include:
Review of the facility's policy titled, Food Safety Guidelines, undated, revealed .The food shall be clearly marked to indicate the date or day by which the food shall be consumed or discarded .
During an observation of the food preparation area on 11/3/2024 at 9:45 AM, with the Certified Dietary Manager (CDM), revealed the following:
1. 80 ounce opened bag of grits contained in sealed storage bag with opened date: 9/18/2024 and discard date: 10/18/2024 and available for use.
2. An unopened 4-pound roll of deli bologna with received date as: 8/16/2024 and use by date: 9/3/2024 and available for use.
3. 12 ounce container of ground black pepper that was opened to air and available for use.
4. 12 ounce container of ground allspice sealed with open date of 6/1/2024 and discard date of 8/1/2024 and available for use.
During an observation and interview on 11/3/2024 at 10:19 AM, the CDM confirmed that the bologna, grits, and allspice were expired, had not been discarded, and was available for use.
During an observation and interview on 11/3/2024 at 10:24 AM, the CDM confirmed that the ground black pepper was open, not properly sealed to prevent contamination, and available for use.