CRITICAL
(K)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0657
(Tag F0657)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, medical record review, observation, and interview, the facility failed to revise the care plan for smoki...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, medical record review, observation, and interview, the facility failed to revise the care plan for smoking safely with effective interventions to prevent accidents for 5 of 5 (Resident #22, #102, #30, #88, and #180) sampled residents reviewed for smoking which placed these residents in Immediate Jeopardy.
Immediate Jeopardy (IJ) is a situation in which the provider's noncompliance with one or more requirements of participation has caused or is likely to cause serious injury, harm, impairment, or death to a resident.
The Interim Administrator, Assistant Administrator, Director of Nursing (DON), Assistant Director of Nursing (ADON), Infection Preventionist, Quality and Infection Preventionist Director, and Minimum Data Set (MDS) Coordinator #2, were notified of the IJ on 7/12/19 at 9:32 PM, in the Conference Room.
The facility was cited at scope and severity of Immediate Jeopardy for F657-K.
The extended survey was conducted on 7/12/19 through 7/15/19.
The Immediate Jeopardy was effective 9/8/18 through 7/15/19 and the IJ was removed on 7/15/19.
An acceptable Allegation of Compliance (AOC), which removed the immediacy of the jeopardy, was received on 7/14/19 at 5:30 PM, and the corrective actions were validated onsite by the surveyors on 7/14/19 and 7/15/19 through review of assessments, auditing tools, in-service training records, policies, observations, and staff interviews.
The noncompliance continues at F657-E for monitoring of effectiveness of the corrective actions.
The findings include:
1. The facility's Care Plan policy with a revision date of 10/23/18 documented, .PURPOSE .To provide guidelines for identifying a resident's care needs .To provide guidelines for structuring an approach through interventions to address their care needs .An individualized care plan will be established for each resident to provide effective and person centered care .New Care Plans will be initiated as new needs are identified in order to meet the individualized needs of each resident .The plan should be kept current and flexible to meet the resident's changing problems or needs .
2. The facility's Smoking Policy dated 12/94 and revised 4/11/19 documented, .Residents who were admitted prior to 11/15/12 will be allowed to continue smoking until their discharge .All resident smoking materials are to be kept secured by the facility .Visitors need to check with charge nurse/nurse before giving smoking materials to ANY resident of Care Centers .
3. Medical record review revealed Resident #22 was admitted to the facility on [DATE] and readmitted on [DATE] with diagnoses of Diabetes Mellitus, Cerebral Infarction, Heart Failure, Major Depression, Morbid Obesity, and Anxiety.
Medical record review of Resident #22's Care Plan for smoking was dated 1/29/18.
The Care Plan interventions for smoking had not been revised since the care plan was initiated on 1/29/18.
Medical record review of Resident #22's care plan for falls dated 1/29/18 with revisions documented the following:
.2/15/19 .Interventions .Resident was witnessed going outside through breakroom door at skilled care and tipping over to the right as his wheels went off side walk pavement .Fence beside side walk was pushed over during the fall. Skin tears to right arm and elbow. Resident counseled to not use this door in the future. Sign posted to keep breakroom door closed and door to outside locked at all times .
Medical record review of a MDS assessment dated [DATE] revealed Resident #22 had a Brief Interview for Mental Status (BIMS) score of 4 which indicated Resident #22 was severely cognitively impaired and was non-compliant.
Observations in the Hall 6 Smoking Porch on 7/8/19 at 12:49 PM revealed Resident #22 was smoking without staff supervision.
3. Medical record review revealed Resident #102 was admitted to the facility on [DATE] with diagnoses of Hemiplegia (paralysis on one side of her body), Dysphagia, Anxiety Disorder, Alzheimer's Disease, Expressive Language Disorder, and Benign Neoplasm of the Brain.
Medical record review of the MDS assessment for Resident #102 dated 3/13/19 documented a BIMS score of 12 which indicated Resident #102 was moderately impaired cognitively.
A Web Event Summary Report dated 3/23/19 documented, .At 7:30 pm tech [technician] noted cigarette burn to abdomen, ashes in navel, burn hole in pants. Area not draining or wet. Dry with slight redness around it .
Medical record review of the Order Audit Report for Resident #102 dated 3/25/19 documented, .Resident to be supervised at all times while smoking (Do Not leave alone while smoking) .
The care plan intervention was revised on 4/12/19 for Resident #102 to smoke unsupervised. The care plan for smoking for Resident #102 was not revised until 4/12/19.
Revision of the care plan on 6/27/19 documented, .RESIDENT MUST BE SUPERVISED/ACCOMPANIED BY STAFF WHILE SMOKING .RESIDENT IS NOT TO BE LEFT ALONE WHILE SMOKING .
Observations in the Hall 6 Smoking Porch on 7/8/19 at 12:49 PM, revealed Resident #102 smoking without staff supervision.
Interview with MDS Coordinator #1 on 7/10/19 at 10:30 AM, in the Conference Room, MDS Coordinator #1 was asked if the care plan was updated. MDS Coordinator #1 stated, I need to look at his [physician] progress note. I will get with him for a clarification order.
MDS Coordinator #1 failed to answer whether the care plan had been revised.
Interview with MDS Coordinator #2 on 7/12/19 at 10:50 AM, in the Conference Room, MDS Cordiantor #2 was asked why Resident #102 had the intervention to be supervised while smoking on 6/27/19. MDS Coordinator #2 stated, .I am not sure .we have been talking about it .
Interview with MDS Coordinator #1 on 7/12/19 beginning at 11:04 AM, in the Conference Room, MDS Coordinator #1 was asked about the care plan not being revised for Resident #102 after a burn was found on Resident #102's abdomen. MDS Coordinator #1 stated, .we did not have a care plan meeting, we did not have time for a meeting that week .
4. Medical record review revealed Resident #30 was admitted to the facility on [DATE] and readmitted [DATE] with diagnoses of Hemiplegia and Hemiparesis (paralysis on one side of his body) Following Cerebral Infarction Affecting Left Non-Dominant Side, Asthma, Noncompliance with Medication Regimen, Hypertension, Atherosclerotic Heart Disease, Dysphagia, Hyperlipidemia, Tobacco Use, and Alcohol Dependence.
Medical record review of a Progress Note dated 3/30/19 documented, .Behavior is rebellious over the last week. Has been sneaking outside to smoke with another patient despite being told that someone either staff or family must accompany him .
Resident #30 did not have a care plan for smoking when he was admitted on [DATE]. Resident #30's care plan was not revised to reflect elopement risk related to history of attempts to leave the facility unattended and impaired safety awareness status until 4/4/19.
Observations in the Hall 6 Smoking Porch on 7/8/19 at 12:49 PM revealed Resident #30 smoking without staff supervision.
5. Medical record review revealed Resident #88 was admitted to the facility on [DATE] and readmitted on [DATE] with diagnoses of Congestive Heart Failure, Hemiplegia and Hemiparesis (paralysis on one side of his body), Cerebral Infarction Affecting Dominant Right Side, Diabetes Mellitus, Use of Anti Coagulants, Chronic Kidney Disease and Asthma.
Medical record review of a Care Plan dated 3/17/16 for Resident #88 documented, .6/24/19 .Resident is grandfathered in [allowed to smoke] but must smoke in designated area smoke at designated times .
Resident #88 was transferred from (Named facility) sister building to present building on 9/19/18.
Medical record review of an annual MDS dated [DATE] documented Resident #88 had a BIMS score of 12 which indicated moderate cognitive impairment and had functional impairment to both arm and leg on one side of his body.
The smoking care plan for Resident #88 was not revised until 6/24/19. According to the facility's policy there was no designated times for supervised smoking and the smoking materials were to be secured by the facility.
6. Medical record review revealed Resident #180 was admitted to the facility on [DATE] with diagnoses of Hemiparesis (paralysis on one side of his body), Pneumonia, Depression, Insomnia, Anxiety, Hepatitis C, Hyperlipidemia, Alcohol Dependence, Hypertension, Coronary Artery Disease, Cerebral Infarction, Nontraumatic Subarachnoid Hemorrhage, Dysphagia, Chronic Obstructive Pulmonary Disease, and Rhabdomyolysis.
Medical record review of an admission MDS dated [DATE] documented Resident #180 had a BIMS score of 12 which indicated moderate cognitive impairment and he had impairment on one side of his body.
Medical record review of a Care Plan for Resident #180 dated 12/20/18 revealed Resident #180's care plan did not address smoking and noncompliance by the resident.
Observations in the Hall 6 Smoking Porch on 7/8/19 at 12:49 PM revealed Resident #180 smoking without staff supervision.
Interview with MDS Coordinator #1 on 7/10/19 at 10:30 AM, in the Conference Room, MDS Coordinator #1 confirmed the care plans were not revised to reflect smoking safely with effective interventions to prevent accidents.
Refer to F689.
The surveyors verified the AOC by:
The Interdisciplinary Team, consisting of the DON, ADON, Infection Preventionist, Activity Director, MDS Coordinators, Dietician, and Social Services will meet daily after morning meeting, to assure review of any updates and revisions to the resident care plans are occurring, appropriately and accurately and that those changes are being properly communicated to the licensed nurses, direct care and dietary staff members. An updated communication system has been developed whereby changes entered into the residents' care plan are updated on the electronic documentation system. Those changes will be reflected on the Nurse Aide [NAME] and any significant issues will be discussed face to face during the daily nursing staff huddles and during shift report. The care plans of residents who smoke have been updated to reflect the current Smoking Policy. These care plans will be updated at least quarterly or as necessary by the MDS Coordinators. Being that the facility is going Smoke Free on 8/12/19 newly admitted residents, who smoke, will be educated regarding the Smoke Free policy and will be reflected on their care plans. The surveyors interviewed the ADON and were provided information to review when the care plans will be updated. Audits will be completed to ensure updates are maintained.
Noncompliance continues at a scope and severity level of E for monitoring of the effectiveness of the corrective actions.
The facility is required to submit a Plan of Correction.
CRITICAL
(K)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, medical record review, observation, and interview, the facility failed to ensure a safe environment that...
Read full inspector narrative →
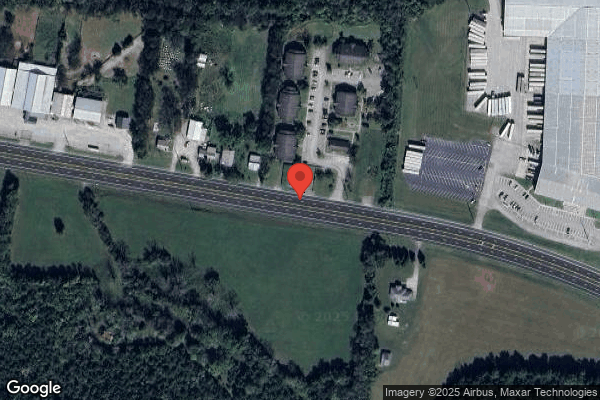
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, medical record review, observation, and interview, the facility failed to ensure a safe environment that provided supervision to eliminate the risk of elopement and accidents for 9 of 9 (Resident #22, #102, #18, #12, #13, #38, #2, #70, and #377) wandering and smoking residents reviewed and failed to ensure residents were supervised while smoking to prevent accident hazards for 5 of 5 (Resident #22, #30, #88, #102, and #180) smoking residents. The 5 of 5 (Resident #22, #30, #88, #102, and #180) smoking residents also had knowledge and used the exit door key pad codes provided to them by the staff, allowing the residents to exit the building independently without staff supervision, were allowed to smoke unsupervised, and were allowed to keep smoking materials (cigarettes and lighters) on their person. The 7 of 7 (Resident #2, #12, #13, #18, #38, #70, and #377) cognitively impaired, vulnerable residents with wanderguards (ankle band tracking system that automatically locked the doors and alarmed) were at elopement risk, when the facility had nonfunctioning sensor alarms or no sensor alarms on 5 of 8 (Hall 1 door, Hall 2 Dining Room door, Hall 3 Dining Room door, Hall 4 [NAME] door, and Hall 6 door) exit doors. The facility was 156 feet from a heavily traveled 4 lane state highway.
The failure of the facility to provide supervision and to prevent accidents resulted in HARM when Resident #22 and #102 had falls with injury when these residents were allowed to use the exit code to the doors to leave a safe area to an unsafe area.
The failure of the facility to ensure the exit doors had functioning wanderguard sensor alarms and the failure to check and repair the exit doors placed Resident #12, #13, and #18 in Immediate Jeopardy when these residents with wanderguards were able to exit the building, and this had the potential to affect the other wandering residents (Resident #2, #38, #70, and #377). The failure of the facility to provide supervision during smoking had the potential to cause serious harm or injury, and placed Resident #22, #30, #88, #102, and #180 in Immediate Jeopardy.
Immediate Jeopardy (IJ) is a situation in which the provider's noncompliance with one or more requirements of participation has caused or is likely to cause serious injury, harm, impairment, or death to a resident.
An extended survey was conducted on 7/12/19 through 7/15/19.
The Interim Administrator, the Assistant Administrator, the Director of Nursing (DON), the Assistant Director of Nursing (ADON), the Quality and Infection Preventionist Director, the Infection Preventionist, and Minimum Data Set (MDS) Coordinator #2 were notified of the Immediate Jeopardy on 7/12/19 at 9:32 PM, in the Conference Room.
The facility was cited IJ at F689 K which is Substandard Quality of Care.
An acceptable Allegation of Compliance (AOC), which removed the immediacy of the jeopardy, was received on 7/14/19 at 5:30 PM, and the corrective actions were validated onsite by the surveyors on 7/14/19 and 7/15/19 through review of assessments, auditing tools, in-service training records, policies, observations, and staff interviews.
The Immediate Jeopardy was effective from 9/8/18 through 7/15/19 and the IJ was removed on 7/15/19.
The noncompliance continues at F689-E for monitoring of effectiveness of the corrective actions.
The findings include:
1. The facility's Smoking Policy with a revision date of 4/11/19 documented, .OBJECTIVE .To restrict smoking to a minimum and reduce risks to residents .who smoke, including adverse effects .the risk of fire .All resident smoking materials are to be kept secured by the facility .Visitors need to check with charge nurse/nurse before giving smoking materials to ANY resident of Care Centers .
The facility's Oxygen Administration - Hazards and Pitfalls policy with a revision date of 9/17 documented, .The most frequent cause of fire when oxygen is being administered is the lighting of a cigarette. This hazard is greatly increased with the administration of oxygen. Smoking is strictly against the rules and regulations in rooms where oxygen is being administered .
Review of the facility's Elopement Risk/ Wanderguard policy with a revision date of 4/11/19 documented, .Any resident with an altered mental status who has demonstrated behavior that puts them at risk for wandering/elopement will be considered an elopement risk .PROCEDURE .Document behavior in Nursing Notes. Be descriptive as to behavior resident is demonstrating .Resident will wear wanderguard bracelet .
2. Medical record review revealed Resident #22 was admitted to the facility on [DATE] and readmitted [DATE] with diagnoses of Diabetes Mellitus, Cerebral Infarction, Heart Failure, Major Depression, and Anxiety.
Medical record review of a MORSE FALL SCALE assessment dated [DATE] documented, .Moderate Risk for Falling .
Medical record review of the Care Plan for Resident #22 revised on 7/8/19 documented, .The resident is (Moderate) risk for falls .Interventions .2/15/19 Resident was witnessed [staff witnessed from inside the building] going outside through [employee] breakroom door at skilled care and tipping over to the right as his wheels went off sidewalk pavement. Fence beside side walk was pushed over during the fall. Skin tears to right arm and elbow. Resident counseled to not use this door in the future. Sign posted to keep breakroom door closed and door to outside locked at all times .
Medical record review of a Nurses Progress Incident Note dated 2/15/19 at 12:52 PM documented, .at 0645 [6:45 AM] this am pt [patient] went outside to smoke. he [He] went out the staff lounge door. he [He] was reaching for the door knob to come back into building when his w/c [wheelchair] tipped over the edge of the sidewalk. he [He] and the w/c was found lying on the white fence that was knocked over. he [He] was lying on his rt [right] side. his [His] rt arm has 3 large skin tears and some bruising .
Medical record review of a Progress Note Skin/Wound Note dated 2/15/19 at 1:45 PM documented, .3 skin tears to right arm noted .Re-approximated 2 skin tears with steri strips [wound closure device used instead of stitches] .
Review of a Web Event Summary Report dated 2/15/19 documented, .Resident [#22] was exiting the building in wheelchair through skilled breakroom when his wheelchair wheels on the right side fell off the pavement causing him to turn over to the right side against a fence that fell over with him .Assisted up x [times] 4 staff members. Skin tears to right arm .Resident [#22] counseled to not attempt to go outside unassisted. Doors to breakroom are to be kept closed at all times (punch lock for staff only) and doors to outside are to be locked at all times. resident [Resident] and staff voice understanding .
Medical record review of the admission MDS dated [DATE] revealed Resident #22 had a Brief Interview for Mental Status (BIMS) score of 4, which indicated severe cognitive impairment, and required limited to extensive staff assistance with activities of daily living (ADLs).
Medical record review of a MORSE FALL SCALE assessment for Resident #22 dated 7/8/19 documented, .High Risk for Falling .
Interview with Licensed Practical Nurse (LPN) #4 on 7/12/19 at 11:04 AM, in the Conference Room, LPN #4 stated, .I was in the skilled hall and I glanced out window I saw his [Resident #22] arm go up and a body go up. He was outside .said he was reaching to let himself back in .he got there alone .I would call that a witnessed fall .
Observations at the Hall 6 Smoking Porch Exit door on 7/8/19 at 12:51 PM, revealed Resident #22 propelled himself to the door and entered a code in the door lock key pad, opened the door with the metal handicap push button, and entered the Smoking Porch.
Interview with the ADON on 7/11/19 at 2:35 PM, in the Conference Room, the ADON was asked if Resident #22 had a fall. The ADON confirmed he went into the break room and out the side door, and he turned over his wheelchair. The ADON stated, I'm not sure how he got into the break room door. It .has a key pad on it. After getting in the break room, the door to the outside is unlocked.
Observations in the courtyard on 7/11/19 at 2:44 PM, revealed the back door of the breakroom lead to the courtyard. The side walk had a drop off. The courtyard was not a secured area. There was not a secured area outside the building.
Resident #22 entered an unsafe area from a safe area, unsupervised, and sustained 3 skin tears requiring steri-strips, which resulted in HARM to Resident #22.
3. Medical record review revealed Resident #102 was admitted to the facility on [DATE] with diagnoses of Hemiplegia (paralysis), Dysphagia, Anxiety Disorder, Alzheimer's Disease, Expressive Language Disorder, and Benign Neoplasm of the Brain.
Medical record review of the Care Plan for Resident #102 revised on 6/27/19 documented, .The resident has had an actual fall .Interventions .1/10/19 At 15:30 [3:30 PM] was outside smoking [on Smoking Porch], bent forward to pick up cigarette from ground and fell out of wc [wheelchair] and hit her head .has small hematoma to forehead between eys [eyes], small abrasion to bridge of nose and 5cm [centimeters] x 1.5cm skin tear to shin .Assigned staff supervision with resident when smoking .
Review of a Web Event Summary Report dated 1/11/19 documented, .Resident [#102] was outside smoking, she bent forward to pick up cigarette off ground and fell out of wc, hit her head causing a small hematoma to forehead between eyes, and abrasion to bridge of nose and skin tear 5 cm X 1.5 to right shin .steri-strips [wound closure strips] applied The care plan was updated 1/10/19 for Resident #102 to be supervised with smoking.
Medical record review of the annual MDS dated [DATE] revealed Resident #102 had a BIMS score of 12, which indicated moderate cognitive impairment.
Observations in the Hall 6 Smoking Porch on 7/8/19 at 12:51 PM, revealed Resident #102 propelled herself out the door to the Smoking Porch (an unsecured area).
Interview with the DON and MDS Coordinator #1 on 7/10/19 at 9:41 AM, in the Conference Room, MDS Coordinator #1 was asked if residents knew the code to the door. MDS Coordinator #1 and the DON confirmed residents did know the code to the Smoking Porch Exit door. The DON and MDS Coordinator #1 were asked if the residents could go freely out to smoke at any time. The DON and MDS Coordinator #1 stated, Yes.
Interview with the Interim Administrator on 7/12/19 at 11:35 AM, in the Conference Room, the Interim Administrator was asked if Resident #102 should have been outside alone. The Interim Administrator stated, We [Administrative staff] don't think so, no .
Resident #102 entered an unsafe area from a safe area, unsupervised, and sustained a skin tear requiring steri-strips and a hematoma, which resulted in HARM to Resident #102.
4. Medical record review revealed Resident #18 was admitted to the facility on [DATE] and readmitted [DATE] with diagnoses of Chronic Kidney Disease Stage 4, Anxiety, Anemia, Hypothyroidism, Depression, Heart Failure, Abdominal Aortic Aneurysm, Chronic Obstructive Pulmonary Disease, Osteoarthritis, Enlarged Prostate, Neurogenic Bladder, and Urinary Tract Infection.
Medical record review of a significant change MDS dated [DATE] and the quarterly MDS dated [DATE] revealed a BIMS score of 8, which indicated moderate cognitive impairment.
The Web Event Summary dated 9/14/18 documented, .8:30am Resident went out side door of Hall 4, has wanderguard on. Dtr [daughter] .and FNP [Family Nurse Practitioner] notified .
Medical record review of the Care Plan for Resident #18 revised 7/8/19 documented, .The resident is an elopement risk/wanderer r/t [related to] Disorientation to place, Impaired safety awareness .Interventions .9/14/18 Resident was able to get outside door. Tech [Certified Nursing Technician] nearby and retrieved resident without incident. Wanderguard in place. Maintenance contacted to check on door security .Distract resident from wandering by offering pleasant diversions, structured activities, food, conversation, television, book. Resident prefers .
Medical record review of the WANDERING RISK SCALE assessments dated 1/14/19 and 4/14/19 revealed a score of 10 which indicated At Risk to Wander.
Review of a Web Event Summary Report for Resident #18 dated 1/31/19 documented, .[on 1/30/19] Resident was sitting outside door on south hall, CNA [Certified Nursing Assistant] student thought that he was waiting to go smoke and let him outside, resident was found up against fence with wc on top of him, he did have small cut to right 4th finger .Intervention .Neurochecks initiated .student tech educated on protocol on letting residents outside and also which residents are allowed to smoke unattended. Discussed smoking policy and protocal [protocol] for letting residents outside in huddle, also put in task a reminder that resident is not allowed outside unattended .
Observations in Resident #18's room on 7/8/19 at 12:15 PM revealed Resident #18 seated in his wheelchair and appeared confused.
Interview with the ADON on 7/11/19 at 7:15 PM, in the Conference Room, the ADON confirmed Resident #18 exited the building on 9/14/18 and maintenance was contacted and stated, .not sure why maintenance was notified .
Interview with LPN #3 on 7/14/19 at 6:26 PM, in the Fine Dining Room, LPN #3 was asked if there had been any problems with the wanderguards functioning correctly. LPN #3 stated, Some of the wanderguards were not working properly with all the doors .I have seen [Resident #18] .he is very persistent .sometimes it doesn't alarm .
5. Medical record review revealed Resident #12 was admitted to the facility on [DATE] and readmitted [DATE] with diagnoses of Alzheimer's Disease, Depression, Diabetes, Seizures, Congestive Heart Failure, Generalized Muscle Weakness, Chronic Kidney Disease Stage 4, and Hypertension.
Medical record review of a Web Event Summary Report dated 9/8/18 documented, .2:30 pm Resident and roommate [Resident #13] was outside bldg [building] underneath awning at end of hall 4 .Work order to maintenance to have doors checked . (The Hall 4 [NAME] door had a wanderguard sensor that was not functioning appropriately).
Medical record review of a Progress Note for Resident #12 dated 9/12/18 documented, .Resident and roommate went to front door on skill hall and attempted to elope. Resident also came to back door by nurse's station and attempted to elope .
Review of the physician orders and the MARS revealed Resident #12 had a wanderguard since 9/11/18.
Medical record review of the annual MDS dated [DATE] revealed a BIMS score of 7, which indicated severe cognitive impairment and used wander/elopement alarms.
Medical record review of the Care Plan for Resident #12 revised 7/8/19 documented, .The resident is an elopement risk r/t Impaired safety awareness .Interventions .9/8/18 Resident found standing outside .just getting some fresh air .Distract resident from wandering by offering pleasant diversions, structured activities, food, conversation, television, book. Resident prefers Date Initiated: 09/11/2018 .WANDER ALERT: Wander guard in place Date Initiated: 09/11/2018 .
Medical record review of WANDERING RISK SCALE assessments dated 1/3/19, 4/3/19, and 7/3/19 documented, .High Risk to Wander .
Observations in Hall 4 on 7/8/19 at 12:20 PM, revealed Resident #12 ambulating on the hall with a rolling walker.
Interview with the ADON on 7/14/19 at 4:32 PM, in the Conference Room, the ADON was asked about Resident #12 exiting the building. The ADON stated, .There was a family member or someone else's family member let them out under the awning on Hall 4 .
6. Medical record review revealed Resident #13 was admitted to the facility on [DATE] and readmitted [DATE] with diagnoses of Alzheimer's Disease, Other Abnormalities of Gait and Mobility, Generalized Muscle Weakness, Repeated Falls, Chronic Kidney Disease Stage 3, Congestive Heart Failure, Anxiety, Hypertension, Osteoporosis, Depression, and Atrial Fibrillation.
Review of the physician orders and the MARS revealed Resident #13 had a wanderguard since 4/24/18.
Medical record review of a Web Event Summary Report for Resident #13 dated 9/8/18 documented, .2:30 pm Resident was found with roommate [Resident #12] outside of bldg. underneath awning at end of Hall 4 .has on Wanderguard .Work order to have door checked .9-10-18 .
Review of Maintenance Work Orders documented the following:
a. 9/10/18 .Door going outside not working properly .hall 5 .
b. 9/10/18 .Hall 4 exterior door (where linen is brought in) and the skilled dining room exit door is [are] not locking appropriately (they are suppose to lock automatically) and the wander guard is not working properly on these doors .This needs to be looked at asap [as soon as possible] .Hall 4 exterior door (where linen is brought in) .
c. 9/14/18 .Hall 4 doors are not locking down with wander guard .resident [Resident #18] with wander guards opened doors today .Hall 4 [Hall 4 [NAME] door]outside doors .
There was no documentation the doors were repaired or checked.
Medical record review of Progress Notes documented:
a. 9/12/18 .Resident and roommate [Resident #12] went to front door on skill hall and attempted to elope. Resident also came to back door by nurse's station and attempted to elope .
b. 1/10/19 .has a wander guard in place d/t confusion and risk of elopement .
c. 2/12/19 .Roaming halls wanting to leave with pocketbook on shoulder .
Medical record review of the quarterly MDS dated [DATE] revealed a BIMS score of 3, which indicated severe cognitive impairment, and daily use of a wander/elopement alarm (wanderguard).
Medical record review of the WANDERING RISK SCALE assessments for Resident #13 dated 1/4/19, 4/3/19, and 7/8/19 documented, .High Risk to Wander .
Medical record review of the Care Plan for Resident #13 revised 7/8/19 documented, .The resident has impaired cognitive function/dementia or impaired thought processes r/t Alzheimer's, Dementia . Interventions . supervise as needed. Date Initiated: 10/12/2017 .The resident is an elopement risk r/t Impaired safety awareness . Interventions .4/23/18 . Wanderguard anklet applied .9/8/18 Resident found standing just outside door .was getting some fresh air. Resident redirected back into facility without issue. Date Initiated: 09/11/2018 .
Observations on Hall 4 on 7/14/19 at 1:57 PM, revealed Resident #13 ambulating in the hall using a rolling walker. She had a wanderguard to her right ankle.
Interview with the Facilities Director on 7/12/19 at 12:03 PM, in the Conference Room, the Facilities Director was asked if he had to check the exit doors because a resident had been found outside the building. The Facilities Director stated, No ma'am.
Interview with the Maintenance Technician on 7/15/19 at 10:55 AM, in the Conference Room, the Maintenance Technician was asked about the doors that did not alarm or lock on 9/10/18 when a resident with a wanderguard approached. The Maintenance Technician stated, They [staff] told me it just wasn't locking. We had the security guard come over and make sure of the times they [doors] were locking .
The Maintenance Technician confirmed the door was not checked or repaired for wanderguard functioning.
7. Medical record review revealed Resident #38 was admitted to the facility on [DATE] and readmitted on [DATE] with diagnoses of Alzheimer's Disease, Impulse Disorder, Depression, Dementia with Behavioral Disturbance, Hypertension, Hallucinations, and Repeated Falls.
Medical record review of the admission MDS dated [DATE] documented moderate cognitive impairment per staff assessment, required supervision with transfers, walking, and locomotion.
Medical record review of the Care Plan for Resident #38 with a revision date of 7/8/19 documented, .The resident is an elopement risk/wanderer r/t Disoriented to place, Impaired safety awareness, Resident wanders aimlessly .Interventions .Distract from wandering by offering pleasant diversions, structured activities, food, conversation, television, book. Resident prefers .Date Initiated: 05/02/2019 .WANDER GUARD IN PLACE .Date Initiated: 05/02/2019 .
Medical Record review of the Wander Elopement Risk Assessments for Resident #38 dated 4/30/19, 6/28/19 and 7/12/19 documented, .High Risk to Wander .
Medical record review of Progress Notes dated 4/30/19 through 7/6/19 documented Resident #38 was frequently wandering in and out of other resident rooms, had unsteady gait with stumbling steps noted at times, had exit seeking behaviors, was difficult to redirect, had poor safety awareness, and needed constant supervision.
Medical record review of a Progress Note dated 5/4/19 documented, .Resident [#38] has exhibited exit seeking behavior all day. She walks independently without assistive device. Resident walks from door to door trying to get outside. She was observed walking out the front door with a group of visitors on Skilled Care .Unable to redirect resident from exit seeking due to dementia .
Observations in the Skilled Hall on 7/8/19 at 11:20 AM revealed Resident #38 was seated in a chair holding a baby doll, oriented to person only, and talking about wanting to get home with the rest of the family.
Interview with the ADON on 7/14/19 at 4:27 PM, in the Conference Room, the ADON stated, She [Resident #38] was really hard to redirect .she would walk until she tired herself out .It [behaviors] started 5/2/19 and ended 6/27/19 when she went out to the hospital. The ADON was asked when the wanderguard was reordered and why. The ADON stated, .7/12/19 .She [Resident #38] showed signs of trying to exit seek again . The ADON confirmed Resident #38 had a history of exit-seeking behavior.
8. Medical record review revealed Resident #2 was admitted to the facility on [DATE] and readmitted [DATE] with diagnoses of Hypertensive Heart Disease with Heart Failure, Hemiplegia (paralysis) Affecting Right Dominant Side, Hypothyroidism, Depression, Atrial Fibrillation, Gastro-Esophageal Reflux Disease, Presence of a Cardiac Pacemaker, and Anemia, Generalized Muscle Weakness, and Other Abnormalities of Gait and Mobility.
Medical record review of a Physician order dated 4/17/19 documented, .WANDERGUARD BRACELET AT ALL TIMES every day and night shift for safety .
Medical record review of a Progress Note for Resident #2 dated 5/2/19 documented, .Continue to try to get out the front door .said I tried so hard to escape and I could not .Wanderguard on patient left ankle intact .
Medical record review of a Progress Note dated 5/5/19 documented, .He has wandered on and off all day. His primary mode of locomotion is by wheelchair. He self propels with his feet, he has tried to exit front doors and is difficult to redirect .
Medical record review of a Progress Note for Resident #2 dated 5/10/19 at 9:24 AM documented, .Patient testing doors and wandering up and down hallway and into other patients [patients'] rooms. He is difficult to redirect at times and not redirect-able at others .
Medical record review of a Progress Note dated 5/10/19 at 12:40 PM documented, .Patient anxious. Testing doors. Propelling self in wheelchair into others [others'] rooms .
Medical record review of the Care Plan for Resident #2 revised 6/13/19 documented, .The resident has an ADL self-care performance deficit .Interventions .WANDERGUARD BRACELET AT ALL TIMES Date Initiated: 04/04/2019 .The resident has impaired cognitive function/dementia or impaired thought processes r/t memory loss, impaired safety awareness, behavioral symptoms . Interventions . WANDERGUARD BRACELET AT ALL TIMES Date Initiated: 04/04/2019 .
Medical record review of the quarterly MDS dated [DATE] revealed moderate cognitive impairment by staff assessment and required the use of wander/elopement alarms.
Observations in Resident #2's room on 7/8/19 at 12:35 PM and on 7/8/19 at 4:00 PM, revealed Resident #2 lying in bed, alert with a wanderguard device in place.
9. Medical record review revealed Resident #70 was admitted to the facility on [DATE] and readmitted on [DATE] with diagnoses of Cerebrovascular Disease, Chronic Obstructive Pulmonary Disease, Generalized Muscle Weakness, Repeated Falls, Diabetes, Pulmonary Hypertension, and Other Abnormalities of Gait and Mobility.
Medical record review of the quarterly MDS dated [DATE] documented a BIMS score of 3 which indicated severe cognitive impairment, and required staff assistance for all ADLs.
Medical record review of Progress Notes dated 3/13/19 documented, .has a wanderguard in place d/t risk for wandering/exiting building unassisted .
Medical record review of the Care Plan for Resident #70 revised 6/4/19 documented, .The resident has impaired cognitive function/dementia or impaired thought processes . Interventions .supervise as needed Date Initiated: 02/23/2018 .Potential for Elopement .Interventions .Wanderguard to be applied (remain in place at all times) d/t possible elopement Date Initiated: 04/19/2018 .
Medical record review of Progress Notes dated 6/10/19 documented, .has a wanderguard in place d/t risk for wandering/exiting building unassisted .
Medical record review of a Physician order for Resident #70 dated 7/8/19 documented, .Wander Guard to ankle d/t possible elopement .
Observations in the South Dining Room on 7/12/19 at 10:13 AM revealed Resident #70 seated in a wheelchair coloring. He was alert and confused, and had a wanderguard to his ankle.
10. Medical record review revealed Resident #377 was admitted to the facility on [DATE] with diagnoses of Trochanter Bursitis of Bilateral Hips, Intervertebral Disc Disorders, History of Falling, Hypothyroidism, Hypertension, Hyperlipidemia, Dementia, Anemia, and Cognitive Communication Deficit.
Medical record review of a Progress Note dated 7/9/19 documented, .has been observed ambulating out of other pt's [patient's] rooms .has also attempted to go out of main entrance doors stating that I am going to my daughters [daughter's] house .
Medical record review of the Order Summary Report documented, .Wander guard at all times .Start Date .07/10/2019 .
Observations in Resident #377's room on 7/11/19 at 2:17 PM revealed Resident #377 seated in a chair with a wanderguard on her left ankle.
Interview with the ADON on 7/14/19 at 4:19 PM, in the Conference Room, the ADON was asked why Resident #377 had a wanderguard. The ADON stated, .she did attempt to exit building .
11. Observations at the Hall 4 [NAME] Exit door on 7/10/19 at 3:46 PM, revealed the Facilities Director had a wanderguard tester device in his hand and held it near the exit door. No alarm sounded. The Facilities Director held the testing device up to the door again and no alarm sounded. The Facilities Director tried the third time, and the alarm sounded.
Interview with the Facilities Director at the Hall 4 [NAME] exit door on 7/10/19 at 3:50 PM, the Facilities Director stated, This [door alarm] should have went off .
Observations of all facility exit doors on 7/11/19 beginning at 3:35 PM, revealed the Facilities Director used a handheld wanderguard device, for checking the wanderguard alarm system but the Hall 4 [NAME] door did not lock when approached on first 2 attempts (the door should have automatically locked and alarmed when approached with the wanderguard device). The Facilities Director stated, It's [alarm] working intermittently. The Facilities Director used a second wanderguard alarm device and the Hall 4 [NAME] door only locked or alarmed intermittently. The Facilities Director stated, .left lower door alarm is not working . The Facilities Director stated the [NAME] 4 Hall door had an area of the door that was not working, there was only a certain area that was working and this was why the door would lock and alarm intermittently. The Facilities Director was asked if the door was secure to protect residents from elopement. The Facilities Director stated, It's a 1 foot area in the center of the door that's not picking up the wander guard signal .sensors need adjusting . The Facilities Director stated, .[Hall 6] door stays locked all the time, and you put in a code to get out. The Facilities Director had a wanderguard testing device in his hand, entered the door code, opened the door 3 times, and no alarm sounded. The Facilities Director stated, This door .is not equipped with a working wanderguard sensor .
Interview with the Interim Administrator on 7/10/19 at 2:10 PM, in the Conference Room, the Interim Administrator was asked if the area where the residents went out to smoke was in an enclosed courtyard. The Interim Administrator confirmed the courtyard was not secured and residents could leave the premises.
Interview with the Interim Administrator on 7/11/19 at 4:27 PM, at the Hall 6 Exit door during wanderguard testing, the Interim Administrator stated, A wanderer could get out.
Interview with the Interim Administrator and the Facilities Director during observations of all 8 facility exit doors on 7/11/19 beginning at 5:07 PM, the Facilities Director and the Interim Administrator confirmed 4 of 8 (Hall 6 door, Hall 3 Dining Room door, Hall 2 Dining Room door, and Hall 1 door) exit doors were not equipped with wanderguard device alarms and the wanderguard sensor for the Hall 4 [NAME] door was not functioning correctly.
Observations at the Hall 4 [NAME] Hall door by the laundry room on 7/11/19 beginning at 8:10 PM, revealed the door was unlocked and unsecured.
Interview with the Interim Administrator, DON, ADON, and the Facilities Director, on 7/12/19 at 11:04 AM, the Facilities Director stated, I thought the keypads were the first defense. We were checking the keypad not the wanderguard. I thought [wanderguard] was our last line of defense .
Interview with the Maintenance Technician on 7/15/19 at 10:55 AM, in the Conference Room, the Maintenance Technician was asked what kind of checks he had been doing on the doors related to the wanderguards. The Maintenance Technician stated, I would just check to see if they couldn't stroll on out the door without pressing the keypad number. The Maintenance Technician was asked if all the doors were equipped for the wanderguards. The Maintenance Technician stated, 3 . The Maintenance Technician confirmed there were 4 exit doors in the facility that were not equipped with wanderguard alarms prior to 7/12/19 and the Hall 4 [NAME] door wanderguard sensor was not functioning correctly prior to 7/12/19. The Maintenance Technician confirmed he had not been routinely checking the doors for wanderguard functioning.
Interview with the Interim Administrator and the Assistant Administrator on 7/15/19 at 11:50 AM, in the Conference Room, the Interim Administrator was asked if he had the measurements to the highway. Measurements provided and confirmed by the Interim Administrator on 7/15/19 at 11:50 AM revealed the facility was 156 [TRUNCATED]
CRITICAL
(K)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Administration
(Tag F0835)
Someone could have died · This affected multiple residents
Based on the Interim Administrator's Contract, Director of Nursing Job Description, medical record review, observation, and interview, the Interim Administrator failed to administer the facility in a ...
Read full inspector narrative →
Based on the Interim Administrator's Contract, Director of Nursing Job Description, medical record review, observation, and interview, the Interim Administrator failed to administer the facility in a manner that enabled the facility to use its resources effectively and efficiently to attain and maintain the highest practicable well-being of the residents. Administration failed to ensure the residents that smoked had adequate supervision, and failed to provide oversight and training of staff to ensure the security devices for the exit doors were operational and the exit codes to the doors remained secure. The Administration's failure placed Residents #2, #12, #13, #18, #22, #30, #38, #70, #88, #102, #180, and #377 in Immediate Jeopardy when staff did not assess, report, implement, evaluate or monitor for resident safety concerns for smoking and elopements.
Immediate Jeopardy (IJ) is a situation in which the provider's noncompliance with one or more requirements of participation has caused or is likely to cause serious injury, harm, impairment, or death to a resident.
The Interim Administrator, Assistant Administrator, Director of Nursing (DON), Assistant Director of Nursing (ADON), Infection Preventionist, Quality and Infection Preventionist, and the Minimum Data Set (MDS) Coordinator #2, were notified of the Immediate Jeopardy on 7/12/19 at 9:32 PM, in the Conference Room.
The facility was cited at scope and severity of Immediate Jeopardy for F657-K, F689-K, F835-K, F841-K, and F867-K.
The Immediate Jeopardy was effective 9/8/18 through 7/15/19 and the IJ was removed on 7/15/19.
An extended survey was conducted on 7/12/19 through 7/15/19.
An acceptable Allegation of Compliance (AOC), which removed the immediacy of the jeopardy, was received on 7/14/19 at 5:30 PM, and the corrective actions were validated onsite by the surveyors on 7/14/19 and 7/15/19 through review of assessments, auditing tools, in-service training records, policies, observations, and staff interviews.
The noncompliance continues at F835-E for monitoring of effectiveness of the corrective actions.
The findings include:
The facility's Interim Administrator Contract dated 4/12/19 documented, .This Agreement shall be governed by and construed in accordance with the laws of the State of Tennessee .The Contractor agrees to .Oversees all activities of the care center in accordance with established policies and federal and state guidelines .Develop strategic plans for profitability and accountability for all operations and programs .Administer, direct and coordinate the business .Recommend and lead changes to improve the care center .Maintain a state administrator license .Create functional strategies and specific objectives for the care center and develop budgets/policies/procedures to support the functional infrastructure .Implement Administrator-in-Training Program .
The facility's Director of Nursing Job Description dated 6/17/19 documented, .Under the direction of the Administrator, the DON has 24-hour responsibility for the effective implementation of the philosophy, goals, policies, and procedures .The DON has authority to make decisions .in the areas of patient care .Demonstrated leadership ability and potential managerial competency .Evidence of this includes, but is not limited to .ability to confront/resolve issues, ability to motivate others, ability to plan, organize, and direct the activities of others .Assist the Administrator in development, implementation and evaluation of on-going service programs that assure quality nursing and resident care programs consistent with health system mission .Evaluates on-going programs as assigned by Administrator .Monitors/maintains care center compliance with regulatory, accrediting and health system policy for resident services, and environmental and personnel safety .and/or universal precautions procedures as evidenced by PI [Performance Improvement] reports, incident follow-ups, staff meeting minutes and direct observation by Administrator .Oversees Care Center PI program which monitors and evaluates critical aspects of care .Accurately identifies real/potential problems affecting the services and implements solutions with follow-through and communications . ensures department delivers quality services in accordance with applicable policies, procedures, and professional standards .
Interview with the DON on 7/10/19 at 9:41 AM, in the Conference Room, the DON was asked if the residents knew the security codes to the exit doors and if residents could go out freely at anytime. The DON stated, Yes.
Interview with the Interim Administrator, DON, ADON, MDS Coordinator #1 on 7/10/19 at 1:33 PM, in the Conference Room, the Interim Administrator was asked if they had identified problems with smoking at the facility. The Interim Administrator stated, We talked about smoking .June .that's when we formally as a group said, 'guys we need to address this issue' .talked about a supervised schedule . The Interim Administrator was asked if a supervised schedule had been implemented. The Interim Administrator stated, Not yet. The Administrator was asked if the residents were allowed to have their smoking materials, including lighters, in their possession, and allowed to go out unsupervised. The Interim Administrator stated, That's correct . The Interim Administrator confirmed the Hall 6 Smoking Porch opened to a Courtyard that was not secure or enclosed.
Interview with the Interim Administrator on 7/11/19 at 4:27 PM, at the Hall 6 exit door during wander guard testing, the Interim Administrator stated, A wanderer could get out. The Interim Administrator was unable to state how long the 5 of 8 wanderguard door alarm devices had not been functioning.
Interview with the Interim Administrator and the Assistant Administrator on 7/14/19 at 9:15 AM, in the Conference Room, the Interim Administrator was asked when he became aware that residents were smoking unsupervised. The Interim Administrator stated, .This is really something pretty serious .around the middle of the month of June . The Interim Administrator stated, .we would be periodically walking out, and we would say wait a minute. There is nobody out here with these [residents] .I had been working with .the consultant .one of the things she said we need to be jumping on . The Interim Administrator was asked about residents having lighters in their possession in their rooms when they received oxygen therapy. The Interim Administrator stated, .just learning they had lighters, oxygen or not .I don't have this documented but I sat out with [Named Resident #88 and #22], and said I understand you have lighters, and we can't let you have those .
Administration failed to provide oversight of staff when they failed to ensure a safe and consistent smoking regimen for residents which resulted in IJ for Resident #22, #30, #88, #102, and #180. The Administration failed to ensure staff maintained the confidential codes to the secure exit doors, which allowed residents to exit the building unsupervised. Administration failed to ensure the safety of residents with elopement risk, by not ensuring the wanderguard security devices on the exit doors were operational which placed Resident #2,#12, #13, #18, #38, #70, and #377 in IJ.
Refer to F657 and F689.
The surveyors verified the AOC by:
1. The facility's Leadership Team consisting of the Interim Administrator, Assistant Administrator, DON, ADON, Minimum Data Set Coordinator #2, Infection Preventionist, and Activity Director have been assessing the procedures related to resident smoking practices in an attempt to balance residents' rights while ensuring the safety of all residents and patients in the building. While the facility's planned goal is to incorporate a Smoke Free Campus policy, a short term intervention providing safe supervision for smoking residents has been implemented until proper notice can be provided to those affected residents and resident representatives. The Leadership Team began the development of an updated Smoking Policy, a Designated Smoking Time Schedule and a Staff Monitoring Tool to ensure there was a structured program in place for oversight and safety assurance for those residents who expressed a desire to smoke. The final policy and protocols were implemented 7/10/19. On 7/10/19 the Leadership Team met with the facility staff members and each affected resident to explain the facility's position on supervised smoking, safety concerns and the processes going forward. Even though there was reluctance and concern expressed by the affected residents, all agreed to voluntarily surrender any smoking paraphernalia on their person and in their rooms. Each resident room was visited to ensure no additional smoking items were overlooked. All such paraphernalia is kept locked up and secured by the Unit 6 Charge Nurse and is only being released to the assigned smoking monitor during the designated smoking times.
The surveyors interviewed all facility staff which included all disciplines and staff on each shift. The surveyors reviewed the new smoking policy, staff monitoring tool, and interviewed the Nurse on the medication cart for Hall 5 where the smoking materials were secured.
2. The Interim Administrator and Assistant Administrator met with the five (5) residents, who desire to smoke, on 7/14/19 to discuss the Designated Smoking Time Schedule in order to gain their input and acceptance of the new set time schedule for smoking. They were informed that reasonable accommodations will be provided for those who might not be able to meet the exact Designated Smoking Time Schedule and informed of the impending 8/12/19 date as the time in which the facility will become Smoke Free. All indicated that they understood and had every intention of complying.
The surveyors reviewed the new Designated Smoking Time Schedule and the Daily Smoking Monitoring Tool.
3. The Social Service staff have called and reached all but five (5) families/representatives as of 7/14/19 and informed them of the new Smoking and Door Code changes; those who were not reached were left messages and the facility will continue to reach out to all families until all have been properly informed. In addition to personal contact with families, the facility has posted a notice on each outside door, outlining the process for gaining entry into the building. As an additional communication effort the facility has mailed a letter with the same details, officially notifying all family members of the facility's plan to become a Smoke Free Campus. Those letters will be mailed to each responsible party on 7/15/19.
The surveyors reviewed resident charts to verify the calls were documented. the surveyors observed the Social Service staff calling the families to update the famlies on the new smoking and Door Code changes.
4. The facility Maintenance Director and Administrator performed a complete operational assessment of all of the facility exit doors on July 11, 2019, and determined that five (5) of the eight (8) exit doors had not been completely equipped with full wandering prevention [elopement] capabilities. While these doors were protected by a magnetic locking system, it was determined that an additional antenna alarm system installation would provide additional safety and protection. A certified door alarm vendor was immediately contacted upon discovery and arrived on site at 7:15 A.M. on 7/12/19 and installed the additional monitoring devices. The system was tested by the Maintenance Department and was working as designed. The Facilities Director and Maintenance Technicians will oversee the functionality of the system by conducting daily tests of the exit door equipment and resident/patient transmitting devices for two weeks. If all equipment is found to be functioning properly, checks will move to weekly. The audits will occur no less than weekly going forward.
The surveyors reviewed the new maintenance log for monitoring and tested the doors to ensure the doors were functioning appropriately. The door codes were changed and distributed to designated nursing staff only.
Noncompliance continues at a scope and severity level of E for the monitoring of the effectiveness of the corrective actions.
The facility is required to submit a Plan of Correction.
CRITICAL
(K)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0841
(Tag F0841)
Someone could have died · This affected multiple residents
Based on review of the Medical Director's Agreement Contract, policy review, medical record review, observation, and interview, the Medical Director failed to ensure resident care policies were develo...
Read full inspector narrative →
Based on review of the Medical Director's Agreement Contract, policy review, medical record review, observation, and interview, the Medical Director failed to ensure resident care policies were developed and implemented to use resources effectively and efficiently to attain and maintain the highest practicable functioning of all residents by failing to ensure an effective plan to assure the residents' environment was safe and that vulnerable residents were adequately supervised. The Medical Director failed to identify issues and concerns in the facility related to smoking safety and elopement risk, which resulted in Immediate Jeopardy (IJ) for Resident #2, #12, #13, #18, #22, #30, #38, #70, #88, #102, #180, and #377 when staff failed to assess, report, implement, evaluate or monitor for resident safety concerns related to smoking and elopements.
Immediate Jeopardy (IJ) is a situation in which the provider's noncompliance with one or more requirements of participation has caused or is likely to cause serious injury, harm, impairment, or death to a resident.
The Interim Administrator, Assistant Administrator, Director of Nursing (DON), Assistant Director of Nursing (ADON), Infection Preventionist, Quality and Infection Preventionist, and Minimum Data Set (MDS) Coordinator #2, were notified of the Immediate Jeopardy on 7/12/19 at 9:32 PM, in the Conference Room.
The facility was cited a scope and severity of Immediate Jeopardy for F657-K, F-689-K, F835-K, F841-K, and F867-K.
The extended survey was conducted on 7/12/19 through 7/15/19.
The Immediate Jeopardy was effective 9/8/18 through 7/15/19 and the IJ was removed on 7/15/19.
An acceptable Allegation of Compliance (AOC), which removed the immediacy of the jeopardy, was received on 7/14/19 at 5:30 PM, and the corrective actions were validated onsite by the surveyors on 7/14/19 and 7/15/19 through review of assessments, auditing tools, in-service training records, policies, observations, and staff interviews.
The noncompliance continues at F 841-E for monitoring of effectiveness of the corrective actions.
The findings include:
1. The Medical Director's Professional Services Agreement Contract signed 7/24/09 by the Medical Director, documented, .Overall coordination and execution of medical care .Assisting in developing procedures .Participating in establishing policies, procedures and guidelines designed to assure the provision of adequate, comprehensive services .Participating in the resident care management system .Participating in the Centers' inservice education program .Establishing with other health care professionals, policies designed to assure the governing body that all health care professionals practice within the scope .Providing consultation to the Centers' Administrator, Director of Nurses, and Social Services regarding the Centers' ability to meet the psychosocial, medical and physical needs of the residents .Advising the Administrator about the adequacy and appropriateness of the Centers scope of services for residents, medical equipment, and professional support staff .Helping to assure a safe and sanitary environment for residents and personnel .reviewing and evaluating occurrence reports .Identifying hazards to health and safety .Making relevant recommendations to the Administrator .Monitoring and evaluating quality and appropriateness of medical services as an integral part of the overall quality assessment and improvement program .Serving on committees .
2. Telephone interview with the Medical Director on 7/15/19 at 8:18 AM, the Medical Director was asked how he was involved in resident management. The Medical Director stated, I am the attending. That allows me to be directly involved with their care and planning. The Medical Director was asked if he had provided consultation to the facility's Administration staff regarding the facility's ability to meet the needs of the residents. The Medical Director stated, Yes, I do that on daily and weekly basis by reviewing conditions, looking at their needs, if we are able to meet their needs. The Medical Director was asked if he was involved in the implementation of smoking policies when the 2 residents (Resident #88 and #102) were grandfathered in to smoke. The Medical Director stated, No . The Medical Director was asked if he reviewed and evaluated occurrence reports. The Medical Director stated, once a week .I review them. The Medical Director was asked if he had talked with Administration about unsupervised smoking and Resident #102's burn incident. The Medical Director stated, I honestly didn't remember it .I'm sure I signed the incident report .burn on skin and clothing .That would be normal process. The Medical Director was asked if he was aware residents were allowed to keep lighters and cigarettes in their rooms while they received oxygen. The Medical Director stated, That is not good .That is very risky with oxygen involved. I don't think that was a good idea. The Medical Director was asked if unsupervised smoking was appropriate. The Medical Director stated, .It would make sense to supervise them. The Medical Director was asked if he was aware residents were going out the doors unsupervised with wanderguards on. The Medical Director stated, .that's interesting .maintenance definitely should be checking that system. The Medical Director was asked how he assured a safe environment for residents. The Medical Director stated, I think QA [Quality Assurance] meetings are key . The Medical Director was asked if he monitored and evaluated the quality and appropriateness of medical services as an integral part of the overall quality assessment and improvement program and how often he attended. The Medical Director stated, Monthly .
3. The Medical Director failed to ensure the residents received staff supervision for smoking and elopement risk, failed to assist the facility with the establishment, development, and implementation of safe smoking policies, and failed to ensure residents were not allowed to have lighters when oxygen was in use. The Medical Director failed to ensure vulnerable residents with wanderguards and elopement risks were protected from elopement accidents.
Refer to F689.
4. The Medical Director failed to ensure Administration was responsible for the identification, development, and implementation of appropriate policies and procedures to maintain the highest practicable well-being of all residents.
Refer to F835.
5. The Medical Director failed to ensure the Quality Assurance Performance Improvement Committee provided a safe environment for cognitively impaired residents with at risk behaviors related to smoking safety and elopement and that the residents were supervised and monitored to prevent accidents, which resulted in IJ for Resident #2, #12, #13, #18, #22, #30, #38, #70, #88, #102, #180, and #377.
Refer to F867.
The surveyors verified the AOC by:
1. The facility's Leadership Team consisting of the Interim Administrator, Assistant Administrator, DON, ADON, Minimum Data Set Coordinator #2, Infection Preventionist, and Activity Director have been assessing the procedures related to resident smoking practices in an attempt to balance residents' rights while ensuring the safety of all residents and patients in the building. While the facility's planned goal is to incorporate a Smoke Free Campus policy, a short term intervention providing safe supervision for smoking residents has been implemented until proper notice can be provided to those affected residents and resident representatives. The Leadership Team began the development of an updated Smoking Policy, a Designated Smoking Time Schedule and a Staff Monitoring Tool to ensure there was a structured program in place for oversight and safety assurance for those residents who expressed a desire to smoke. The final policy and protocols were implemented 7/10/19. On 7/10/19 the Leadership Team met with the facility staff members and each affected resident to explain the facility's position on supervised smoking, safety concerns and the processes going forward. Even though there was reluctance and concern expressed by the affected residents, all agreed to voluntarily surrender any smoking paraphernalia on their person and in their rooms. Each resident room was visited to ensure no additional smoking items were overlooked. All such paraphernalia is kept locked up and secured by the Unit 6 Charge Nurse and is only being released to the assigned smoking monitor during the designated smoking times.
The surveyors interviewed all facility staff which included all disciplines and staff on each shift. The surveyors reviewed the new smoking policy, staff monitoring tool, and interviewed the Nurse on the medication cart for Hall 5 where the smoking materials were secured.
2. The Interim Administrator and Assistant Administrator met with the five (5) residents, who desire to smoke, on 7/14/19 to discuss the Designated Smoking Time Schedule in order to gain their input and acceptance of the new set time schedule for smoking. They were informed that reasonable accommodations will be provided for those who might not be able to meet the exact Designated Smoking Time Schedule and informed of the impending 8/12/19 date as the time in which the facility will become Smoke Free. All indicated that they understood and had every intention of complying.
The surveyors reviewed the new Designated Smoking Time Schedule and the Daily Smoking Monitoring Tool.
3. The facility Maintenance Director and Administrator performed a complete operational assessment of all of the facility exit doors on July 11, 2019, and determined that five (5) of the eight (8) exit doors had not been completely equipped with full wandering prevention [elopement] capabilities. While these doors were protected by a magnetic locking system, it was determined that an additional antenna alarm system installation would provide additional safety and protection. A certified door alarm vendor was immediately contacted upon discovery and arrived on site at 7:15 A.M. on 7/12/19 and installed the additional monitoring devices. The system was tested by the Maintenance Department and was working as designed. The Facilities Director and Maintenance Technicians will oversee the functionality of the system by conducting daily tests of the exit door equipment and resident/patient transmitting devices for two weeks. If all equipment is found to be functioning properly, checks will move to weekly. The audits will occur no less than weekly going forward.
The surveyors reviewed the new maintenance log for monitoring and tested the doors to ensure the doors were functioning appropriately. The door codes were changed and distributed to designated nursing staff only.
Noncompliance continues at a scope and severity level of E for the monitoring of the effectiveness of the corrective actions.
The facility is required to submit a Plan of Correction.
CRITICAL
(K)
Immediate Jeopardy (IJ) - the most serious Medicare violation
QAPI Program
(Tag F0867)
Someone could have died · This affected multiple residents
Based on review of the Administrator's job description, review of the Medical Director's job description, review of the Director of Nursing (DON) job description, medical record review, and interview,...
Read full inspector narrative →
Based on review of the Administrator's job description, review of the Medical Director's job description, review of the Director of Nursing (DON) job description, medical record review, and interview, the Quality Assurance Performance Improvement (QAPI) committee failed to ensure an effective QAPI program recognized an ongoing concern related to smoking safety, residents with elopement risks that had knowledge of exit door codes and nonfunctioning wanderguard sensors on exit doors. The QAPI committee failed to ensure the facility identified the root cause of the concerns, developed appropriate plans of action, ensured systems and processes were in place and were consistently followed by staff to address quality concerns. The QAPI committee failed to ensure interventions to prevent unsupervised smoking were consistently implemented or followed, that the facility was administered in a manner that enabled it to use its resources effectively and efficiently, that the Medical Director assisted the facility with identifying, evaluating, and addressing clinical concerns, coordinated the medical care and provided clinical guidance and oversight regarding the implementation of resident care policies and procedures for residents that smoke and for residents with risk of elopement. The QAPI committee failed to ensure smoking and wandering assessments were timely and accurate. The failure of the QAPI Committee to ensure the facility implemented and/or provided care and services for the residents that smoked and demonstrated exit seeking behaviors placed 5 of 5 residents in Immediate Jeopardy (IJ) when Resident #22, #30, #88, #102, and #180 smoked without supervision and safe smoking care interventions were not provided as recommended. The failure of the QAPI Committee to ensure the facility implemented and/or provided care and services for the residents that demonstrated exit seeking behaviors placed 7 of 7 residents in Immediate Jeopardy when Resident #2, #12, #13, #18, #38, #70, and #377 had nonfunctioning wanderguards and door sensors, and maintenance failed to identify the sensor doors as nonfunctional.
Immediate Jeopardy (IJ) is a situation in which the provider's noncompliance with one or more requirements of participation has caused or is likely to cause serious injury, harm, impairment, or death to a resident.
The Interim Administrator, Assistant Administrator, Director of Nursing (DON), Assistant Director of Nursing (ADON), Infection Preventionist, Quality and Infection Preventionist for the health system, and the Minimum Data Set (MDS) Coordinator, were notified of the Immediate Jeopardy on 7/12/19 at 9:32 PM, in the Conference Room.
The facility was cited a scope and severity of Immediate Jeopardy for F657-K, F689-K, F835-K, F841-K, and F867-K.
The Immediate Jeopardy was effective 9/8/18 through 7/15/19 and the IJ was removed on 7/15/19.
An extended survey was conducted on 7/12/19 through 7/15/19.
An acceptable Allegation of Compliance (AOC), which removed the immediacy of the Jeopardy, was received on 7/14/19 at 5:30 PM, and the corrective actions were validated onsite by the surveyors on 7/14/19 and 7/15/19 through review of assessments, auditing tools, in-service training records, policies, observations, and staff interviews.
The noncompliance continues at F867-E for monitoring of effectiveness of the corrective actions.
The findings include:
1. The facility's Interim Administrator Contract dated 4/12/19 documented, .This Agreement shall be governed by and construed in accordance with the laws of the State of Tennessee .The Contractor agrees to .Oversees all activities of the care center in accordance with established policies and federal and state guidelines .Develop strategic plans for profitability and accountability for all operations and programs .Administer, direct and coordinate the business .Recommend and lead changes to improve the care center .Maintain a state administrator license .Create functional strategies and specific objectives for the care center and develop budgets/policies/procedures to support the functional infrastructure .Implement Administrator -in-Training Program .
2. The facility's Director of Nursing Job Description dated 6/17/19 documented, .Under the direction of the Administrator, the DON has 24-hour responsibility for the effective implementation of the philosophy, goals, policies, and procedures of the hospital and the nursing department and their effect on patient care in a designated unit.Evaluates on-going programs as assigned by Administrator .Monitors/maintains care center compliance with regulatory, accrediting and health system policy for resident services, and environmental and personnel safety .Monitors the staff's understanding of established emergency .and/or universal precautions procedures as evidenced by PI [Performance Improvement] reports, incident follow-ups, staff meeting minutes and direct observation by Administrator .Oversees Care Center PI program which monitors and evaluates critical aspects of care .Accurately identifies real/potential problems affecting the services and implements solutions with follow-through and communications .Is responsible for care center's operational excellence; ensures department delivers quality services in accordance with applicable policies, procedures, and professional standards .
3. The facility's Medical Director job description dated 7/2016 documented, .The Medical Director is a licensed physician in this state and is responsible for .Overseeing and helping develop and implement care-related policies and practices .Participating in efforts to improve quality of care and services .Acting as a consultant to the director of nursing services in matters relating to resident care services .Helping assure that residents receive adequate services appropriate to meet their needs .Helping assure that the resident care plan accurately reflects the medical regimen .Participating in staff meetings concerning .quality assurance and performance improvement .resident care policies .Assuring that physician services comply with current rules, regulations, and guidelines concerning long-term care .
Interview with the Interim Administrator on 7/13/19 at 3:08 PM, in the Conference Room, the Interim Administrator was asked if the Quality Assurance Committee (QAC) developed appropriate plans of action for smoking or elopements. The Interim Administrator confirmed that the QAC had not discussed the smoking concerns or the security door issue. The Interim Administrator was asked if the QAC had discussed the problem with the doors. The Interim Administrator confirmed he had discovered the problem at the same time we [surveyors] did during the survey this week. The Interim Administrator stated, .My spot checking that I did with [Facilities Director] was good, I just checked the wrong doors .
5. The Facility's QAPI committee failed to identify, develop, and implement appropriate plans of action to ensure care plans were reviewed, updated, and implemented for care of residents with diminished safety awareness.This resulted in IJ for Resident #22, #30, #88, #102, and #180.
Refer to F657.
6. The QAPI Committee failed to provide an acceptable standard of care for residents with diminished safety awareness and to prevent elopement. This resulted in Immediate Jeopardy for Resident #2, #12, #13, #18, #22, #30, #38, #70, #88, #180 and #377.
Refer to F689.
The surveyors verified the AOC by:
1. The facility's Leadership Team consisting of the Interim Administrator, Assistant Administrator, DON, ADON, Minimum Data Set Coordinator #2, Infection Preventionist, and Activity Director have been assessing the procedures related to resident smoking practices in an attempt to balance residents' rights while ensuring the safety of all residents and patients in the building. While the facility's planned goal is to incorporate a Smoke Free Campus policy, a short term intervention providing safe supervision for smoking residents has been implemented until proper notice can be provided to those affected residents and resident representatives. The Leadership Team began the development of an updated Smoking Policy, a Designated Smoking Time Schedule and a Staff Monitoring Tool to ensure there was a structured program in place for oversight and safety assurance for those residents who expressed a desire to smoke. The final policy and protocols were implemented 7/10/19. On 7/10/19 the Leadership Team met with the facility staff members and each affected resident to explain the facility's position on supervised smoking, safety concerns and the processes going forward. Even though there was reluctance and concern expressed by the affected residents, all agreed to voluntarily surrender any smoking paraphernalia on their person and in their rooms. Each resident room was visited to ensure no additional smoking items were overlooked. All such paraphernalia is kept locked up and secured by the Unit 6 Charge Nurse and is only being released to the assigned smoking monitor during the designated smoking times.
The surveyors interviewed all facility staff which included all disciplines and staff on each shift. The surveyors reviewed the new smoking policy, staff monitoring tool, and interviewed the Nurse on the medication cart for Hall 5 where the smoking materials were secured.
2. The Interim Administrator and Assistant Administrator met with the five (5) residents, who desire to smoke, on 7/14/19 to discuss the Designated Smoking Time Schedule in order to gain their input and acceptance of the new set time schedule for smoking. They were informed that reasonable accommodations will be provided for those who might not be able to meet the exact Designated Smoking Time Schedule and informed of the impending 8/12/19 date as the time in which the facility will become Smoke Free. All indicated that they understood and had every intention of complying.
The surveyors reviewed the new Designated Smoking Time Schedule and the Daily Smoking Monitoring Tool.
3. The facility Maintenance Director and Administrator performed a complete operational assessment of all of the facility exit doors on July 11, 2019, and determined that five (5) of the eight (8) exit doors had not been completely equipped with full wandering prevention [elopement] capabilities. While these doors were protected by a magnetic locking system, it was determined that an additional antenna alarm system installation would provide additional safety and protection. A certified door alarm vendor was immediately contacted upon discovery and arrived on site at 7:15 A.M. on 7/12/19 and installed the additional monitoring devices. The system was tested by the Maintenance Department and was working as designed. The Facilities Director and Maintenance Technicians will oversee the functionality of the system by conducting daily tests of the exit door equipment and resident/patient transmitting devices for two weeks. If all equipment is found to be functioning properly, checks will move to weekly. The audits will occur no less than weekly going forward.
The surveyors reviewed the new maintenance log for monitoring and tested the doors to ensure the doors were functioning appropriately. The door codes were changed and distributed to designated nursing staff only.
Noncompliance continues at a scope and severity level of E for the monitoring of the effectiveness of the corrective actions.
The facility is required to submit a Plan of Correction.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation, and interview, the facility failed to ensure accurate Minimum Data Set (MDS) assess...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation, and interview, the facility failed to ensure accurate Minimum Data Set (MDS) assessments were conducted for residents with wander/elopement alarms for 2 of 7 (Resident #5 and #70) sampled residents reviewed with elopement risk.
The findings include:
1. Medical record review revealed Resident #5 was admitted to the facility on [DATE] and readmitted [DATE] with diagnoses of Chronic Obstructive Pulmonary Disease (COPD), Anxiety, Generalized Muscle Weakness, Abnormalities of Gait and Mobility, Hypertension (HTN), Anemia, and Repeated Falls.
Medical record review of a Progress Note dated 9/24/18 documented, .Wanderguard put on Right leg for safety precautions d/t [due to] wandering in hallways asking how to get out of this place .
Medical record review of an annual MDS dated [DATE] revealed Resident #5 had a Brief Interview for Mental Status (BIMS) score of 7, which indicated severe cognitive impairment and no use of wander/elopement alarms (wanderguard).
Medical record review of the quarterly MDS dated [DATE] revealed Resident #5 had a BIMS score of 7, which indicated severe cognitive impairment and no use of wander/elopement alarms (wanderguard).
Medical record review of a Physician's Order for Resident #5 dated 6/27/19 documented, .Wanderguard in place every day and night shift for safety precautions .
Observations in Resident #5's room on 7/12/19 at 10:09 AM, revealed Resident #5 had a wanderguard device on her ankle.
Interview with MDS Coordinator #2 on 7/13/19 at 3:07 PM, outside the Conference Room, MDS Coordinator #2 confirmed the MDS assessments for Resident #5 dated 9/26/18 and 6/26/19 were inaccurate related to wander/elopement alarms (wanderguard).
2. Medical record review revealed Resident #70 was admitted to the facility on [DATE] and readmitted [DATE] with diagnoses of Cerebrovascular Disease, COPD, Muscle Weakness, Repeated Falls, Diabetes, Pulmonary HTN, and Abnormalities of Gait and Mobility.
Medical record review of Physician orders dated 4/19/18 documented, .Wander guard to ankle d/t possible elopement .
Medical record review of an annual MDS dated [DATE] documented a BIMS score of 3, which indicated severe cognitive impairment and no wander/elopement alarms (wanderguards) in use
Medical record review of a Progress Note dated 3/13/19 documented, .has a wanderguard in place d/t risk for wandering/exiting building unassisted .
Medical record review of Physician orders dated 4/10/19 documented, .Wander guard to ankle d/t possible elopement .
Medical record review of the quarterly MDS dated [DATE] documented a BIMS score of 3, which indicated severe cognitive impairment and no wander/elopement alarms in use.
Medical record review of a Progress Note dated 6/10/19 documented, .has a wanderguard in place d/t risk for wandering/exiting building unassisted .
Observations in the South Dining Room on 7/12/19 at 10:13 AM, revealed Resident #70 seated in a wheelchair coloring and he had a wanderguard device to his ankle.
Interview with MDS Coordinator #2 on 7/13/19 at 3:07 PM, outside the Conference Room, MDS Coordinator #2 confirmed the MDS assessments for Resident #70 dated 2/20/19 and 5/22/19 were inaccurate related to wander/elopement alarms.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation, and interview, the facility failed to provide care and services for an indwelling u...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation, and interview, the facility failed to provide care and services for an indwelling urinary catheter for 1 of 1 (Resident #227) sampled residents reviewed for urinary catheters.
The findings include:
Medical record review revealed Resident #227 was admitted to the facility on [DATE] with diagnoses of Fracture Right Pubis, Fracture of Sacrum, Dementia with Behavioral Disturbance, and Urinary Retention.
Observations in Resident #227's room on 7/12/19 at 8:19 AM revealed Resident #227 had an indwelling urinary catheter.
Medical record review of the Physician's Orders revealed there was no order for the urinary catheter from the admission date until 7/12/19.
Medical record review revealed there was no order for catheter care and there was no documentation of catheter care being performed.
Interview with the Infection Preventionist on 7/12/19 at 2:17 PM, at the Administration Desk, the Infection Preventionist confirmed Resident #227 had the indwelling urinary catheter since admission on [DATE].
Interview with the Staff Development Coordinator (SDC) on 7/12/19 at 2:23 PM at the Skilled Nurses' Station, the SDC was asked if there should be a physician's order for a urinary catheter. The SDC stated, Yes, there should be. The SDC confirmed catheter care should be done twice a day and as needed.
Interview with the Assistant Director of Nursing (ADON) on 7/12/19 at 2:57 PM, in the ADON Office, the ADON was asked if there should be an order for a urinary catheter and catheter care. The ADON stated, Absolutely . The ADON was asked how often she expected staff to perform catheter care for a resident with an indwelling urinary catheter. The ADON stated, Once a shift and as needed. The ADON was asked if the catheter care should be documented. The ADON stated, Yes.
The facility was unable to provide a physician's order for the indwelling urinary catheter or that catheter care was performed for Resident #227.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation, and interview, the facility failed to ensure accurate and complete medical records ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation, and interview, the facility failed to ensure accurate and complete medical records for 7 of 56 (Resident #2, #22, #30, #88, #102, #180, and #377) sampled residents reviewed.
The findings include:
1. Medical record review revealed Resident #2 was admitted to the facility on [DATE] and readmitted [DATE] with diagnoses of Hypertensive Heart Disease with Heart Failure, Hemiplegia (Paralysis on one side of his body), Hypothyroidism, Depression, Atrial Fibrillation, Gastro-esophageal Reflux Disease, Cardiac Pacemaker, Anemia, Generalized Muscle Weakness, and Abnormalities of Gait and Mobility.
Medical record review of a Progress Note dated 3/13/19 documented, .Alert and oriented to self .
Medical record review of a WANDERING RISK SCALE dated 3/13/19 documented, .The resident is comatose, dependent on ADL [activities of daily living] and cannot move without assistance, and/or stuporous .YES . The Wandering Risk Scale was incomplete and did not have the following areas completed:
a. Mental Status
b. Mobility
c. Speech Patterns
d. History of wandering
e. Diagnosis.
Medical record review of a Progress Notes dated 3/14/19 documented, .alert and oriented and able to verbalize his needs .
Observations on 7/8/19 at 12:35 PM revealed Resident #2 in bed, awake and alert.
Medical record review of the Wander Risk assessment dated [DATE] revealed it was inaccurate related to documentation the resident was in a comatose state. The Progress Note documented the resident was alert and oriented. The Wander Risk Assessment was incomplete.
2. Medical record review revealed Resident #22 was admitted to the facility on [DATE] and readmitted [DATE] with diagnoses of Diabetes Mellitus, Cerebral Infarction, Heart Failure, Major Depression, and Anxiety.
Medical record review of the admission Minimum Data Set (MDS) dated [DATE] revealed Resident #22 had a Brief Interview for Mental Status (BIMS) score of 4 which indicated severe cognitive impairment. The resident required limited to extensive staff assistance with Activities of Daily Living (ADL) and used tobacco and required oxygen therapy.
Medical record review of SMOKING-SAFETY SCREEN assessments documented the following:
a. 1/30/19 .no cognitive loss, resident can light own cigarette, resident is not going to smoke while a resident in this facility.
b. 7/2/19 .no cognitive loss .resident does not need facility to store lighter and cigarettes .Resident can safely light a cigarette and smoke safely without supervision .
Medical record review of the Smoking-Safety Screens revealed Resident #22 had no cognitive loss and had the ability to light a cigarette. The MDS assessment documented Resident #22 had severe cognitive impairment and needed extensive assistance with ADLs.
3. Medical record review revealed Resident #30 was admitted to the facility on [DATE] and readmitted [DATE] with diagnoses of Hemiplegia & Hemiparesis following Cerebral Infarction Affecting Left Non-Dominant Side, Asthma, Noncompliance with Medication Regimen, Hypertension, Atherosclerotic Heart Disease, Dysphagia, Hyperlipidemia, Tobacco Use, and Alcohol Dependence.
Medical record review of the quarterly MDS dated [DATE] revealed a BIMS score of 15, which indicated no cognitive impairment, and required extensive assistance with ADLs.
Medical record review of the Smoking-Safety Screen dated 7/2/19 revealed Resident #30 had no dexterity problems and had the ability to light a cigarette, but medical record review revealed a diagnosis of Hemiparesis (paralysis on one side of the body) and the MDS assessment documented Resident #30 needed extensive assistance with ADLs. The Smoking - Safety Screen assessment was inaccurate.
4. Medical record review revealed Resident #88 was admitted to the facility on [DATE] and readmitted on [DATE] with diagnoses of Cerebrovascular Disease, Hemiplegia (Pasralysis on one side of his body), Congestive Heart Failure, Dementia, Atrial Fibrillation, Chronic Obstructive Pulmonary Disease, Aphasia, Hypertension, Diabetes, Nicotine Dependence, Coronary Artery Disease, and Implantable Cardiac Defibrillator.
Medical record review of the quarterly MDS dated [DATE] revealed Resident #88 had range of motion impairment on one side for upper and lower extremities and required extensive assistance for ADLs.
Medical record review of the Smoking Safety Screen dated 6/12/19 revealed Resident #88 had no dexterity problems, but medical record review revealed a diagnosis of Hemiparesis and the MDS revealed Resident #88 required extensive assistance with ADLs.
5. Medical record review revealed Resident #102 was admitted to the facility on [DATE] with diagnoses of Hemiplegia (Paralysis on one side of her body), Dysphagia, Anxiety Disorder, Alzheimer's Disease, Expressive Language Disorder, and Benign Neoplasm of the Brain.
Medical record review of an annual MDS dated [DATE] revealed Resident #102 had a BIMS score of 12 which indicated moderate cognitive impairment and the resident used tobacco and oxygen.
Review of a Web Event Summary Report dated 3/23/19 documented the resident received the burn to the abdomen inside the facility.
Interview with MDS Coordinator #2 on 7/11/19 at 2:12 PM in the Conference Room, MDS Coordinator #2 confirmed the Web Event Summary Report dated 3/23/19 was inaccurate and stated, This was coded in error it should have been coded 11, which is other, outside.
Medical record review of a SMOKING-SAFETY SCREEN dated 12/19/18 documented Resident #102 had cognitive loss, was visually impaired, and retained her own cigarettes and lighter.
Medical record review of a SMOKING-SAFETY SCREEN dated 3/19/19 documented, .Does resident have cognitive loss .Yes .visual defects .No .Does resident need facility to store lighter and cigarettes .No .
Medical record review of a SMOKING-SAFETY SCREEN dated 4/12/19 documented, .Does resident have cognitive loss .Yes .visual defects .No .Does resident need facility to store lighter and cigarettes No .
Medical record review of a SMOKING-SAFETY SCREEN dated 6/19/19 documented, .Does resident have cognitive loss .Yes .visual defects .No .Does resident need facility to store lighter and cigarettes No .
Interview with the Assistant Director of Nursing (ADON) on 7/14/19 at 4:21 PM in the Conference Room, the SMOKING-SAFETY SCREEN dated 12/19/18, 3/19/19, 4/12/19, and 6/19/19 were reviewed with the ADON, and she confirmed the Smoking Safety Screens were inaccurate. The ADON was asked if Resident #102 had cognitive loss on the Smoking Safety Screen dated 12/19/19, which was coded as no cognitive loss. The ADON stated, She does [have cognitive loss] The ADON stated, We go over everything in the team meeting. We talk about all the residents then MDS [Coordinator] will go back and fill the screen out. The ADON was asked if Resident #102 had Alzheimer's Disease would that be a cognitive loss. The ADON stated, Yes, as a diagnosis .She should be coded Yes .
The ADON was asked if the Resident #102 had any visual deficits on the Smoking Screen dated 3/19/19, 4/12/19, and 6/19/19 which was coded as No. The ADON stated, .Should be marked Yes. The ADON was asked if the resident had any dexterity problems. The ADON stated, It should be marked .Yes. The ADON was asked if Resident #102 could light her own cigarette. The ADON stated, She always did . The ADON was asked if Resident #102 needed the facility to store her lighter and cigarettes. The ADON stated, .she does at this time, We should have stored them .
Review of the medical record for Resident #102 revealed the record was inaccurate as to the resident's cognition and smoking safety.
6. Medical record review revealed Resident #180 was admitted to the facility on [DATE] and readmitted [DATE] with diagnoses of Hemiparesis (Paralysis on one side of his body), Depression, Insomnia, Anxiety, Hepatitis C, Hyperlipidemia, Alcohol Dependence, Hypertension, Coronary Artery Disease, Cerebral Infarction, Nontraumatic Subarachnoid Hemorrhage, and Chronic Obstructive Pulmonary Disease.
Medical record review of an admission MDS assessment dated [DATE] revealed Resident #180 had a BIMS score of 12 which indicated Resident #180 was moderately cognitively impaired.
Medical record review of a WANDERING RISK SCALE dated 4/1/19 documented the resident had dementia and was cognitively impaired.
Medical record review of a Progress Note dated 4/4/19 documented, .alert and oriented with episodes of confusion and forgetfulness .
Medical record review of a SMOKING-SAFETY SCREEN dated 7/2/19 documented the resident was not cognitively impaired.
Interview with the ADON on 7/14/19 at 4:21 PM in the Conference Room, the ADON was asked about the cognition documentation on the Wandering Risk Scale dated 4/1/19 and the Smoking Safety Screen dated 7/2/19. The ADON was asked if the documents were accurate. The ADON stated, They are not correct .He does not have a dementia diagnoses. That one is wrong [pointed to wandering screen] .
7. Medical record review revealed Resident #377 was admitted to the facility on [DATE] with diagnoses of Dementia, Trochanteric Bursitis of Bilateral Hips, Intervertebral Disc Disorders, History of Falling, Hypothyroidism, Hypertension, Hyperlipidemia, Anemia, and Cognitive Communication Deficit.
Medical record review of an admission WANDERING RISK SCALE dated 7/1/19 documented the resident did not have a diagnosis of dementia.
Medical record review of a Progress Note dated 7/9/19 documented, .has been observed ambulating out of other pt's [patient's] rooms .pt. [Patient] has also attempted to go out of main entrance doors stating that I am going to my daughter's house .
Interview with the ADON on 7/14/19 at 4:19 PM in the Conference Room, the ADON confirmed the Wandering Risk Assessment was inaccurate related to the diagnosis of Dementia.