CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, job description review, review of facility investigations, medical record review, observation, and inter...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, job description review, review of facility investigations, medical record review, observation, and interview, the facility failed to ensure the Resident Rights to be free from abuse/neglect for 2 of 5 sampled residents (Resident #3 and #6) reviewed for abuse. The facility's failure to ensure a resident's right to be free from abuse/neglect resulted in Immediate Jeopardy when the facility failed to provide adequate supervision for 2 vulnerable residents with severe cognition impairment. Resident #6 exited the facility unsupervised and without staff knowledge on 2 separate occasions, 6 days apart on 11/9/2022 and 11/15/2022; and Resident #3, exited the facility unsupervised and without staff knowledge on 12/20/2022.
Immediate Jeopardy (IJ) is a situation in which the provider's noncompliance with one or more requirements of participation has caused, or is likely to cause, serious injury, harm, impairment, or death to a resident.
The Administrator, Director of Nursing and the Regional Director of Operation were notified of the Immediate Jeopardy (IJ) for F-600 during the complaint investigation on 1/9/2023 at 4:40 PM, in the Conference Room.
The facility was cited at F-600 at a scope and severity of J, which is Substandard Quality of Care.
A partial extended survey was conducted from 1/10/2023 through 1/13/2023.
The Immediate Jeopardy existed from 11/9/2022 through 1/16/2023.
An acceptable Removal Plan, which removed the immediacy of the jeopardy, was received on 1/12/2023 at 9:03 PM, and was validated onsite by the surveyors on 1/17/2023 through review of in-services, audits, and staff interviews conducted.
The findings include:
1. Review of the facility's policy titled, Abuse, Neglect and Exploitation, revised 10/24/2022, revealed .It is the policy of this facility to provide protections for the health, welfare, and rights of each resident by developing and implementing written policies and procedures that prohibit and prevent abuse neglect .Neglect .means failure of the facility, its employees, or service providers to provide goods and services to a resident that are necessary to avoid physical harm, pain, mental anguish, or emotional distress .
2. Review of the facility's Administrator Job Description signed 12/1/2015, revealed .Responsible for the efficient and profitable operation of the facility, facility compliance with .State and Federal rules and regulations, and providing the highest quality of care possible .Manages the day-today operation of the facility .Implements control systems to ensure accountability of all departments .Ensures all employees receive orientation and ongoing training to meet the quality goals of the organization .Knowledge of Long term Care and Medicare and Medicare regulations and standards .
Review of the facility's Director of Nursing Job description signed 9/26/2022, revealed .Manages the facility nursing program in accordance with the Nurse Practice Act, applicable State and Federal regulations, and policies and procedures .Round on unit at least once daily .Manage the Nursing Department with the goal of achieving and maintaining the highest quality of care .Identification of training needs .Assures that all clinical protocols and nursing policies and procedures are followed .Assumes complete responsibilities for the Center in absence of Administrator .
3. Review of medical record revealed Resident #6 was admitted to the facility on [DATE], with diagnoses of Parkinson's Disease, Osteoarthritis, Major Depression, Chronic Obstructive Pulmonary Disease, Repeated Falls, and Hypertension.
Review of the quarterly Minimum Data Set (MDS) dated [DATE], revealed Resident #6 had a Brief Interview for Mental Status (BIMS) score of 4, which indicated severe cognition impairment, and wandering behavior was not coded.
Review of the 24 HOUR REPORT/CHANGE OF CONDITION REPORT dated 10/21/2022 revealed, .[Named Resident #6] .Exit seeking .
Review of the 24 HOUR REPORT/CHANGE OF CONDITION REPORT dated 10/23/2022 revealed, .[Named Resident #6] .wandering [increased] shift/evening .
Review of the Progress Note dated 10/23/2022 revealed, .Resident wandering throughout evening shift. Resident attempted to exit facility x [times] 2 .
Review of the Progress Note dated 11/9/2022 revealed .On 11/9/2022, [Named Resident #6] was last seen in her room going to the restroom by the nurse. At 7:40 [7:40 PM], door alarmed [alarm] sounded .Resident was located outside of 300/400 hall side emergency door by CNA [Certified Nursing Assistant] and nurse .
Review of an Incident Report dated 11/9/2022 revealed .7:00 pm resident was given meds [medication] per MAR [Medication Administration Record]. 7:25 pm resident was seen going to the restroom in her room. At 7:45 pm door alarm sounded and alerted staff. Doors were checked quickly and staff discovered door that was sounding off. Nurse and CNA located resident outside of door and resident was brought inside .
Review of the timeanddate.com website revealed the weather on 11/9/2022 was a high of 70 degrees Fahrenheit (F) and a low of 61 degrees F.
Review of the Elopement/Wandering in-service conducted on 11/10/2022 revealed the facility educated 8 of 49 staff members.
Review of an Incident Report dated 11/15/2022 revealed .On 11/15/22, [Named Resident #6] exited the emergency door located in the dining room area around 11 pm. She was last seen sitting in front of the nurses station by staff. As staff was getting prepared to a round on patients, they noticed .[Named Resident #6] was no longer sitting at the nursing station and she wasn't in her room. Staff immediately took action to check all doors and [Named Resident #6] chair was located in front of dining room emergency exit door. She was located outside by the dumpsters and was brought inside .
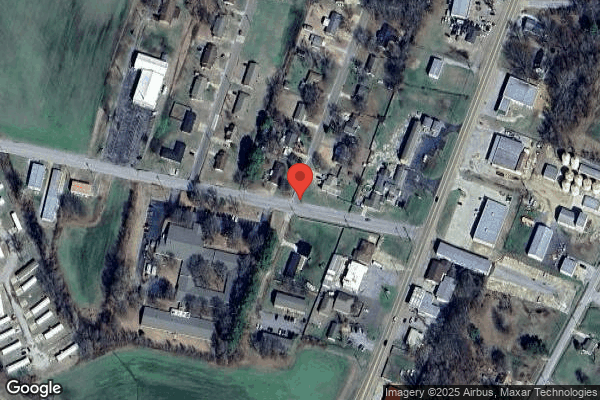
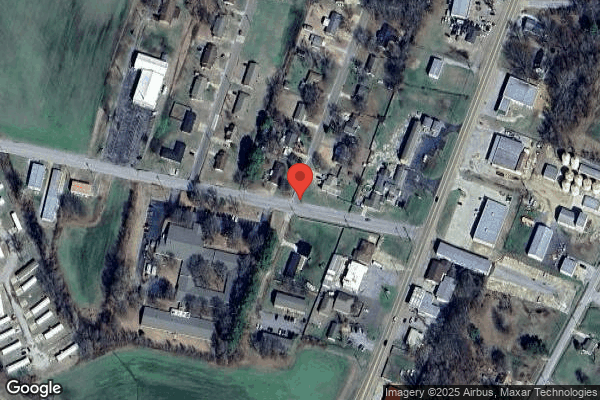
Observation outside of the facility on 1/5/2023 at 8:47 AM with the Maintenance Director revealed just outside the dining room exit door on the side of the facility was 3 large PVC (a type of plastic piping that is used in a variety of applications) pipes frames made for privacy screens, an old biohazard [NAME] with the broken wood on the bottom of the doors, 2 large barrels to the right of the biohazard [NAME] filled with dark greasy substance, and a milk crate to the left side of the biohazard [NAME]. There was an opening between service door and the biohazard [NAME] with 8 milk crates and trash lying on the ground, and 3 broken wooden pallets were lying up against the side of the biohazard [NAME]. On the back side of the biohazard [NAME] in front of boiler room, there was a lot of trash and debris including 5 (5) gallon buckets, 10 additional milk crates, a gray cart with trash and debris, and a wet cardboard box, 3 large trash cans filled with trash, and 8 wooden planks lying on the ground. The dumpster area had trash all over around the 2 trash bins, including part of a broken wooden pallet. One of the dumpsters had 2 of the lids open, the other dumpster was overflowing with trash. Across on a grassy area, an old air conditioner was lying on the ground. The grassy area lead to an open field that lead to a major highway.
Review of the timeanddate.com website revealed the weather on 11/15/2022 had a high temperature of 43 degrees F and a low of 41 degrees F.
The facility was unable to provide documentation Resident #6 was assessed by the Nurse Practitioner or the Medical Doctor post elopement on 11/9/2022 and 11/15/2022.
During an interview on 1/10/2023 at 7:55 AM, the Director of Nursing (DON) was asked if there was documentation the resident followed up with the Nurse Practitioner or Medical Director. The DON stated .No .I only have the one .
Review of Resident #6's Discharge to Nursing Facility Summary dated 11/22/2022, revealed .is transferring to a locked nursing facility r/t [related to] several attempted elopements .
During an interview on 1/4/2022 at 8:30 AM, the Maintenance Director was asked if he know of any residents getting out of the facility. The Maintenance Director stated .not to get out, but got the door open a time or two .
During a telephone interview on 1/4/2022 at 7:22 PM, CNA #6 was asked about Resident #6 getting out of the facility. CNA #6 stated .it was in November .I just arrived at work .went to the floor .noticed she was not there .I asked if anyone seen her .we knew she wandered a lot .we all started searching for her .we started in the building first .[Named CNA #7] found her wheelchair at the dining room door .found her outside .she was to the left of the parking lot past the dumpsters .she was sitting on the ground .she had her Bible and pullouts [briefs] .there were no alarms going off .that is another reason we did not know where she wandered to .she had on a shirt and black pants, shoes .it was cold outside .she was muddy .it was mostly on her pants .she was a little damp .we got her in the shower .she was cold to the touch .we let her warm up a little bit before putting her in the shower .
During an interview on 1/4/2023 at 7:36 PM, CNA #7 was asked about Resident #6 getting out of the facility. CNA #7 stated .she got out the exit door on the 500 Hall .she was right outside the door on the sidewalk . CNA #7 was asked if she saw Resident #6 exited the facility. CNA #7 stated No . CNA #7 was asked about Resident #6 getting out the dining room door. CNA #7 stated .[Named CNA #6] came in to work early .me and her was to do walking rounds .we passed her [Resident #6] room .[Named CNA #6] said where is [Named Resident #6] .notified the nurse .[Named CNA #6] went one way .I went another way .when I came back around I went looking in the dining room .her wheelchair was sitting in front of the exit door .we all went outside since it was dark .she was past the dumpsters .she was sitting down .got mud all over my new white shoes .we took the wheelchair out with us and put her in the wheelchair .brought her back inside .wrapped her in a blanket to warm up for a minute .gave her a shower since she was in the grass and the mud .she was just muddy .her shoes and pants where she was sitting on her butt .pack of briefs and her Bible had mud on it . CNA #7 was asked how long Resident #6 was outside. CNA #7 stated .we looked for her in the building for 5 minutes .
During an interview on 1/8/2023 at 10:57 AM, the Assistant Director of Nursing (ADON) confirmed in a statement Resident #6 was found approximately 150 feet from the dining room exit door.
During an interview on 1/9/2023 at 2:15 PM, LPN #2 was asked to explain how she checked wanderguard placement and the function. LPN #2 stated .I just check that it's on and clipped .put in the wheelchair and take it to the door . The LPN was asked which door she checked the wandgerguard with. LPN #2 stated .whatever door is the closest . LPN #2 was asked if she had been checking the function of the wanderguard. LPN #2 stated .No .
The facility only has one door equipped for the wanderguard system, which is the front door in the main lobby.
During a telephone interview on 1/11/2023 at 7:22 AM, Licensed Practical Nurse (LPN) #3 was asked about Resident #6 getting out of the facility. LPN #3 stated .the first time she got out, she exited the door on the 400 hall .the alarm sounded and we went to the door .she was right by the gate outside .it may have been 5 minutes . LPN #3 was asked if she saw Resident #6 exit the facility. LPN #3 confirmed she did not. LPN #3 was asked about Resident #6 getting out of the facility on 11/15/2022 through the dining room exit door. LPN #3 stated .she was not in her room .she went out the side dining room door .she was past the garbage cans back there .She left her chair [wheelchair] at the door entrance at the door she walked outside .when she came back in she .was cold .she was muddy on her knees from being on the ground .her knees were red when we took her pants off .it was from the coldness .they went back to the normal color .she was sitting on the ground .it was muddy .it had rained that day .it was cold that night .they took her to the shower .her hands was [were] muddy where she was trying to get up or something .Bible and pullouts [briefs] was [were] muddy .she had on blue jeans .sleeves that came to the elbow not long sleeves .church shoes .some socks on .she had mud on her shoes .she was shivering .she did not have on a jacket .we warmed her up first .then gave her a shower .we got her back to her room and she went to sleep .
During a telephone interview on 1/11/2023 at 7:51 AM, LPN #4 was asked if she could tell me how Resident #6 looked when she was brought back into the facility on [DATE]. LPN #4 stated .she was by the dumpsters .she was sitting on her bottom .in mud .it was muddy .she had on shirt and pants .had on shoes .her pants were muddy .her Bible and brief was muddy .
During a telephone interview on 1/11/2023 at 2:26 PM, CNA #6 was asked if she could tell me about Resident #6 elopement on 11/15/2022. CNA #6 stated .I did assist in getting her inside .they was getting her up off the ground .she had mud on pants leg and her hand .I know her Bible was muddy .I went to get her some new clothes to put on .because of the mud .took her to the shower .we did turn the heaters on .let the water warm up .I do remember her knees being red .no broken skin .I do remember her shoes were also muddy .I went to clean her shoes and bible with a Sani wipes .we gave her a shower .she wanted to go to bed .I went to the hopper room and cleaned them [Bible and shoes] .hands were cold to the touch .she was cold .it was cold for an older person .
4. Review of medical record revealed Resident #3 was admitted to the facility on [DATE], with a readmission date of 10/16/2022, with diagnoses of Alzheimer's Disease, Hypertension, Adult Failure to Thrive, History of Falls, and Anxiety Disorder.
Review of the quarterly MDS dated [DATE] revealed Resident #3 had a BIMS score of 3, which indicated severe cognition impairment, and wandering behavior was not coded.
Review of an Incident Report dated 12/20/2022 revealed, .This nurse was sitting at the nursing's station putting in orders, the CNA on duty came to the nurse's station and stated .[Named Resident #3] got out .The CNA stated that the resident's wheelchair was in front of the 200-hall door, and door had not shut completely behind resident .and the resident had exited on foot. The CNA said that she heard the alarm sounding at the 200-hall door when she went to check call lights, but there was no alarm sounding at the nurse's station, so I was unaware of the situation until alerted by said CNA. The resident was brought back in safely. She was wearing a shirt, sweater over the shirt, and winter coat, jogging pants, socks, and shoes. She had clothing with her (sweater and two shirts) and a bottle of coca cola. Resident was assessed. She stated 'I am looking for my momma and daddy .
Observation on the 200 and 300 Hall closed unit on 1/4/2022 at 8:50 AM when entering the 300 Hall closed unit there were double fire doors with a white box mounted on the door which had a 3 second chime when the door opened and closed. When entering the 200 Hall closed unit there were double fire doors and a white box mounted on the door which had a 3 second chime when the doors opened and closed
Observation on the 200 and 300 Hall closed unit on 1/9/2023 at 9:50 AM with Housekeeper #1 revealed several empty rooms used for storage open and unlocked on the 200 Hall closed unit, Biohazard Room locked, Laboratory Room that was unlocked with Covid testing supplies, isolation cart, a bucket of disinfectant wipes, bottle of hand sanitizer, hopper room unlocked. The 200 hall has a fire extinguisher hanging on the wall. The 200 hall and the 300 Hall had a nursing station in the middle of the two hall that had a medication cart, a fire extinguisher hanging on the wall next to the medication cart, and a metal storage rack. On the 300 Hall closed unit are offices for the Social Work, MDS Coordinator, ADON, Maintenance Director. Entering the 200 and the 300 Hall are double fire doors with a 3 second chime box.
Observation on the 300 Hall closed unit on 1/10/2023 at 8:00 AM with the Maintenance Director revealed a double fire door with the 3 second chime mounted to the doors.
Observation on the 300 Hall on 1/10/2023 at 3:40 PM revealed the Regional Maintenance Director was working on the double fire door installing new door alarms with key code.
During an interview on 1/10/2023 at 3:40 PM the Regional Maintenance Director was asked about the new door alarms. The Regional Maintenance Director stated, .replaced the chimes on the fire door leading to the 300 hall and the 200 hall closed unit .made so can't turn off .sound constant alarm till the code is reset .to help keep unauthorize people from getting back here .like the resident .
Observation outside the 200 Hall exit door on 1/13/2023 at 4:09 PM, revealed a concrete sidewalk leading to the apartments next door. The sidewalk had scattered pine needles and leaves. The end of the concrete sidewalk was covered with mud and leaves. At the end of the muddy sidewalk there was a dumpster running over with trash, and the parking lot for the apartments. To the left of the parking lot at the edge of the grassy area were 16 mailboxes mounted on 5 wooden frames. The apartment parking lot lead to a 2-lane road.
Review of the timeanddate.com website revealed the weather on 12/20/2022 with a high of 39 degrees F and a low of 36 degrees F.
During an interview on 1/4/2022 at 2:35 PM, CNA #7 was asked if she knew of any resident exiting the facility. CNA #7 stated .[Named Resident #3] .got out of back door on the 200 hall .There are no patients back there .It's behind closed double doors .seen wheelchair in front of the door .she was out of the wheelchair .it was dark .called nurse station for help .went outside . she was found at the mailboxes near the apartments .
During an interview on 1/4/2023 at 3:04 PM, CNA #11 was asked if he knew of any residents getting out of the facility. CNA #11 stated .which time .Not too long ago, the last time she [Resident #3] got out was mid-December .she managed to get herself out .she went through the double doors on the 200 hall .she went out the door and no one knew she left .the alarm did no go off at the desk .I was out on lunch .came back .[Named CNA #7] told me she got out .she was over by the mail boxes by the apartment .I feel like that was the second time she got out that day .
During a telephone interview on 1/4/2023 at 3:41 PM, LPN #7 was asked if she knew of any residents getting out of the facility. LPN #7 stated .it's been weeks ago .it was dark .that was not my hall .she [CNA #7] called to the nursing station .she said come help me get [Named Resident #3] . when I went back there .she [CNA #7] was bringing her [resident #3] back into the back door .on the end of 200 hall .that we are not using .
During a telephone interview on 1/4/2023 at 4:09 PM, LPN #6 was asked if she could tell me about the incident when Resident #3 got out of the facility. LPN #6 stated .I was on the hall doing my med [medication] pass .I came to the nursing station .[Named CNA #7] .told me she [Named Resident #3] had gotten out .
During a telephone interview on 1/5/2023 at 12:08 PM, the Nurse Practitioner (NP) was asked if she was aware the facility had 3 elopements. The Nurse Practitioner stated .I was not aware of all of them .I don't think they got past the parking lot .[Named Resident #3] .exited the building .[Named Resident #6] .I know she got out of the facility .The NP was asked if a resident was found outside unsupervised, was it considered safe. The NP stated .no unsupervised, it's not safe .
During a telephone interview on 1/5/2023 at 12:35 PM, the Medical Director was asked what he was told about the residents who eloped from the facility. The Medical Director stated .told one of them eloped from the side door, and one made it out of the building. [Named Resident #6] .the door was not working .alarm did not go off .[Named Resident #3] .she made it out, and the alarm did not go off .it was at night . The Medical Director was asked what he considered an elopement. The Medical Director stated .resident step out the structure unsupervised. That is an elopement, even if they step one foot out .have to be notified for that . The Medical Director was asked if a resident should be outside unsupervised and unattended, and if that was considered a safe area. Medical Director stated .No, ma'am it's not safe .
The facility neglected to adequately supervise Resident #3 and #6 to prevent incidents of elopement.
5. The surveyors verified the Removal Plan through review of in-services, audits, and conducting staff interviews.
a. The identified residents- Resident # 6 was placed on 1:1 supervision on 11/15/2022 until discharge to a locked unit on 11/22/2022. The surveyor confirmed with recorded review and interviews.
b. On 11/15/2022 the charge nurse checked the door the resident exited and noted the alarm was manually disabled, staff stayed at the door until the maintenance director was contacted and gave instruction on how to re-engage the alarm. The surveyor confirmed with interviews.
c. The Charge Nurse checked the function of all exit doors and found no other concerns on 11/15/2022. The surveyor confirmed with interviews.
d. The facility completed an investigation of the event occurring on 11/15/2022 and determined the root cause to be that the alarm was manually disabled by the Maintenance Director to bring furniture in and out of the dining room and was not turned back on. The surveyor confirmed with interviews.
e. The Maintenance Director was re-educated on door alarms need to be engaged at all times on 11/16/2022 by the Administrator. The surveyor confirmed with interviews.
f. The identified Resident #3 was placed on 1:1 supervision on 12/20/2022 until door repair on 12/21/2022. The door was monitored by assigned staff starting on 12/20/2022 until repaired on 12/21/2022 by the Regional Maintenance Director. The surveyor confirmed with interviews.
g. The Administrator checked the function of all exit doors on 12/20/2022 and found all to be functioning except the door identified with a broken wire to the sensor. The door was secured but the alarm was not audible at the nurse's station. The door was being monitored by staff until repair on 12/21/2022. The surveyor confirmed with interviews and record review.
h. Investigation was completed and root cause determined to be a broken sensor wire leading to the annunciator which did not alarm at the nurse's station. Further investigation revealed condensation had caused the molding that was holding the wire, to pull away from the wall resulting in wires pulling away from the alarm box and not sounding at the nurse's station. The surveyor confirmed with interviews.
i. Facility exit doors were checked for function 5 x (times) week by the maintenance Director ongoing as well as 7 x week by the Administrator for 2 weeks. The surveyor confirmed with interviews and audits.
j. Cognitively impaired residents with wandering behaviors are placed with a wanderguard bracelet to alert the facility of the resident exiting to any area that is not secured or alarmed. The surveyor confirmed with interviews.
k. Resident #6 was last seen at approximately 10:40 PM, during staff rounds and was located at 11:00 PM. Resident #3 was last seen at approximately 5:10 PM and located at 5:18 PM. The surveyor confirmed with interviews.
l. On 11/16/2022 all exit alarms were inspected by the Maintenance Director and the ability to disengage the alarm was removed making all alarms unable to be disengaged. On 11/16/2022 all exit alarms were checked and found to be functioning by the Maintenance Director and the ability to disengage alarms was removed from all exit doors on 11/16/2022 by the Maintenance Director. The surveyor confirmed with interviews.
m. On 11/17/2022 the Interdisciplinary Team (IDT) completed a review of all current residents to identify any that were at risk of elopement. Any at risk of elopement had a review of their wanderguard orders to verify functioning is checked daily by the licensed nurses and care plans to determine if the care plan was appropriate to meet the safety and supervision needs of the resident. Any needed corrections were made at that time. Cognitively impaired residents with wandering behaviors are assessed to determine the risk of elopement and based on risk factors a care plan is developed to provide safety without restriction of movement and quality of life. Interventions and supervision level is based on risk factors and resident needs and are resident specific. The surveyor confirmed with interviews.
n. On 12/21/2022 the IDT completed a review of all current residents to identify any that were at risk of elopement. Any at risk of elopement had a review of their wander guard orders to verify functioning is checked daily by the licensed nurses and care plans to determine if the care plan was appropriate to meet the safety and supervision needs of the resident. Any needed corrections were made at that time. Cognitively impaired residents with wandering behaviors are assessed to determine the risk of elopement and based on risk factors a care plan is developed to provide safety without restriction of movement and quality of life. Interventions and supervision level is based on risk factors and resident needs and are resident specific. The surveyor confirmed with interviews.
o. On 12/21/2022 all exit door alarms were checked by the Maintenance Director and Regional Maintenance Director with no concerns identified. A Specialty tape was applied to all wiring of exit alarms to prevent dislodgement of condensation on 12/21/2022 by the Maintenance Director and Regional Maintenance Director. The surveyor confirmed with interviews and observation.
p. Resident # 6, Beginning on 11/16/2022 facility staff were re-educated on the Unsafe Wandering and Elopement Prevention.
On 11/16/2022 the ability to disengage all alarms on exit doors was removed by the Maintenance Director. The surveyor confirmed with interviews.
q. Resident # 3, Beginning 12/20/2022 facility staff were re-educated on the elopement policy by the DON (Director of Nursing) or designee with no staff working after 12/20/2022 without having had this re-education. The surveyor confirmed with interviews.
r. Beginning 11/15/2022 and ongoing door functionality will be checked 5 x per week for functionality by the Maintenance Director. The surveyor confirmed with interviews.
s. Beginning 12/21/2022 The Administrator or designee will check door functionality 3 x per week for two weeks. The surveyor confirmed with interviews.
t. Beginning 11/21/2022 the Administrator or Designee conducted elopement drills monthly on random shifts with all shifts having at least one drill per quarter. Drills were conducted on 11/21/2022 second shift, 12/1/2022 day shift and 1/5/2023 on day shift by the Administrator. All staff present in the facility at the time of the drill participate. The surveyor confirmed with interviews and record review.
u. An adhoc (as needed) QA (Quality Assurance) Committee meeting was held on 11/17/2022 to review the actions taken after the 11/15/2022 event and again on 12/21/2022 which included the Medical Director, DON, Administrator, ADON (Assistant Director of Nursing)/ Infection Control Nurse and Department Heads. The surveyor confirmed with interviews.
v. On 1/9/2022 an ad [NAME] QA Committee meeting was held to review the past noncompliance as well as the IJ citations and abatement plan/ plan of correction. The Medical Director, DON, Administrator, ADON/ Infection Control Nurse and Department Heads were in attendance. The surveyor confirmed with interviews.
w. The Administrator/Designee will review results of the door checks with the QA Committee monthly for three months or anytime concerns are identified for further recommendations as needed. The surveyor confirmed with interviews.
The facility's noncompliance of F-600 continues at a scope and severity of D for monitoring the effectiveness of the corrective actions.
The facility is required to submit a Plan of Correction.
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Investigate Abuse
(Tag F0610)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, job description review, medical record review, observation and interview the facility failed to thorough...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, job description review, medical record review, observation and interview the facility failed to thoroughly investigate 3 incidents of elopement for 2 of 5 sampled residents (Resident #3 and #6) reviewed for elopement and wandering. The facility's failure to thoroughly investigate an incident of elopement resulted in Immediate Jeopardy when 2 vulnerable residents with severe cognition impairment exited the building without authorization or staff supervision. Resident #3 exited the facility on 2 separate occasions, 6 days apart, and Resident #6 exited the building in cold weather without authorization or staff supervision. The facility failure to thoroughly investigate the incidents of elopement resulted in immediate Jeopardy.
Immediate Jeopardy (IJ) is a situation in which the provider's noncompliance with one or more requirements of participation has caused, or is likely to cause, serious injury, harm, impairment, or death to a resident.
The Administrator, Director of Nursing and the Regional Director of Operation were notified of the Immediate Jeopardy (IJ) for F-610 during the complaint investigation on 1/9/2023 at 4:40 PM, in the Conference Room.
The facility was cited at F-610 at a scope and severity of J, which is Substandard Quality of Care.
The Immediate Jeopardy existed from 11/9/2022 through 1/16/2023.
An acceptable Removal Plan, which removed the immediacy of the jeopardy, was received on 1/9/2023 at 10:53 AM, and was validated onsite by the surveyors on 1/17/2023 through observations, review of audits, meeting minutes, and staff interviews.
The findings include:
1. Review of the facility's policy titled, Abuse, Neglect and Exploitation, revised 10/24/2022, revealed .It is the policy of this facility to provide protections for the health, welfare, and rights of each resident by developing and implementing written policies and procedures that prohibit and prevent abuse neglect .Neglect .means failure of the facility, its employees, or service providers to provide goods and services to a resident that are necessary to avoid physical harm, pain, mental anguish, or emotional distress .The facility will designated and Abuse Prevention /Coordinator in the facility who is responsible for reporting allegations or suspected abuse, neglect .to the state survey agency .Investigation of alleged Abuse, Neglect .Identifying and interviewing all involved persons .witnesses .others who might have knowledge of the allegations .Provide complete and thorough documentation of the investigation .Reporting of all alleged violation to the Administrator, state agency, adult protective services .within specified timeframes .Immediately, but not later than 2 hours after the allegations is made, if the events that cause the allegation involve abuse .
Review of the facility's policy titled, Incidents and Accidents Reporting, revised 8/11/2022, revealed .It is the policy of this facility for staff to utilize electronic and /or approved forms to report, investigate and review any accidents or incidents that occur or allegedly occur, on facility property and may involve or allegedly involved a resident .An 'incident' is defined as an occurrence or situation that is not consistent with the routine care of a resident or with the routine operation of the organization .The purpose of incident reporting is .Assure that appropriate and immediate interventions are implemented and corrective actions are taken to prevent recurrences and improve the management of resident care .Incident/accident reports will be reviewed by the QAPI committee on a routine basis to be analyzed. Analysis may include, for example, considering the severity of hazard, the immediacy of risk, and trends such as time of day, location .Incidents that rise the level of abuse .neglect .will be managed and reported according to the facility's abuse prevention policy .The following incidents/accidents require an incident/accident report but are not limited .Elopement .The nurse will notify the resident's practitioner to inform them of the incident/accident .The resident family or representative will be notified of the incident/accident .The nurse .will enter the incident/accident information into the appropriate form/system within 24 hours of occurrence and will document all pertinent information .Documentation should include the date, time, nature of the incident, location, initial findings, immediate interventions, notifications .follow-up interventions .obtain the witnesses' account .
Review of the facility's policy titled, Unsafe Wandering & [and] elopement Prevention, revised 1/1/2022, revealed .Every effort will be made to prevent unsafe wandering and elopement episodes .Should an elopement .occur, the contributing factors, as well as the interventions' tried, will be documented on the nurses' notes .upon return of the resident to the facility, the Director of Nursing Services or charge Nurse should .examine the resident for injuries .Contact the Attending Physician and report what happen .Contact the resident's responsible party and inform him/her of the incident .file incident report .Complete an Elopement assessment .Should an employee discover that a resident is missing from the facility .The Licensed nurse will assign a staff member to begin a head count of all residents .Assign staff to conduct and interior search of the facility .conduct and exterior search of the facility .The Licensed nurse will also .Contact .Responsible Party .Validated the head count is accurate and all residents are accounted for .
2. Review of the facility's Director of Nursing Job description signed 9/26/2022, revealed .Manages the facility nursing program in accordance with the Nurse Practice Act, applicable State and Federal regulations, and policies and procedures .Round on unit at least once daily .Manage the Nursing Department with the goal of achieving and maintaining the highest quality of care .Identification of training needs .Assures that all clinical protocols and nursing policies and procedures are followed .Assumes complete responsibilities for the Center in absence of Administrator .
3. Review of medical record revealed Resident #6 was admitted to the facility on [DATE], with diagnoses of Parkinson's Disease, Osteoarthritis, Major Depression, Chronic Obstructive Pulmonary Disease, Repeated Falls, and Hypertension.
Review of the Care Plan initiated on 7/2/2022 revealed, .The resident is at risk for falls related to History of falls .Provide for .transfers .ambulation .
Review of the Care Plan initiated 7/5/2022 revealed, .The resident is an elopement risk/a wanderer/wants to go home .11/9/2022, resident attempted to leave facility .11/15/2022, resident attempted to leave facility .
Review of the Progress Notes dated 7/5/2022, 7/15/2022, 7/20/2022, and 7/27/2022 revealed, .Behavior .wandering/exit seeking .
Review of the Progress Note dated 9/1/2022 revealed, .Resident was out of chair and started to open the door on 400 east. Nurse was present and stopped resident .
Review of the quarterly Minimum Data Set (MDS) dated [DATE] revealed Resident #6 had a Brief Interview for Mental Status (BIMS) score of 4, which indicated severe cognition impairment, and wandering behavior was not coded.
Review of the Progress Note dated 10/23/2022 revealed, .Resident wandering throughout evening shift. Resident attempted to exit facility x [times] 2 .
Review of an Incident Report dated 11/9/2022 revealed, .7:00 pm resident was given meds [medication] per MAR [Medication Administration Record]. 7:25 pm resident was seen going to the restroom in her room. At 7:45 pm door alarm sounded and alerted staff .Nurse and CNA [Certified Nursing Assistant] located resident outside of door and resident was brought inside .
Review of the Progress Note dated 11/9/2022 revealed, .On 11/9/2022, [Named Resident #6] was last seen in her room going to the restroom by the nurse. At 7:40 [7:40 PM], door alarmed sounded .Resident was located outside of 300/400 [400 East] hall side emergency door .Resident was brought inside and to her room .
Review of the timeanddate.com website revealed the weather on 11/9/2022, had a high temperature of 70 degrees Fahrenheit (F) and a low of 61 degrees.
Review of the witness statements dated 11/9/2022 revealed, .[Named CNA #7] was charting in the conference room when I heard a door alarm go off .I preceded to check outside and [Named Resident #6] was outside in her wheelchair with a gown and shoes on .last time I had seen the resident before the incident was in the hallway by her room around 7:35 [PM] .Resident found outside at 7:45 [PM] .
The facility provided 4 witness statements; one from Licensed Practical Nurse (LPN) #3, CNA #7, CNA #13 and CNA #14.
The facility's investigation had no other interviews with other staff members to ensure there were no other incidents.
Review of the RECORD OF IN-SERVICE dated 11/10/2022 revealed, .We need to treat exit seeking as an incident when they are exit seeking or attempting to exit the building .Immediate intervention needs to be in place .activities specific to resident .Psych [psychiatric] consult .Medication review if other haven't worked .
Review of the In-service signature sheets dated 11/10/2022, revealed 8 of 49 nursing staff members were in-serviced on elopement and wandering and the need to treat exit seeking as an incident.
During an interview on 1/9/2023 at 2:31 PM, CNA #7 was asked where Resident #6 was found. CNA #7 stated .she was found outside in her wheelchair sitting on the concrete patio .
Review of the Progress Note dated 11/15/2022 revealed a second incident of Resident #6 exiting the building unsupervised, .11/15/22, at 10:40 pm, [Named Resident #6] was last seen in front of the nurses station. Staff went to start doing a round on resident care and observed that [Named Resident #6] was no longer sitting at the nurse station and she wasn't in her room. Around 11 pm [11:00 PM], we .discovered [Named Resident #6] wheelchair in front of the dining area emergency exit. Chair alarm was in place but was removed by resident. [Named Resident #6] was found near dumpsters on side of building .
Review of an Incident Report dated 11/15/2022 revealed, .On 11/15/22, [Named Resident #6] exited the emergency door located in the dining room area around 11 pm [11:00 PM]. She was last seen sitting in front of the nurses station by staff. As staff was getting prepared to a round .they noticed .[Named Resident #6] was no longer sitting at the nursing station and she wasn't in her room .[Named Resident #6] chair was located in front of dining room emergency exit door. She was located outside by the dumpsters and was brought inside .
Review of the Progress Notes dated 11/17/2022 revealed, .Increased episodes of wandering/exit seeking .
On 11/15/2022, Resident #6 had eloped from the facility and was found outside sitting on the ground in mud. There was no fall incident report documented or fall assessment completed.
Review of the timeanddate.com revealed the weather on 11/15/2022, had a high temperature of 43 degrees F and a low of 41 degrees.
The investigation failed to document Resident #6's condition when found outside sitting on the ground. The resident was not evaluated by the Medical Doctor or the Nurse Practitioner after being found outside in 41-degree weather sitting in the mud and shivering.
The facility's investigation had no other interviews with other staff members to ensure there were no other incidents. The incident of elopement was not reported to the State Agency or APS during the time of the elopement. APS was not notified until 1/9/2023. The facility provide statements from LPN #4 and CNA #13 that were undated.
During a telephone interview 1/6/2023 at 12:00 PM, Resident #6's daughter confirmed she visited the facility 11/17/2022 and was not notified of her mother's (Resident #6) elopement from the facility on 11/15/2022. The daughter stated she was not aware until the facility called her on 11/18/2022 and informed her that her mother would need to be discharged to another facility.
Review of the 24 HOUR REPORT/CHANGE OF CONDITION REPORT dated 11/20/2022 revealed, .[Name Resident #6] Exit Seeking all night .
Review of the inservices dated 11/14/2022, revealed 10 nursing staff members were inserviced on the Fall Protocol, 9 LPN's and one Registered Nurse (RN). The facility had an average of 46-49 total staff members.
Review of the Discharge to Nursing Facility Summary dated 11/22/2022, revealed .is transferring to a locked nursing facility r/t [related to] several attempted elopements .
During an interview on 1/4/2023 at 7:03 PM, LPN #3 confirmed Resident #6 exited the facility and was found outside past the garbage dumpsters. LPN #3 confirmed she did not see Resident #6 exit the facility.
During an interview on 1/4/2023 at 7:36 PM, CNA #7 confirmed Resident #6 had exited the facility twice in the month of November and was found outside. CNA #7 confirmed she did not see Resident #6 exit the facility.
4. Review of the medical record revealed Resident #3 was admitted to the facility on [DATE] with a readmission date of 10/16/2022 and had diagnoses of Alzheimer's Disease, Hypertension, Adult Failure to Thrive, History of Falls, and Anxiety Disorder.
Review of the quarterly MDS dated [DATE] revealed Resident #3 had a BIMS of 3, which indicated severe cognition impairment, and wandering behavior was not coded.
Review of the Care Plan revised 11/30/2022 revealed, .Resident will not exit facility unaccompanied by staff or family .Documents wandering behavior .1/7/2021 .distract from wandering by offering pleasant diversion .1/7/2021 .WANDER ALERT .wander guard-check function .
Review of an Incident Report dated 12/20/2022 revealed, .This nurse was sitting at the nursing's station putting in orders, the CNA on duty came to the nurse's station and stated .[Named Resident #3] got out .200 hall .The CNA stated that the resident's wheelchair was in front of the 200-hall door, and door had not shut completely behind resident .resident had exited on foot. The CNA said that she heard the alarm sounding at the 200-hall door when she went to check call lights, but there was no alarm sounding at the nurse's station, so I was unaware of the situation until alerted by said CNA. The resident was brought back in .wearing a shirt, sweater over the shirt, and winter coat, jogging pants, socks, and shoes. She had clothing with her (sweater and two shirts) and a bottle of coca cola. Resident was assessed. She stated I am looking for my momma and daddy .
Review of the Nursing Home Progress Notes completed by the Medical Director dated 12/30/2022 revealed no documentation or mention of the resident's elopement on 12/20/2022.
Review of witness statement dated 12/20/2022 revealed, .[Named CNA #7] .heard .exit door going off .[Named Resident #3] had went outside .brought her inside .incident happened at 5:18 pm last seen at 5:10 [5:10 PM] .
The facility failed to obtain witness statement on all shifts. The facility obtained witness statements from LPN #6 and CNA #7 on 12/20/2022.
The facility provided in-services to 20 staff members on 12/26/2022 on the elopement education and respond to missing resident. The facility had an average of 46-49 staff members.
Review of the Incident report did not identify where the resident was found, or measurement of the resident's distance traveled. The resident was not placed on 1:1 observation until 12/20/2022 at 8:00 PM, more than 2 and a half hours after the elopement incident.
Review of the Committee Agenda/Minutes Ad-hoc dated 12/21/2022, revealed .doors will be checked 5 times a week by Maintenance Director and 3 times a week for 2 weeks by the Administrator for functionality and visually for wiring .Resident will remain 1:1 until appropriate intervention is in place and effective .Wanderguards were check [checked] for functionality .reports were pulled to verify that wanderguards had been checked appropriately .
The Administrator provided a floor plan of the facility with the exit doors circled and no dates documented when the doors and wires were checked. The Maintenance Director was unable to provide documentation of the wanderguards being checked in TELS (is a technology-based system for delivering life safety, asset management, maintenance, and repair services to building management professionals) system.
Review of second Incident report for resident #3 dated 1/14/2023 revealed, .Resident sitting with this nurse at the nurses station while nurse was charting assessment. The door alarm starting going off and this nurse looked up and saw it was where the smokers were going out the .Courtyard door. Within a few seconds the alarm got louder, and this nurse looked up to see the Front door alarm going off. I looked around and resident wasn't sitting behind me. I ran around the desk and saw resident sitting in the vestibule in her wheelchair with her hands on the door. The door didn't open. Resident was still in her wheelchair covered up with the blanket she had been covered up in most of the morning .
The Administrator provided a floor plan of the facility with the exit doors circled and no dates documented when the doors and wires were checked. The Maintenance Director was unable to provide documentation of the wanderguards being checked.
During an interview on 1/4/2023 at 5:28 PM and 1/12/1023 at 4:24 PM, the Director of Nursing (DON) was asked if she got statements from the staff members. The DON stated, .only the 2 statement .one from LPN #6 and CNA #7 .they were the ones taking care of the resident [Resident #3] . The DON confirmed she should have gotten statements on all shifts.
Review of the IN-SERVICE ATTENDANCE RECORD SIGNATURE SHEET dated 1/9/2023 revealed LPN #3, #2, #3 and #4 were in-serviced on how to check wanderguaurd function. During the investigation LPN #2 confirmed she was not checking the wanderguard functioning, just the placement.
During an interview on 1/4/2022 at 2:35 PM, CNA #7 was asked if she knew about any residents exiting the facility. CNA #7 stated .[Named Resident #3] .got out of back door on the 200 hall .there are no patients back there [200 hall close unit] .It's behind closed double doors .goes to the 200 hall .seen wheelchair in front of the door .she was out of the wheelchair .it was dark .called nurses station for help .
During a telephone interview on 1/4/2023 at 4:09 PM, LPN #6 confirmed Resident #3 exited the facility on 12/20/2022, and was found by staff outside.
During an interview on 1/4/2023 4:45 PM, the Assistant Director of Nursing (ADON) was asked about Resident #3's elopement. The ADON stated .I was at home .got phone call at 7 pm .I asked what type clothes she had on .when was the last time staff seen her .was 5:10 PM .found at 5:18 PM .that what I was told .did staff write statements .[Named Administrator] .notify everyone .MD, RP, the Administrator and DON .called the Maintenance Director to check the door .make sure it was fixed .he beat me here .I went to the door .he [Named Maintenance Director] could not get it to work .it was alarming at the door .but not the nursing station .sensor at the top of the door the wire was hanging out of it .there was some construction men going in and out the door .4 hours the day prior to the event .[Named Maintenance Director] fixed the box in house .It was in December before Christmas .we have a trigger system event for abuse .injury of unknown origin .I was told a resident getting out of the building is not a reportable event . The ADON confirmed the incidents of elopement were not reported to the State Survey Agency (SSA).
During an interview on 1/4/2023 at 5:29 PM the Administrator was asked about the elopement on 12/20/2022. The Administrator stated .I got phone call at around 7:30-7:50 PM .they had her back in the building .the door did not alarm .that was the root cause .we did not report it .it was not required for use to report an elopement . The Administrator was asked if the staff members called a code. The Administrator stated .I don't know if they did .checked .head count .they did not put it on a form .when have elopement .we do a head count .we don't document anything .we have such a small building .
During an interview on 1/10/2023 at 9:21 AM, the Social Service Director was asked what her roll was when the facility has an elopement. The Social Service Director stated .I put them on standards of care [SOC] a QA [quality assistance] tool for behavior and monitor them for 4 weeks .the one on [Named Resident #3] .I did not know she got out the building .[Named Resident #6] .with her we started working on placement .we had her on for behaviors after first incident .her family had told me when admitted she wandered at night looking for her husband .so when she had her elopement add her to the SOC .looking for patterns and intervention those kind of thing .
Review of the Quality Assistance Form, review of the forms form June 2022 through January 2023 revealed no documentation of Resident #3 and #6 wandering behaviors.
During an interview on 1/12/2023 at 4:24 PM, the Director of Nursing (DON) was asked whose responsibility it was to update the care plan interventions. The DON stated .any nurse can go and update the care plan .should update the care plan if the resident had a change . The DON was asked what intervention was in place for each of the elopements. The DON stated .I don't remember without looking through everything . The DON was asked if all direct care staff members should have been educated. The DON stated .this was for just the nursing for intervention to put in place . The DON was asked if the CNAs were educated on the interventions. The DON stated .No .
The DON was asked if a resident is found outside the facility would that be considered an elopement. The DON stated .we were not told she was outside, the nurse called [Named LPN #3] .she was not outside, and that is why we did not start a full investigation. We were told she was not outside, her chair was at the door . The DON stated .when I came in the next morning .reviewed the statements .talked with them .it was confusing . The DON was asked about asking the other staff members. The DON stated .yes .we should have talked to everyone who worked . The DON was asked if the Medical Doctor or NP followed up with Resident #3 or #6. The DON stated No . The DON was asked if a resident was found on the ground, what did she expect the staff to document. The DON stated .should have done an incident report if they had a fall .had them complete another unwitnessed fall .fall assessment .pain assessment .vital signs . The DON was asked if the interventions put in place were effective with the 3 elopements. The DON stated .There is room for improvement .
Review of the facility's investigation revealed the facility did not complete a thorough investigation for the incidents of elopement There were no written statements from nurses or staff providing direct care to the resident on the previous shifts.
The facility was unable to provide documentation a head count was done according to policy after the searches for the missing residents.
Refer to F-600, F-610, and F-689.
5. The surveyors verified the Allegation of Compliance (AoC) Removal Plan through review of education and sign-in sheets, observations, and interviews for the immediate corrective actions listed below:
a. The identified residents- Resident # 6 was placed on 1:1 supervision on 11/15/2022 until discharge to a locked unit on 11/22/2022. The facility completed an investigation of the event and determined the root cause to be that the alarm was manually disabled by staff to bring furniture in and out of the dining room and was not turned back on. Staff responsible was re-educated on door alarms need to be engaged at all times on 11-16-2022 by the Administrator. The surveyor confirmed by interviews and observations.
b. Resident #3 was placed on 1:1 supervision on 12/20/2022 until door repair on 12/21/2022. Door was monitored by staff starting on 12/20/2022 until repaired on 12/21/2022 by the Regional Maintenance Director. An Investigation was completed, and root cause determined to be a broken sensor wire leading to the annunciator which did not alarm at the nurse's station. Further investigation revealed condensation had caused the molding that was holding the wire, to pull away from the wall resulting in wires pulling away from the alarm box and not sounding at the nurse's station. The surveyor confirmed by interviews and observations.
c. The Administrator on 1/9/2023 completed a review of the risk management events in the past 30 days to determine if any other elopements had occurred without investigation and no other elopements were noted to have occurred. The surveyor confirmed by interviews.
d. The Administrator reviewed on 1/9/2023 all investigations of abuse and neglect in the past 30 days to determine if any lacked investigation or statements and no concerns were identified. The surveyor confirmed by interviews.
e. On 1/9/2023 the VP (Vice President) of Clinical Services completed education with the Administrator and Director of Nursing on investigating including root cause analysis and identifying and interviewing involved persons including the alleged victim, alleged perpetrator, witnesses, and others who might have knowledge of the allegations. The surveyor confirmed by interviews.
f. The Administrator of Designee will review any allegations of abuse or neglect weekly x (times) 8 weeks to validate a thorough investigation with root cause analysis and appropriate witness statements. Results of the reviews will be presented to the QA (Quality Assurance) Committee monthly x 2 months or anytime concerns are identified for further recommendations as needed. The surveyor confirmed by interviews.
g. On 1/9/2023 an ad hoc (as needed) QA Committee meeting was held to review the past noncompliance as well as the IJ citations and abatement plan/plan of correction. The Medical Director, DON, Administer, ADON/Infection Control Nurse and Department Heads in attendance. No further recommendations were made. The surveyor confirmed by interviews and observation.
The facility's noncompliance of F-610 continues at a scope and severity of D for monitoring the effectiveness of the corrective actions.
The facility is required to submit a Plan of Correction.
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, job description review, review of facility investigations, review of dateandtime.com website, medical re...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, job description review, review of facility investigations, review of dateandtime.com website, medical record review, observation, and interview, the facility failed to ensure a safe environment to prevent 3 incidents of elopement for 2 of 5 sampled residents (Resident #3 and #6) reviewed for elopement and wandering behaviors; and failed to ensure fall interventions were implemented for 3 of 6 sampled residents (Resident #2, #3, and #5) reviewed for falls. The facility's failure to ensure a safe environment resulted in Immediate Jeopardy when Resident #3 and Resident #6, vulnerable residents with severe cognition impairment, exited the building without authorization or staff supervision. Resident #3 eloped from the facility through a malfunctioning exit door on the 200 hall and walked 75 feet in 36-degree Fahrenheit (F) weather to a nearby apartment complex's mailboxes. Staff were unaware of Resident 3's location for an undetermined amount of time. The mailboxes were 155 feet from a busy 2-lane road. Resident #6 exited the facility unsupervised and without staff knowledge on 2 separate occasions, 6 days apart. On 11/9/2022, Resident #6 exited the building without authorization or staff supervision through the 400 hall exit door in 61 degree F weather and was found on the patio approximately 8-10 feet from the exit door. On 11/15/2022, Resident #6 exited the building through a malfunctioning exit door in the dining room and walked 150 feet in 41-degree F weather to the back of the building near the dumpsters without supervision and was found sitting on the ground in mud. The staff were unaware of Resident 6's location for an undetermined amount of time. The exit door was 88 feet from the busy 2-lane road. The 200 hall, 400 hall, and the dining room doors did not have a wanderguard monitoring system in place.
Immediate Jeopardy (IJ) is a situation in which the provider's noncompliance with one or more requirements of participation has caused, or is likely to cause, serious injury, harm, impairment, or death to a resident.
The Administrator, Director of Nursing and the Regional Director of Operation were notified of the Immediate Jeopardy (IJ) for F-689 during the complaint investigation on 1/9/2023 at 4:40 PM, in the Conference Room.
The facility was cited Immediate Jeopardy at F-689.
The facility was cited F-689 at a scope and severity of J, which is Substandard Quality of Care.
The Immediate Jeopardy existed from 11/9/2022 through 1/16/2023.
A partial extended survey was conducted from 1/10/2023 through 1/13/2023.
A Removal Plan which removed the immediacy of the jeopardy was received on 1/12/2023 at 9:03 PM, and was validated onsite by the surveyors on 1/17/2023 through review of inservice education, root cause analysis review, review of audit tools, review of QAPI minutes, Interdisciplinary Team (IDT) meeting minutes, and staff interviews on all shifts.
The findings include:
1. Review of the facility's policy titled, Fall Prevention Program, revised 1/1/2022 revealed, .Each resident will be assessed for the risk of falling and will receive care and services in according with the level of risk to minimize the likelihood of falls .upon admission the nurse will indicate the resident's fall risk and initiate interventions on the resident's baseline care plan, in accordance with the resident's level of risk .When a resident who does not have a history of falling experiences a fall, the resident will be placed on the facility's Fall Prevention Program .Each resident's risk factors and environmental hazards will be evaluated when developing the resident's comprehensive plan of care .When any resident experiences a fall, the facility will .Assess the resident .complete a post-fall assessment .complete an incident report .Notify physician and family .Review the resident's care plan and update as indicated .Document all assessments and actions .Obtain witness statements in the case of injury .
Review of the facility's policy titled, Incidents and Accidents Reporting revised 8/11/2022 revealed, .It is the policy of this facility for staff to utilize electronic and /or approved forms to report, investigate and review any accidents or incidents that occur or allegedly occur, on facility property and may involve or allegedly involved a resident .An incident is defined as an occurrence or situation that is not consistent with the routine care of a resident or with the routine operation of the organization .The purpose of incident reporting is .Assure that appropriate and immediate interventions are implemented and corrective actions are taken to prevent recurrences and improve the management of resident care .The following incidents/accidents require an incident/accident report but are not limited .allegations of abuse .Elopement .The nurse will notify the resident's practitioner to inform them of the incident/accident .The resident family or representative will be notified of the incident/accident .The nurse .will enter the incident/accident information into the appropriate form/system within 24 hours of occurrence and will document all pertinent information .Documentation should include the date, time, nature of the incident, location, initial findings, immediate interventions, notifications .follow-up interventions .obtain the witnesses' account .
Review of the facility's policy titled, Unsafe Wandering & [and] elopement Prevention revised 1/1/2022 revealed, .Every effort will be made to prevent unsafe wandering and elopement episodes .Should an elopement .occur, the contributing factors, as well as the interventions' tried, will be documented on the nurses' notes .upon return of the resident to the facility, the Director of Nursing Services or charge Nurse should .examine the resident for injuries .Contact the Attending Physician and report what happen .Contact the resident's responsible party and inform him/her of the incident .file incident report .Complete an Elopement assessment .Should an employee discover that a resident is missing from the facility, he/she should .The Licensed nurse will assign a staff member to begin a head count of all residents .Assign staff to conduct and interior search of the facility .conduct and exterior search of the facility .The Licensed nurse will also .Contact .Responsible Party .Validated the head count is accurate and all residents are accounted for .
2. Review of the facility's signed Administrator Job Description signed 12/1/2015 revealed, .Responsible for the efficient and profitable operation of the facility, facility compliance with .Stated and Federal rules and regulations, and providing the highest quality of care possible .Manages the day-today operation of the facility Implements control systems to ensure accountability of all departments .Ensures all employees receive orientation and ongoing training to meet the quality goals of the organization .Knowledge of Long term Care and Medicare and Medicare regulations and standards .
Review of the facility's signed Director of Nursing Job description signed 9/26/2022 revealed, .Manages the facility nursing program in accordance with the Nurse Practice Act, applicable State and Federal regulations, and policies and procedures .Round on unit at least once daily .Manage the Nursing Department with the goal of achieving and maintaining the highest quality of care .Identification of training needs .Assures that all clinical protocols and nursing policies and procedures are followed .Assumes complete responsibilities for the Center in absence of Administrator .
3. Review of medical record revealed Resident #6 was admitted to the facility on [DATE] with diagnoses of Parkinson's Disease, Osteoarthritis, Major Depression, Chronic Obstructive Pulmonary Disease, Repeated Falls, and Hypertension.
Review of the quarterly Minimum Data Set (MDS) dated [DATE] revealed Resident #6 had a Brief Interview for Mental Status (BIMS) score of 4, which indicated severe cognition impairment, and wandering behavior was not coded.
Review of the Progress Note dated 9/1/2022 reveale,d .Resident was out of chair and started to open the door on 400 east. Nurse was present and stopped resident .
Review of the 24 HOUR REPORT/CHANGE OF CONDITION REPORT dated 9/29/2022, 10/10/2022, and 10/16/2022 revealed, .[Named Resident #6] wandering .
Review of the 24 HOUR REPORT/CHANGE OF CONDITION REPORT dated 10/21/2022 revealed, .[Name Resident #6] Exit Seeking .
Review of the Progress Note dated 10/23/2022 revealed, .Resident wandering throughout evening shift. Resident attempted to exit facility x2 [times 2]. Resident became combative with CNA [Certified Nursing Assistant] multiple times, scratching, pinching and raising her hand to slap can [Certified Nursing Assistant]. Resident redirected several times .
Review of the 24 HOUR REPORT/CHANGE OF CONDITION REPORT dated 10/23/2022 revealed, .[Name Resident #6] Wandering [arrow up] for increased Shift .
Review of the 24 HOUR REPORT/CHANGE OF CONDITION REPORT dated 11/4/2022, revealed .[Name Resident #6] wandering all night .
Review of the 24 HOUR REPORT/CHANGE OF CONDITION REPORT dated 11/9/2022 revealed, .[Name Resident #6] Attempted to leave facility .
Review of the Progress Note dated 11/9/2022 revealed, .On 11/9/2022, [Named Resident #6] was last seen in her room going to the restroom by the nurse. At 7:40 [7:40 PM], door alarmed .Resident was located outside of 300/400 hall side emergency door by CNA and nurse. Resident was brought inside and to her room .
Review of an Incident Report for Resident #6 dated 11/9/2022 revealed, .7:00 pm resident was given meds [medication] per MAR [Medication Administration Record]. 7:25 pm resident was seen going to the restroom in her room. At 7:45 pm door alarm sounded and alerted staff .Nurse and CNA located resident outside of door and resident was brought inside .
Observation and interview on 1/9/2023 at 2:31 PM, with CNA #7 at the 400 Hall East door revealed there were 2 double fire doors with a 3-second chime alarm. The exit door lead out to the concrete patio. The 400 Hall East exit door had a 15-second egress bar and a white box with keypad alarm. CNA #7 confirmed the chime on the double fire doors was not working, and she had to change the batteries in the box.
Observation outside the 400 Hall exit door on 1/13/2023 at 9:24 AM, revealed a concrete patio with 2 chairs, a plastic table, and a wooden fence. The patio lead to an outside open area leading to the apartments next door.
Review of a SAFETY CHECK LOG dated 11/9/2022 revealed safety checks on Resident #6 began at 12:00 AM, and were discontinued on 11/9/2022 at 6:00 PM.
Review of the timeanddate.com website revealed the weather on 11/9/2022 was a high temperature of 70 degrees F and a low of 61 degrees F.
The facility was unable to provide documentation that Resident #6 was assessed by a physician or other provider after the elopement incident.
Review of the Elopement/Wandering in-service conducted on 11/10/2022 revealed the facility only educated 8 of 49 staff members.
Review of the Progress Note dated 11/15/2022 revealed, .11/15/22, at 10:40 pm, [Named Resident #6] was last seen in front of the nurses station. Staff went to start doing a round on resident care and observed that [Named Resident #6] was no longer sitting at the nurse station and she wasn't in her room. Around 11 pm, we immediately took action in checking all doors and discovered [Named Resident #6] wheelchair in front of the dining area emergency exit. Chair alarm was in place but was removed by resident. [Named Resident #6] was found near dumpsters on side of building and was brought inside .Dining area emergency door exit was set to off .
Review of an Incident Report dated 11/15/2022 revealed .On 11/15/22, [Named Resident #6] exited the emergency door located in the dining room area around 11 pm [11:00 PM]. She was last seen sitting in front of the nurses station by staff. As staff was getting prepared to a round .they noticed .[Named Resident #6] was no longer sitting at the nursing station and she wasn't in her room. Staff immediately took action to check all doors and [Named Resident #6] chair [wheelchair] was located in front of dining room emergency exit door. She was located outside by the dumpsters and was brought inside.
Review of the timeanddate.com showed the weather on 11/15/2022 revealed a high temperature of 43 degrees F and a low of 41 degrees F.
Review of the 24 HOUR REPORT/CHANGE OF CONDITION REPORT dated 11/20/2022 revealed, .[Name Resident #6] Exit Seeking all night .
Review of Resident #6's Discharge to Nursing Facility Summary dated 11/22/2022 revealed, .is transferring to a locked nursing facility r/t [related to] several attempted elopements .
During a telephone interview on 1/4/2022 at 7:22 PM, CNA #6 confirmed she was aware of Resident #6's wandering behaviors, and that Resident #6 had wandered outside of the facility and was found sitting outside in the cold. CNA #6 stated, .there were no alarms going off .it was cold outside .she was muddy .she was a little damp .she was cold to the touch .we let her warm up a little bit before putting her in the shower .
During an interview on 1/4/2023 at 7:36 PM, CNA #7 was asked about Resident #6 getting out of the facility. CNA #7 confirmed Resident #6 exited the facility without her knowledge twice in November 2022, and the second time she was found outside in the dark in cold weather. CNA #7 stated .her wheelchair was sitting in front of the dining room exit door .it was dark .we found her .past the dumpsters .she was sitting down .I got mud all over my new white shoes .wrapped her in a blanket to warm up for a minute .gave her a shower since she was in the grass and the mud .she was just muddy .her shoes and pants where she was sitting on her butt .
During an interview on 1/8/2023 at 10:57 AM, the Assistant Director of Nursing (ADON) confirmed Resident #6 was found outside approximately 150 feet from the dining room exit door.
During a telephone interview on 1/11/2023 at 7:22 AM, Licensed Practical Nurse (LPN) #3 confirmed Resident #6 exited the facility twice in November 2022, without her knowledge. LPN #3 stated .when she [Resident #6] came back in .she was cold .she was muddy on her knees from being on the ground .her knees were red when we took her pants off .it was from the coldness .she was sitting on the ground .it was muddy .it had rained that day .it was cold that night .they took her to the shower .her hands was [were] muddy where she was trying to get up or something .Bible and pullups was muddy .she had on blue jeans .sleeves that came to the elbow not long sleeves .church shoes .some socks on .she had mud on her shoes .she was shivering .she did not have on a jacket .
During a telephone interview on 1/11/2023 at 7:51 AM, LPN #4 was asked how Resident #6 looked when she was brought back into the facility on [DATE]. LPN #4 stated .she was [found] by the dumpsters .she was sitting on her bottom .she was in mud .it was muddy .she had on shirt and pants .shoes .her pants were muddy .her Bible and brief was muddy .
During an in interview on 1/11/2023 at 10:46 AM, the Assistant Director of Nursing (ADON) was asked when a resident is found sitting on the ground outside would consider a fall. The ADON stated .I would say so .she has to get on the ground . the ADON was asked if have an unwitnessed fall what should the staff member do. The ADON stated .should always leave them sitting .assess them .full skin assessment .fall assessment .follow up fall assessment .assess the head make sure have not hit head .assess pain level .If I had known .I would have told them to initial a fall assessment . The ADON was asked to look in point click care for Resident #6's fall assessments and was asked should resident have fall assessment and follow up assessments. The ADON confirmed the resident did not have any fall assessments in point click care.
During a telephone interview on 1/11/2023 at 2:26 PM, CNA #6 was asked if she could tell me about Resident #6 elopement on 11/15/2022. CNA #6 stated .I was looking in the building .other staff members were outside .they was getting her up off the ground .she had mud on pants leg and her hand .I know her Bible was muddy .I do remember her knees being red .I do remember her shoes were also muddy .I went to clean her shoes and Bible with a Sani wipe .we gave her a shower .hands were cold to the touch .she was cold .it was cold for an older person .
The facility was unable to provide any documentation that Resident #6 was assessed by a physician or other provider after being found shivering outside in the cold.
4. Review of medical record revealed Resident #3 was admitted to the facility on [DATE], with a readmission date of 10/16/2022, with diagnoses of Alzheimer's Disease, Hypertension, Adult Failure to Thrive, History of Falls, and Anxiety Disorder.
Review of the quarterly MDS dated [DATE] revealed Resident #3 had a BIMS of 3, which indicated severe cognition impairment, and wandering behavior was not coded.
Review of the 24 HOUR REPORT/CHANGE OF CONDITION REPORT dated 9/28/2022, 9/29/2022, 10/6/2022, 10/10/2022 and 11/4/2022 revealed, .[Name Resident #3] Wandering .
Review of the 24 HOUR REPORT/CHANGE OF CONDITION REPORT dated 11/5/2022 revealed, .[Name Resident #3] exit seeking .
Review of an Incident Report dated 12/20/2022 revealed, .This nurse was sitting at the nursing's station putting in orders, the CNA on duty came to the nurse's station and stated .[Named Resident #3] got out .200 hall .The CNA stated that the resident's wheelchair was in front of the 200-hall door, and door had not shut completely behind resident .and the resident had exited on foot. The CNA said that she heard the alarm sounding at the 200-hall door when she went to check call lights, but there was no alarm sounding at the nurse's station, so I was unaware of the situation until alerted by said CNA. The resident was brought back in safely. She was wearing a shirt, sweater over the shirt, and winter coat, jogging pants, socks, and shoes. She had clothing with her (sweater and two shirts) and a bottle of coca cola. Resident was assessed. She stated I am looking for my momma and daddy .
Observation on the 200/300 Hall closed unit on 1/9/2023 at 9:50 AM, with Housekeeper #1 revealed several empty rooms used for storage open and unlocked, a locked Biohazard Room, a Laboratory Room that was unlocked with Covid testing supplies, an isolation cart, a bucket of disinfectant wipes, bottle of hand sanitizer, and an unlocked hopper room. The Social Worker, MDS Coordinator, Assistant Director of Nursing (ADON), and the Maintenance Director offices were on this unit on the 300 hall. Upon entering the closed 200/300 hall section there were a set of double fire doors with a 3-second chime alarm.
Review of the timeanddate.com revealed the weather on 12/20/2022 was a high temperature of 39 degrees F and a low of 36 degrees F.
Observation outside the 200 Hall South exit door on 1/13/2023 at 4:09 PM revealed a concrete sidewalk leading to the apartments next door. The sidewalk had scattered pine needles and leaves at various spots on the sidewalk. The end of the concrete sidewalk was covered with mud and leaves. There was a dumpster running over with trash at the end of the sidewalk, and just past the dumpsters was the apartment parking lot. To the left of the parking lot there were 16 mailboxes mounted on 5 wooden frames. The apartment parking lot lead to a 2-lane road.
During an interview on 1/4/2022 at 2:35 PM CNA #7 stated, .[Named Resident #3] .got out of back door on the 200 hall .there are no patients back there .Its behind closed double doors .seen wheelchair in front of the door .she was out of the wheelchair .it was dark .she was found at the mailboxes near the apartments .
During an interview on 1/4/2023 at 3:04 PM, CNA #11 was asked if he knew of anyone getting outside the facility. CNA #11 stated .which time .the last time she [Resident #3] got out was mid-December .she went through the double door on the 200 hall .she went out the door and no one knew she left .the alarm did no go off at the desk .she [was] over by the mailbox by the apartment .I feel like that was the second time she got out that day .
During a telephone interview on 1/4/2023 at 3:41 PM, LPN #7 was asked if she knew of any residents getting out of the facility. LPN #7 confirmed Resident #3 had exited the facility without staff knowledge.
During a telephone interview on 1/4/2023 at 4:09 PM, LPN #6 confirmed Resident #3 had exited the facility without staff knowledge.
During a telephone interview on 1/4/2023 at 6:29 PM, LPN #1 confirmed she had been told in report that Resident #3 had exited the facility without staff knowledge.
During an interview on 1/4/2022 at 8:30 AM, the Maintenance Director was asked if any residents had gotten out of the facility. The Maintenance Director stated .not to get out but got the door open a time or two .
During a telephone interview on 1/5/2023 at 12:08 PM, the Nurse Practitioner (NP) if she was aware the facility had 3 elopements. The Nurse Practitioner stated .I was not aware of all of them .spoke to the Medical Director this morning and he stated he got called .I don't think they got past the parking lot .[Named Resident #3] .exited .[Named Resident #6] .I know she got out the facility . The NP was asked if it was safe for a resident to be outside unsupervised. The NP stated .no unsupervised it's not safe .
During a telephone interview on 1/5/2023 at 12:35 PM, the Medical Director was asked if a resident should be outside unsupervised and unattended and was that considered safe. The Medical Director stated .no, ma'am it's not safe .
During an interview on 1/9/2023 at 2:15 PM, LPN #2 was asked to explain how she checked the wanderguard placement and function. LPN #2 stated .I just check that it's on and clipped .put in the wheelchair and take it to the door . The LPN was asked which door had the wanderguard sensor. LPN #2 stated .whatever door is the closest . LPN #2 was asked if she had been checking the function of the wanderguard. LPN #2 stated .No .
The facility only has one door equipped for the wanderguard system, which is the front door in the main lobby.
The facility was unable to provide documentation a head count was completed after the search of the missing resident according to their policy.
The facility neglected to adequately supervise Resident #3 and #6 to prevent incidents of elopement.
5. Review of medical record revealed Resident #2 was admitted to the facility on [DATE], with a readmission date of 1/2/2023, with diagnoses of Parkinson's Disease, Hypertension, Dementia, Chronic Obstructive Pulmonary Disease, Bipolar Disorder, and Anxiety Disorder.
Review of quarterly Minimum Data Set (MDS) assessment dated [DATE] revealed Resident #2 had a Brief Interview for Mental Status (BIMS) score of 9, which indicated moderate cognitive impairment, and falls was not coded.
Review of the Care Plan dated 1/2/2023 revealed, .The resident is at risk for falls r/t [related to] Balance .Unsteady gait .bedside commode stabilized to prevent tipping over, fall intervention 3.30.2021 [3/30/2021] .Fall 02/07/2022 .Recurrent falls .Soft helmet in place r/t risk of falls and risk of injury .
Observation in the resident's room on 1/11/2023 at 2:18 PM with the ADON revealed Resident #2 had no bed side commode or helmet.
6. Review of medical record revealed Resident #3 was admitted to the facility on [DATE], with a readmission date of 10/16/2022, with diagnoses of Alzheimer's Disease, Hypertension, Adult Failure to Thrive, History of Falls and Anxiety Disorder.
Review of the quarterly MDS dated [DATE] revealed Resident #3 had a BIMS of 3, which indicated severe cognition impairment, and falls were not coded.
Review of the Care Plan revised 11/30/2022 revealed, .Anti-roll backs and dysum [non-skip mat] added to wheelchair for fall intervention 9/23/19 [9/23/2019] .
Observation at the nursing station on 1/11/2023 at 2:11 PM with the ADON revealed Resident #3 sitting at the nursing station in her wheelchair. ADON assisted resident to a standing position, there was no Dysum mat in the Resident #3's wheelchair.
7. Review of medical record revealed Resident #5 was admitted on [DATE], with a readmission on [DATE], with diagnoses of Adult Failure to Thrive, Repeated Falls, Hepatitis C, Chronic Obstructive Pulmonary Disease, Depression, and Anxiety Disorder.
Review of the quarterly MDS dated [DATE] revealed Resident #3 had a BIMS of 14, indicating he was cognitively intact and had 2 falls since admission.
Review of the Care Plan revised on 11/30/2022 revealed, .at risk for falls r/t Balance Deficits .History of falls .Intervention .Break extender added to wheelchair .Non-Skid tape applied to the floor at bedside .non-skid tape to floor in front of toilet .Anti-Roll backs on wheelchair applied to wheelchair .
Observation in Resident #5's room on 1/11/2022 at 1:55 PM with the ADON, revealed there were no anti-roll-backs or break extender on the wheelchair and no nonskid tape on the floor.
During an interview on 1/11/2023 at 2:21 PM, the ADON was asked if staff should follow care plan for intervention for falls. The ADON stated .They should .
8. The surveyors verified the Allegation of Compliance (AoC) Removal Plan through record review, observations, audit reviews, review of education and sign-in sheets, and interviews for the immediate corrective actions listed below:
a. The identified residents- Resident # 6 was placed on 1:1 supervision on 11/15/2022 until discharge to a locked unit on 11/22/2022. Surveyors confirmed through record review and interviews.
b. On 11/15/2022 the charge nurse checked the door the resident exited and noted the alarm was manually disabled, staff stayed at the door until the maintenance director was contacted and gave instruction on how to re-engage the alarm. The surveyor confirmed with interviews.
c. The Charge Nurse checked the function of all exit doors and found no other concerns on 11/15/2022. The surveyor confirmed with interviews.
d. The facility completed an investigation of the event occurring on 11/15/2022 and determined the root cause to be that the alarm was manually disabled by the maintenance director to bring furniture in and out of the dining room and was not turned back on. The surveyor confirmed with interviews.
e. Maintenance Director was re-educated on door alarms need to be engaged at all times on 11/16/2022 by the Administrator. The surveyor confirmed with interviews.
f. The identified Resident #3 was placed on 1:1 supervision on 12/20/2022 until door repair on 12/21/2022. The door was monitored by assigned staff starting on 12/20/2022 until repaired on 12/21/2022 by the Regional Maintenance Director. The surveyor confirmed with interviews.
g. The Administrator checked the function of all exit doors on 12/20/2022 and found all to be functioning except the door identified with a broken wire to the sensor. The door was secured but the alarm was not audible at the nurse's station. The door was being monitored by staff until repair on 12/21/2022. The surveyor confirmed with interviews and record review.
h. Investigation was completed and root cause determined to be a broken sensor wire leading to the annunciator which did not alarm at the nurse's station. Further investigation revealed condensation had caused the molding that was holding the wire, to pull away from the wall resulting in wires pulling away from the alarm box and not sounding at the nurse's station. The surveyor confirmed with interviews.
i. Facility exit doors were checked for function 5 x week by the Maintenance Director ongoing as well as 7 x week by the Administrator for 2 weeks. The surveyor confirmed with interviews and audit reviews.
j. Cognitively impaired residents with wandering behaviors are placed with a wanderguard bracelet to alert the facility of the resident exiting to any area that is not secured or alarmed. The surveyor confirmed with interviews.
k. Resident #6 was last seen at approximately 10:40 PM, during staff rounds and was located at 11:00 PM. Resident #3 was last seen at approximately 5:10 PM and located at 5:18 PM. The surveyor confirmed with interviews.
l. On 11/16/2022 all exit alarms were inspected by the Maintenance Director and the ability to disengage the alarm was removed making all alarms unable to be disengaged. On 11/16/2022 all exit alarms were checked and found to be functioning by the Maintenance Director and the ability to disengage alarms was removed from all exit doors on 11/16/2022 by the Maintenance Director. The surveyor confirmed with interviews.
m. On 11/17/2022 the Interdisciplinary Team (IDT) completed a review of all current residents to identify any that were at risk of elopement. Any at risk of elopement had a review of their wanderguard orders to verify functioning is check daily by the licensed nurses and care plans to determine if the care plan was appropriate to meet the safety and supervision needs of the resident. Any needed corrections were made at that time. Cognitively impaired residents with wandering behaviors are assessed to determine the risk of elopement and based on risk factors a care plan is developed to provide safety without restriction of movement and quality of life. Interventions and supervision level is based on risk factors and resident needs and are resident specific. The surveyor confirmed with interviews.
n. On 12/21/2022 the IDT completed a review of all current residents to identify any that were at risk of elopement. Any at risk of elopement had a review of their wander guard orders to verify functioning is check daily by the licensed nurses and care plans to determine if the care plan was appropriate to meet the safety and supervision needs of the resident. Any needed corrections were made at that time. Cognitively impaired residents with wandering behaviors are assessed to determine the risk of elopement and based on risk factors a care plan is developed to provide safety without restriction of movement and quality of life. Interventions and supervision level is based on risk factors and resident needs and are resident specific. The surveyor confirmed with interviews.
o. On 12/21/2022 all exit door alarms were checked by the Maintenance Director and Regional Maintenance Director with no concerns identified. A Specialty tape was applied to all wiring of exit alarms to prevent dislodgement of condensation on 12/21/2022 by the Maintenance Director and Regional Maintenance Director. The surveyor confirmed with interviews and observation.
p. Resident # 6, Beginning on 11/16/2022 facility staff were re-educated on the Unsafe Wandering and Elopement Prevention.
On 11-16-2022 the ability to disengage all alarms on exit doors was removed by the Maintenance Director. The surveyor confirmed with interviews.
q. Resident # 3, Beginning 12/20/2022 facility staff were re-educated on the elopement policy by the DON (Director of Nursing) or designee with no s[TRUNCATED]
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
QAPI Program
(Tag F0867)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, review job description review, and interview, the facility failed to ensure an effective Quality Assuran...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, review job description review, and interview, the facility failed to ensure an effective Quality Assurance Performance Improvement (QAPI) program that recognized ongoing problems with resident safety to prevent, identify, report, and thoroughly investigate, allegations of abuse and neglect. The QAPI committee failed to assure the facility was administered in a manner to use its resources effectively and efficiently, and that the Regional Director of Operation assisted the facility with identifying, evaluating, addressing clinical concerns, coordinating the care, and providing clinical guidance and oversight. Failure of the facility to implement and/or provide interventions to maintain safety of the residents and ensure the residents highest quality of care resulted in the likelihood of a serious event when Resident #3 exited the facility without staff knowledge or supervision through a malfunctioning exit door and when Resident #6 exited the facility without staff knowledge or supervision on 2 separate occasions, 6 days apart, one through a malfunctioning exit door. The QAPI committee program failed to identify the root cause of elopement. The facility failed to report and thoroughly investigate allegations of abuse and neglect. The facility QAPI program failed to provide oversight that established and implemented policies and procedures to ensure the facility provided effective housekeeping services and maintenance services to maintain a sanitary, orderly, and comfortable environment. These failures resulted in Immediate Jeopardy for Resident #3 and #6 and Substandard Quality of Care in environment.
Immediate Jeopardy (IJ) is a situation in which the provider's noncompliance with one or more requirements of participation has caused, or is likely to cause, serious injury, harm, impairment, or death to a resident.
The Administrator, Director of Nursing and the Regional Director of Operation were notified of the Immediate Jeopardy (IJ) for F-600, 609, 610, and 868 during the complaint investigation on 1/9/2023 at 4:40 PM, in the Conference Room.
The Administrator was notified of the Immediate Jeopardy (IJ) for F-835 during the complaint investigation on 1/11/2023 at 10:23 AM, in the Conference Room.
The Administrator was notified of the Immediate Jeopardy (IJ) for F-867 on 1/13/2023 at 12:53 PM, in the Conference Room.
The facility was cited Immediate Jeopardy at F-600, F-609, F-610, F-689, F-835, and F-867.
The facility was cited at F-600, F-609, F-610, and F-689 at a scope and severity of J, which is Substandard Quality of Care.
The Immediate Jeopardy existed from 11/9/2022 through 1/16/2023.
A Removal Plan which removed the immediacy of the jeopardy was received on 1/13/2023 at 3:27 PM, and was validated onsite by the surveyors on 1/17/2022 through review of Quality Assurance Performance Improvement (QAPI) minutes, signature sheets, and staff interviews on all shifts.
The findings include:
Review of the facility's policy titled QAPI Plan (Quality Assurance Performance Improvement Plan), revised 10/24/2022 revealed .It is the policy of this facility to systematically collect data as part of the QAPI program to ensure the care and services it delivers meet acceptable standards of quality in accordance with recognized stands of practice. In addition the purpose of this document is to serve as a plan to assist the facility in development, implementation, and maintenance of an effective, comprehensive, data driven QAPI program that focuses on indicators of the outcomes of care and quality of life. The goal is to create a process that ensures care and services delivered meet accepted standards of quality .Key components of this plan .Tracking and measuring performance .Identifying and prioritizing quality deficiencies .Monitoring and evaluating the effectiveness .performance improvement activities and revising as needed .QAPI .Audits .Elopement-Monthly .Environment -Monthly .Careplans-Monthly .Facility QAA Committee shall be interdisciplinary and shall .Consist at a minimum of .The Director of Nursing Services .the Medical Director of his/her designee .At least three other members of the facility's staff, at least one of which must be the administrator, owner, a board member or other individual in a leadership role .Infection Preventionist .A member of direct care staff .Develop and implement appropriate plan of action to correct identified qualify deficiencies .Regularly review and analyze data, including data collected under the QAPI program .act on available data to make improvements .The QAA committee must sign to verify approved of all plans of correction .Program Activities .Measures affecting resident health, safety .quality of care .Corrective Action .Once the root cause of a problem is identified, the QAA committee over sees the development of and appropriate corrective action .Corrective action plans include .A definition of the problem - which includes determining contributing cause of the problem .Measurable goals .Step-by-step interventions to correct the problems and achieve established goals .A description of how the QAA committee will monitor to ensure changes yield the expected results .
Review of the facility's signed Administrator Job Description revealed .Responsible for the efficient and profitable operation of the facility, facility compliance with .Stated and Federal rules and regulations, and providing the highest quality of care possible .Manages the day-today operation of the facility Implements control systems to ensure accountability of all departments .Ensures all employees receive orientation and ongoing training to meet the quality goals of the organization .Knowledge of Long term Care and Medicare and Medicare regulations and standards .
Review of the facility's signed Director of Nursing Job description revealed .Manages the facility nursing program in accordance with the Nurse Practice Act, applicable State and Federal regulations, and policies and procedures .Round on unit at least once daily .Manage the Nursing Department with the goal of achieving and maintaining the highest quality of care .Identification of training needs .Assures that all clinical protocols and nursing policies and procedures are followed .Assumes complete responsibilities for the Center in absence of Administrator .
Review of the Unnamed Roster dated 8/28/2022 revealed .Administrator .MDS [Minimum Data Set Coordinator] .SSD [Social Service Director] .Ancillary Services Marketing .
Review of the Unnamed Roster dated 11/26/2022, revealed . Administrator .DON [Director of Nursing] .ADON [Assistant Director of Nursing] .SSD [Social Service Director] .Marketing .
During an interview on 1/12/2023 at 4:24 PM, the Director of Nursing (DON) was asked if the facility interventions were affective with the 3 elopements. The DON stated .No .there is room for improvement .
During an interview on 11/13/2022 at 11:33 AM, the Administrator was asked if Resident #6 exited/attempt from the facility on 11/9/2022. The Administrator stated .our investigation .that was relayed to me she was found at the door and the alarm was sounding at the door .we have morning meeting .we talked about on 11/9/2022 .I don't know of any other attempts on the 24 hour report talked about in the clinical /morning qa [Quality Assurance] meeting we should have known about it and documents we should have acted on that .things should have been addressed . The Administrator was asked should the facility have addressed documentation of Resident #6 attempt time 2 on the 10/23/2022. The Administrator stated .If we have wandering behavior .they should be redirecting .they should let us know .It was not identified as a problem in QA until she exited the building 11/15/2022 .It is important for all staff to know what to do for and elopement .an attempt is just as serious as and elopement .the time to do and intervention is no .if see wandering with a purpose .it's important for us to keep the residents safe .
The QAPI committee failed to ensure Administration developed and implemented policies and procedures, had a system in place to monitor nursing services and facility staff, and had a system to ensure allegations of abuse were thoroughly reported and investigated.
Refer to F-600, F-609, F-610, and F-689
The QAPI committee failed to have a QAPI program that was ongoing, comprehensive, and addressed the full range of care and services provided by the facility and utilized the best available evidence to define and measure indicators of facility goals that reflected processes of care for residents with allegations of abuse.
Refer to F-600, F-744, and F-835
The QAPI committee failed to provide ongoing communication between the facility, Administrative staff, including the Administrator, and the Director or Nursing to ensure identified concerns were addressed in a timely manner.
Refer to F-837
The surveyors verified the Allegation of Compliance (AoC) Removal Plan through review of education and sign-in sheets, observations, and interviews for the immediate corrective actions listed below:
1. On 11-17-2022 and 12-20-2022 the Interdisciplinary Team (IDT) completed a review of all current residents to identify any that were at risk of elopement. Any at risk of elopement had a review of their wander guard orders to verify functioning is check daily by the licensed nurses and care plans to determine if the care plan was appropriate to meet the safety and supervision needs of the resident. Any needed corrections were made at that time. Cognitively impaired residents with wandering behaviors are assessed to determine the risk of elopement and based on risk factors a care plan is developed to provide safety without restriction of movement and quality of life. Interventions and supervision level is based on risk factors and resident needs and are resident specific. The Surveyor confirmed by observation, record review, and interviews.
2. The DON (Director of Nursing) completed an audit of all current residents on 1-06-2023 to identify those that were an elopement risk. There were five (5) residents identified as having the potential to be affected. The Surveyor confirmed by observation, record review, and interviews.
3. On 1-13-2023 the Regional Director of Operations observed the QAPI (Quality Assurance and Performance Improvement) committee adhoc (when necessary or needed) review of incident reports in the past 30 days including elopements or elopement attempts and observed the QAPI committee discussion of root cause analysis, investigation, neurological assessments, MD/NP (Medical Director/Nurse Practitioner) notification and supervision.The Surveyor confirmed by review of meeting minutes and signature sheets, and interviews.
4. On 1-13-2023 the Regional Director of Operations added to the facility QAPI template a review of incident events investigations, root cause analysis, neurological assessment if suspected fall, MD (Medical Director) notification, elopement attempts or changes in elopement risk. The Administrator or designee will present results of these reviews to the QAPI committee monthly for three months. The Surveyor confirmed by review of meeting minutes and signature sheets, and interviews.
5. The QAPI committee was re-educated by the Regional Director of Operations on the QAPI process on 1-13-2023. The review included a review of accuracy of incident for type, neurological assessment if suspected fall, root cause analysis, through investigation, MD/NP notification, elopement or elopement attempt and supervision. The committee will consist of at a minimum the Administrator, Director of Nursing, Assistant Director of Nursing/IP (Infection Preventionist), Social Services Director with the Medical Director attending at least quarterly. The Surveyor confirmed by observation, record review, and interviews.
6. The Regional Director of Operations will attend the QAPI committee meeting monthly for three months to evaluate effectiveness of the QAPI committee including incident review, investigation, root cause analysis, elopement and elopement attempts and other areas for a systematic approach for resident safety and supervision. The Surveyor confirmed through interviews.
7. On 1-13-2023 an ad [NAME] QAPI was held to review the Immediate Jeopardy and removal plan. Participants include the Administrator, RDO, Director of Nursing, Assistant Director of Nursing/IP, Social Services Director, Activity Director, MDS Nurse, BOM, Maintenance Director and Dietary Manager. The Medical Director attended by phone. The Surveyor confirmed by observation, record review, and interviews.
The facility's noncompliance of F-867 continues at a scope and severity of D for monitoring the effectiveness of the corrective actions.
The facility is required to submit a Plan of Correction.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, medical record review, and interview, the facility failed to notify the responsible party for 1 of 4 (Re...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, medical record review, and interview, the facility failed to notify the responsible party for 1 of 4 (Resident #3) sampled residents reviewed for elopement.
The findings included:
1. Review of the facility's policy titled, Notification of Changes, revised 1/1/2022 revealed, .The purpose of this policy is to ensure the facility promptly informs the resident, consults the resident's physician .and notifies, consistent with his or her authority, resident's representative when there is a change requiring notification .
2. Review of medical record revealed Resident #3 was admitted on [DATE] with diagnoses of Alzheimer's Disease, Hypertension, Adult Failure to Thrive, History of Falls and Anxiety Disorder.
Review of the quarterly Minimum Data Set (MDS) assessment dated [DATE] revealed Resident #3 had a Brief Interview for Mental Status (BIMS) score of 3 indicating severe cognition impairment, and wandering behavior was not coded.
During a telephone interview on 1/6/2022 at 8:15 AM, Resident #3's daughter confirmed she was not notified of her mother's (Resident #3) elopement from the facility on 12/20/2022.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, medical record review, and interview, the facility failed to report incidents of elopement for 2 of 5 sa...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, medical record review, and interview, the facility failed to report incidents of elopement for 2 of 5 sampled residents (Resident #3 and #6) reviewed for wandering and elopement. Resident #3, a vulnerable resident with severe cognition impairment, exited the facility on 12/20/2022 without staff knowledge or supervision; and Resident #6, a vulnerable resident with severe cognition impairment, exited the facility on 11/9/2022 and 11/15/2022 without staff knowledge or supervision.
The findings include:
1. Review of the facility's policy titled, Incidents and Accidents Reporting, revised 8/11/2022, revealed .It is the policy of this facility for staff to utilize electronic and/or approved forms to report, investigate and review any accidents or incidents that occur or allegedly occur, on facility property and may involve or allegedly involved a resident .An incident is defined as an occurrence or situation that is not consistent with the routine care of a resident or with the routine operation of the organization .The purpose of incident reporting is .Assure that appropriate and immediate interventions are implemented and corrective actions are taken to prevent recurrences and improve the management of resident care .Incident/accident reports will be reviewed by the QAPI committee on a routine basis to be analyzed. Analysis may include, for example, considering the severity of hazard, the immediacy of risk, and trends such as time of day, location .Incidents that rise the level of abuse .neglect .will be managed and reported according to the facility's abuse prevention policy .The following incidents/accidents require an incident/accident report but are not limited .allegations of abuse .Elopement .The nurse will notify the resident's practitioner to inform them of the incident/accident .The resident family or representative will be notified of the incident/accident .The nurse .will enter the incident/accident information into the appropriate form/system within 24 hours of occurrence and will document all pertinent information .Documentation should include the date, time, nature of the incident, location, initial findings, immediate interventions, notifications .follow-up interventions .obtain the witnesses' account .
Review of the facility's policy titled, Abuse, Neglect and Exploitation, revised 10/24/2022, revealed .It is the policy of this facility to provide protections for the health, welfare, and rights of each resident by developing and implementing written policies and procedures that prohibit and prevent abuse neglect .Neglect .means failure of the facility, its employees, or service providers to provide goods and services to a resident that are necessary to avoid physical harm, pain, mental anguish, or emotional distress .The facility will designate an Abuse Prevention Coordinator in the facility who is responsible for reporting allegations or suspected abuse, neglect .to the state survey agency .Reporting of all alleged violation to the Administrator, state agency, adult protective services .within specified timeframes .Immediately, but not later than 2 hours after the allegations is made, if the events that cause the allegation involve abuse .
2. Review of the facility's signed Administrator Job Description dated 12/1/2015 revealed, .Responsible for the efficient and profitable operation of the facility, facility compliance with .Stated and Federal rules and regulations, and providing the highest quality of care possible .Manages the day-today operation of the facility .Implements control systems to ensure accountability of all departments .Ensures all employees receive orientation and ongoing training to meet the quality goals of the organization .Knowledge of Long term Care and Medicare and Medicare regulations and standards .
Review of the facility's signed Director of Nursing Job description dated 9/26/2022 revealed, .Manages the facility nursing program in accordance with the Nurse Practice Act, applicable State and Federal regulations, and policies and procedures .Round on unit at least once daily .Manage the Nursing Department with the goal of achieving and maintaining the highest quality of care .Identification of training needs .Assures that all clinical protocols and nursing policies and procedures are followed .Assumes complete responsibilities for the Center in absence of Administrator .
3. Review of medical record revealed Resident #6 was admitted to the facility on [DATE], with diagnoses of Parkinson's Disease, Osteoarthritis, Major Depression, Chronic Obstructive Pulmonary Disease, Repeated Falls, and Hypertension.
Review of the quarterly Minimum Data Set (MDS) dated [DATE] revealed Resident #6 had a Brief Interview for Mental Status (BIMS) score of 4, which indicated severe cognition impairment, and wandering behavior was not coded.
Review of an Incident Report for Resident #6 dated 11/9/2022 revealed .7:00 pm resident was given meds per MAR [Medication Administration Record] .7:25 pm resident was seen going to the restroom in her room .At 7:45 pm door alarm sounded and alerted staff .Nurse and CNA located resident outside .
The Facility failed to report incident of elopement on 11/9/2022.
Review of an Incident Report dated 11/15/2022 revealed, .On 11/15/22, [Named Resident #6] exited the emergency door located in the dining room area around 11 pm [11:00 PM]. She was last seen sitting in front of the nurses station by staff. As staff was getting prepared to a round on patients .[Named Resident #6] was no longer sitting at the nursing station and she wasn't in her room. Staff immediately took action to check all doors and [Named Resident #6] chair [wheelchair] was located in front of dining room emergency exit door. She was located outside by the dumpsters and was brought inside .
The facility failed to report incident of elopement on 11/15/2022.
During an interview on 1/4/2023 at 7:03 PM, Licensed Practical Nurse (LPN) #3 confirmed Resident #6 exited the facility and was found outside past the garbage dumpsters. LPN #3 confirmed she did not see Resident #6 exit the facility.
During an interview on 1/4/2023 at 7:36 PM, CNA #7 confirmed Resident #6 had exited the facility twice in the month of November and was found outside. CNA #7 confirmed she did not see Resident #6 exit the facility.
The allegation of elopement was reported to the Adult Protective Services (APS) by email on 1/9/2023 at 10:26 PM, for Resident #6. Resident #6 eloped from the facility on 2 separate occasion and only one incident 11/15/2022 was reported to APS.
4. Review of the medical record revealed Resident #3 was admitted on [DATE], with a readmission date of 10/16/2022, with diagnoses of Alzheimer's Disease, Hypertension, Adult Failure to Thrive, History of Falls and Anxiety Disorder.
Review of the quarterly MDS dated [DATE] revealed Resident #3 had a BIMS score of 3, which indicated severe cognition impairment, and wandering behavior was not coded.
Review of an Incident Report dated 12/20/2022 revealed, .This nurse was sitting at the nursing's station putting in orders, the CNA [Certified Nursing Assistant] on duty came to the nurse's station and stated .[Named Resident #3]'s got out .The CNA stated that the resident's wheelchair was in front of the 200 hall door, and door had not shut completely behind resident .and the resident had exited on foot. The CNA said that she heard the alarm sounding at the 200 hall door when she went to check call lights, but there was no alarm sounding at the nurse's station, so I was unaware of the situation until alerted by said CNA. The resident was brought back in safely. She was wearing a shirt, sweater over the shirt, and winter coat, jogging pants, socks, and shoes. She had clothing with her (sweater and two shirts) and a bottle of coca cola. Resident was assessed. She stated 'I am looking for my momma and daddy .
The facility failed to report incident of elopement on 12/20/2022.
During an interview on 1/4/2022 at 2:35 PM, CNA #7 was asked if she knew about any residents exiting the facility. CNA #7 stated .[Named Resident #3] .got out of back door on the 200 hall .there are no patients back there[200 hall close unit] .It's behind closed double doors .goes to the 200 hall .seen wheelchair in front of the door .she was out of the wheelchair .it was dark .called nurses station for help .
During a telephone interview on 1/4/2023 at 4:09 PM, LPN #6 confirmed Resident #3 exited the facility on 12/20/2022, and was found by staff outside.
During an interview on 1/4/2023 4:45 PM, the Assistant Director of Nursing (ADON) was asked about Resident #3's elopement. The ADON stated .I was at home .got phone call at 7 pm .I asked what type clothes she had on .when was the last time staff seen her .was 5:10 PM .found at 5:18 PM .that what I was told .did staff write statements .[Named Administrator] .notify everyone .MD, RP, the Administrator and DON .called the Maintenance Director to check the door .make sure it was fixed .he beat me here .I went to the door .he [Named Maintenance Director] could not get it to work .it was alarming at the door .but not the nursing station .sensor at the top of the door the wire was hanging out of it .there was some construction men going in and out the door 4 hours the day prior to the event .[Named Maintenance Director] fixed the box in house .It was in December before Christmas .we have a trigger system event for abuse .injury of unknown origin .I was told a resident getting out of the building is not a reportable event . The ADON confirmed the incidents of elopement were not reported to the State Survey Agency (SSA).
The allegation of elopement was reported to APS by email on 1/9/2023 at 10:15 PM, for Resident #3. The elopement occurred on 12/20/2022.
During an interview on 1/4/2023 at 5:28 PM, the Administrator was asked if she should have reported the incident of elopement to the SSA. The Administrator stated .we did not report it .it was not required for us to report an elopement .
During an interview on 1/9/2023 at 3:53 PM, the Regional Director of Operation was asked should the facility have reported the elopements. The Regional Director of Operation stated .our understanding with reportable to the state has to fall under abuse .no we don't report an elopement to the state .
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on Service Agreement review, Director of Maintenance Job Description review, observation, and interview, the facility fail...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on Service Agreement review, Director of Maintenance Job Description review, observation, and interview, the facility failed to ensure that waste was properly contained and maintained in a sanitary condition to prevent the harborage and feeding of pests when 2 of 2 dumpsters (Dumpster #1 and #2) were observed overflowing with trash with lids opened, and garbage lying around the grounds of the facility.
The findings include:
Review of the facility's undated SERVICE AGREEMENT revealed .Healthcare will provide all management .labor and materials necessary to perform the housekeeping .services on premises of the Facility .
Review of the Director of Maintenance job description, revealed .Supervise the maintenance department .is responsible for .efficient function of physical plant .environmental system .the appearance .upkeep of the facility grounds .Participates in facility .Performance Improvement Program .
Observations just outside the dining room exit door on the side of the facility on 1/5/2023 at 8:47 AM, revealed 3 large PVC (a type of plastic piping that is used in a variety of applications) pipe frames made for privacy screens, an old biohazard [NAME] with broken wood at the bottom of the doors and green discoloration up the front of the door, 2 large barrels to the right of the biohazard [NAME] with dark greasy substance, and a milk crate to the left side of the biohazard [NAME]. There was an opening between the service door and the biohazard [NAME] with 8 milk crates lying on the ground, and a dust pan with the handle filled with water, a soda can, trash, and 3 broken wooden pallets lying up against the side of the biohazard [NAME]. On the back side of biohazard [NAME] in front of boiler room, was a lot of trash and debris, 5 (5) gallon buckets, 10 additional milk crates lining the back wall of the facility, a gray cart with trash and debris, and a wet cardboard box. There were 3 large trash cans filled with trash and 8 wooden planks lying on the ground in front of the boiler room. The dumpster area had trash all around the 2 trash bins, including part of a broken wooden pallet, gloves, milk cartons, juice containers, boost boxes, and condiment packets. One dumpster had 2 of the lids open, and the other dumpster was overflowing with trash. An old air conditioner was lying on the ground, and the surrounding area of the ground had trash scattered all around.
During an interview on 1/5/2023 at 8:51 AM, the Maintenance Director confirmed the outside area was last cleaned on 6/10/2022, and the outside area needed to be cleaned.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on Service Agreement review, Director of Maintenance Job Description review, admission Packet review, policy review, obser...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on Service Agreement review, Director of Maintenance Job Description review, admission Packet review, policy review, observation, and interview, the facility failed to provide effective housekeeping/pest control services and maintenance services to maintain a sanitary, orderly, and comfortable environment as evidenced by roach infestations in 9 of 51 resident rooms (room [ROOM NUMBER], #111, #114, #209, #210, #313, #412, #415 and #419), and 3 of 10 Staff areas (Laundry Wash Room, Staff Break Room, and Pantry/Snack Room) observed, and outside on the facility grounds.
The findings include:
Review of the facility's policy titled, 5-Step Daily Room Cleaning, revised 10/25/2016, revealed .Damp Mop .As with dust mopping, start in the far corner of the room, move all furniture necessary, and run the mop along the edges first. Never push the mop into a corner as this leads to build up .
Review of the facility's undated SERVICE AGREEMENT revealed .Healthcare will provide all management .labor and materials necessary to perform the housekeeping and laundry services on premises of the Facility .
Review of the Director of Maintenance job description, revealed .Supervise the maintenance department .is responsible for .efficient function of physical plant .environmental system .the appearance .upkeep of the facility grounds .Participates in facility .Performance Improvement Program .
Review of the Name Service Group Project Schedule, revealed .Tue [Tuesday] .Pull Furniture Odd Rooms .Trash Cans .Wed [Wednesday] .Pull Furniture Even Rooms .Trash Cans .
Review of the handwritten treated area for roaches dated 1/9/2023, observation from the Maintenance Director revealed the following rooms observed with roaches 100, 102, 109, 111, 115, 114, 116, 117, 201, 205, 209, 213, 215, 401, 310. 311, 312, 313, 315, 317, 405, 412, 413, 417, 419, Nourishment/Pantry Room, Break Room, and the Nursing Station.
Review of the Name Pest Control Company Invoice dated 1/10/2023, revealed the following rooms were treated 101, 103, 104, 106, 108, 110, 112, 113, 203, 207, 209, 211, 213, 314, 316, 402, 403, 404, 406, 407, 408, 409, 410, 411, 412, 414, 416, 418, boiler room, dry storage, soiled laundry, laundry, environmental service, material management, administration offices x 4, and the copier room.
During an interview on 1/4/2023 at 10:51 AM, Certified Nursing Assistant (CNA) #4 confirmed she saw roaches in rooms [ROOM NUMBERS].
Observation in the bathroom for room [ROOM NUMBER] on 1/4/2023 at 3:28 PM, revealed multiple dead roaches under a laundry basket at the sink area and under a basket on the right side of the toilet.
Observation in the Snack/Pantry Room on 1/4/2023 at 3:30 PM, revealed a live roach on the wall behind the equipment, and multiple dead roaches behind the equipment and a snack cart against the wall.
Observation in the bathroom for room [ROOM NUMBER] on 1/5/2023 at 4:45 PM, revealed multiple dead roaches under a basket, trash can and laundry basket.
During an interview on 1/5/2023 at 4:45 PM, Resident #13 was asked if she had any problems with roaches in her room. Resident #13 stated .yes .they used to crawl all over me at night .I don't like that .
During an interview on 1/6/2022 at 8:15 AM, Resident #3's daughter was asked if she had seen any roaches. The Daughter stated .Yes, ma'am .in the bathroom mostly .we have battled the roaches .
Observation in the bathroom for room [ROOM NUMBER] on 1/9/2023 at 9:12 AM, revealed multiple dead roaches under a basket below the sink and beside the toilet under a basket and under the garbage can. Additionally, 3 live roaches were observed beside the toilet.
Observation in the bathroom for room [ROOM NUMBER] on 1/9/2023 at 9:13 AM, revealed 2 live roaches, one crawling on the commode and one on the floor.
Observation in the Pantry on 1/9/2023 at 9:14 AM, revealed the floor behind the equipment with multiple dead roaches.
Observation in the bathroom for room [ROOM NUMBER] on 1/9/2023 at 9:19 AM, revealed 2 live roaches, one crawling on the floor and the other crawling on the commode.
Observation in room [ROOM NUMBER] on 1/9/2023 at 9:22 AM, revealed dead roaches near the bathroom door, and behind and on the sides of the dresser.
Observation in room [ROOM NUMBER] on 1/9/2023 at 9:28 AM, revealed multiple dead roaches behind the overnight stand.
During an interview on 1/9/2023 at 9:28 AM, Housekeeping Staff Member #1 stated .this room [room [ROOM NUMBER]] used to be really bad .you can tell they have sprayed [pest control spray] .
During an interview on 1/9/2023 at 9:29 AM, Resident #12 was asked if she had seen any roaches in her room. Resident #12 stated .Oh, yeah [yes] .
Observation and interview in room [ROOM NUMBER] on 1/9/2023 at 9:32 AM, with Housekeeping Staff Member #1 revealed 4 dead roaches behind the refrigerator, 3 live roaches behind the nightstand, and 2 dead roaches behind the dresser. Housekeeping Staff Member #1 stated .in this room we had another problem .when I open the drawers to the dresser they were running everywhere .
Observation and interview in room [ROOM NUMBER] on 1/9/2023 at 9:38 AM, with Housekeeping Staff Member #1, revealed large amount of small black spots in the inner corners of the cabinets. Housekeeping Staff Member #1 confirmed the black spots were roach feces.
Observation and interview in the room [ROOM NUMBER] on 1/9/2023 at 9:41 AM, with Housekeeper Staff Member #1 revealed several dead roaches behind the nightstand. Housekeeping Staff Member #1 confirmed the roaches on the floor.
Observation and interview in room [ROOM NUMBER] on 1/9/2023 at 9:46 AM, with Housekeeper Staff Member #1 revealed a dead roach in front of the dresser, and 2 live roaches crawled across the floor from underneath the oxygen concentrator.
During an interview on 1/9/2023 at 10:00 AM, Housekeeping Staff Member #1 was asked if roaches in the facility were acceptable. Housekeeping Staff Member #1 stated .No, we don't pull the furniture every day .we pull the furniture once a week .we should not have live roaches in the rooms .should not have crumbs on the floor .that is a breeding ground they can feed off .they [housekeeping staff] are not pulling and sweeping behind furniture .should not have .roaches in the laundry room .the staff break room. Housekeeping Staff Member #1 was asked who was responsible for checking the rooms each day. Housekeeping Staff Member #1 stated .Me and the supervisor .
Observation in the Laundry Washroom on 1/9/2023 at 10:21 AM, with Housekeeping Staff Member #1 revealed a pallet with several buckets of chemicals behind the washer with 2 live roach crawling up one of the buckets, and 2 large roaches crawling on the floor under the dirty linen cart.
Observation in the Staff Break Room on 1/9/2023 at 10:25 AM, with Housekeeping Staff Member #1 revealed 2 roaches crawling on the floor in front of the refrigerator. Housekeeping Staff Member #1 pulled out the refrigerator away from the wall, revealing multiple roaches all over the floor and up the sides of the wall and cabinet. They were to numerous to count.
During an interview on 1/9/2023 at 9:04 AM, Housekeeping Staff Member #1 was asked if she noticed any roaches in the facility. The Housekeeping staff member #1 stated .Yeah [Yes] .when I see them .[roaches] .I let the Maintenance man know .it's when you move the furniture you will see some .it was bad when I first started .
During an interview on 1/4/2023 at 3:04 PM, CNA #11 was asked if he had seen any roaches in the facility. CNA #11 stated .yes .they are everywhere .I have seen them climbing on the walls .they are bad in the Snack/Pantry Room .
During an interview on 1/5/2023 at 4:18 PM, Resident #11 was asked if she had seen any roaches in the facility. Resident #11 stated Yes, it's infested .
During an interview on 1/9/2023 at 8:47 AM, Laundry Staff Member #1 confirmed she had seen roaches in the Laundry Room.
During an interview on 1/10/2023 at 12:36 PM, the Pest Control Technician was asked about the roach infestation in the facility. The Pest Control Technician confirmed there was evidence in the resident rooms of a roach infestation.
During an interview on 1/13/2023 at 12:05 PM, the Administrator was asked if the facility had an effective pest control. The Administrator stated No .