CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure that each resident received adequate supervi...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure that each resident received adequate supervision to prevent accidents for one (Resident #1) of 10 residents reviewed for supervision.
The facility failed to ensure Resident #1 received adequate supervision while Resident #1 was unaccounted for approximately 36 minutes from 5:40 PM to 6:16 PM on 09/04/24 travelling approximately 500 feet while she eloped from the 200 hall exit door. Resident #1 was found approximately 100 feet from the front entrance along the side of the facility.
The Immediate Jeopardy (IJ) template was provided to the facility on [DATE] at 4:10 PM. While the IJ was removed on 10/04/24 at 2:10 PM, the facility remained out of compliance at a scope of isolated and a severity level of potential for more than minimal harm because all staff was not aware of and did not implement the facility's Elopement Prevention, Elopement Response, and emergency codes policies.
This failure could place residents requiring supervision at risk for injury and accidents with potential for more than minimal harm.
Findings included:
Record review of Resident #1's face sheet revealed an [AGE] year-old female with an original admission date of 02/23/22 and a current admission date of 07/09/24. Pertinent diagnosis included Unspecified Dementia (diagnosis given when a person has dementia but it does not fit into a specific type).
Record review of Resident #1's Quarterly MDS assessment section C, cognitive patterns, dated 09/12/24 revealed a BIMS score of 4 (severe impairment).
Record review of Resident #1's care plan revealed the focus The resident is at risk for wandering initiated on 09/05/24. Interventions listed for this focus included:
Assess for fall risk initiated on 09/05/24
Distract resident from wandering by offering pleasant diversions, structured activated, food, conversation, television, book initiated on 09/05/24 and revised on 09/27/24
Identify pattern of wanderings: Is wandering purposeful, aimless or escapist? Is resident looking for something? Does it indicate the need for more exercise? Intervene as appropriate initiated on 09/05/24
If the resident is exit seeking, stay with the resident and notify the charge nurse by calling out, sending another staff member, call system, etc. initiated on 09/05/24.
Monitor for fatigue and weight loss initiated on 09/05/24.
Provide structured activities: toileting, walking inside and outside, reorientation strategies including signs, pictures and memory boxes initiated on 09/05/24.
Further record review of Resident #1's care plan revealed the focus At risk for elopement as evidenced by: actual elopement due to acute confusion initiated on 09/04/24 and revised on 09/05/24. Interventions listed for this focus included:
Assess/record/report to MD risk factors for potential elopement such as: Wandering, Repeated requests to leave facility, statements such as 'I'm leaving' 'I'm going home', attempts to leave facility, elopement attempts from previous facility, home, or hospital initiated on 09/05/24.
Supervise closely and make regular compliance rounds whenever resident is in room initiated on 09/05/24.
Determine the reason the resident is attempting to elope. Is the resident looking for something or someone? Does it indicate the need for more exercise? Intervene as appropriate initiated on 09/05/24.
Provide structured activities: toileting, walking inside and outside, reorientation strategies including sign, pictures, and memory boxes initiated on 09/05/24.
Distract resident from elopement attempts by offering pleasant diversions, structured activities, food, conversation, television, books initiated on 09/05/24.
If the resident is exit seeking, stay with the resident and notify the charge nurse by calling out, sending another staff member, call system, etc. initiated on 09/05/24.
Record review revealed Resident #1 had elopement risk assessments dated 06/04/24 and 09/04/24 with scores of 6 and 17, respectively. Interviews with staff revealed a score of 10 or higher indicated the resident was an elopement risk.
Record review of the provider investigation report dated 09/12/24 revealed the following narrative:
Resident was in COVID isolation down hot zone hallway. an unknown employee put in the master code at the end of the hall to unlock the door. When master code was put in the door remained unlocked and disabled the alarm. Resident wheeled out of her room on the 200 hall and went to the end of the hall. She stated to staff she pushed on the door and it opened up so she went through the door. Resident started to wheel down the facility drive way once she was outside. A passerby saw her and called the facility to notify. Staff went outside to retrieve resident. She was heading back towards the front door and stated she went through a door and was looking for her room. Resident was assessed and no injuries or concerns were noted by staff. Resident was placed on 1:1 due to acute confusion. Once resident returned to original room acute confusion left and resident has had no concerns and has not been wandering.
Further review of the provider investigation report revealed in-services covering Elopement Prevention/Elopement Response were conducted for 61 staff members on 09/05/24 by the ADM.
Further review of the provider investigation report revealed Resident #1 was last seen in the facility before elopement on 09/04/24 at 5:40 PM. Resident #1 was not brought back into the facility until 6:16 PM, 36 minutes later.
In an interview with the MS on 10/01/24 at 12:25 PM, the MS stated the master code could no longer be used to unlock any of the doors. The MS stated he removed the master code from all doors on 09/05/24, the day after the elopement incident. The MS stated that when the master code turned off the alarm and unlocked the door. The MS stated that in order to turn the alarm back on and lock the door, the master code would have to be input again. The MS stated only one code worked on each exit door from the facility now, and the door would only stay unlocked to be opened for several seconds before the alarm sounded if the door was still open. The MS stated he did not know who had access to the master code. The MS stated the master code had been the same since he started working at the facility in 2019. The MS stated he checked the doors every day he works. The MS stated when checking the doors he confirmed the alarms, locks, and codes worked properly from both inside and outside the facility.
Record review of the maintenance logs from 08/01/24 to 10/01/24 revealed the door alarm and lock checks were completed 5 days per week.
During an observation on 10/01/24 at 1:20 PM, this surveyor input the master code into all exit doors in the facility. The master code was ineffective in all doors except for the 100 hall exit door. After inputting the code, the door unlocked and alarm deactivated. The door could freely open and close without it locking or the alarm sounding. The MS was informed the master code still worked on the exit door for hall 100 and he removed the code from the door.
In an interview with the AD on 10/01/24 at 12:46 PM, The AD stated during an elopement, the ADM would be notified and staff would search for the resident. The AD stated she thought there was a 10 minute timeframe to find the resident. The AD stated she could not remember the last elopement in-service received but thought it was about a month ago. The AD stated the facility had not had an elopement in a while and could not remember the last one. The AD stated the last resident she remembered leaving the facility did not really leave the facility but just stepped out the door. The AD stated for an event to be considered an elopement, the resident must have been outside the building heading for the street. The AD stated if a resident left the facility and the staff did not know about it, it would absolutely be an elopement. The AD stated she heard about a resident going out the back door and rolled herself out of the building, but did not get any training about that incident. The AD stated Resident #1 was not the only resident on the COVID unit the day of her elopement. The AD stated the facility did not use wander guards. The AD stated all staff received in-services when there was an elopement and that she had been dealing with the illness of her husband and could not remember if she received the elopement in-service. The AD stated if the elopement occurred at night the ADM would be notified regardless of the time of the elopement. The AD stated while staff were outside looking for the resident, the staff inside would continue searching and conduct a head count of residents.
In an interview with DA H on 10/01/24 at 12:56 PM, DA H stated if she learned about a resident leaving the facility when they were not supposed to she would call 911 and the ADM. DA H stated she had not received any training on elopements and had not received any training on the codes to the exit doors. DA H stated she had not been working at the facility long but felt like she should know the codes and elopement procedures.
In an interview with Resident #1 on 10/01/24 at 1:01 PM, Resident #1 stated her children come to visit her in the facility. Resident #1 stated she currently lived in room [ROOM NUMBER]. Resident #1 stated she enjoyed going outside, playing bingo, and putting on makeup. Resident #1 stated when she wanted to go outside she asked an employee to open the door for her. Resident #1 stated the staff member does not go outside with her, and that they just open the door and let her go out alone. Resident #1 stated that when she went outside she mostly stayed in the front patio area. Resident #1 stated she could not remember moving to the 200 hall, having COVID, or leaving the facility on 09/04/24. Resident #1 stated she had not heard of any residents eloping during her time at the facility.
In an interview with RN E on 10/01/24 at 1:10 PM, RN E was unable to name the correct code to signify an active elopement. RN E stated during an elopement she would stop what she was doing, make sure the doors were locked, and start a head count. RN E stated she would open the door and look outside once she found out who was missing. RN E stated she depended on the door alarms to notify staff that a resident had left the facility. RN E stated staff did receive training on elopement. RN E stated she thought there was a resident that left the facility 2 months ago. RN E stated she received in-service after that elopement but could not remember when specifically. RN E stated she was not at the facility when the elopement occurred. RN E stated once an elopement was identified, the first thing staff should do was look through rooms to try to identify who was missing. RN E stated someone in charge would call a code orange and expect staff to be looking outside while some would look inside. RN E stated resident rounding was typically every 2 hours. RN E stated there were residents that left the facility for dialysis or appointments, but those residents do not sign out during those situations. RN E stated residents signed out when they left with their family on other outings. RN E stated residents that sit just outside the facility did not need to sign out.
In an interview with LVN J on 10/02/24 at 1:03 PM, LVN J stated Resident #1 had good days and bad days regarding exit-seeking behaviors. LVN J stated on Resident #1's bad days she would pack up her belongings and put her bag in the lobby and say she was leaving. LVN J stated when Resident #1 is in that frame of mind she would stay in it all day. LVN J stated on those days Resident #1 would push on the door and ask other people to let her out. LVN J stated Resident #1 displayed these behaviors weekly. LVN J stated if a resident eloped, she would look in the facility to see in the resident is in the building, call the RP, and then start looking outside. LVN J stated there were steps in the elopement procedure. LVN J stated if they noticed a resident missing, it would be communicated to look in the facility for the resident while other staff members would look in the sign out book. LVN J stated staff would call the RP and ADM while also looking outside. LVN J stated all of these steps happen simultaneously. LVN J stated she had an elopement drill months ago but could not recall when. LVN J stated there were no specific roles for staff members. LVN J stated rounding on residents was every 2 hours. LVN J stated she used to have the master code, but did not know who was supposed to know it. LVN J stated she did not think nursing staff were supposed to have the code, but were using it. LVN J stated the master code unlocked the door, and will not relock until the master code was entered again. LVN J stated residents were allowed to go outside, but only with a staff member. LVN J stated she did not know what the score represented on an elopement risk assessment. LVN J stated if a resident was exit-seeking, they could be put on 15-minute checks until it was determined they were no longer necessary. LVN J stated once a resident was triggered for elopement assessment due to a high assessment score, the resident would be assessed by the ADM.
In an interview with CNA F on 10/2/24 at 1:56 PM, CNA F stated she was not at the facility when Resident #1 eloped. CNA F stated when a code orange was called, staff would be looking inside and outside for residents, family would be called, and administration would be notified. CNA F stated the last time she was in-serviced on elopement was about 2 weeks ago.
In an interview with CNA G on 10/02/24 at 2:03 PM, CNA G stated she was not working the day of the elopement. CNA G stated when a code orange was called, staff would start a head count and tell the ADM. CNA G stated staff would check doors and call family. CNA G stated the last time she received an elopement in-service was on 09/05/24. CNA G stated the master code would open the door and keep it open until the master code was put in again to lock the door. CNA G stated she did not know if the code was used on other doors, but knew it was used on the 200 hall back door. CNA G stated a little of everyone used the master code. CNA G stated she heard about Resident #1's elopement the day after it happened. CNA G stated Resident #1 had a history of pushing on doors and trying to get out. CNA G stated last week, Resident #1 packed up all of her belongings and was sitting in the front lobby, pushing on the door occasionally. CNA G stated resident rounding occurred every 2 hours, but that the fell behind sometimes.
In an interview with CNA K on 10/02/24 at 2:52 PM, CNA K stated she was working on the 100 hall the day of Resident #1's elopement. CNA K stated LVN L went outside and brought Resident #1 back inside the facility. CNA K stated she did know the master code, and that nurses would use the master code when taking out linens. CNA K stated the master code must be put in twice - once for unlocking and once for locking the door. CNA K stated she never used the master code. CNA K stated she did not know how many people knew the master code. CNA K stated the 200 hall was typically only used for residents in isolation due to medical conditions. CNA K stated code orange signified an elopement. CNA K stated during an elopement they would start looking for the resident. CNA K stated they would break up into groups and go down their halls. CNA K stated she received a phone call from a friend at 6:14 PM stating Resident #1 was outside the facility. CNA K stated the friend that called her was a former employee at the facility. CNA K stated her friend happened to be driving by the facility at the time Resident #1 was outside towards the front of the building. CNA K stated since the elopement the staff takes extra care to keep an eye on Resident #1. CNA K stated Resident #1 would go to the window and look out and sometimes stated she wanted to go home. CNA K stated Resident #1 sometimes packed her stuff up and sat on the couch in the front lobby. CNA K stated she had not seen Resident #1 try to open any exit doors. CNA K stated the residents in isolation on the 200 hall were rounded on every 2 hours. CNA K stated Resident #1 received her dinner at around 5:00 PM, so that may have been the last time she was seen before the elopement. CNA K stated there were times when no staff were present on the 200 hall with the COVID residents. CNA K stated she had never seen a door unlocked before.
In an interview with the ADM on 10/02/24 at 3:40 PM, the ADM stated there was an attempted elopement back in January of this year. The ADM stated after that attempt the door code was changed and knowledge of it was limited to only staff and contractors. The ADM stated they do elopement drills once per month. The ADM stated during an elopement, the staff would check all rooms and the sign out binder. The ADM stated if the resident was not found in 15 minutes they would start notifying all important people. The ADM stated they would search the inside and the outside at the same time. The ADM stated they did 4 elopement drills in September 2024. The ADM stated on 09/04/24, the ADON called her at 6:17 PM to inform her that Resident #1 had exited the 200 hall door. The ADM stated the ADON pushed on the 200 hall door and it was not locked. The ADM stated someone had put in the master code and disabled the locks and alarm. The ADM stated Resident #1 was put on 1 to 1 for 24 hours after the elopement. The ADM stated after the 1 to 1 ended, Resident #1 was checked on every 15 minutes for the next few days. The ADM stated Resident #1 was assessed after the elopement and no injuries were found. The ADM stated that resident used to pack up her belongings and say she was going home, and that she still did so occasionally but never attempted to leave. The ADM stated the master code was only supposed to be known by her, the maintenance supervisor, and the housekeeping supervisor. The ADM stated she had never seen anybody use the code except during an evacuation. The ADM stated she had spoken to MS about changing the master code before the elopement, but that he told her he did not know how to change the code from the doors. The ADM stated she did not know how many employees knew the master code at the time of Resident #1's elopement. The ADM stated MS figured out how to remove the master code on 09/05/24, the day after the elopement, and proceeded to remove the master code from all exit doors at that time. The ADM stated they did an elopement assessment on every resident after the elopement of Resident #1. The ADM stated they did door checks 3 times per day for the next 8 days after the elopement of Resident #1. The ADM stated 3 residents were in the 200 hall on 09/04/24. The ADM stated cameras are in the facility, but that they cannot record anything. The ADM stated she had been trying to get the cameras fixed for many months.
In an interview with CNA M on 10/02/24 at 5:54 PM, CNA M stated she was working on the 300 hall during the elopement of resident #1. CNA M stated she heard CNA K yell out at approximately 6:15 PM that Resident #1 got out of the unit. CNA M stated when a code orange is called, the staff would go down every hall and check every room for the resident. CNA M stated they would search by themselves. CNA M stated the last time she was part of an elopement drill was in November 2023 on day shift. CNA M stated she was aware of the master code and knew the combination. CNA M stated all of the staff should have been aware of the master code. CNA M stated she had seen other CNA's and housekeepers use the master code. CNA M stated Resident #1 was not allowed to go outside without supervision.
In an interview with CNA N on 10/02/24 at 6:22 PM, CNA N stated she was working on the 100 hall during the elopement of Resident #1. CNA N stated she did not hear any commotion prior to seeing other staff members wheeling in Resident #1 through the front door at around 6:15 PM. CNA N stated during a code orange they would assess the situation and try to find the resident. CNA N stated she would search her hall. CNA N stated they would search the entire inside of the facility before checking the outside. CNA N staff members would search their respective assigned hallways and rooms. CNA N stated she did not recall the last time she took part in an elopement drill. CNA N stated there were 2 codes that worked on the doors. CNA N stated she knew the master code, but did not use it. CNA N stated she had never seen anyone use the master code. CNA N stated she had never seen one of the exit doors unlocked. CNA N stated Resident #1 was not allowed to go outside unsupervised.
In an interview with LVN L on 10/02/024 at 6:39 PM, LVN L stated he was the one who wheeled Resident #1 inside the facility after CNA K received the phone call which notified the facility her elopement. LVN L stated Resident #1 was approximately 100 feet from the entrance of the facility when he got to her. LVN L estimated it would take Resident #1 approximately 3-5 minutes to get from the 200 exit door to where he found her outside. LVN L stated when he reached Resident #1 outside she told him she was trying to go home. LVN L stated he performed a head-to-toe check on Resident #1 after getting her back to the 200 hall and found no injuries. LVN L stated he checked the 200 hall exit door and found that it was closed, but unlocked. LVN L stated he was aware there was a code that turned off the locks and alarms, but he did not know the code. LVN L stated he had seen other staff use the master code. LVN L stated he thought most staff knew the master code. LVN L stated during an elopement, his role was to inform everybody, and if the resident could not be found in 15-30 minutes he would call the police. LVN L stated during an elopement, they will search the inside first, and then move to the outside if they could not find the resident. LVN L stated he was in-serviced on elopements after this incident. LVN stated he has never been part of an elopement drill in 3-4 years on night shift. LVN L stated Resident #1 was not allowed to go outside unsupervised.
In an interview with LVN O on 10/02/24 at 7:18 PM, LVN O stated she checked the door after Resident #1 was returned to her room and found that it was closed, but was not locked and the alarm was not set. LVN O stated she knew the master code, but she had never used it. LVN O stated the only time she could remember the master code used was during an emergency. LVN O stated during a code orange she would do an initial sweep and yell out for everyone to start searching their hallways and rooms. LVN O stated they would sweep the inside a second time before searching the outside. LVN O stated a staff member notify the ADM and then call the police if the resident could not be located. LVN O stated she did not think Resident #1 was allowed to go outside unsupervised. LVN O stated she received an in-service on elopement after this incident. LVN O stated she thought the last elopement drill on her night shift was 2-3 years ago when a resident was found in the kitchen bathroom.
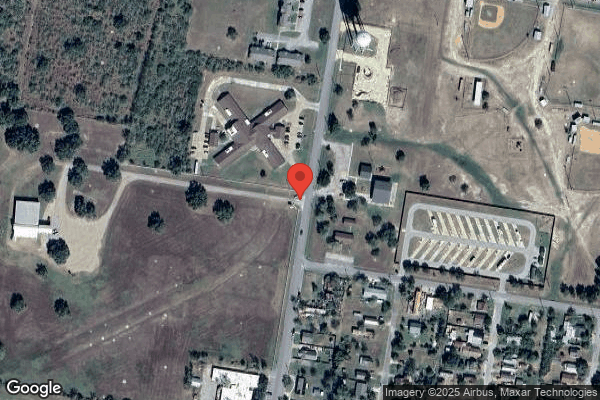
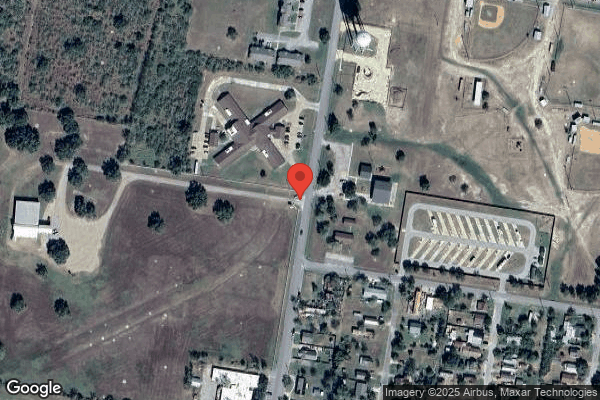
During an observation on 10/03/24 at 9:15 AM, this surveyor paced out the distance from the 200 hall exit door to where LVN L stated he found Resident #1 during her elopement. The distance between where Resident #1 was found and the 200 hall exit door was approximately 500 feet. Resident #1 was also approximately 100 feet from a street when she was found by LVN L.
Record review of the facility policy Elopement Prevention dated 10/27/10 reflected the following:
Physical Plant
1. All facility exits that residents have access to will have a device in place to alert staff of possible elopement attempts.
Examples of these devices:
Wanderguard system
Keypad exit magnetic locks
Keyed Alarms
Secured Unit
Or a combination of the above.
Staff will receive training during their orientation process and then annually regarding:
Elopement prevention
Operation of all exit devices
Actions to take if elopement occurs
Record review of the facility policy Elopement Response dated 10/27/10 reflected the following:
A resident is determined missing when he/she leaves the facility without the staff's knowledge.
Deployment Procedure:
A. Charge Nurse on each unit send staff down each hall to check each room, including bathroom, closet and bed for correct resident.
B. Check all rooms on the hall including tub and bathrooms, linen closets and any recreation rooms. Check all common areas and offices.
If unable to locate resident in the building, proceed as follows:
A. Unaffected Area - Charge Nurse designates one CNA per hall to remain on unit along with him/herself and sends remaining staff to affected area.
B. Affected Area - Charge Nurse assigns staff to specific outside areas to ensure that all surrounding areas are searched.
C. After 30 minutes, if the resident has not been found, the following calls must be made:
Report missing resident to the police
Update responsible party
Update administrator/ VP of Risk Management, ADO, COO, and VP of Clinical Services
Record review of the undated facility policy Emergency Code Reference reflected Orange= Elopement or Missing Resident
An Immediate Jeopardy (IJ) was identified on 10/03/24 at 4:10 PM. The IJ template was presented to the ADM, and a plan of removal was requested.
PLAN OF REMOVAL FOR IMMEDIATE JEOPARDY
Problem: F689 Free of Accident- Elopement
Interventions:
Elopement risk assessments completed for all residents in facility on 10/3/24.
Any resident identified as an elopement risk had monitoring initiated in point of care by RCN on 10/3/24 for CNAS to report any exit seeking behaviors immediately.
Any residents identified as an elopement risk had a care plan completed by RCN on 10/3/24 indicating elopement risk for charge nurses to review.
Administrator Completed check of all facility exit doors on 10/3/24 to ensure they are functioning properly.
Inservices
Staff (to include new hires and agency) were in serviced on the following topics 10/3/24, any staff not present for in servicing will not be allowed to assume their duties until in serviced. Admin or designee will staff have received the below in-services.
Elopement policy
Elopement prevention policy
Emergency code reference
Facility Sign out book
Administrator completed Inservice with Maintenance director on 10/3/24 regarding Monitoring Door codes/locks to ensure they are functioning appropriately 5 times a week.
Monitoring:
Maint Director or designee will check Door alarm or lock function will be monitored 5times a week for each exit door to ensure they are functioning appropriately.
Documentation will be maintained in a monitoring log. This monitoring will continue for 6 weeks and periodically thereafter to ennsure compliance.
[NAME] or designee will conduct 2 elopement drills per week, 1 drill between 6am-6pm and 1 drill between 6pm and 6am.
Elopement drill will be completed for 6 weeks and periodically there after to ensure compliance.
Don or designee will review resident sign out book 5 times a week to ensure residents sign in and out of facility correctly x 6 weeks and periodically there after to ensure compliance. Documentation will be placed on monitoring log
DON /Designee will review 2 times a week for all new admits/re admit or post elopement or attempted elopement to ensure that any residents at risk for elopement have interventions in place x 6 weeks and periodically there after to ensure compliance. Documentation will be placed on monitoring log.
The [Medical Director] was notified of this plan on 10/3/24 and an off cycle QAPI plan was initiated regarding this event.
Verification of Plan of Removal:
In an interview with RN A on 10/4/24 at 10:35 AM, RN A stated if there was an elopement, a code orange would be called to alert staff to start a head count of residents and start looking inside and outside of the facility as well as closets, showers, and anywhere someone could be. RN A stated staff would also check the out on pass binder to see if the resident was out of the facility. RN A stated staff would also notify administration. RN stated if a resident was not found within 30 minutes of searching, local law enforcement would be notified. RN stated the family of the resident would be notified if resident was found or not.
In an interview with RN S on 10/4/24 at 10:43 AM, RN S stated if code orange was called, staff start a head count of residents and start looking everywhere, every crack and crevasse. RN S stated staff would look outside simultaneously while someone was checking the out on pass binder. RN S stated if a resident was not found within 30 minutes, local law enforcement would be notified to report a missing person. RN S stated there was no master code utilized and all doors have alarms on them and lock when closed.
In an interview with CNA N on 10/04/24 at 10:52 AM, CNA N stated she would start by notifying staff that is working, divide the halls among staff, and begin searching for the resident. CNA N stated she would next call the DON, ADM, and notify family. CNA N stated after searching for 30 minutes she would call the police. CNA N stated the elopement policies were in the black binder at the nurse's station. CNA N stated the emergency code for a missing resident was orange. CNA N stated the sign out book was being used.
In an interview with SNA C on 10/4/24 at 10:51 AM, SNA C stated if a code orange was called staff would split up and start looking for the resident and begin a head count. SNA C stated staff would start looking in all the rooms, kitchen, bathrooms, closets, showers, as well as the out on pass binder to see if the resident possibly left out on pass with family. SNA C stated if a resident was not found within 30 minutes, staff, the resident's family, and the police would be notified. SNA C stated there was no master code and all the doors locked once the door closed after putting in the code to be let out. SNA C stated the doors had an alarm and would go off and alert staff that someone was trying to exit the facility without a code.
In an interview with SNA B on 10/4/24 at 10:57 AM, SNA B stated if a code[TRUNCATED]
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to send a copy of the notice of transfer or discharge, and the reaso...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to send a copy of the notice of transfer or discharge, and the reasons for the transfer or discharge in writing to the resident, resident representative, or the Office of the State Long-Term Care Ombudsman for one of six residents (Resident #8) reviewed for transfer and discharge.
The facility failed to notify the Resident and Resident Representative of the transfer or discharge and the reason in writing and in a language or manner they understand.
This failure could affect residents at the facility by placing them at risk of being discharged and not having access to available advocacy services, discharge/transfer options, and the appeal processes.
Findings included: Record review of Resident #8's face sheet revealed she is an [AGE] year-old female admitted to the facility on [DATE]. Diagnoses included Unspecified Dementia, Syncope, Malnutrition, Urinary Tract Infection, Pain, Muscle Wasting, Depression, and Anxiety.
Interview with Resident #8's RP, 9/26/24 at 10:51 AM, stated that R#8 is doing so much better since being moved to an assisted living facility with a memory care unit. She stated she is eating better, gaining weight, not falling, taking less medication, and walking better. She stated she was grateful R#8 had to be sent to the hospital because it was the doctor in the hospital that found that she was being over medicated. She felt like no one was listening to her at the other facility, and that R#8 was just kicked out. She stated they were not given a notice or anything but were told that they needed to find another facility or take her home and needed to know by the end of the day when and where she would be going. They had to have her out the next day.
Interview with CNA D, 9/26/24 at 1051 AM, she denied remembering R#8's fall. Remembered the R#8 wandering frequently. CNA D does not recall the resident or family reporting abuse or neglect. She stated R#8 was prone to falls so fall precautions used were: lower bed, fall mat, therapy evals if needed.
Interview with ADON, 9/26/24 at 12:42 PM, she sated resident #8 had a UTI and was confused and trying to use the trashcan as a toilet. She stated resident #8 was more independent when she arrived, but gradually became more forgetful. ADON remembered having a disagreement with the previous DON about the medications and remembered the psych doctor had ordered clonazepam for her, and when resident #8 started the medication, she had a fall while trying to sit on the couch and missed. Family had stated they didn't think she needed to be on the medicine. ADON brought to the DONs attention that they were giving her a whole tablet instead of a half tablet. She stated they were giving her the whole tablet when she thought she was supposed to only be getting ½ tablet but doesn't remember the exact situation. ADON felt like the previous DON was covering something up, so she thinks the previous DON got the order for the whole tablet. ADON didn't feel the resident needed that high of a dose. ADON stated the previous DON was accusing the LVNs of taking Resident #8s meds but refused to drug test the nurses. She does remember resident having diarrhea but doesn't remember her being in briefs. She remembered her exiting out the door, but she thinks it was when a family member had let her out or she followed a family member out the door. She stated that resident #8 would stand by the door and push until the alarm went off trying to get out. She also stated she thinks residents must have a 30-day notice prior to discharge.
Interview with Administrator, 9/26/24 at 2:30 PM, she stated if it is no longer considered a safe facility for the resident, such as elopement, the facility will give them shorter notice, but unsure of the exact time frame the notice should be given in. Other than elopement it's a 30-day notice. Stated she didn't do a written notice with the family or resident that she can recall but will look for copy of it. Discharge was related to wandering and medication issues. She stated family kept wanting to try something new, but not giving it time to work. She does not remember the med error about her getting a whole tab, but remembered there was something going on in relation to the family not wanting that medication, and wanting it changed to something else, but denied it being a med error. Administrator denied remembering if there was any abuse or neglect reported to her, but if it was reported, she would investigate within her 2-hour window and report to state if needed. After checking for a discharger or transfer notice, she came back and stated she never gave them a written discharge notice.
Interview with CNA E, 9/27/24 at 9:48 AM, she stated she is trained on abuse, neglect, and exploitation all the time, as well as falls and incidents. Last training was recently, sometime this month, but she doesn't remember the exact date. CNA E denied ever seeing abuse in the facility. She stated she would report to the administrator or person in charge if the administrator was gone. CNA E did not remember Resident #8 falling, as well as her diarrhea and being in briefs. She stated they don't double up on briefs, and also did not remember hearing of her being over medicate. Stated she has heard of other CNAs doubling up on briefs, but no one on her team does this because it is not allowed. CNA E denied knowing anything about Resident #8's discharge process or paperwork.
Interview with CNA F, 9/27/24 at 10:35 AM, she stated Resident #8 was always trying to get out the door, and she did get out one day. CNA F stated they try to redirect residents from the doors and getting out the door. If a resident is missing, CNA F stated she would reach out to the van driver, who keeps up with the list of residents that have left the facility. CNA F denied ever hearing of mistreatment or abuse with Resident #8. CNA F stated she never saw Resident #8 trying to use trashcan as restroom, and she never heard any complaints that she was being over medicated. CNA F denied knowing anything about Resident #8's discharge process or paperwork.
Interview with LVN G, 9/27/24 at 11:00 AM, she stated that she does remember a chaotic time with trying to get the resident's medications straight, but it wasn't due to medication errors, but due to every time the doctor ordered or changed something, the family wouldn't give it time to work, and would complain to have it changed or adjusted. She stated that there was never a med error because the med order was clarified with the provider to be sure they were giving it appropriately, and she remembered the provider specifically telling them the order was correct, and to give as ordered. She denied remembering if the resident was given appropriate transfer or discharge paperwork.
Interview with Director of Medical Records, 9/27/24 at 4:45 PM, she stated that written notices are rarely hand delivered anymore, but they typically email them. She stated that if the nurses do not put their part in correctly to discharge the resident home, then the system does not trigger her to given written discharge/transfer notice. She also stated that in conjunction to Resident #8 never having a written discharge or transfer notice, she could not find three of the discharge notices on the list that were supposed to have been done. She stated they recently had a meeting to discuss better ways of tracking and improving written notices, but are still working on it, and that she is going to mention this issue in the next meeting.
Record review of Discharge summary dated [DATE] revealed Resident #8's discharge summary was completed, but there is no written transfer or discharge notice. Discharge summary revealed that plan of care was reviewed, and there was an elopement risk and wandering behavior. Discharge summary also revealed that discharge options were reviewed with family, and family understands resident is not safe here, and they consent to resident being transferred.
Record review of Resident #8's progress notes dated 1/20/24 revealed that resident had exited the facility behind someone leaving, and that 15-minute observations were conducted, as well as an emergency meeting between family and facility management was to be held on 1/22/24.
Record review of facility Discharge and Transfer policy, effective 12/2017 and revised 4/10/24, under subsection Facility Initiated Discharge, revealed the facility may initiate transfers and discharges in the following circumstances: necessary for the resident's welfare and resident's needs cannot be met. It also revealed, under subsection Notification of Discharges, that for a facility initiated non-emergent transfer or discharge of a resident, the facility will notify the resident and the resident's representative of the transfer or discharge and the reasons for the move in writing and in a language and manner they understand with at least 30 days notice prior to discharge, and additionally the facility will send a copy of the notice of transfer or discharge to the representative of the Office of the Stated Long-Term Care (LTC) Ombudsman.
Record review of an Admission/Discharge To/From Report dated 9/26/2024 revealed 5 separate residents listed as transfer or discharges but only showed written notifications done for three out of the five residents listed. Resident #8 is not listed as written transfer or discharge notification was never even initiated.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to revise and review the care plans for 2 of 9 residents (R#4 and R#...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to revise and review the care plans for 2 of 9 residents (R#4 and R#7) whose care plans were reviewed, in that:
1)The facility failed to ensure R#4's care plans to reflect actual falls.
2)The facility failed to update R#7's care plans to reflect actual falls.
These failures could place residents at risk of receiving incorrect care and cause health complications with subsequent illnesses or injury.
Findings were:
1)Record review of R#4's face sheet revealed an [AGE] year-old female with an admission date of 08/17/20. Diagnoses included cognitive communication deficit, dizziness, muscle wasting, other symptoms and signs involving the musculoskeletal system, abnormalities of gait and mobility, diabetes with neuropathy, major depression, osteoporosis, arthritis, dementia, history of falling, sacrum fracture, and sepsis from a UTI. R#4's quarterly MDS revealed a BIMS of 7, indicating moderate cognitive impairment. She required minimal assistance with dressing and footwear, set-up with oral and personal hygiene, and was independent with eating. She had a wheelchair and could self-propel. She was incontinent of bladder and bowel.
Record Review of R#4's quarterly care plan dated 08/11/24 revealed she was at risk for falls r/t psychotropic medication use and dx of dementia Abnormal gait Date Initiated: 06/05/2024 Revision on: 09/27/2021. All interventions were dated 09/27/21 and included anticipate needs, call light and personal items within reach, family education, ensure appropriate footwear, review and determine the cause of past falls. Fall mat and bed low were the most recent entries in the care plan with initiation and revision dates of 06/23/24. Actual unwitnessed falls with injury dated 09/18/23 and 09/24/23 were not in R#4's care plan.
In an interview with CNA D on 09/26/24 at 10:51 am, she stated she was in-serviced over falls and abuse but did not remember the date and stated it was recently.
In an interview with RN A on 09/26/24 at 10:55 am, she stated the process after a resident had fallen either witnessed or unwitnessed, whoever first discovered a fall would report to her, and she would assess the resident, then notify the ADM, DON, and ADON. She said she was in-serviced about two weeks ago on falls and ANE. She said falls were definitely supposed to be in the care plans.
In an interview with the ADON on 09/26/2024 at 12:45 pm, she stated they document these incidents. She said the process for falls was the nurse would assess residents, notify the doctor, DON, Admin, ADON, and family, as well as call EMS if the resident needed to be sent out. She said she could not remember the most recent fall in-service, but stated they got in-serviced sometimes with falls as well as monthly at meetings.
Interview with the ADM on 10/04/2024 at 3:00 pm revealed actual falls with injury should be in the care plan. She said the DON and nurses should be entering information and updating care plans timely. She said the care plans were important because staff use the care plans to know what was going on with the resident, so the care plans needed to be updated as events or changes happen, not just quarterly.
In an interview with the ADM on 10/07/2024 at 3:50 pm, she stated the facility did not have a policy for residents signing out when they left the facility and the sign out logs were the only means they had of keeping track of the whereabouts of residents when they left the facility for outside activities/program for senior adults, or when they left out on pass. She said falls were supposed to be updated in care plans when they happen, otherwise care plans should be updated quarterly.
In an interview with the MDS nurse on 10/07/2024 at 2:51 pm, she stated almost every resident had a generic order for may go out on pass with meds, but those going to the special offsite activities/program for senior adults should have orders specific to that, because those orders would come from the psychiatrists. She said falls should be in the care plans.
Record review of R#4's fall events revealed she had actual unwitnessed falls with injury (skin tear) dated 09/18/23 and 09/24/23 for which she was hospitalized for altered mental status (AMS).
Record review of R#4's hospital records dated 09/19/23-09/22/23 indicated R#4 had fallen at the facility due to AMS because of a urinary tract infection (UTI).
Record review of the facility's eTransfer form dated 01/03/24 indicated R#4 was sent to the local hospital after a fall for AMS. This fall was not addressed in R#4's care plan.
Record review of R#4's weekly fall risk assessments dated 04/17/24-06/06/24 indicated she was a high fall risk. Quarterly fall risk assessments dated 01/12/24 indicated R#4 was a high fall risk. Fall risk assessments dated 04/13/23 and 06/29/23 indicated R#4 was a high fall risk.
2)Record review of R#7's face sheet revealed an [AGE] year-old female with an original admission date of 09/26/21 and a re-admission on [DATE]. Diagnoses included encephalopathy (a group of conditions of damage or disease that affects the brain causing brain dysfunction), dementia, diabetes with neuropathy, right leg fracture, abnormalities of gait and mobility, muscle weakness, lack of coordination, major depression, chronic kidney disease, and fatigue. R#7's quarterly MDS dated [DATE] revealed a BIMS of 2, indicating severe cognitive impairment. She required substantial assistance with footwear, partial assistance with lower body dressing, and toileting, supervision with showering, upper body dressing, oral and personal hygiene, and was independent with eating, and transferring. She had a manual wheelchair and could self-propel. She was frequently incontinent of bladder and always incontinent of bowel. Her active diagnosis was other neurological conditions.
Observation and interview with R#7 on 10/07/2024 at 9:40 am revealed she was in bed sleeping. Her hair appeared clean, and she had on clean clothing. There was a fall mat on the floor at bedside, the bed was against the wall on the other side. The bed was in low position. She was able to swallow crushed meds in pudding and hold and drink a nutrition supplement. She was awakened by the nurse for meds. She was able to answer simple questions but did not remember falling or breaking her hip.
In an interview with CNA D on 09/26/24 at 10:51 am, she stated she was in-serviced over falls and abuse but did not remember the date and stated it was recently.
In an interview with RN A on 09/26/24 at 10:55 am, she stated the process after a resident had fallen either witnessed or unwitnessed, whoever first discovered a fall would report to her, and she would assess the resident, then notify the ADM, DON, and ADON. She said she was in-serviced about two weeks ago on falls and ANE. She said falls were definitely supposed to be in the care plans.
In an interview with the ADON on 09/26/2024 at 12:45 pm, she stated they document these incidents. She said the process for falls was the nurse would assess residents, notify the doctor, DON, Admin, ADON, and family, as well as call EMS if the resident needed to be sent out. She said she could not remember the most recent fall in-service, but stated they got in-serviced sometimes with falls as well as monthly at meetings.
Interview with the ADM on 10/04/2024 at 3:00 pm revealed actual falls with injury should be in the care plan. She said the DON and nurses should be entering information and updating care plans timely. She said the care plans were important because staff use the care plans to know what was going on with the resident, so the care plans needed to be updated as events or changes happen, not just quarterly.
In an interview with LVN J on 10/07/2024 at 9:43 am revealed she had known R#7 for a couple of years. She said on or around 04/18/24, R#7 was walking with her walker towards the 400 hall. She said she heard a crash, in front of the MDS office. She said R#7 was on the floor with her walker on top of her. She said she assessed R#7 and discovered hip pain. She said she called 911 & transferred R#7 to the local hospital. LVN J said R#7 had her same shoes (sneakers) on as usual. She said R#7 could not say why or how she fell. She said no one saw it happen. LVN J said R#7 was in the hospital for several days, up to a week. She said R#7 had surgery and had not been able to get back to her baseline. LVN J said physical therapy was working with her and she could take some steps. LVN J said R#7 could walk around the facility all day but now she can't. She said sometimes R#7 propels herself in her wheelchair, but it's as if she forgets and starts scooting the chair. LVN J said R#7's mentation had not changed-she was always forgetful because of her dementia. She said R#7 knew her name and could answer simple questions in the moment. LVN J said the ADON & DON should be updating care plans-the charge nurses don't really do that. She said it was important to have updated care plans so everyone was aware of what was going on, such as what could and could not be done or do. She said she did not often look at care plans, unless there was a new resident. She said she would not know if they were updated or not. She said care plans were extremely important for communication you learn a lot. She said her patients pretty much stayed the same. She said since she was a charge nurse, she got information in report. She said she did not know if the CNAs had access to the care plans. She said CNAs used the [NAME]-that's where they would find changes. She said the ADON and DON updated the [NAME]'s.
In an interview with the MDS nurse on 10/07/2024 at 10:20 am revealed she did the comprehensive care plans and the nurse's input anything outside of the quarterly, such as diet changes, falls, etc. She said she audited care plans quarterly but could not say when she last audited a care plan.
Record review of R#7's profile revealed her care plan conference was 322 days overdue - 11/17/23. R#7's quarterly care plan dated 08/02/24 revealed she was at risk for falls r/t psychotropic medication use and dx of dementia and Abnormal gait Date Initiated: 09/27/2021 Revision on: 06/05/2024. The goal included she would not sustain serious injury through the review date. Date Initiated: 09/27/2021 Revision on: 09/30/2022 Target Date: 08/18/2024. She would be free of falls through the review date. Date Initiated: 06/29/2023 Revision on: 06/30/2023 Target Date: 08/18/2024. Interventions included: Anticipate and meet the resident's needs. Date Initiated: 09/27/2021, Be sure the resident's call light, is within reach and encourage the resident to use it for assistance as needed. Date Initiated: 09/27/2021, educate the resident/family/caregivers about safety reminders and what to do if a fall occurs. Date Initiated: 09/27/2021. Encourage the resident to participate in activities that promote exercise, physical activity for strengthening and improved mobility Date Initiated: 09/27/2021, Revision on: 10/04/2021. Ensure that the resident is wearing appropriate footwear when ambulating or mobilizing in WC Date Initiated: 09/27/2021, Revision on: 10/04/2021 o Keep furniture in locked position. Date Initiated: 09/27/2021. Keep needed items, water, etc, in reach. Date Initiated: 09/27/2021. Medication review Date Initiated: 06/30/2023. Place the bed in the lowest position while resident is in bed Date Initiated: 06/23/2024. Pt evaluate and treat as ordered or PRN. Date Initiated: 09/27/2021. Review information on past falls and attempt to determine cause of falls. Record possible root causes. Alter remove any potential causes if possible. Educate resident/family/caregivers/IDT as to causes. Date Initiated: 09/27/2021. Staff x 1 to assist with transfers Date Initiated: 09/27/2021. The resident needs a safe environment with: even floors free from spills and/or clutter; adequate, glare-free light; a working and reachable call light, the bed in low position at night; Slide rails as ordered, handrails on walls, personal items within reach) Date Initiated: 09/27/2021 Revision on: 10/04/2021. The resident needs activities that minimize the potential for falls while providing diversion and distraction Date Initiated: 09/27/2021. The resident uses fall mat x1 while in bed Date Initiated: 06/23/2024 Revision on: 06/23/2024. The resident is on Pain medication Therapy Date Initiated: 02/08/2023 Revision on: 03/07/2023. Monitor for increased risk for falls Date Initiated: 03/07/2023. The actual fall with injury on 04/18/24 was not reflected in the care plan. The most recent revision to R#7's care plan was 06/23/24.
Record review of R#7's nursing progress notes dated 04/18/24 at 2:13 am revealed notified by staff that resident was lying on floor between fridge and bed, resident alert to name, follows commands, denied any acute pain. ROM (range of motion), VS (vital signs), and neuro status is WNL (within normal limits) for residents' baseline. No bumps, bruises or injuries noted. All proper parties notified. 4/18/2024 at 10:05 am Activity Note Text: Resident was ambulating with her walker to the 400 Hall and fell, this nurse heard a loud noise and upon stepping out of a room, resident was noted to be laying on the floor with her walker underneath her, resident 1st c/o pain to her right hip, then c/o pain to her left hip. [NAME] removed from underneath resident, otherwise resident not moved, 911 immediately called, VS taken all WNL. Per EMTs (emergency medical technician) resident transferred to stretcher via inflatable back board. Resident transported to the local hospital. 4/18/2024 10:05 Nursing Progress Note Text: This nurse was in room [ROOM NUMBER] when a loud noise was heard, looked out the door and saw the resident lying on her back on the floor on top of her walker. Staff rushed to resident, who stated that she fell, but she doesn't know why. Also c/o of bilat hip pain, 911 called for emergent transfer to local hospital for possible hip fx. MD/RP notified and agreed with transfer. VS taken and WNL. Resident not moved until EMTs arrived and transferred to stretcher.
Record review of x-ray report dated 04/18/24 revealed R#7 had a right hip fracture.
Record review of R#7's quarterly fall risk assessments dated 04/13/23, 06/29/23, 01/12/24, 04/17/24, 04/18/24, 04/22/24, 05/07/24, 05/16/24, 05/30/24 and 06/06/24 were scored high risk from 13-22.
Record review of the facility's undated Comprehensive Care Planning policy documented .Resident's preferences and goals may change throughout their stay, so facilities should have ongoing discussions with the resident and resident representative, if applicable, so that changes can be reflected in the comprehensive care plan. The resident's care plan will be reviewed after each admission, quarterly, annual and/or significant change MDS assessment, and revised based on changing goals, preferences and needs of the resident and in response to current interventions.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide a safe, functional, sanitary, and comfortable environment for residents, staff, and the public in one (300 hall) of f...
Read full inspector narrative →
Based on observation, interview, and record review, the facility failed to provide a safe, functional, sanitary, and comfortable environment for residents, staff, and the public in one (300 hall) of four halls reviewed for environment.
The facility failed to ensure the shower room on the 300 hall was closed and locked.
This failure could place residents, staff, and visitors at risk for falls and result in serious injury.
The findings:
During an observation on 10/4/24 at 3:55 p.m., the 300 hall shower room was closed but unlocked.
During an observation on 10/9/24 at 9:36 a.m., the 300 hall shower room door was propped open with door stopper. No residents were observed in the hall.
In an interview and observation on 10/4/24 at 3:56 p.m., SNA C was able to open 300 hall shower room. When SNA C tried to lock the shower door, the door did not lock. SNA C stated the shower door lock had been broken for maybe about a week but could not remember and stated she thought it was reported but did not know. SNA C stated all shower rooms should be locked at all times for resident safety.
In an interview on 10/4/24 at 4:01 p.m., the DON was able to open the shower room door. The DON was able to lock the shower door while it was open, so the keypad is working. The DON tried to lock the door while closed and door would sound like it was locking and would not stay locked when the handle was turned down. The DON stated this was the first time she was made aware the shower room on the 300 hall was not locking.
In an interview on 10/4/24 at 4:00 p.m., the MS stated the 300 hall shower door was not locking for about 6 weeks. The MS stated he inspected the door and that is when he realized the lock was broken. The MS stated he spoke with administration about the lock being broken and was informed they would have to order a new one, but the locks were on back order and was waiting to get a new lock. The MS stated he tried to fix the lock a few times, but it was not working. The MS stated he was going to swap out the locks on the DON's door so the 300 hall shower room could lock properly.
Record review of Maintenance Log/ Work Orders dated 7/1/24 to 10/3/24 reflected no work order or for 300 hall shower room door/lock.
In an interview on 10/9/24 at 9:40 a.m., RN E stated all shower doors are supposed to be closed and locked for resident privacy, safety, and to prevent falls. RN E stated she did not notice the shower door was propped open as she was in a resident's room and just came out. RN E stated staff do get in-services on making sure shower rooms are closed and locked when not in use periodically but could not state when the last one was.
In an interview on 10/9/24 at 9:45 a.m., CNA D stated there was a new shower aide that worked that morning who just and thinks she could have been the one to leave the shower door open but was not sure. CNA D denied leaving the shower door open and stated her, and another aide were in a room with a resident and did not see the shower door open or she would have closed it for resident safety. CNA D stated last week staff had an in-service on making sure shower rooms/storage rooms were locked at all times.
In an interview on 10/9/24 at 9:45 a.m., SNA C stated she thought a new shower aide that just started working at the facility was the one to leave the shower door open. SNA C denied leaving the shower door open and stated she did not see the shower door open as she was helping a resident in the room. SNA C stated there was an in-service on making sure shower rooms/storage rooms were locked at all times last week.
In an interview on 10/9/24 at 10:30 a.m., the DON stated the new CNA was not giving showers on the 300 hall. The DON stated the CNA's working the 300 hall were the ones scheduled to give showers that morning. The DON stated all staff, including new staff had training/onboarding training on all shower doors should be closed and locked at all times. The DON stated she was going to perform another in-service on keeping shower doors closed and locked immediately. The DON stated it was important all shower room doors were kept closed to ensure resident and visitor safety.
Record review of in-service on shower rooms being locked at all times dated 10/7/24.
Record review of the facility's Hazardous Communication Program policy dated 2003 stated:
37. Doors to hazardous areas must be kept closed unless provided with an approved hold-open device such as an alarm activated magnetic hold-open device. Doors must be single-swing type with positive latching hardware.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to develop and implement a comprehensive person-centered...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to develop and implement a comprehensive person-centered care plan for each resident, that included measurable objectives and time frames to meet the resident's physical, mental and psychosocial needs, for six residents (R#6, R#2, R#3, R#5, R#18, and #19) of sixteen residents reviewed for comprehensive care plans, in that:
1)The facility failed to ensure floor mats were in place for R#6 while in bed as stated in the care plan.
2)The facility failed to ensure R#2's care plans reflected he was eligible to attend special offsite activities/program for senior adults without signing out in the sign-out logs.
3)The facility failed to update R#3's care plans to reflect she was eligible to attend special offsite activities/program for senior adults without signing out in the sign-out logs.
4)The facility failed to update R#5's care plans reflected he was eligible to attend special offsite activities/program for senior adults without signing out in the sign-out logs.
5)The facility failed to update care plans for R#18 who had bruising and swelling to her finger and R#19 had a large bruise to her right upper arm.
6)The facility failed to update care plans for R#19 who had a large bruise to her right upper arm.
These failures could place residents at risk for not receiving necessary care or services to address their needs and prevent subsequent illnesses or injury.
The findings included:
1)Record review of R#6 ' s face sheet dated [DATE] reflected an [AGE] year-old-female with an original admission date of [DATE]. Diagnoses included heart failure, dementia (loss of memory, language, problem-solving and other thinking abilities that affect daily life), muscle weakness, diabetes mellitus (insufficient production of insulin in the body) and unsteadiness on feet.
Record review of R#6 ' s care plan dated [DATE] with a revision date of [DATE] stated Resident #6 was at risk for falls related to hypertension and diabetes mellitus. Interventions included floor mats at bedside when bed was in use.
Record review of R#6 ' s MDS dated [DATE] reflected a BIMS of 2 (severe cognitive impairment).
In an interview and observation on [DATE] at 9:53 a.m., the MDS Coordinator observed R#6's room with this surveyor and confirmed R#6 did not have floor mats at bedside while R#6 was in bed as stated in the care plan. The MDS Coordinator stated R#6 should have floor mats placed beside the bed while R#6 was in bed. The MDS Coordinator stated sometimes housekeeping would move the floor mats when they were cleaning and usually puts them back down but stated she did not see the housekeeper in the room. The MDS Coordinator stated staff should know to put the floor mats on the floor when R#6 was in bed. The MDS Coordinator stated it was important to implement Resident #6 ' s care plan as it was person-centered and to prevent falls.
In an interview on [DATE] at 10:08 a.m., the DON stated R#6 should have floor mats as indicated on the care plan. The DON stated a floor mat should be utilized since it was part of the resident ' s intervention and was individualized to the person ' s plan of care.
In an interview on [DATE] at 11:13 a.m., RN A stated R#6 should have a floor mat while in bed. RN A stated when she went into R#6 ' s room earlier, there was a floor mat at the bedside. RN A stated she could not recall when the last in-service was on following care plans. RN A stated care plans should be followed since it was person-centered, and floor mats were used as an intervention for fall risk residents.
In an interview on [DATE] at 11:27 a.m., CNA B stated R#6 should have a floor mat while she was in bed. CNA B stated she was not sure if she saw the floor mat on the ground for R#6 earlier that day and if she did not, then she overlooked it and did not realize it was not there when it should have been. CNA B stated the floor mat was needed to prevent falls and care plans need to be followed. CNA B stated she does not remember when the last in-service was for following care plans.
2)Record review of R#2's face sheet revealed a [AGE] year-old female with an original admission date of [DATE] and a re-admission date of [DATE]. Diagnoses included dementia, stroke, abnormalities of gait and mobility, cognitive communication deficit, and major depression. R#2's quarterly MDS dated [DATE] revealed a BIMS of 5, indicating severe cognitive impairment. Her functional abilities required substantial assistance with oral and personal hygiene, toileting, bathing, dressing including footwear, and all mobility. She could not walk and required a motorized wheelchair which she could control. She was incontinent of bladder and bowel. Her active diagnoses included non-traumatic brain dysfunction, cancer, stroke, non-Alzheimer's dementia, malnutrition, and depression. She was on hospice and required scheduled pain medication.
Record review of R#2's quarterly care plan dated [DATE] revealed she had a focus for poor safety awareness and inability to care for self, initiated and revised on [DATE]. The focus for acute confusional episodes initiated on [DATE] and revised on [DATE] had interventions including monitor, record and report to physician new onset of delirium, changes in behavior, altered mental status, variation in cognitive function, communication decline, disorientation, lethargy, restlessness and agitation, altered sleep cycle, dehydration, infection, delusions, and hallucinations. Date initiated [DATE]and no revision date. Focus: R#2 needs out of room social, spiritual, and stimulus activities and mental stimulation, will participate in special events, karaoke, music, trivia, social gatherings, coffee chat. Dates initiated and revised: [DATE]. The goal included .have the choice of participating in the special offsite activities/program for senior adults virtual or activity group activities. Date initiated [DATE], revision date [DATE]. There were no other revisions.
In an interview with the ADM on [DATE] at 3:50 pm, she stated the facility did not have a policy for residents signing out when they left the facility and the sign out logs were the only means they had of keeping track of the whereabouts of residents when they left the facility for outside activities/program for senior adults, or when they left out on pass. She said falls were supposed to be updated in care plans when they happen, otherwise care plans should be updated quarterly.
In an interview with the MDS nurse on [DATE] at 2:51 pm, she stated almost every resident had a generic order for may go out on pass with meds, but those going to the special offsite activities/program for senior adults should have orders specific to that, because those orders would come from the psychiatrists. She said falls should be in the care plans.
Record review of R#2's physician active orders as of [DATE] revealed no specific order to attend special off-site activities/program for senior adults or go out on pass.
Record review of the facility's schedule for certain residents, including R#2, to attend special off-site activities/program for senior adults revealed R#2 was scheduled for [DATE], [DATE], [DATE], [DATE], [DATE], [DATE], [DATE], [DATE], [DATE] and [DATE]. [DATE] and [DATE] indicated R#2 had a virtual (tablet) visit. There were no other indicators in the special off-site activities/program for senior adult's schedule that R#2 had refused any offsite or other virtual visits, nor was she signed out at any time.
Record review of the facility's sign-out books revealed there were no names on the pages of the sign out books for any date prior to [DATE].
3)Record review of R#3's face sheet revealed a [AGE] year-old female with an admission date of [DATE]. Diagnoses included dementia, anxiety, impulse disorder, bipolar disorder, major depressive disorder, recurrent-severe, with psychotic symptoms, mood disorder, post-traumatic stress disorder (PTSD), insomnia, schizoaffective disorder, personality change due to known physiological condition, muscle wasting, seizures, and abnormalities of gait and mobility. R#3's quarterly MDS dated [DATE] revealed a BIMS of 4, indicating severe cognitive impairment. She required substantial assistance with dressing and footwear, set-up with oral and personal hygiene, and was independent with eating. She had a wheelchair and could self-propel. She was incontinent of bladder and bowel. Her active diagnoses were non-traumatic brain dysfunction, cancer, heart failure, non-Alzheimer's dementia, seizures, anxiety, depression, PTSD, and Bipolar.
Observation and interview with R#3 on [DATE] at 1:36 pm revealed she could speak but could not hold a conversation. Her hair was clean and combed, her clothes were clean and there were no foul odors. She was wearing a long-sleeved sweater. She was slowly self-propelling in her wheelchair about the facility. She had a visual impairment and was unable to see well, as whenever someone came up to her to speak with her, she would not look directly at them, but towards their voice. She wore eyeglasses. She could not say if she attended special off-site activities/program for senior adults.
In an interview with the ADM on [DATE] at 3:50 pm, she stated the facility did not have a policy for residents signing out when they left the facility and the sign out logs were the only means they had of keeping track of the whereabouts of residents when they left the facility for outside activities/program for senior adults, or when they left out on pass. She said falls were supposed to be updated in care plans when they happen, otherwise care plans should be updated quarterly.
In an interview with the MDS nurse on [DATE] at 2:51 pm, she stated almost every resident had a generic order for may go out on pass with meds, but those going to the special offsite activities/program for senior adults should have orders specific to that, because those orders would come from the psychiatrists. She said falls should be in the care plans.
Record review of R#3's quarterly care plan dated [DATE] revealed o Monitor for escalating anxiety, depression or suicidal thought and report immediately to the nurse Date Initiated: [DATE] o Perform the following de-escalation techniques as required: music, coloring, heritage program discussions, sitter Date Initiated: [DATE], Revision on: [DATE]. o Assist me to identify strengths, positive coping skills and reinforce these Date Initiated: [DATE]. o Continue with seeing Psych Services Date Initiated: [DATE]. o The resident uses anti-anxiety medications Date Initiated: [DATE]. Paradoxical side effects: Mania, Hostility and rage, Aggressive or impulsive behavior, Hallucinations. Date Initiated: [DATE]. R#3's care plan had no indication she attended special off-site activities/program for senior adults. The latest revision in R#3's care plan was [DATE], indicating R#3's care plans had not been updated or revised quarterly.
Record review of R#3's physician active orders as of [DATE] revealed no specific order to attend special off-site activities/program for senior adults. There was an order dated [DATE] that she may go out on pass with meds.
Record review of R#3's elopement risk assessments dated [DATE], [DATE], [DATE], and [DATE] documented R#3 was a high risk for elopement.
Record review of the facility's schedule for certain residents, including R#3, to attend special off-site activities/program for senior adults revealed R#3 was scheduled for [DATE], [DATE], [DATE], [DATE], [DATE], and [DATE]. There were no other indicators in the special off-site activities/program for senior adult's schedule that R#3 had refused any offsite or virtual visits, nor was she signed out at any time.
Record review of the facility's sign-out books revealed there were no names on the pages of the sign out books for any date prior to [DATE].
Interview with the ADM on [DATE] at 3:00 pm revealed actual falls with injury should be in the care plan. She said the DON and nurses should be entering information and updating care plans timely. She said the care plans were important because staff use the care plans to know what was going on with the resident, so the care plans needed to be updated as events or changes happen, not just quarterly.
In an interview with the ADM on [DATE] at 3:50 pm, she stated the facility did not have a policy for residents signing out when they left the facility and the sign out logs were the only means they had of keeping track of the whereabouts of residents when they left the facility for outside activities/program for senior adults, or when they left out on pass. She said falls were supposed to be updated in care plans when they happen, otherwise care plans should be updated quarterly.
In an interview with the MDS nurse on [DATE] at 2:51 pm, she stated almost every resident had a generic order for may go out on pass with meds, but those going to the special offsite activities/program for senior adults should have orders specific to that, because those orders would come from the psychiatrists. She said falls should be in the care plans.
4)Record review of R#5's face sheet revealed a [AGE] year-old male with an original admission date of [DATE] and a re-admission on [DATE]. He was his own representative. Diagnoses included diabetes with neuropathy, right leg cellulitis, unsteadiness and abnormalities of gait and mobility, muscle weakness, dementia, lack of coordination, obesity, major depression, anxiety, mood disorder, and age-related physical debility. R#5's quarterly MDS dated [DATE] revealed a BIMS of 12, indicating moderate cognitive impairment. He required substantial assistance with footwear, lower body dressing, and toileting, supervision with showering, set-up with upper body dressing, and was independent with oral and personal hygiene, eating, and transferring. He had a manual wheelchair and could self-propel. He was frequently incontinent of bladder and bowel. His active diagnoses were medically complex conditions.
Observation of R#5's room revealed he was not in the room on [DATE] at 10:11 am.
In an interview with RN E on [DATE] at 10:12 am, she said she was also looking for R#5 because she needed to give him his meds. She said she did not see him in the common areas, and he was probably in his room.
In an interview with RN E on [DATE] at 10:13 am, she said R#5 was not in his room and there was a sign-out binder at the nurse's station. Upon realizing there were no signatures in the sign out logs, she sought out the ADON.
Observation and interview with the ADON on [DATE] at 10:13 am, two sign-out binders were observed on the upper deck of the nurse's station. The ADON stated neither one had any resident's names signed in them. The ADON explained that one binder was for special off-site activities/program for senior adults and had a [DATE] appointment sheet, the other binder was for going out on pass and general. The ADON said she was unaware of R#5's whereabouts and called the appointment she thought he might be at. She verified his presence off site.
In an interview with the ADM on [DATE] at 10:29 am, she said residents in the special off-site activities/program for senior adults were picked up on Tuesdays and Thursdays. She said the ones who attend the special off-site activities/program for senior adults did not sign out and were kept track of separately. She said she would let us know how residents were kept up with, and where it was located, but right now she was not sure who kept up with residents leaving and going or how to prove it. She said the other sign out book was for other residents who were for going out on pass and general. When asked about R#5, and nurses stated they thought he was in his room, R#5 was not in his room and the staff did not know where the resident was. R#5 was out of the facility for an appointment and no sign out book was done.
In an interview with R#5 on [DATE] at 3:30 pm, he said he rarely, if ever signed out when he left the facility to go the special off-site activities/program for senior adults. He said the facility had a list of the residents that went there and that was how they knew if they (those residents) were gone.
In an interview with the ADM on [DATE] at 12:15 pm, she stated the facility had a sign out book but did not implement it until [DATE]. The ADM stated that the nurses were the ones who monitored the sign out book The ADM stated she was in charge of making sure the nurses were monitoring the sign out book but had not been ensuring it was being done. The ADM stated the facility did not have a policy for the sign out book. When asked about how the facility monitored the residents' whereabouts, the ADM stated the residents told the nurses so they should know but there was no way of knowing for sure since there was no monitoring in place. The ADM said the facility did not have a policy regarding the residents signing out.
Record Review of R#5's quarterly care plan dated [DATE] revealed R#5 required hypnotic medications Date Initiated: [DATE] Revision on: [DATE]. The resident uses anti-anxiety medications Date initiated [DATE] Revision on [DATE]. The resident requires antidepressant medication Date initiated [DATE] Revision on [DATE]. R#5 is dependent on staff for activities, cognitive stimulation, and social interaction. Dates initiated and revised on [DATE]. Interventions included assist by: with arranging community activities. Arrange transportation. Date Initiated: [DATE]. There was no revision date. R#5 has little or no activity involvement r/t depression, disinterest, R#5 wishes not to participate. Dates initiated and revised [DATE]. Interventions included R#5's preferred activities are the special offsite activities/program for senior adults online. Dates initiated and revised [DATE].
There were no updates regarding Resident #5 leaving the community to attend an outside activity.
Record review of R#5's elopement risk assessments dated [DATE] through [DATE] triggered for elopement risk.
Record review of R#5's physician active orders as of [DATE] revealed no specific order to attend special off-site activities/program for senior adults. There was an order dated [DATE] that he may go out on pass with meds.
Record review of the facility's schedule for certain residents, including R#5, to attend special off-site activities/program for senior adults revealed R#5 was scheduled for [DATE], [DATE] (tablet), [DATE] (tablet), [DATE] (in person), [DATE], [DATE], [DATE], [DATE], [DATE] (in person), and [DATE]. There were no other indicators in the special off-site activities/program for senior adult's schedule that R#5 had refused any offsite or virtual visits, nor was he signed out at any time.
Record review of the facility's sign-out books revealed there were no names on the pages of the sign out books for any date prior to [DATE].
In an interview with the MDS nurse on [DATE] at 10:20 am revealed she did the comprehensive care plans and the nurse's input anything outside of the quarterly, such as diet changes, falls, etc. She said she audited care plans quarterly but could not say when she last audited a care plan.
5)Record review of admission record revealed R#18 was an [AGE] year-old female with diagnoses of Dementia, Muscle Wasting, Abnormalities of Gait and Mobility, Muscle Weakness, Disorientation, Anxiety, and Depression.
Record review of medical diagnoses for R#18 revealed she did not reveal a diagnosis of gout.
Record review of R#18's care plan conference dated [DATE] revealed R#18's right index finger pain and was treated with ibuprofen.
Record review of all of R#18's care plans did not note the fact that resident may get finger or hand caught in wheels on wheelchair during transfers or mobility, nor does it indicate that resident sometimes hit her hand on her nightstand or bedside table.
Record review of nurses' note, dated [DATE], revealed injury to R#18's right index finger with fracture and increased pain. This note also revealed that resident had stated that she jammed her finger during morning care.
Record review of injury nurses' note, dated [DATE], revealed that R#18 had a fracture of right index finger.
Record review of progress notes, dated [DATE], revealed R#18 presented with bruising, pain and swelling to right index finger and x-ray was ordered. Progress note dated [DATE] revealed Ibuprofen was ordered as needed for pain. Progress note dated [DATE] revealed continued monitoring R#18 for pain, bruising and swelling, and that resident was able to open and close hand with minimal pain. Progress note dated [DATE] and [DATE] revealed follow-up x-ray showed no evidence of fracture to right index finger as previously thought.
Record review of x-ray report from radiology, for R#18, dated [DATE], revealed multiple views of the right index finger demonstrated no evidence of fracture.
Record review of provider investigation report for R#18, interview with the Administrator, dated [DATE], revealed that resident told administrator on [DATE] that she jammed finger while getting ready, but on [DATE] told staff that she got her hand caught in her wheelchair.
Record review revealed that staff were in-serviced [DATE] over abuse and neglect.
Observation of R#18, [DATE], revealed that the resident had minor swelling and bruising to right thumb.
Interview on [DATE] at 10:45 AM with R#18, she stated she did not remember injuring her finger previously, and that it was her thumb that was injured. She stated she had the bruising and swelling to her right thumb because she banged it on a loose screw when she wheeled herself. She stated she had lived in this facility most of her life. She also stated that someone came and stole her teeth out of her mouth, and that she could not find her toothbrush. R#18 also stated that she never got her hand caught in her wheelchair.
Interview on [DATE] at 10:51 AM with RN H, she stated she remembered the swelling and bruising to R#18's finger and thought she may have hit it on something because she had had previous bruising from bumping things. Stated she claimed that someone stole her tooth while she was sleeping at night. Thinks she may be on a blood thinner but can't recall for sure. Resident#18 has never claimed or reported any abuse to her.
Interview on [DATE] at 12:42 PM with ADON, she stated the first x-ray showed a fracture, but the second x-ray showed no fracture. She stated that R#18 told her it happened during transfer. ADON also stated that R#18's right thumb was currently swollen with mild bruising, and resident told her that she thought something may have bit her or that she may have hit it on her bedside table. Resident had never claimed or reported any abuse or neglect to her.
Interview [DATE] at 1:35 PM with PTA, he stated he previously had R#18 on services, most recently was for cellulitis of foot, but did not remember R#18 having any falls around the time of the swelling and bruising to her finger or recently. He stated she had some difficulty with transfers but denied remember her having any bruising or swelling anywhere. He stated that if he was aware of a resident fall, he called the DON to come check on resident to assess them. Stated he had been in-serviced on falls and abuse, neglect and exploitation (ANE), and that the administrator wass the ANE coordinator. If resident claimed or reported abuse to him, he would assess the resident then tell the charge nurse and administrator.
Interview [DATE] at 2:35 pm with the Administrator, she stated R#18 denied knowing what happened, but stated she had pain. Also, stated the resident had gout, and it happened with gout flare ups at times. First x-ray showed fracture, but the next two x-rays did not show fracture, but, per the Administrator, the facility concluded that she caught her finger or hand in her wheelchair. Administrator also stated that thumb was currently bruised and swollen, and nursing staff reported to her in the past that it had happened previously.
Interview [DATE] at 9:48 AM with CNA E, she stated she was in-serviced and trained on ANE all the time with falls and incidents, and that the last training was recent, sometime this month. CNA E denied ever seeing abuse in the facility or R#18 ever reporting abuse to her, or anyone getting rough with her. She stated she would report any abuse to the administrator or the person in charge if the administrator was gone. She stated she was unsure of how R#18 got the injury, but thought it may have come from her wheelchair, but she had not known her to have had injuries such as this in the past.
Interview on [DATE] at 10:30 AM with CNA F, she stated she remembered R#18's finger being swollen and bruised but did not remember what happened to it. She denied receiving any complaints of abuse or mistreatment from any residents, and she stated that R#18 bumped into things frequently. CNA F denied ever hearing anyone say anything about R#18's fingers ever getting caught in her wheelchair.
Interview on [DATE] at 1:16 PM with the Administrator, she stated she searched for care plans for R#18 for both a finger injury and/or a wheelchair injury (wheelchair was the outcome of their previous investigation). She stated the care plans were completed by multiple people to include herself, the DON and the ADON, and that she would own up to it and admit that this incident was never care planned. She also stated she knew they had a problem with their care plans, but she was hoping since hiring a new DON it would get worked out.
6)Record review of admission record for R#19 revealed that she was an [AGE] year-old-female with diagnoses of Dementia, Major Depressive Disorder, Dependence on wheelchair, Protein - Calorie malnutrition, anxiety, restlessness and agitation, pain, and altered mental status. (R#19 was deceased as of [DATE])
Record review of all of R#19's care plans revealed that pulling out midlines and other peripheral IV sites were not care planned. R#19's MDS revealed she had a BIMS of 4, indicating severe cognitive impairment.
Record review of progress note dated [DATE] revealed R#19 pulled out peripheral IV site.
Record review of progress note dated [DATE] revealed R#19 pulled out midline.
Record review of progress note dated [DATE] revealed R#19 pulled out midline and had a moderate amount of bleeding, and a pressure dressing was applied.
Record review of nurses' note dated [DATE] revealed 5cm x 7cm blue and purple bruise to R#19's upper right arm. Resident denied knowing how bruise got there.
Record review of progress note dated [DATE] revealed R#19 had a bruise of unknown origin that appeared on the clinical alerts on the clinical dashboard on [DATE], and administrator notified. Assessment of bruise on [DATE] revealed bruise was parallel to previous midline area that R#19 had pulled out on [DATE].
Record review of progress note dated [DATE] revealed bruise to R#19's right upper arm remained dark purple in center and faded to a lighter maroon, and green/yellow. Area was tender to touch and measured 9cm x 9cm. Resident #19 unable to state how bruise occurred.
Interview [DATE] at 12:50 PM with ADON, she stated she remembered the bruise to R#19's right arm, and that she had a PICC line or midline around that time but did not remember if it was on her right arm. She stated R#19 had pulled out midlines and IVs in the past. She did not remember her falling or having any altercations with other residents. The ADON stated she remembered R#19 bruised easily but did not remember if she was on a blood thinner or not.
Interview [DATE] at 1:40 PM with the PTA, he stated he remembered the bruise on R#19's arm, but was not sure how it happened, but it possibly happened during a transfer because she was difficult to transfer. He stated he remembered R#19 hollered constantly and was hard to transfer. He said he did not remember her having a PICC or midline.
Interview [DATE] at 2:39 PM with Administrator, she stated R#19 had pulled out PICC or midline the day before the bruise showed up in the same area on her arm. There had been a pressure dressing in that area. She stated resident had history of pulling out PICC lines and midlines. She is unsure if R#19 bruises easily, and not sure if she was on a blood thinner. Administrator stated she searched the care plan for PICC or Midline being pulled out by R#19 but stated that she could not find this one either, and that she knew they had a problem with their care plans, but she was hoping since hiring a new DON it would get worked out.
Interview [DATE] at 10:40 AM with CNA F, she stated she remembered the bruise to R#19's arm, and that R#19 had a wrap or dressing to her arm. She stated R#19 had pulled out PICC lines in the past. CNA F stated R#19 had never complained about abuse or neglect to her, and she never noticed staff or other residents get rough with her.
Interview [DATE] at 9:48 AM with CNA E, she stated she had been in-serviced and trained on abuse, neglect and exploitation many times with falls and incidents. Last training was recently, sometime this month. CNA E denied ever seeing or suspecting abuse in the facility, and she stated she would report it to the administrator or person in charge if the administrator was gone. CNA E remembered R#19's bruise had purple and green and was approximately the size of her hand. She said she was unsure of how R#19 got that bruise, but she thinks she pulled out her PICC line. CNA E said she was unsure if resident had done that in the past and denied any staff getting rough with her. CNA E stated R#19 had never complained about abuse to her.
Record review of the facility's undated Comprehensive Care Planning policy documented .Resident's preferences and goals may change throughout their stay, so facilities should have ongoing discussions with the resident and resident representative, if applicable, so that changes can be reflected in the comprehensive care plan. The resident's care plan will be reviewed after each admission, quarterly, annual and/or significant change MDS assessment, and revised based on changing goals, preferences and needs of the resident and in response to current interventions.
Record review of Comprehensive Care Planning policy not dated stated:
Each resident will have a person-centered comprehensive care plan developed and implemented to meet his other preferences and goals, and address the resident ' s medical, physical, mental, and psychosocial needs.
The comprehensive care plan will reflect interventions to enable each resident to meet his/her objectives.
Interventions are the specific care and services that will be implemented.