THE REHAB CENTER AT BRISTOL




Over 2 years since last inspection. Current conditions may differ from available data.
The Rehab Center at Bristol has a Trust Grade of C, meaning it is average and ranks in the middle of nursing homes in the area. It is positioned at #163 out of 285 facilities in Virginia, placing it in the bottom half of the state's rankings, and it is the second-best option in Bristol City County. Unfortunately, the facility is worsening, as it has increased its issues from 2 in 2024 to 3 in 2025. Staffing is decent with a 3/5 rating and a turnover of 52%, which is similar to the state average of 48%. On a positive note, the facility has not incurred any fines, indicating compliance with regulations, and it boasts more RN coverage than 85% of Virginia facilities, which helps catch potential problems. However, there are notable weaknesses. A serious incident occurred where a resident fell and sustained a head injury due to inadequate supervision during bathing. Additionally, there were concerns about the facility's failure to thoroughly investigate allegations of abuse for multiple residents, which raises significant safety questions. Lastly, cleanliness issues were reported, including a pervasive odor of urine and debris in the hallways, indicating that the environment may not always be as comfortable as families would hope. Overall, while there are strengths in staffing and RN coverage, the facility has critical areas that need improvement to ensure resident safety and comfort.
- Trust Score
- C
- In Virginia
- #163/285
- Safety Record
- Moderate
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 52% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Virginia facilities.
- Skilled Nurses ✓ Good
- Each resident gets 47 minutes of Registered Nurse (RN) attention daily — more than average for Virginia. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 24 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Near Virginia average (3.0)
Meets federal standards, typical of most facilities
Near Virginia avg (46%)
Higher turnover may affect care consistency
The Ugly 24 deficiencies on record
Oct 2025
3 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on observation, record review, interview, and facility document and policy review, the facility failed to provide adequate supervision to prevent accidents for 1 (Resident #101) of 4 residents r...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, record review, facility document review, and interview, the facility failed to ensure an allega...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility policy review, record review, facility document review, and interview, the facility failed to have evidence th...
Read full inspector narrative →
Mar 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on staff interview, clinical record review and facility document review, the facility staff failed to provide activities of daily living (ADL) care to one of six residents in the survey sample, ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, resident interview, staff interview and clinical record review, the facility staff failed to provide respiratory care consistent with the comprehensive person-centered care plan ...
Read full inspector narrative →
Oct 2022
11 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on staff interview and facility document review, the facility staff failed to provide copies of notice of resident transfers and discharges to a representative of the Office of the State Long-Te...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
2. For Resident #36 the facility staff failed to provide activities of daily living (ADL) care in regards to facial hair.
Resident #36's face sheet listed diagnoses which included, but not limited to...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
3. For resident #44, facility staff failed to ensure a medication regimen review (MRR) was performed for the month of February 2022.
Resident #44 diagnosis list includes, but is not limited to the fol...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on resident interview, staff interview, clinical record review, facility document review, and during a medication pass and pour observation the facility staff failed to ensure a medication error...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview, and facility document review, the facility staff failed to dispose of expired specimen tu...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Laboratory Services
(Tag F0770)
Could have caused harm · This affected 1 resident
Based on staff interview and clinical record the facility staff failed to obtain a physician ordered laboratory test for 1 of 19, Resident #36.
The findings included:
For Resident #36 the facility sta...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observations, staff interviews, and facility document review, the facility staff failed to ensure food was stored under safe and sanitary conditions in 2 of 2 unit nourishment rooms.
The fin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
2. During a medication pass and pour observation the facility staff were observed to touch Resident #55's medications with their bare hands.
10/25/22 beginning at approximately 7:38 a.m., the surveyo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on staff interview, clinical record review, and facility document review, the facility staff failed to offer and provide the resident and/or resident representative education regarding the benef...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on staff interview, family interview, and facility document review the facility staff to ensure a clean, comfortable, homelike environment for 1 of 2 floors, and one of 19 residents, Resident #3...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected multiple residents
Based on staff interview and facility document review, the facility staff failed to maintain an infection prevention and control program to include an antibiotic stewardship program.
The findings incl...
Read full inspector narrative →
May 2019
8 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on staff interview, facility document review and new employee file review, the facility staff failed to obtain a criminal background check on 1 of 25 newly hired employees of the facility (Emplo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview and clinical record review, the facility staff failed to follow physician's orders for administration o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation and staff interview, the facility staff failed to have narcotic box in the medication refrigerator permanently affixed for 1 of 2 units in the nursing facility (Unit 2 on second f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation, staff interview and facility document review, the facility staff failed to date spices after they have been opened in the facility kitchen.
The findings included:
The surveyor we...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview and clinical record review, the facility staff failed to ensure a complete and accurate clinical record...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview and clinical record review, the facility staff failed to ensure medications were available to be admini...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observation and clinical record review, the facility staff failed to ensure the medication error rate was less than 5% on 1 of 2 units in the nursing facility. (Unit 2, second floor) The medi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview and clinical record review, the facility staff failed to follow infection control guidelin...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most Virginia facilities.
- • 24 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • Grade C (55/100). Below average facility with significant concerns.
About This Facility
What is The Rehab Center At Bristol's CMS Rating?
CMS assigns THE REHAB CENTER AT BRISTOL an overall rating of 3 out of 5 stars, which is considered average nationally. Within Virginia, this rating places the facility higher than 0% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is The Rehab Center At Bristol Staffed?
CMS rates THE REHAB CENTER AT BRISTOL's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 52%, compared to the Virginia average of 46%.
What Have Inspectors Found at The Rehab Center At Bristol?
State health inspectors documented 24 deficiencies at THE REHAB CENTER AT BRISTOL during 2019 to 2025. These included: 1 that caused actual resident harm and 23 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates The Rehab Center At Bristol?
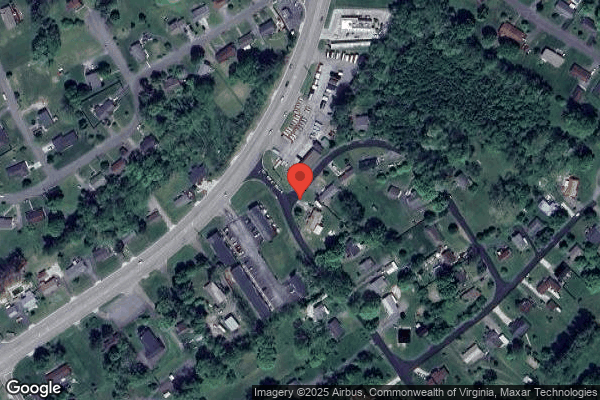
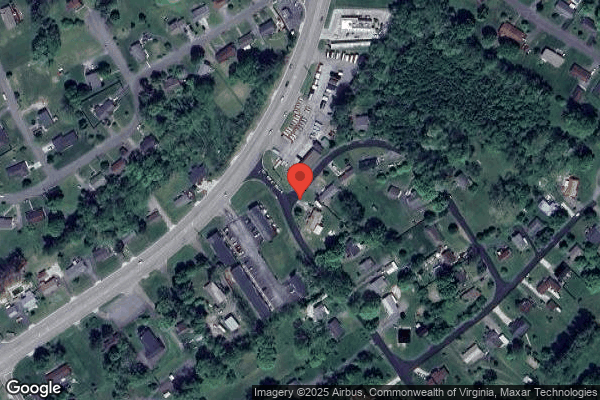
THE REHAB CENTER AT BRISTOL is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 90 certified beds and approximately 83 residents (about 92% occupancy), it is a smaller facility located in BRISTOL, Virginia.
How Does The Rehab Center At Bristol Compare to Other Virginia Nursing Homes?
Compared to the 100 nursing homes in Virginia, THE REHAB CENTER AT BRISTOL's overall rating (3 stars) is below the state average of 3.0, staff turnover (52%) is near the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting The Rehab Center At Bristol?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is The Rehab Center At Bristol Safe?
Based on CMS inspection data, THE REHAB CENTER AT BRISTOL has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #100 of 100 nursing homes in Virginia. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at The Rehab Center At Bristol Stick Around?
THE REHAB CENTER AT BRISTOL has a staff turnover rate of 52%, which is 6 percentage points above the Virginia average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was The Rehab Center At Bristol Ever Fined?
THE REHAB CENTER AT BRISTOL has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is The Rehab Center At Bristol on Any Federal Watch List?
THE REHAB CENTER AT BRISTOL is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.