CRITICAL
(J)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. For Resident #97 (R97), the facility staff failed to provide supervision for safe LOA (leave of absence).
On 7/9/24 at 10:08 ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. For Resident #97 (R97), the facility staff failed to provide supervision for safe LOA (leave of absence).
On 7/9/24 at 10:08 a.m., R97 was interviewed. He stated that he leaves the premises and walks across the street to the store about once a week by himself. He also stated that he lets the front desk, and the nurses know before leaving, but staff do not supervise his trips. He stated that he should be using his cane to walk, but he does not.
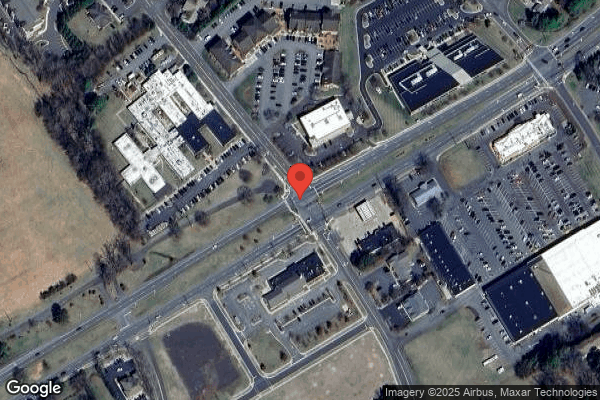
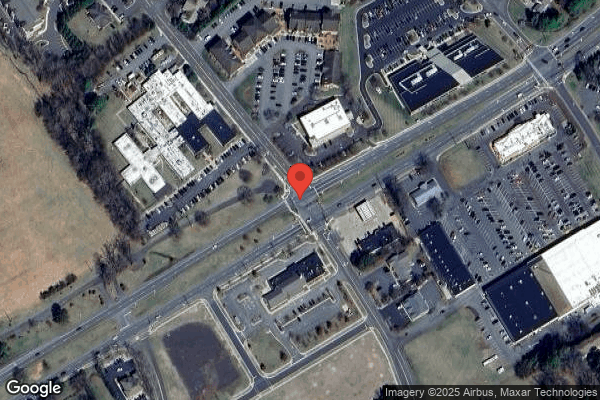
On 7/9/24 at 5:50 PM, R97 was observed walking over to Walgreens without a cane. He looked both ways on his way to Walgreens while crossing Sunset Lane. He was observed crossing 4 lanes of traffic across the street with no staff supervision. He walked with a shuffling gait. Upon his return to the facility, he was observed crossing the same 4 lanes of traffic with no staff supervision and did not look for oncoming traffic.
On the most recent MDS (minimum data set), an admission assessment with an ARD (assessment reference date) of 4/17/24, R97 was admitted to the facility 4/11/24. R97 was coded as being moderately impaired for making daily decisions, having scored 12 out of 15 on the BIMS (brief interview for mental status). The resident was coded as having a walker and wheelchair and not attempting to walk 150 feet due to medical condition or safety concern.
A review of R97's clinical record revealed the resident signed out once to leave the facility on 3/10/24.
A review of physical therapy recommendations for 5/29/24- 6/25/24 revealed, in part: Pt (Patient) was re-educated as to the potential benefits of using an amb. (ambulation) device (vs. no device) - as well as to wear shoes with all standing/amb. Activity to minimize fall risk (in light of recent fall).
A review of R97's physical therapy discharge summary for 5/29/24- 6/25/ revealed, in part: Ambulation .Walking 10 feet on uneven surfaces= supervision or touching assistance. 1 step (curb) = Supervision or touching assistance.
A review of R67's care plan revealed, wheeled walker for ambulation and transfers.
On 7/9/24 at 3:42 p.m., LPN (licensed practical nurse) #3 was interviewed. She stated that, to know if a resident is safe to leave, they look at their BIMS score, and it has to be above a 10. She also stated, with the BIMS score anything below 8 staff the resident is cognitively impaired. She stated that MDS does the BIMS coding on the residents, so if nursing staff disagree with a BIMS of someone trying to leave, nursing staff will look at safety. LPN #3 stated that in the past, staff had to assess people who wanted to leave and that somebody would go with them and see if they knew how to cross the street. She stated that as a floor nurse if someone wants to leave, she has to check if the resident is their own responsible party and if they are not, have them sign out in the sign out book. LPN#3 stated if the resident cannot sign out, a X is documented in the sign out book and a staff sign beside the X. She stated that nurses try to write a note for documentation. She also stated that sign out sheets tell staff where the person is, but they will call the resident if they want to check up.
On 07/09/24 at 4:03 p.m., OSM (other staff member) #20, the Rehab Manager, was interviewed. She stated that if residents wish to independently leave the facility, therapy assesses them on community outings if that was something desired at admission. She also stated that it is something that is documented in therapy's evaluations and discharge summary. OSM #20 stated that therapy makes the determination that it is safe for residents to leave after they ambulate with residents or simulate those type of environments. She stated that therapy assess for safety so things like assistance device management and awareness of surroundings would be included in that. She also stated that R97's need for a cane or walker can increase the chances of injury if not used properly. OSM #20 further stated that the therapy staff did not specifically evaluate R97 for community outings, but the resident was assessed as requiring supervision or touching assistance when walking 10 feet on uneven surfaces. OSM #20 stated supervision meant someone should have eyes on the resident. OSM #20 stated that if R97 independently ambulated in the community without a complete assessment, and without supervision, he could have a fall with an injury.
The facility policy, Leave of Absence (LOA), revealed, in part: When patients leave the center for reasons other than a medical transfer initiated by the center, the patient and/or responsible party will provide signature, accepting complete responsibility of the patient and absolving the management, personnel, and the attending physician of responsibility for any deterioration in condition or accident that may happen while the patient is away.
On 7/9/24 at 5:42 p.m., ASM (administrative staff member) #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services, and ASM #4, the regional vice president of clinical services, were notified of Immediate Jeopardy (IJ). The Administrator made the Medical Director aware of the Immediate Jeopardy via telephone on 7/9/24 at 7:32pm.
No further information was provided prior to exit.
5. The facility failed to provide a safe environment for Resident #136 while on LOA (leave of absence)
On 7/9/24 at 7:53 AM, Resident #136 was observed ambulating independently with a rollator walker off facility property. Resident #136 was observed crossing the street at two points of a major intersection using the pedestrian walkways. Resident #136's gait was shuffling and show. He turned into the facility driveway and walked down the center of the driveway where cars were entering and exiting, rather than using the facility sidewalk. He was wearing a red and yellow safety vest. Resident #136 stated he goes to the local gas station each morning, then returns to the facility to eat breakfast. He stated after breakfast each day, he leaves the facility to go off the property to a local wellness center.
Resident #136 was admitted to the facility on [DATE] with diagnosis that included but were not limited to: ASCVD (atherosclerotic cardiovascular disease), atrial fibrillation and Poly osteoarthritis.
The most recent MDS (minimum data set) assessment, a quarterly assessment, with an ARD (assessment reference date) of 6/21/24, coded the resident as scoring a 15 out of 15 on the BIMS (brief interview for mental status) score, indicating the resident was not cognitively impaired. A review of the MDS Section GG-functional abilities and goals coded the resident as being independent for bed mobility, transfer, dressing and eating; supervision for hygiene and bathing.
A review of the comprehensive care plan dated 9/13/23 revealed, FOCUS: The resident requires assistance with ADLS (activities of daily living). INTERVENTIONS: Resident frequently signs self out LOA, have provided safety vest to wear as tolerated. Remind resident to use walker for ambulation and transfers.
A review of Resident #136's Elopement Risk Assessment dated 6/19/24, scored the resident as a '3'= low risk. There was no evidence of an assessment to determine the resident's safety to leave the facility independently on leave of absence.
A review of Resident #136's sign-out sheet, revealed the last time he signed out was 12/23.
On 7/9/24, the facility receptionist was interviewed. She stated the resident leaves the facility each morning, and that he is supposed to sign out on his unit.
An interview was conducted on 7/9/24 at 3:45 PM with LPN (licensed practical nurse) #3. When asked what is your role when a resident wants to leave the facility, LPN #3 stated, we check if they are their own RP (responsible party), their BIMS, sign them out in the sign out book and write a note in the sheet, what time they went out. If they are gone a long time, we call the resident's cell phone, 'just checking on you, when are you coming back'. If they are their own RP they must sign out, if they are not their own RP, we call the RP and get permission and then 2 nurses' sign. If the resident cannot sign their name, we have them do an X and then 2 nurses' witness. I am assuming Resident #136 has been assessed because he has a safety vest as on my days off, I have seen him at the pharmacy and the grocery store.
On 7/11/24 at 9:10 AM, ASM (administrative staff member) #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services and ASM #4, the vice president of operations was made aware of the finding.
The facility's LOA (Leave of Absence) policy revealed the following, When patients leave the center for reasons other than a medical transfer, the patient will provide signature accepting complete responsibility of the patient for any deterioration in condition or accident that may happen while the patient is away. Upon return to the facility, the patient will sign back in with date and time.
No further information was provided prior to exit.
Immediate Jeopardy:
A. On 7/8/24 at 4:17 PM, the findings of Immediate Jeopardy and substandard quality of care were confirmed during a phone call with the State Agency, related to concerns identified for resident smoking. On 7/8/24 at 5:38 PM, ASM #1 (Administrative Staff Member) the administrator, ASM #2, the Director of Nursing, ASM #3 the Regional Director of Clinical Services, and ASM #4 the Regional [NAME] President of Operations, were informed of the Immediate Jeopardy and subsequent SQC (substandard of care) finding and the need to complete a plan of removal. The Administrator made the Medical Director aware of the Immediate Jeopardy via telephone on 7/8/24 at 6:18 PM. On 7/8/24 at 9:48 PM, ASM #4 presented an acceptable plan of correction which was accepted on 7/8/24 at 9:49 PM.
B. On 7/9/24 at 5:30 PM the findings of Immediate Jeopardy and substandard quality of care were confirmed during a phone call with the State Agency, related to concerns identified for LOA ( resident leave of absence.) On 7/9/24 at 5:42 PM, ASM #1, #2, #3 and #4, were informed of the Immediate Jeopardy and subsequent SQC finding and the need to complete a plan of removal. The Administrator made the Medical Director aware of the Immediate Jeopardy via telephone on 7/9/24 at 7:32 PM. On 7/10/24 at 11:05 AM, ASM #4 presented an acceptable plan of correction which was accepted on 7/10/24 at 12:07 PM. The facility alleges abatement of the Immediate Jeopardy on 7/10/24 at 6:00 P.M
F689 Accidents and Hazards Abatement:
1. Plan of Corrective Action for those residents found to be affected by the deficient practice:
A. Resident #148 had a skin assessment performed on 7/8/24 and no burns were noted. Resident's smoking items were obtained by staff and put into a safe storage area. Resident re-educated on smoking policy and procedure, to include smoking location, smoking times, cigarette disposal, and smoking item storage. Resident had a smoking assessment completed on 7/8/24 that deemed him as safe supervised smoker without any adaptive equipment needed.
A. Resident #90 had a skin assessment performed on 7/8/24 and no burns were noted. Resident's smoking items were obtained by staff and put into a safe storage area. Resident re-educated on smoking policy and procedure, to include smoking location, cigarette disposal. Resident had a smoking assessment completed on 7/8/24 that deemed him as safe independent smoker without any adaptive equipment needed.
B. Resident #97 was placed on 1:1 supervision to ensure his safety and to not leave the building unattended. A therapy evaluation request was placed on 7/9/24 to conduct an assessment for the ability to leave the building independently. Resident was educated that if he were to leave the building, he needed to sign out on the sign out sheet and let the nurse know he was leaving the building. A new elopement assessment was completed on 7/9/24 and he was deemed a low elopement risk.
2. Corrective Actions taken for residents with potential to be affected by deficient practice:
A. All residents who smoke have the potential to be affected by this deficient practice. The facility Interdisciplinary Team will conduct resident smoking safety assessments on 7/8/24 assessing residents for safe smoking criteria. All residents assessed to be a smoker will have all smoking materials stored by the facility to be distributed if they are deemed requiring supervision, during approved smoking times by 7/9/24. The Facility Administrator will conduct a town hall meeting on 7/9/24 at 8:30 A.M. with the residents that smoke and review facility smoking policy and consequences for non-compliance.
B. All residents who leave the building have the potential to be affected by this deficient practice. The facility licensed nursing staff will conduct new elopement assessments on all residents to determine elopement risk. Identified residents that leave the building unattended will have an evaluation by therapy to determine their ability to safely leave the building unattended on a leave of absence or an approved medical leave. The Interdisciplinary Team will discuss the outcome of evaluations with a medical provider to obtain leave of absence order as indicated.
3. Systemic Changes put into place to ensure the deficient practice does not recur:
A. The Interdisciplinary Team (Administrator, Director of Nursing, Assistant Director of Nursing, Director of Social Work, Activities Director, Dietary Manager, Business Office Manager, Director of Maintenance, Director of Housekeeping and Laundry, Human Resources, and Unit Managers) will be educated by the Regional Director of Clinical Services on facility smoking policy to include resident safe smoking practices, supervision with smoking, and resident non-compliance with smoking policy. Starting 7/8/24 all staff will be educated, and no staff member will be permitted to return to work until they have completed the mandatory education on facility smoking policy, safe smoking and supervision, and non-compliance with smoking policy. Smokers that require supervision will be monitored by Activities staff or Nursing staff or by another appropriate person. A list of smokers will be provided to the monitor to include those who require supervision and adaptive equipment needed. The monitor will distribute smoking materials to those who require supervision and ensure materials are collected once smoking is completed. This education will be provided to all new employees as part of new hire orientation to include agency staff.
B. The Interdisciplinary Team (Administrator, Director of Nursing, Assistant Director of Nursing, Director of Social Work, Activities Director, Dietary Manager, Business Office Manager, Director of Maintenance, Director of Housekeeping and Laundry, Human Resources, and Unit Managers) will be educated by the Regional Director of Clinical Services on the Leave of Absence Policy to include ensuring residents sign out when leaving and returning to the building, any resident that desires to be independent in the community will require a interdisciplinary evaluation from Therapy/Nursing and the physician prior to being deemed safe to leave independently, what to do if a resident refuses to sign out, the nursing staff must write a note that the resident refused and verbalized they were leaving the building; and that all residents must exit via the front door only. The medical providers will be educated by the Director of Nursing on the process of evaluation for residents who desire to leave the building independently. Starting 7/10/24 all staff will be educated by the Director of Nursing/designee, and no staff member will be permitted to return to work until they have completed the mandatory education on facility Leave of Absence Policy and above. A list of those residents that leave the facility and have been deemed safe to be in the community unattended will be posted at the nurse's station and front desk. The list will be maintained and updated by the nursing department as changes occur. Any new or existing residents that have not been deemed safe to be independent will not be allowed to leave the building without being accompanied by a family member or staff member. New or re-admitted residents that are admitted to the facility and have a desire to leave the facility independently will have an evaluation performed by the therapy department for safety and independence in consultation with the medical provider to approve the leave of absence. The Interdisciplinary Team will review the approved list weekly during the risk meeting for any changes needed. Resident sign out books will be located at each nursing unit, this will be maintained by the medical records department when a resident admits, discharges or room changes occurs. The nursing staff, receptionist or an employee that assists with any exits or after-hours exits out of the building will ensure residents are signed out prior to leaving. Residents are only permitted to leave through the front door. Residents will be tracked for Leave of Absence's through the sign-out books at each nursing station. This education will be provided to all new employees as part of the new hire orientation to include agency staff. On 7/10/24 Residents will be educated during Resident Council on the new process for Leave of Absence policy for those that wish to leave the facility independently. Resident Family Members will be educated by Social Services or designee on the new process of evaluation for independently leaving the building, signing in and out of the building for a leave of absence.
A. The Administrator to conduct an ADHOC Quality Assurance Performance Improvement Meeting on 7/9/24 including the Administrator, Director of Nursing, Assistant Director of Nursing, MDS Coordinator, Director of Social Work, Activities Director, Dietary Manager, Business Office Manager, Director of Maintenance, Director of Housekeeping and Laundry, Human Resources, Medical Director and Unit Managers.
B. The Administrator to conduct an ADHOC Quality Assurance Performance Improvement Meeting on 7/10/24 including the Administrator, Director of Nursing, Assistant Director of Nursing, MDS Coordinator, Director of Social Work, Activities Director, Dietary Manager, Business Office Manager, Director of Maintenance, Director of Housekeeping and Laundry, Human Resources, Medical Director and Unit Managers.
4. A. Facility will monitor residents for change in condition to determine if a new smoking assessment is needed or will be done quarterly per policy. If a resident is observed by a smoking monitor with unsafe smoking practices, the resident will be stopped from smoking and have a new assessment completed to determine any changes to ensure safe smoking ability. The Administrator or designee will do random audits three times weekly x 4 weeks, then weekly x 4 weeks then monthly x 2 months to ensure residents that require supervision during smoking are supervised during the approved smoke time, staff are maintaining smoking materials for those residents during nonsmoking times and that all residents are smoking in the designated area.
B. Facility will monitor residents for changes in condition to see if a new therapy evaluation will be needed to reassess safety. The Administrator or designee will audit the sign out sheets three times weekly x 4 weeks, then weekly x 4 weeks then monthly x 2 months to ensure that residents are signing out and if a resident refuses to sign out, there is a nurses note present in the medical record.
5. The facility alleges abatement of the Immediate Jeopardy on 7/10/24 at 6:00 PM.
Monitoring of corrective action to ensure the deficient practice does not recurA. On 7/9/24, the plan of removal for smoking concerns was verified by the surveyors onsite. The education completed by the administration regarding the facility's smoking policy and procedures was verified. Interviews were conducted with the staff of each department. All staff interviewed properly stated the smoking policy and procedures. A list of residents who smoke and their status as being independent or requiring supervision was posted at each nurse's station and the front desk. Observation was made of the designated smoking area on 7/9/24 at 11:20 AM. Residents identified as smokers were observed with staff supervision of all residents during smoking and all safety measures were in place, including a new fire extinguisher cabinet on the wall outside the door in the courtyard, with a new fire extinguisher in it. In addition, a smoking blanket was observed on the wall next to the fire extinguisher. This was in addition to the one just inside the door to the courtyard. The Immediate Jeopardy was abated on 7/9/24 at 1:46 PM, the IJ for part A (smoking) was removed
B. On 7/11/24, the plan of removal for leave of absence was verified by the surveyors onsite. The education completed by the administration regarding the facility's leave of absence policy and procedures was verified. Resident assessments were being completed to determine which residents were safe for independent leave of absence and which residents required supervision. Interviews were conducted with staff from each department. All staff interviewed properly stated the leave of absence policy and procedures. A review of the sign out book revealed the book was updated, and one was available at each nurse's station. A list of residents allowed to leave the facility independently was posted at the front desk and nurse's stations. On 7/11/24 at 10:32 AM, the IJ for the LOA (leave of absence) was removed.
4. For Resident #120, the facility staff failed to implement a LOA (leave of absence) process for resident safety to ensure the facility had knowledge of Resident #120's whereabouts at all times.
On the most recent MDS (Minimum Data Set), a quarterly assessment dated [DATE], Resident #120 was coded as moderately impaired in ability to make daily life decisions, scoring a 12 out of a possible 15 on the BIMS (Brief Interview for Mental Status exam).
A review of the physical therapy notes revealed the following:
On 3/21/23 was documented, Gait training over indoor/outdoor surfaces for distance of 1033 (feet) without AD (assistive device) over concrete/carpet/grass/tile .focusing on directional changes and obstacle negotiation.
On 3/27/23 was documented, Pt (patient) ambulated around building on uneven and even surfaces. Patient performed gait training showing ability to maneuver through environment and crouch when needed without LOB (loss of balance) over lvl (level) and unlevl (unleveled) surfaces (grass/concrete) .
On 3/30/23 was documented, Pt performed gait training on level and unlevel surfaces both inside and outside for over 1000ft (feet). Also demonstrated ability to ascend and descend stairs to test balance and coordination .
On 4/1/23 was documented, Gait training throughout facility over 1000 (feet) .focusing on directional changes and obstacle negotiation .
On 4/3/23 was documented, Gait training over indoor/outdoor surfaces (I) (independently) without AD (assistive device) focusing on directional changes and obstacle negotiation with no LOB (loss of balance) noted.
The above reflected the resident's ability to safely ambulate over various level and unlevel surfaces for an extensive distance in 2023.
Further review of the clinical record revealed that Resident #120 has not had any falls in the calendar year of 2024 from 1/1/24 through this survey of 7/11/24.
A nurse's note dated 4/9/24 documented, He went to (name of drugstore across the street) .
A review of the sign out sheet for Resident #120 revealed the last time he actually signed out to go anywhere was on 10/18/23. There was no sign out for a leave of absence since 10/18/23 up through this survey of 7/11/24.
On 7/9/24 at 9:20 AM, Resident #120 states he goes out about three times a week across the street to the local drug store. He stated that he does not tell anyone and does not sign out. He stated that he has no issues with walking, has had no falls, and does not need the assistance of a walker or wheelchair. He stated that he looks out for traffic and is careful about crossing the street.
On 7/9/24 at 3:44 PM, an interview was conducted with LPN #3 (Licensed Practical Nurse). She stated that Resident #120 signs himself out frequently, goes to (local drug store across the street). She stated that she has not actually seen him cross the road, but that he is aware of his surroundings, is steady on feet, requires no assistive devices, has no disability with ambulation, but is hard of hearing. She stated that if a resident wants to leave the facility independently, that staff should check to see if the resident is their own RP (responsible party), check their BIMS, make sure they have their cell phone available, and have them sign out in the sign out book. She stated that everyone has to sign out when they leave. She stated that if possible, find out what they want and see if someone can go get it for them, so they do not have to go out if it is a really hot or cold day. She stated that risks would include heat stroke, passing out, getting hit by a car. When asked about the likelihood of these things happening, she stated that it could happen to anyone. She stated that a resident with a physical impairment or need for assistive devices increases the likelihood of something happening. She stated that therapy can help assess a resident to see if they are safe to leave independently.
On 7/10/24 at 2:22 PM an interview was conducted with LPN #8. She stated that she always see him in the building, never seen him go out. He has never notified me he was going out.
A review of the comprehensive care plan failed to reveal any interventions for the resident to go on leave of absence independently.
The facility policy, Leave of Absence documented, When patients leave the center for reasons other than a medical transfer initiated by the center, the patient and/or responsible party will provide signature, accepting complete responsibility of the patient and absolving the management, personnel, and the attending physician of responsibility for any deterioration in condition or accident that may happen while the patient is away. 1. Before a patient leaves the premises for any reason other than a medical transfer initiated by the center, the patient and/or responsible party must notify a licensed nurse on the unit. 2. A licensed nurse ensures that medical approval of the leave has been provided by the patient's provider. This can be in the form of a provider's order. 3. The Release of Responsibility for Leave of Absence (LOA) Form is filled out prior to leaving the center, the date, time, and signature of the person accepting responsibility is filled in. 4. The estimated time of return is provided to a licensed nurse. 5. A licensed nurse will make arrangements with the pharmacy for any necessary medications to be sent with the patient, if applicable. 6. If the patient will not be returning to the center on the same day as the beginning of the leave, the patient and/or responsible party must also notify nursing, Admissions Director, Business Office Manager, or the Administrator prior to or at the time of departure to initiate a Voluntary Bed Retention Agreement, if applicable. 7. A licensed nurse will note the LOA in the medical record. 8. Upon return to the center, the patient or responsible party will sign back in with date and time on the LOA form and a center staff will sign the form accepting responsibility of the patient at that time. 9. A licensed nurse will note return in the medical record, including the condition of the patient or any issues experienced during the LOA expressed by the patient or responsible party (fall, bruise, skin tear, change in condition, etc.). 10. Notify the provider, if necessary, and document in the medical record.
No further information was provided prior to exit. Based on observation, resident interview, staff interview, clinical record review and facility document review, it was determined that the facility staff failed to provide adequate supervision for residents smoking and leaving the building, for five of 50 residents in the survey sample; Residents #148, #90, #97, #120, and #136. 1. For Resident #148, the facility staff failed to provide resident supervision and safety for smoking. Resident #148 was assessed on the Smoking Safety Screen dated 3/8/24 and 6/8/24 as requiring supervision for smoking. On 7/8/24 at 3:00 PM, Resident #148 was observed smoking in an outdoor garden area with raised plant beds. There was no staff supervision present, no safe cigarette disposal receptacle, no fire blanket and no fire extinguisher in the immediate area. 2. For Resident #90 (R90), the facility staff failed to provide supervision for safety. 3. For Resident #97 (R97), the facility staff failed to provide supervision for safe leave of absence. On 7/9/24 at 5:50 PM, R97 was observed walking over to Walgreens without a cane. This resulted in Immediate Jeopardy (IJ) and SQC (substandard quality of care), which was identified in the area of Quality of Care on 7/8/24 at 4:17 PM for concerns related to smoking and on 7/9/24 at 5:30 PM for concerns related to unsupervised leave of absences. The plan of removal for the immediacy related to smoking concerns was accepted on 7/8/24 at 9:49 PM and as related to leave of absence concerns on 7/9/24 at 6:09 PM. The IJ was removed on 7/9/24 at 1:46 PM related to smoking concerns and on 7/11/24 at 10:32 AM related to the leave of absence issues, with the Scope and Severity lowered to a Level 2, Pattern.
4. For Resident #120, the facility staff failed to evidence staff were aware of the resident leaving the facility to ambulate unsupervised across the street to the local drug store. On 7/9/24 at 9:20 AM, Resident #120 stated that he leaves the facility two to three times a week to go across the street to the local drug store and does not sign out and does not notify staff that he is leaving.
5. The facility failed to provide a safe environment for Resident #136 On 7/9/24 at 7:53 AM, Resident #136 was observed ambulating independently with a rollator walker off facility property. Resident #136 was observed crossing the street at two points of a major intersection using the pedestrian walkways. Resident #136's gait was shuffling and show. He turned into the facility driveway and walked down the center of the driveway where cars were entering and exiting, rather than using the facility sidewalk. He was wearing a red and yellow safety vest.
The findings include:
1. For Resident #148, the facility staff failed to prevent the resident from smoking unsupervised, in an unapproved area devoid of any safety requirements (staff supervision, safe disposal of cigarette butts, smoking blanket and fire extinguisher) on 7/8/24 at 3:00 PM.
Resident #148 was admitted to the facility on [DATE] and was coded on the most recent MDS (Minimum Data Set), a quarterly assessment dated [DATE], as being cognitively intact in ability to make daily life decisions, scoring a 14 out of a possible 15 on the BIMS (Brief Interview for Mental Status exam).
On 7/8/24 at 3:00 PM, Resident #148 was observed self-propelling his wheelchair down the main front sidewalk of the facility towards the wooded area. He then turned right onto another sidewalk and entered through a gate into a facility garden area with raised plant beds. He then was observed obtaining a cigarette and lighter from his person and lighting it. At this time he was interviewed and stated that he goes to this area to smoke and he keeps his smoking materials on his person. He was observed to throw his cigarette butt on the ground.
On 7/8/24 at 3:24 PM, Resident #148 was still observed to be smoking in garden area. There was no staff present for supervision, no devices for the[TRUNCATED]
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, resident interview, staff interview, clinical record review and facility document review, it was determined that the facility staff failed to maintain the call bell in a position...
Read full inspector narrative →
Based on observation, resident interview, staff interview, clinical record review and facility document review, it was determined that the facility staff failed to maintain the call bell in a position accessible to the resident for two of 50 residents in the survey sample, Resident #89 and Resident #13.
The findings include:
1. For Resident #89 (R89), the facility staff failed to maintain the call light in a position where they could access it.
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 6/18/24, the resident scored 11 out of 15 on the BIMS (brief interview for mental status) assessment, indicating the resident was moderately impaired for making daily decisions. Section GG coded R89 not having any impairment in the upper extremities and being dependent on staff for toileting and requiring substantial/maximal assistance for personal hygiene.
The comprehensive care plan for R89 documented in part, ADLs (activities of daily living): [Name of R89] has an ADL self-care performance deficit r/t (related to) activity intolerance, muscle weakness, AMS (altered mental status) . Created on: 06/01/2020. Under Interventions it documented in part, .Encourage the resident to use bell to call for assistance. Frequently will not use call bell. Date Initiated: 10/26/2021. Created on: 06/01/2020
Revision on: 06/22/2023 .
On 7/9/24 at 9:05 a.m., an observation was made of R89 in their room. R89 was observed in bed with the call bell lying on the floor to the right side of the bed. At this time, an interview was attempted with R89. When asked if they could reach their call bell, R89 stated, I don't know where it is.
An additional observations of R89's call bell on the floor was made on 7/9/2024 at approximately 9:38 a.m.
On 7/10/24 at 10:10 a.m., an interview was conducted with CNA (certified nursing assistant) #2. CNA #2 stated that the call bell should be placed within reach of the resident at all times. She stated that this was to ensure that the resident could call them if they needed anything. She stated that staff rounded on residents at least every two hours and checked call bell placement anytime they went into the room. She stated that they clipped the call bell cord onto the sheet or the bed to make sure it stayed within reach of the resident and did not fall on the floor.
On 7/10/24 at 10:15 a.m., an interview was conducted with LPN (licensed practical nurse) #3. LPN #3 stated that the call bell should be within reach of the resident at all times for them to call if they needed assistance.
On 7/11/2024 at approximately 9:12 a.m., ASM #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services and ASM #4, the regional vice president of operations were made aware of the concern.
On 7/11/2024 at approximately 11:51 a.m., ASM (administrative staff member) #4, the regional vice president of operations stated that the facility did not have a policy regarding call bell placement.
No further information was presented prior to exit.
2. For Resident #13 (R13), the facility staff failed to maintain the call light in a position where they could access it.
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 6/13/24, the resident scored 7 out of 15 on the BIMS (brief interview for mental status) assessment, indicating the resident was severely impaired for making daily decisions. Section GG coded R13 not having any impairment in the upper extremities and being dependent on staff for toileting and requiring substantial/maximal assistance for personal hygiene.
The comprehensive care plan for R13 documented in part, Long Term Care: [Name of R13] requires assistance with their activities of daily living due to advanced age, chronic health conditions, recent hospitalization. Created on: 01/24/2023. Revision on: 04/08/2024. It further documented, Falls: [Name of R13] is at risk for falls. Created on: 01/23/2023. Under Interventions it documented in part, .remind the resident to use their call light to ask for assistance with ADLs (activities of daily living). Date Initiated: 01/23/2023.
On 7/9/24 at 8:24 a.m., an observation was made of R13 in their room. R13 was observed in bed asleep. The call bell was observed to be placed on the upper grab bar hanging down towards the floor behind R13's head out of reach. A staff member was observed entering R13's room at 8:28 a.m. and exited the room at 9:05 a.m. An observation of the call bell on 7/9/24 at 9:07 a.m. revealed the call bell in the same location out of R13's reach.
An additional observations of R13's call bell on 7/9/24 at 1:05 p.m. revealed the call bell in the same location.
On 7/10/24 at 10:10 a.m., an interview was conducted with CNA (certified nursing assistant) #2. CNA #2 stated that the call bell should be placed within reach of the resident at all times. She stated that this was to ensure that the resident could call them if they needed anything. She stated that staff rounded on residents at least every two hours and checked call bell placement anytime they went into the room. She stated that they clipped the call bell cord onto the sheet or the bed to make sure it stayed within reach of the resident.
On 7/10/24 at 10:15 a.m., an interview was conducted with LPN (licensed practical nurse) #3. LPN #3 stated that the call bell should be within reach of the resident at all times for them to call if they needed assistance. LPN #3 observed R13's call bell which was observed to be wrapped on the upper grab bar on the right side of the bed near the resident's head out of reach. LPN #3 stated that the call bell should be placed near the residents hand where they could easily reach it.
On 7/11/2024 at approximately 9:12 a.m., ASM #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services and ASM #4, the regional vice president of operations were made aware of the concern.
No further information was presented prior to exit.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, clinical record review and facility document review, it was determined the facility staff failed to im...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, clinical record review and facility document review, it was determined the facility staff failed to implement the baseline care plan for one of 50 residents in the survey sample, Residents #470.
The findings include:
The facility failed to implement a baseline care plan to monitor Resident #470's Aspira Drain.
Resident #470 was admitted to the facility on [DATE] with diagnosis that included but were not limited to cancer, congestive heart failure and adult failure to thrive.
The most recent MDS (minimum data set) assessment, a Medicare 5-day assessment, with an ARD (assessment reference date) of 7/10/24, coded the resident as scoring a 14 out of 15 on the BIMS (brief interview for mental status) score, indicating the resident was not cognitively impaired. A review of the MDS Section GG-functional abilities and goals coded the resident as requiring max assist for bed mobility, transfer, hygiene/bathing and supervision for eating.
A review of the comprehensive care plan dated 7/10/24 revealed, FOCUS: Resident has an Aspira drain. INTERVENTIONS: Drain as ordered. Dressing to be changed as ordered.
A review of the physician's orders dated 7/8/24, revealed, Right Aspira drain site: Cleanse with NS (normal saline), apply drain sponge and cover with Tegaderm every day shift.
On 7/8/24 at approximately 2:00 PM, an interview was conducted with Resident #470. When asked if she was a new admission, Resident #470 stated, yes, a few days ago. I have cancer and have a drain in.
An interview was conducted on 7/10/24 at 1:45 PM with LPN (licensed practical nurse) #2. When asked the purpose of the baseline care plan, LPN #2 stated, to identify the issues and care needs of the resident upon admission. When asked if a resident with a drain, should have the drain included in the baseline care plan, LPN #2 stated, yes.
On 7/11/24 at 9:10 AM, ASM (administrative staff member) #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services and ASM #4, the vice president of operations was made aware of the finding.
The facility's Baseline Care Plan policy revealed the following, A licensed nurse, in coordination with the interdisciplinary team, develops and implements an individualized care plan for each patient in order to provide effective, person-centered care, and the necessary health-related care and services to attain or maintain the highest practical physical, mental and psychosocial well-being of the patient. The baseline care plan is initiated and activated within 48 hours of admission.
No further information was provided prior to exit.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident interview, staff interview, clinical record review, and facility document review, it was determin...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident interview, staff interview, clinical record review, and facility document review, it was determined that the facility staff failed to review and revise the comprehensive care plan to reflect the residents current status for two of 50 residents in the survey sample; Resident #148 and #120.
The findings include:
1. For Resident #148, the facility staff failed to review and revise the comprehensive care plan to reflect the smoking assessment that the resident required supervision for smoking. The care plan documented on 3/8/24 that the resident may smoke independently.
Resident #148 was admitted to the facility on [DATE] and was coded on the most recent MDS (Minimum Data Set), a quarterly assessment dated [DATE], as being cognitively intact in ability to make daily life decisions, scoring a 14 out of a possible 15 on the BIMS (Brief Interview for Mental Status exam).
On 7/8/24 at 3:00 PM, Resident #148 was observed self-propelling his wheelchair down the main front sidewalk of the facility towards the wooded area. He then turned right onto another sidewalk and entered through a gate into a facility garden area with raised plant beds. He then was observed obtaining a cigarette and lighter from his person and lighting it. At this time he was interviewed and stated that he goes to this area to smoke and he keeps his smoking materials on his person. He was observed to throw his cigarette butt on the ground.
On 7/8/24 at 3:24 PM, Resident #148 was still observed to be smoking in garden area. There was no staff present for supervision, no devices for the safe disposal of cigarette butts, no fire blanket and no fire extinguisher was observed in the immediate area.
On 7/8/24 at 3:42 PM, in an interview with Resident #148 in his room, he stated that he keeps his lighter and cigarettes on himself at all times. He states that he smokes whenever he wants to and wherever he wants to when outside.
A review of the clinical record revealed that Resident #148 was assessed on Smoking Safety Screen dated 3/8/24 and 6/8/24 as requiring supervision for smoking.
A review of Resident #148's comprehensive care plan revealed one dated 3/8/24 for (Resident #148) prefers to smoke . This care plan included an intervention dated 3/8/24 for May smoke independently. This intervention did not accurately reflect the resident's Smoking Safety Screen that deemed the resident required supervision to smoke.
On 7/10/24 at 3:31 PM, an interview was conducted with LPN #9. She stated that care plans should reflect the resident's condition / status, and care needs, and that nursing can update the care plans as needed. She stated that Resident #148's care plan should have been updated to accurately reflect his status of requiring supervision for smoking, as determined by the Smoking Safety Screen.
The facility policy, Care Planning documented, A licensed nurse, in coordination with the interdisciplinary team, develops and implements an individualized care plan for each resident in order to provide effective, person-centered care .5. Care plans will be updated on an ongoing basis as changes in the patient occur, and reviewed quarterly with the quarterly assessment .
On 7/1/24 at 9:00 AM, ASM #1 (Administrative Staff Member) the administrator, ASM #2, the Director of Nursing, ASM #3 the Regional Director of Clinical Services, and ASM #4 the Regional [NAME] President of Operations, were made aware of the findings. No further information was provided by the end of the survey.
2. For Resident #120, the facility staff failed to review and revise the comprehensive care plan to address the resident's safety and preference of ambulating offsite independently to a local drug store across the street.
On the most recent MDS (Minimum Data Set), a quarterly assessment dated [DATE], Resident #120 was coded as moderately impaired in ability to make daily life decisions, scoring a 12 out of a possible 15 on the BIMS (Brief Interview for Mental Status exam).
On 7/9/24 at 9:20 AM, Resident #120 states he goes out about three times a week across the street to the local drug store. He stated that he does not tell anyone and does not sign out. He stated that he has no issues with walking, has had no falls, and does not need the assistance of a walker or wheelchair. He stated that he looks out for traffic and is careful about crossing the street.
A review of the physical therapy notes revealed the following:
On 3/21/23 was documented, Gait training over indoor/outdoor surfaces for distance of 1033 (feet) without AD (assistive device) over concrete/carpet/grass/tile .focusing on directional changes and obstacle negotiation.
On 3/27/23 was documented, Pt (patient) ambulated around building on uneven and even surfaces. Patient performed gait training showing ability to maneuver through environment and crouch when needed without LOB (loss of balance) over lvl (level) and unlevl (unleveled) surfaces (grass/concrete) .
On 3/30/23 was documented, Pt performed gait training on level and unlevel surfaces both inside and outside for over 1000ft (feet). Also demonstrated ability to ascend and descend stairs to test balance and coordination .
On 4/1/23 was documented, Gait training throughout facility over 1000 (feet) .focusing on directional changes and obstacle negotiation .
On 4/3/23 was documented, Gait training over indoor/outdoor surfaces (I) (independently) without AD (assistive device) focusing on directional changes and obstacle negotiation with no LOB (loss of balance) noted.
The above reflected the resident's ability to safely ambulate over various level and unlevel surfaces for an extensive distance in 2023.
A nurse's note dated 4/9/24 documented, He went to (name of drugstore across the street) .
A review of the comprehensive care plan revealed one dated 11/20/22 for Self-Directed Activities: the resident prefers to participate in self directed activities such as walking & sitting outside.
Further review of the comprehensive care plan failed to reveal any interventions for the resident to go on leave of absence independently to the local drug store across the street.
On 7/9/24 at 3:44 PM, an interview was conducted with LPN #3 (Licensed Practical Nurse). She stated that Resident #120 signs himself out frequently, goes to (local drug store across the street).
On 7/10/24 at 3:31 PM, an interview was conducted with LPN #9. She stated that care plans should reflect the resident's condition / status, and care needs, and that nursing can update the care plans as needed. She stated that Resident #120's care plan should have been updated to reflect his preference of leaving the facility independently.
On 7/1/24 at 9:00 AM, ASM #1 (Administrative Staff Member) the administrator, ASM #2, the Director of Nursing, ASM #3 the Regional Director of Clinical Services, and ASM #4 the Regional [NAME] President of Operations, were made aware of the findings. No further information was provided by the end of the survey.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. For Resident #151 (R151), the facility staff failed to properly groom the resident's fingernails.
On the following dates and...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. For Resident #151 (R151), the facility staff failed to properly groom the resident's fingernails.
On the following dates and times, R152 was seen with fingernails one to one and a half inches long that were yellow in color: 7/8/24 at 12:56 p.m. and 7/10/24 at 12:00 p.m.
R151 was admitted to the facility on [DATE]. On the admission MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 6/26/24, the resident was coded as having an upper extremity impairment on both sides.
A review of R151's clinical record revealed no evidence that she refused grooming assistance at any time.
On 7/11/24 at 10:35 a.m., CNA (certified nursing assistant) #3 was interviewed. She stated that nails should be groomed by CNAs every week.
On 7/11/24 at 10:23 a.m., LPN (licensed practical nurse) #2 was interviewed. She stated that the Resident's nails should be groomed and or cut at least every week.
On 7/11/24 at approximately 12:00 p.m., ASM (administrative staff member) #1 (the administrator), ASM#2 (the director of nursing), ASM #3 (regional director of clinical services) and ASM #4 (regional vice president of operations) were made aware of the above concern.
No further information was provided prior to exit.
Based on observation, resident interview, staff interview, clinical record review and facility document review, it was determined that the facility staff failed to provide ADL (activities of daily living) care for dependent residents for three of 50 residents in the survey sample, Residents #90, #89 and #151.
The findings include:
1. For Resident #90 (R90), the facility staff failed to provide ADL care to assist with personal hygiene. R90 was observed having untrimmed long fingernails on the right hand.
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 6/22/24, the resident scored 10 out of 15 on the BIMS (brief interview for mental status) assessment, indicating the resident was moderately impaired for making daily decisions. Section GG coded R90 requiring partial/moderate assistance for personal hygiene and supervision or touching assistance for bathing.
On 7/8/24 at 3:21 p.m., an observation was made of R90. R90's fingernails on the right hand revealed that they were approximately one-quarter to one-half inch long. At that time an interview was conducted with R90 who stated that they were paralyzed on that side and could not trim their nails themselves.
Additional observations of R90's fingernails were made on 7/8/24 at 4:30 p.m. and 7/10/24 at 10:15 a.m. The fingernails remained untrimmed on the right hand.
The comprehensive care plan for R90 documented in part, ADL (activities of daily living): [Name of R90] has an ADL self-care performance deficit r/t (related to) Activity Intolerance, Stroke . Created on:10/04/2019. Revision on: 05/28/2020. Under Interventions it documented in part, Personal Hygiene/Oral Care: The resident requires staff assistance. Date Initiated: 10/19/2019 .
Review of the clinical record failed to evidence documentation of refusal of care during the dates of observations documented above.
On 7/10/24 at 10:10 a.m., an interview was conducted with CNA (certified nursing assistant) #2. CNA #2 stated that residents fingernails were evaluated during care provided each day and were trimmed by them if the resident was not diabetic. She stated that if the resident was diabetic the nails were trimmed by the nurses. She stated that fingernails were assessed for trimming on shower days and during baths.
On 7/10/24 at 10:15 a.m., an interview was conducted with LPN (licensed practical nurse) #3. LPN #3 stated that residents fingernails were assessed on shower days or when observed when working with the resident. She observed R90's fingernails on the right hand and stated that they were long and needed trimming. LPN #3 asked R90 if they would allow her to trim the nails and R90 stated yes and proceeded to show LPN #3 where their nail clippers were kept.
On 7/11/2024 at approximately 9:12 a.m., ASM (administrative staff member) #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services and ASM #4, the regional vice president of operations were made aware of the concern.
The facility provided document, Mosby's Textbook for Long-Term Care Nursing Assistants ninth edition, 2024 documented in part, Nail and foot care prevents infection, injury, and odors. Hangnails, ingrown nails (nails that grow in at the side) and nails torn away from the skin cause skin breaks. These breaks are portals of entry for microbes. Long or broken nails can scratch skin or snag clothing .
No further information was presented prior to exit.
2. For Resident #89 (R89), the facility staff failed to provide ADL care to assist with personal hygiene. R89 was observed having a brown substance underneath their fingernails on 7/8/24 at 12:47 p.m., 7/9/24 at 9:05 a.m. and 7/10/24 at 9:19 a.m.
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 6/18/24, the resident scored 11 out of 15 on the BIMS (brief interview for mental status) assessment, indicating the resident was moderately impaired for making daily decisions. Section GG coded R89 requiring substantial/maximal assistance for personal hygiene and dependent on staff for bathing.
On 7/8/24 at 12:47 p.m., an observation was made of R89 in their room. R89 was observed lying in bed. Observation of R89's fingernails revealed that they were approximately one-quarter inch long with a brown substance underneath them. At that time an interview was conducted with R89 who stated that the staff did the best they could to take care of them.
Additional observations of R89's fingernails were made on 7/9/24 at 9:05 a.m. and 7/10/24 at 9:19 a.m. Observations revealed the brown substance remaining underneath the fingernails.
The comprehensive care plan for R89 documented in part, ADLs (activities of daily living): [Name of R89] has an ADL self-care performance deficit r/t (related to) activity intolerance, muscle weakness, AMS (altered mental status) . Created on: 06/01/2020. Under Interventions it documented in part, . Bathing/Showering: The resident is a staff assist. Date Initiated: 10/26/2021 . Personal Hygiene/Oral Care: The resident is a staff assist. Resident is edentulous. Date Initiated: 10/26/2021 .
Review of the clinical record failed to evidence documentation of refusal of care during the dates of observations documented above.
On 7/10/24 at 10:10 a.m., an interview was conducted with CNA (certified nursing assistant) #2. CNA #2 stated that residents fingernails were evaluated during care provided each day and were cleaned underneath if observed to be dirty. She stated that fingernails were assessed for trimming on shower days and during baths.
On 7/10/24 at 10:15 a.m., an interview was conducted with LPN (licensed practical nurse) #3. LPN #3 stated that residents fingernails were assessed on shower days or when observed when working with the resident. She stated that the residents nails were cleaned underneath during daily care and if the resident refused it would be documented. LPN #3 observed R89's fingernails and stated, I see what you mean. LPN #3 asked R89 if they would allow them to clean underneath their nails and R89 stated yes.
On 7/11/2024 at approximately 9:12 a.m., ASM (administrative staff member) #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services and ASM #4, the regional vice president of operations were made aware of the concern.
No further information was presented prior to exit.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on observation, staff interview, facility document review and clinical record review, it was determined the facility staff failed to assess and monitor a pressure injury for one of 50 residents ...
Read full inspector narrative →
Based on observation, staff interview, facility document review and clinical record review, it was determined the facility staff failed to assess and monitor a pressure injury for one of 50 residents in the survey sample, Resident #86.
The findings include:
For Resident #86 (R86), the facility staff failed to document the size and stage of the pressure injury (1) on 5/31/24, when treatment was initiated, and failed to monitor the wound with measurements weekly for healing.
On the most recent MDS (minimum data set) assessment, a quarterly assessment, with an assessment reference date of 6/8/24, the resident scored a 15 out of 15 on the BIMS (brief interview for mental status) score, indicating the resident was not cognitively impaired for making daily decisions. In Section M - Skin Conditions, R86 was coded as having one stage two (2) pressure injury.
The wound care nurse practitioner note dated 5/20/24 documented in part, Sacrum scar tissue.
The wound care physician notes dated, 5/31/24, documented in part, Sacrum - stage 2 measuring approximately 1x1x 0.1 cm (centimeters) in size.
The physician order dated 5/31/24, documented, Sacrum: Cleanse with wound cleanser, pat dry. Apply silver alginate and cover with border gauze dressing every day shift for Pressure Stage 2.
The TAR (treatment administration record) for May, June and July 2024, documented the above order. The treatment was documented as having been administered as ordered.
The Skin Observation forms dated the following documented:
5/19/24 - no documentation of a sacrum pressure injury.
5/27/24 - no documentation of a sacrum pressure injury.
6/3/24 - sacrum - pressure - no measurements or stage.
6/10/24 - sacrum - pressure - stage II - no measurements.
6/17/24 - sacrum - pressure - no measurements or stage.
6/24/24 - sacrum - pressure - no measurements or stage.
7/1/24 - sacrum - pressure - no measurements or stage.
7/8/24 - sacrum - pressure - no measurements or stage.
7/9/24 - sacrum - pressure - stage II - no measurements.
The comprehensive care plan dated, 3/1/24, documented in part, Focus: Skin Impairment: The resident has a skin impairment: R/L (right/left) groin necrotizing fasciitis post-surgical, R/L ABD (abdominal) rash, L axilla hidradenitis, L/R scrotum hidradenitis, R lateral groin post-surgical necrotizing fasciitis, L groin post-surgical necrotizing fasciitis, sacrum pressure. The Interventions documented in part, Notify MD (medical doctor) as indicated. Observe area for signs of improvement or decline. Treatment as ordered.
An interview was conducted with RN (registered nurse) #3, the wound nurse, on 7/10/24 at 1:28 p.m. When asked her involvement with R86's pressure injury on the sacrum, RN #3 stated the nurse stopped her in the hall and asked her to look at the resident's bottom. She stated she did and noted a stage II pressure injury. RN #3 stated she put treatment orders in place. When asked where her assessment and measurements of the wound were documented, RN #3 stated her note was in the order, she assumed the other nurse had done everything. She stated there is no documentation or tracking of the wound. When asked the process for tracking pressure injuries, RN #3 stated the wound nurse practitioner doesn't follow this resident as he is seen by a wound clinic. RN #3 was asked if that releases the facility from tracking the wound, RN #3 stated, no that releases just the wound nurse practitioner. When asked how the wounds are tracked, RN #3 stated the nurses do skin assessments weekly on the residents and should be measuring the wounds at that time. RN #3 was asked for documentation of measurements for this pressure injury, RN #3 stated there are none.
An interview was conducted with LPN (licensed practical nurse) #5 on 7/10/24 at 3:10 p.m. When asked the process for doing a skin assessment on residents, LPN #5 stated the nurse's do a skin observation weekly or every seven days, it's based on the resident's shower days. The nurses are to document any skin impairments on the form. LPN #5 was asked if a pressure injury is documented on the form, LPN #5 stated, yes. Do you measure the pressure injury, LPN #5 stated that it should be measured and documented on the form. LPN #5 was asked if a new area is found, what steps does she take, LPM #5 stated the nurse should notify the supervisor or unit manager, document was is observed and do a change in condition form.
An interview was conducted with ASM (administrative staff member) #2, the director of nursing, on 7/10/24 at 3:20 p.m. ASM #2 stated the skin assessments are done once a week or every seven days. Anything the nurse observes during the observation should be documented. When asked what is documented on the form if a resident has a pressure ulcer, ASM #2 stated the form should include what the wound nurse practitioner documents. ASM #2 stated R86 is not followed by the in house wound nurse practitioner, he goes to a wound clinic. ASM #2 was asked if the resident is not followed by the wound nurse practitioner, who measures the wounds, ASM #2 stated if a nurse finds a new area, they notify the wound care nurse and she does an assessment, measures and stages the wound, and puts in new orders for the wound. An LPN cannot stage a wound, but an RN can. The wound nurse is an RN.
On 7/11/24 at 8:19 a.m. ASM #2 returned and stated R86 has been followed by the wound clinic. There is no documentation on the skin observations regarding the wound. Treatment was put in place per recommendations from the wound clinic. R86 is to be seen at the wound clinic today, 7/11/24.
On 7/11/24 at 8:49 a.m. R86's pressure wound was observed with ASM #2 and LPN #6. The wound was measured to be 1.0 x 1.0 x 0 depth. ASM #2 stated it was a stage II pressure injury.
The facility policy, Wounds/Ski Impairments documented in part, Policy: Any wounds and/or skin impairments will be routinely assessed and treated as ordered. Procedure: 1. A licensed nurse will assess patients for any skin impairments, including surgical wound, vascular wounds/ulcers, pressure ulcers/injuries, skin tears, etc 2. The Skin Observation Tool will be complete by a licensed nurse at least every 7 days, detailing any wound/skin impairments. Documentation may also be found in the Wound Provider notes, if applicable. 3. Notify provider with updates and/or changes to the skin impairments. Obtain new orders as necessary. 4. Provide treatments as ordered.
ASM #1, the administrator, ASM #2, ASM #3, the regional director of clinical services, and ASM #4, the regional vice president of operations, were made aware of the above concern on 7/11/24 at 9:00 a.m.
No further information was provided prior to exit.
(1) A pressure injury is localized damage to the skin and underlying soft tissue usually over a bony prominence or related to a medical or other device. The injury can present as intact skin or an open ulcer and may be painful. The injury occurs as a result of intense and/or prolonged pressure or pressure in combination with shear. The tolerance of soft tissue for pressure and shear may also be affected by microclimate, nutrition, perfusion, co-morbidities and condition of the soft tissue. This information was obtained from the following website: http://www.npuap.org/resources/educational-and-clinical-resources/npuap-pressure-injury-stages/.
(2) Stage 2 Pressure Injury: Partial-thickness skin loss with exposed dermis Partial-thickness loss of skin with exposed dermis. The wound bed is viable, pink or red, moist, and may also present as an intact or ruptured serum-filled blister. This information was obtained from the following website: http://www.npuap.org/resources/educational-and-clinical-resources/npuap-pressure-injury-stages/.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0687
(Tag F0687)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview and clinical record review, facility staff failed to provide toenail care for one of 50 re...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview and clinical record review, facility staff failed to provide toenail care for one of 50 residents, Resident #56 (R56).
The findings include:
On the following dates and times was observed with toenails between one and one and half inches long: 7/8/24 at 8:45a.m., 7/9/24 at 9:11a.m., and 7/10/24 at 1:42 p.m.
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 4/4/24. R56 was coded as being dependent for personal hygiene. She was admitted on [DATE] with a diagnosis of traumatic brain dysfunction, seizure disorder and diabetes mellitus.
A review of R56's care plan revealed, Personal hygiene care/Oral Care: The resident requires total assistance of 2x assist .Assist with all cares/ADLs
On 7/11/24 at 10:008 a.m., CNA (certified nursing assistant) #1 was interviewed. She stated that residents receive nail care every day. She stated that if the resident is diabetic then the podiatrist will cut and do toenail care.
On 7/11/24 at 10:59 a.m., LPN (licensed practical nurse) #2 was interviewed. She stated that nurses and nurse's aides can do nail care and toenail care. She also stated that if the resident has fungus or they are diabetic then the podiatrist will complete nail care on toenails.
On 7/11/24 at approximately 12:00 p.m., ASM (administrative staff member) #1 (the administrator), ASM#2 (the director of nursing), ASM #3 (regional director of clinical services) and ASM #4 (regional vice president of operations) were made aware of the above concern.
No further information was provided prior to exit.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview and facility document review, the facility staff failed to apply splints for one of 50 res...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview and facility document review, the facility staff failed to apply splints for one of 50 residents, Resident #56.
Findings include:
For Resident #56 (R56), the facility staff failed to apply right- and left-hand splints.
On the following dates and times, R56 was observed in bed. Left-and right-hand splints were not visible on the resident: 7/8/24 at 3:20 p.m.; 7/9/24 at 9:15 a.m.; and 7/10/24 at 10:15 a.m.
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 4/4/24. R56 was coded as having functional limitation in range of motion. She has an upper extremity impairment on both sides. She was admitted on [DATE] with a diagnosis of traumatic brain dysfunction, seizure disorder, persistent vegetative state and diabetes mellitus.
A review of R56's care plan revealed, in part: Nursing/Rehab Restorative: Splint. PROM (passive range of motion) first then apply splint. See pictures for BUE (bilateral upper extremity) splints located in room, staff in-service provided. Wear all splints/positioner for four hours each shift (8 hours daily, as tolerated). Check for skin irritation/pain.
A review of R56's OT Discharge Summary revealed, Discharge Recommendations and Status .Restorative Programs Established/Trained = Restorative Splint and Brace Program, Other Restorative Program (positioning program) Splint and Brace Program Established/ Trained: B hand splints.
On 7/11/24 at 10:23 a.m., LPN (licensed practical nurse) #2 was interviewed. She stated that staff would know that a resident needs a splint by the physician's orders. She also stated that therapy will communicate if splints are needed. She also stated if splints are needed, they would be documented in the care plan instead of the physician's orders or the mars (medical administration records) and tars (treatment administration records). She also stated that R56 is contracted and should be wearing a splint. She says that staff usually puts the splints on during the night shift and they must have forgotten this time.
On 7/11/24 at approximately 12:00 p.m., ASM (administrative staff member) #1 (the administrator), ASM#2 (the director of nursing), ASM #3 (regional director of clinical services) and ASM #4 (regional vice president of operations) were made aware of the above concern.
No further information was provided prior to exit.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, resident interview, staff interview, clinical record review and facility document review, it was determined that the facility staff failed to maintain a urinary catheter bag in a...
Read full inspector narrative →
Based on observation, resident interview, staff interview, clinical record review and facility document review, it was determined that the facility staff failed to maintain a urinary catheter bag in a sanitary manner for one of 50 residents in the survey sample, Resident #89.
The findings include:
1. For Resident #89 (R89), the facility staff failed to maintain a urinary catheter collection bag in a sanitary manner.
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 6/18/24, the resident scored 11 out of 15 on the BIMS (brief interview for mental status) assessment, indicating the resident was moderately impaired for making daily decisions. Section H coded R89 having an indwelling catheter.
On 7/9/24 at 9:05 a.m., an observation was made of R89 in their room. R89 was observed lying in bed with a catheter bag hanging off of the right side of the bed frame. The catheter bag was observed to be touching the floor. At that time an interview was conducted with R89 who stated that the staff took care of the catheter and they did not do anything with it.
Additional observation of R89's urinary catheter bag touching the floor was made on 7/9/24 at 9:45 a.m. and observation of the urinary catheter bag on 7/10/24 at 9:18 a.m. revealed the bag attached to the grab bar at the head of the bed. R89's head of bed was observed to be elevated with the catheter bag being at R89's chest level.
The comprehensive care plan for R89 documented in part, Catheter: [Name of R89] has a foley catheter. Created on: 02/23/2024. Revision on: 06/24/2024.
On 7/10/24 at 10:10 a.m., an interview was conducted with CNA (certified nursing assistant) #2. CNA #2 stated that urinary catheter bags should be kept lower than the abdominal area to ensure that it drained properly. She stated that the bag should not be on the floor because it was unsanitary.
On 7/10/24 at 10:15 a.m., an interview was conducted with LPN (licensed practical nurse) #3. LPN #3 stated that the urinary catheter bag should be kept below the bladder for proper drainage and to decrease the change of infection. She stated that the bag should not touch the floor because of the chance of infection. She stated that R89 was not a resident that she knew of that messed with the catheter or the urinary catheter bag and if they did it would be documented on the care plan.
On 7/11/2024 at approximately 9:12 a.m., ASM (administrative staff member) #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services and ASM #4, the regional vice president of operations were made aware of the concern.
The facility policy Urinary Catheterizations dated 1/29/24, documented in part, .6. Maintain drainage bags below the level of the bladder. 7. Ensure drainage bags are not touching the floor .
No further information was provided prior to exit.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, staff interivew, facility document review and clinical record review, it was determined the facility staff failed to provide respiratory services for two of 50 residents in the s...
Read full inspector narrative →
Based on observation, staff interivew, facility document review and clinical record review, it was determined the facility staff failed to provide respiratory services for two of 50 residents in the survey sample, Residents #56 and
#13.
The findings include:
1. For Resident #56 (R56), the facility staff failed to administer oxygen at the physician prescribed rate of five liters per minute.
R 56's comprehensive care plan revised on 6/22/21 documented, Oxygen administered as ordered .Further review of R56's clinical record revealed a physician's order dated 06/14/2024 for oxygen at five liters w/ 28% humidification via trach every day and night shift.
On 7/8/24 at 3:00 p.m. and 3/9/24 at 3:18 p.m. and 7/10/24 at 9 p.m., R56 was observed lying in bed receiving oxygen via trach at two and a half liters per minute, as evidenced by the middle of the ball in the oxygen concentrator flowmeter positioned on the two-and-a-half line.
On 7/11/24 at 10:23 a.m., an interview was conducted with LPN (licensed practical nurse) #2. LPN#2 stated that nurses should know how much oxygen to administer based on the resident's order. She also stated that the middle of the ball in the oxygen concentrator should be on the five-liter line if the order is for five liters.
On 7/11/24 at approximately 12:00 p.m., ASM (administrative staff member) #1 (the administrator), ASM#2 (the director of nursing), ASM #3 (regional director of clinical services) and ASM #4 (regional vice president of operations) were made aware of the above concern.
A review of the facility policy, Respiratory Care & Oxygen Equipment, revealed in part, Follow provider's order including' a. Delivery system type b. Flow rate and/or FiO2 concentration, if indicated c. Frequency and duration .Evaluate and document oxygen saturation level and/or vital signs, as indicated.
No further information was presented prior to exit.
2. For Resident #13 (R13), the facility staff failed to provide oxygen as ordered.
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 6/13/24, the resident scored 7 out of 15 on the BIMS (brief interview for mental status) assessment, indicating the resident was severely impaired for making daily decisions. Section O documented R13 receiving oxygen at the facility.
On 7/8/24 at 1:07 p.m., an observation was made of R13 in their room. R13 was observed in bed wearing a hospital gown and an oxygen nasal cannula. The nasal cannula was observed to be attached to a portable oxygen tank placed in a rolling carrier beside R13's bed. Observation of the portable tank revealed the tank flow dial set at zero with the oxygen gauge reading empty. R13 was not able to be interviewed due to their cognition level. Additional observation of R13's nasal cannula attached to the portable oxygen tank set at zero was made on 7/8/24 at approximately 1:30 p.m.
The physician orders for R13 documented in part, Oxygen Therapy - Oxygen at 2L/min (liters per minute) via NC (nasal cannula) every day and night shift. Order Date: 01/08/2024.
The comprehensive care plan for R13 documented in part, Respiratory: [Name of R13] is at risk for respiratory complications secondary to supplementary oxygen requirement. Created on: 01/08/2024. Revision on: 01/08/2024. Under Interventions it documented in part, .administer oxygen as ordered. Date Initiated: 01/08/2024 .
On 7/10/24 at 10:15 a.m., an interview was conducted with LPN (licensed practical nurse) #3. LPN #3 stated that oxygen concentrators were used in resident's rooms and they used the portable oxygen tanks when residents were going out for appointments or going for therapy or activities. She stated that anytime a resident was using a portable tank they should get a full tank and it was checked every two hours to ensure that it was running low or empty. She stated that she was not sure why R13 was on the portable tank in their room and that perhaps the concentrator had malfunctioned but the portable oxygen should not have been empty or set to zero.
On 7/11/2024 at approximately 9:12 a.m., ASM (administrative staff member) #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services and ASM #4, the regional vice president of operations were made aware of the concern.
The facility policy Respiratory Care & Oxygen Equipment dated 1/29/24 documented in part, .Oxygen therapy will be administered per provider's order, according to current standards of practice and equipment will be maintained and stored in a safe and appropriate manner .
No further information was presented prior to exit.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, facility document review, and clinical record review, the facility staff failed to act on a pharmacy r...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, facility document review, and clinical record review, the facility staff failed to act on a pharmacy recommendation for one of 50 residents in the survey sample, Resident #79.
The findings include:
For Resident #79 (R79), the facility staff failed to act on a pharmacy recommendation dated 4/24/24 to discontinue PRN (as needed) use of the anti-psychotic medication Zyprexa (1).
A review of R79's clinical record revealed a physician's order dated 4/1/24 for Olanzapine (Zyprexa) 2.5 mg (milligrams) by mouth every 24 hours as needed.
A pharmacy recommendation dated 4/24/24 documented, Recommend discontinue PRN use of ZYPREXA for agitation. The use of an antipsychotic medication for 3 or less days does not allow adequate time for the medication to reach therapeutic antipsychotic levels and is primarily used for its sedative/anti-anxiety effects. Suggest considering the use of a medication from a different therapeutic class such as a short acting benzodiazepine for PRN use with 14 day stop. Per state and federal guidelines: PRN orders for anti-psychotic drugs are limited to 14 days and cannot be renewed unless the attending physician or prescribing practitioner evaluates the resident for the appropriateness of that medication. The recommendation requested a physician/prescriber response and offered three options:
Discontinue ZYPREXA PRN
Start the following: __________
No change at this time as the benefit outweighs the risk.
No response was documented by the physician or prescriber on the recommendation or in R79's clinical record, and the resident remained on PRN Zyprexa.
On 7/10/24 at 3:03 p.m., an interview was conducted with ASM (administrative staff member) #2 (the director of nursing) and ASM #3 (the regional director of clinical services) ASM #3 stated the pharmacist places routine recommendations into a computer portal. ASM #2 stated she checks the portal almost daily or every other day, uploads the recommendations, prints the recommendations and gives the recommendations to the assigned nurse practitioner. ASM #2 stated the nurse practitioners are supposed to document and implement their response to the recommendations then the recommendations should be given to the medical records employee, so they are loaded into resident charts. ASM #3 stated the practitioners should document a response on the pharmacy recommendation form even if they decline the recommendation.
On 7/11/24 at 8:52 a.m., ASM #1 (the administrator) and ASM #2 were made aware of the above concern.
The facility policy titled, Medication Regimen Review documented, 1. The consultant pharmacist will provide Medication Regimen Review (MRR) reports to provider and Director of Nursing within 72 hours of completion.
2. The physician is to review and sign the patient's individual MRR and document that he/she has reviewed the pharmacist's identified irregularities within 30 days of receipt.
No further information was presented prior to exit.
Reference:
(1) Olanzapine (Zyprexa) is used to treat the symptoms of schizophrenia (a mental illness that causes disturbed or unusual thinking, loss of interest in life, and strong or inappropriate emotions) in adults and teenagers [AGE] years of age and older. It is also used to treat bipolar disorder (manic depressive disorder; a disease that causes episodes of depression, episodes of mania, and other abnormal moods) in adults and teenagers [AGE] years of age and older. Olanzapine is in a class of medications called atypical antipsychotics. It works by changing the activity of certain natural substances in the brain. This information was obtained from the website: https://medlineplus.gov/druginfo/meds/a601213.html.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview and clinical record review, the facility staff failed to ensure a resident was free from an unnecessary...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview and clinical record review, the facility staff failed to ensure a resident was free from an unnecessary psychotropic medication for one of 50 residents in the survey sample, Resident #79.
The findings include:
For Resident #79 (R79), the facility staff failed to ensure the physician or prescribing practitioner evaluated the resident for continued use of the as needed antipsychotic medication Olanzapine (1) and documented the rationale for the continued use.
A review of R79's clinical record revealed a physician's order dated 4/1/24 for Olanzapine (Zyprexa) 2.5 mg (milligrams) by mouth every 24 hours as needed for terminal delirium related to dementia. A review of R79's June 2024 revealed the resident received as needed Olanzapine on 6/5/24.
On 7/10/24 at 3:03 p.m., an interview was conducted with ASM (administrative staff member) #2 (the director of nursing). ASM #2 stated as needed antipsychotic medications should only be ordered for up to 14 days but R79 was having hallucinations and behaviors. ASM #2 stated staff had tried alternative medications that were unsuccessful so R79's hospice physician wanted to continue the use of as needed Olanzapine. ASM #2 was asked to provide physician documentation that the physician evaluated R79 for the continued use of as needed Olanzapine and physician documentation regarding the rationale for continued use. On 7/11/24 at 8:26 a.m., ASM #2 stated she could not provide the requested physician documentation.
On 7/11/24 at 8:52 a.m., ASM #1 (the administrator) and ASM #2 were made aware of the above concern. The facility did not have a policy regarding as needed antipsychotic medications.
No further information was presented prior to exit.
Reference:
(1) Olanzapine (Zyprexa) is used to treat the symptoms of schizophrenia (a mental illness that causes disturbed or unusual thinking, loss of interest in life, and strong or inappropriate emotions) in adults and teenagers [AGE] years of age and older. It is also used to treat bipolar disorder (manic depressive disorder; a disease that causes episodes of depression, episodes of mania, and other abnormal moods) in adults and teenagers [AGE] years of age and older. Olanzapine is in a class of medications called atypical antipsychotics. It works by changing the activity of certain natural substances in the brain. This information was obtained from the website: https://medlineplus.gov/druginfo/meds/a601213.html.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. For Resident #519 (R519), the facility staff failed to secure medications safely in resident room.
On 7/8/24 at 3:49 p.m. an...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. For Resident #519 (R519), the facility staff failed to secure medications safely in resident room.
On 7/8/24 at 3:49 p.m. an observation R519's room revealed Fluticasone Propionate and Salmeterol 100mcg/50mcg Aerosol Powder on top of the bedside table that was left unattended.
R519's clinical record revealed a physician order dated 7/4/24, Fluticasone-Salmeterol 100-50 MCG/ACT Aerosol Powder, breath activated . 1 inhalation in nostril every 12 hours.
On 7/11/24 at 10:32 a.m., LPN (licensed practical nurse) #2 was interviewed. She stated that inhaler should not have been at the bedside. She stated that it is supposed to be stored in the medication cart with the other inhalers. She also stated that residents should not use it without supervision.
On 7/11/24 at approximately 12:00 pm., ASM (administrative staff member) #1 (the administrator), ASM#2 (the director of nursing), ASM #3 (regional director of clinical services) and ASM #4 (regional vice president of operations) were made aware of the above concern.
A review of the facility's policy, Storage of Medications revealed, in part: Medications and biologicals are stored safely, securely, and properly, following manufacturer's recommendations or those of the supplier. The medications supple is accessible only to licensed nursing personnel, pharmacy personnel, or staff members lawfully authorized to administer medications .Medications labeled for individual residents are stored separately from floor stock medications when not in the medication cart.
No further information was provided prior to exit.
Based on observation, staff interview and facility document review it was determined facility staff failed to secure
Medications in a safe and secure manner according to professional standards for two of 50 residents, Resident #32 and Resident #159.
The findings include:
1. The facility staff failed to ensure medications were locked. During the initial resident observation on 7/8/24 at approximately 12:45 PM, upon entrance to Resident #32's room, a bottle of Nystatin powder was observed on bedside table. The Nystatin powder was labeled for another resident. Resident #32 was not in the room at the time. At approximately 3:15 PM Resident #32 was in room, when asked about the Nystatin powder with the other resident's name, Resident #32 stated, no, I did not notice the bottle on the dresser.
Resident #32 was admitted to the facility on [DATE] with diagnosis that included but were not limited to ASCVD (atherosclerotic cardiovascular disease), CKD (chronic kidney disease) and CHF (congestive heart failure).
The most recent MDS (minimum data set) assessment, a quarterly assessment, with an ARD (assessment reference date) of 6/27/24, coded the resident as scoring a 14 out of 15 on the BIMS (brief interview for mental status) score, indicating the resident was not cognitively impaired. A review of the MDS Section GG-functional abilities and goals coded the resident as requiring moderate assist for bed mobility; total dependence for transfer, hygiene/bathing and supervision for eating.
A review of the comprehensive care plan dated 4/2/21 revealed, FOCUS: The resident has a potential for skin
impairments related to decreased mobility and occasional incontinence. INTERVENTIONS: Keep skin clean and dry. Lotion to dry skin. Moisture barrier cream as needed for protection of skin.
An interview was conducted on 7/8/24 at 12:50 PM with LPN (licensed practical nurse) #1. When asked about the Nystatin bottle with a different resident's name on Resident #32's bedside table, LPN #1 stated, no, this is not hers. It must have been left in here when rooms were changed. I am disposing of this now. When asked how medications are to be stored, LPN #1 stated, they are to be locked in the medication cart.
On 7/11/24 at 9:10 AM, ASM (administrative staff member) #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services and ASM #4, the vice president of operations was made aware of the finding.
According to the facility's Storage of Drugs-Biologicals policy which revealed, Only licensed nurses, pharmacy personnel, and those lawfully authorized to administer medications are permitted to access medications. Medication rooms, carts and medication supplies are locked when they are not attended by persons with authorized access.
No further information was provided prior to exit.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0909
(Tag F0909)
Could have caused harm · This affected 1 resident
Based on observation, staff interview, facility document review, and clinical record review, it was determined the facility staff failed to perform a bed inspection for two of 50 residents in the surv...
Read full inspector narrative →
Based on observation, staff interview, facility document review, and clinical record review, it was determined the facility staff failed to perform a bed inspection for two of 50 residents in the survey sample, Residents #86 and #124.
The findings include:
1. For Resident #86, the facility staff failed to inspect the resident's bariatric bed for safety and entrapment.
Resident #86 was observed on 7/8/24 at approximately 12:00 p.m. in bed, with two half side rails on each side of the bed.
The physician order dated, 5/18/24, documented, BB (bariatric bed) bed with 1/2 side rails.
The review of the bed inspection book documented the bed in the room was not the same as the current bed in the room. There was no bed inspection for the bariatric bed in use.
An interview was conducted with OSM (other staff member) #18, the director of maintenance on 7/10/24 at 2:11 p.m. When asked the process to ensure the bariatric beds are inspected for safety and entrapment, OSM #18 stated if there is a bariatric bed need, we place it i the room but only on the B side of the room. We do an inspection based on the same regulations for the other bed frames. OSM #18 was asked why the inspection was not done on the bed, OSM #18 stated he didn't know why.
The facility policy, Bed System Audits, documented, Maintenance will maintain an inventory of all beds in order to conduct annual and intermittent bed system audits to identify and mitigate areas of risk for possible entrapment and bed safety. Procedure: 1. Maintenance will identify each Center bed by number and will conduct a full bed audit on each bed a minimum of annually. The audit will include the frame, the deck, the headboard, the footboard, the mattress, and any installed bed rails and/or assisted devices. 2. Maintenance will also conduct intermittent audit immediately upon notification by nursing of any individual change of bed frame, an assistive device, a mattress, or a bed rail. Maintenance and nursing will collaborate in order to identify gaps, ensure a tight fit of mattress to the bed system and if appropriate, to inspect for mattress compressibility. 3. Any bed rail and or mattress changes implemented and/or newly purchased separately from the bed frame system, will be assessed collaboratively for compatibility in width HBSW (Hospital Bed Safety Workgroup) guidelines, and other areas of potential safety risk within the bed system. 5. For all annual audits, maintenance will complete documentation as outlines in the preventative maintenance electronic record and file printed audits in the Bed System Audits Tracking Manual. Intermittent audits will be recorded on the Intermittent Bed Audit to Reduce the Risk of Patient Entrapment Documentation Log located in the Bed System Audits Tracking Manual.
ASM (administrative staff member) #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services, and ASM #4, the regional vice president of operations, were made aware of the above concern on 7/11/24 at 9:00 a.m.
No further information was provided prior to exit.
2. 1. For Resident #124, the facility staff failed to inspect the resident's bariatric bed for safety and entrapment.
Resident #124 was observed in bed on 7/8/24 at approximately 12:10 p.m. There were two half side rails in place on both sides of the bed.
The physician's order dated 2/8/24, documented, BB bed with 1/2 side rails.
The review of the bed inspection book documented the bed in the room was not the same as the current bed in the room. There was no bed inspection for the bariatric bed in use.
An interview was conducted with OSM (other staff member) #18, the director of maintenance on 7/10/24 at 2:11 p.m. When asked the process to ensure the bariatric beds are inspected for safety and entrapment, OSM #18 stated if there is a bariatric bed need, we place it i the room but only on the B side of the room. We do an inspection based on the same regulations for the other bed frames. OSM #18 was asked why the inspection was not done on the bed, OSM #18 stated he didn't know why.
ASM #1, ASM #2, ASM #3, and ASM #4, were made aware of the above concern on 7/11/24 at 9:00 a.m.
No further information was provided prior to exit.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0944
(Tag F0944)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview and facility document review, it was determined that the facility staff failed to ensure QAPI (quality ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview and facility document review, it was determined that the facility staff failed to ensure QAPI (quality assurance and performance improvement) program training was completed for one of five employees reviewed, OSM (other staff member) #5.
The findings include:
For OSM #5, a floor technician, the facility staff failed to ensure training regarding the facility QAPI program was completed.
OSM #5 was hired on 6/1/23. The facility staff failed to provide evidence that OSM #5 had completed training regarding the facility QAPI program.
On 7/11/24 at 10:52 a.m., an interview was conducted with ASM (administrative staff member) #4, the regional vice president of operations. ASM #4 stated that OSM #5 was set to have the QAPI training added to their computer based training program in August. He stated that they do a general orientation but was not sure if QAPI training was put in the system upon hire or not. He stated that he would look further to see if there was anything more to provide.
On 7/11/24 at 11:51 a.m., ASM #4 stated that they did not have anything additional to provide for OSM #5. At that time, ASM #2, the director of nursing confirmed that during general orientation QAPI training was one of the courses that was initially included in the onboarding education for staff to complete.
The facility assessment dated [DATE] documented in part, .Staff training/education and competencies . Review Relias (computer based education) Annual Calendar for list of all staff training, and the HR (human resource) general orientation completed upon hire, as well as any other specialized program training that may currently be utilized in the Center . The attached Relias 2024 Onboarding All Employees calendar documented a course named Quality & You: QAPI included in the onboarding education for all staff as well as annual education for all staff.
On 7/11/24 at 11:57 a.m., ASM #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services and ASM #4, the regional vice president of operations were made aware of the concern.
No further information was provided prior to exit.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected multiple residents
Based on staff interview and facility document review, the facility staff failed to respond to resident council concerns for two of three resident council meetings reviewed, the May 2024 and June 2024...
Read full inspector narrative →
Based on staff interview and facility document review, the facility staff failed to respond to resident council concerns for two of three resident council meetings reviewed, the May 2024 and June 2024 meetings.
The findings include:
The facility staff failed to respond to the May and June 2024 resident council's concern regarding missing clothing.
A review of the 5/8/24 resident council meeting notes revealed the following documentation, .clothes still missing . A review of the 6/5/24 resident council meeting notes revealed the following documentation, .clothes still being missing .
A review of the facility grievances/concerns for 5/1/24 to the present failed to evidence any grievances regarding the resident council's missing clothing concerns.
On 7/9/2024 at 2:45 p.m., a request was made to ASM (administrative staff member) #4, the regional vice president of operations, for evidence of resolution of concerns voiced by residents regarding missing clothing during the May and June 2024 meetings.
On 7/10/24 at 2:28 p.m., an interview was conducted with OSM (other staff member) #14, environmental service director. OSM #14 stated that activities was responsible for resident council meetings and they were not aware of any concerns voiced during meetings about ongoing missing clothing. OSM #14 stated that they handled individual resident concerns as they came in.
On 7/10/24 at 3:22 p.m., an interview was conducted with OSM #16, the director of recreation. OSM #16 stated that they followed up with resident council concerns differently depending on what the concerns were. She stated that for the concerns with missing clothing she reported them to the director of environmental services and the administrator. She stated that this was a verbal conversation directly with the managers and she had not been documenting any grievances or resolutions of the concerns since she had been in the positron and moving forward she planned to start documenting them.
On 7/11/24 at approximately 9:00 a.m., ASM #4, the regional vice president of operations stated that they did not have any evidence of resolution for the concerns regarding missing clothing voiced at the May and June 2024 resident council meetings.
The facility policy titled, Resident Council dated 11/1/23, documented in part, .10. Document Council concerns/problems in Resident Council Minutes. Individual concerns should be addressed on the company's Service Concern report form. Immediately inform the Administrator of any urgent issues, council concerns, or problems .
The facility policy Grievance dated 1/23/20, documented in part, The patient has a right to voice/file grievances/complaints (orally, in writing or anonymously) without fear of discrimination or reprisal. The Administrator serves as the grievance official of the Center and is responsible for overseeing the grievance process and for receiving and tracking their conclusion.
On 7/11/2024 at approximately 9:12 a.m., ASM #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services and ASM #4, the regional vice president of operations were made aware of the concern.
No further information was provided prior to exit.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected multiple residents
Based on staff interview, facility document review, and clinical record review, the facility staff failed to notify the physician of a change in condition and possible need to alter treatment for one ...
Read full inspector narrative →
Based on staff interview, facility document review, and clinical record review, the facility staff failed to notify the physician of a change in condition and possible need to alter treatment for one of 50 residents in the survey sample, Resident #106.
The findings include:
For Resident #106 (R106), the facility staff failed to notify the physician of the resident's blood sugars over 400, per a physician's order.
A review of R106's clinical record revealed a physician's order dated 4/15/24 that documented to administer Lispro insulin (used to treat diabetes) based on a sliding scale dependent on the resident's blood sugar before meals and at bedtime. The order further documented to contact the physician if R106's blood sugar was greater than 400 or less than 60.
A review of R106's June 2024 and July 2024 MARs (medication administration records) revealed the following blood sugars on the following dates:
6/2/24 11:00 a.m.- 450
6/9/24 11:00 a.m.- 441
6/10/24 7:30 a.m.- 401
6/10/24 4:00 p.m.- 432
6/11/24 4:00 p.m.- 448
6/12/24 4:00 p.m.- 410
6/17/24 9:00 p.m.- 425
6/19/24 4:00 p.m.- 448
6/23/24 9:00 p.m.- 404
6/25/24 11:00 a.m.- 449
7/3/24 9:00 p.m.- 450
7/6/24 9:00 p.m.- 419
Further review of R106's clinical record (including the June 2024 and July 2024 MARs, nurses' progress notes, and change in condition notes) failed to reveal the facility staff contacted the physician regarding any of R106's above blood sugars that were greater than 400.
On 7/10/24 at 1:12 p.m., an interview was conducted with RN (registered nurse) #3. RN #3 stated that if a resident has a physician's order to contact the physician for a blood sugar greater than a specified parameter, then when the nurse takes the blood sugar and the blood sugar is over the parameter, the nurse needs to call the physician to get new orders or maintain current orders, depending on what the physician wants to do. RN #3 stated nurses should evidence the physician notification by documenting a progress note or change in condition note.
On 7/11/24 at 8:52 a.m., ASM (administrative staff member) #1 (the administrator) and ASM #2 (the director of nursing) were made aware of the above concern.
The facility policy titled, Significant Change in Condition documented, 1. A licensed nurse will assess the patient for signs and symptoms of change in condition. 2. Notify provider and document in Progress Notes.
No further information was presented prior to exit.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation, resident interview, staff interview, facility document review and clinical record review, the facility staff failed to maintain a homelike environment for six of 50 residents in ...
Read full inspector narrative →
Based on observation, resident interview, staff interview, facility document review and clinical record review, the facility staff failed to maintain a homelike environment for six of 50 residents in the survey sample, Residents #10, #131, #121, #32, #34 and #104.
The findings include:
1. For Resident #10 (R10), the facility staff failed to maintain the resident's room in good repair.
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 6/5/24, the resident scored 15 out of 15 on the BIMS (brief interview for mental status), indicating the resident was cognitively intact for making daily decisions.
On 7/8/24 at approximately 3:30 p.m., an observation of R10's room was conducted. Blue tape approximately one inch wide was observed along a portion of the baseboard approximately 12 inches long on the window side of the room. The electrical outlet above the area was observed to have blue tape surrounding the plastic outlet cover on each side. The un-taped portions of the baseboard on the wall located along the window side of the room were observed to be separated from the wall exposing dried adhesive on the wall beneath. At this time an interview was conducted with R10 who stated that they did not know why the tape was there and it had been that way for a long time. R10 stated that someone had worked on that area a long time ago and never came back and they felt that it was ugly.
On 7/10/24 at 12:40 p.m., an interview was conducted with OSM (other staff member) #17, maintenance technician. OSM #17 stated that they had a program on their phone which showed them any open work orders for repairs needed in the facility. OSM #17 reviewed the program and stated that there were no open work orders for R10's room. OSM #17 observed the blue tape approximately one inch wide along the baseboard approximately 12 inches long on the window side of the room, the electrical outlet above the area with blue tape surrounding the plastic outlet cover on each side and the un-taped portions of the baseboard on the wall that were separated from the wall exposing dried adhesive on the wall beneath. He stated that it appeared that someone may have attempted to glue the baseboard back to the wall and then taped it to dry and it had not been removed. He stated that he was not sure why the electrical outlet cover was taped. OSM #17 stated that he did not think that the room was homelike with the baseboard coming off the wall and the blue tape on parts of the baseboard and electrical outlet.
On 7/11/24 at approximately 9:12 a.m., ASM (administrative staff member) #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services and ASM #4, the regional vice president of operations were made aware of the concern.
On 7/11/24 at approximately 11:51 a.m., ASM #4, the regional vice president of operations stated that the facility did not have a policy regarding maintaining a homelike environment.
No further information was presented prior to exit.
2. For Resident #131 (R131), the facility staff failed to maintain the resident's room in good repair.
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 5/16/24, the resident scored 15 out of 15 on the BIMS (brief interview for mental status), indicating the resident was cognitively intact for making daily decisions.
On 7/8/24 at approximately 3:27 p.m., an observation of R131's room was conducted. Blue tape approximately one inch wide was observed along a portion of the baseboard approximately 12 inches long on the window side of the room. The electrical outlet above the area was observed to have blue tape surrounding the plastic outlet cover on each side. The un-taped portions of the baseboard on the wall located along the window side of the room were observed to be separated from the wall exposing dried adhesive on the wall beneath. At this time an interview was conducted with R131 who stated that the wall on the window side of the room had looked like that for months. R131 stated that a staff member had taped it up and said they would be back to fix it and never came back. R131 stated that they would like to have it fixed.
On 7/10/24 at 12:40 p.m., an interview was conducted with OSM (other staff member) #17, maintenance technician. OSM #17 stated that they had a program on their phone which showed them any open work orders for repairs needed in the facility. OSM #17 reviewed the program and stated that there were no open work orders for R131's room. OSM #17 observed the blue tape approximately one inch wide along the baseboard approximately 12 inches long on the window side of the room, the electrical outlet above the area with blue tape surrounding the plastic outlet cover on each side and the un-taped portions of the baseboard on the wall that were separated from the wall exposing dried adhesive on the wall beneath. He stated that it appeared that someone may have attempted to glue the baseboard back to the wall and then taped it to dry and it had not been removed. He stated that he was not sure why the electrical outlet cover was taped. OSM #17 stated that he did not think that the room was homelike with the baseboard coming off the wall and the blue tape on parts of the baseboard and electrical outlet.
On 7/11/24 at approximately 9:12 a.m., ASM (administrative staff member) #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services and ASM #4, the regional vice president of operations were made aware of the concern.
No further information was presented prior to exit.
3. For Resident #121 (R121), the facility staff failed to exercise reasonable care for the protection of the resident's property from loss.
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 5/23/24, the resident scored 15 out of 15 on the BIMS (brief interview for mental status), indicating the resident was cognitively intact for making daily decisions.
On 7/8/24 at 12:22 p.m., an interview was conducted with R121 in their room. R121 stated that they had multiple missing clothing items over the course of about a year. R121 stated that they had reported the missing items multiple times to the nursing staff, the social worker and the laundry and they all told them that they would look into it. R121 stated that they were missing all of their underwear, multiple pairs of shorts, multiple shirts, and most recently a shirt and pants set that their family member had brought in to them. R121 stated that all items were labeled with their name prior to going to the laundry. R121 stated that the laundry staff had told them that they were unable to find anything and had given them some of the lost and found clothing and someone had cut off some leggings to make shorts for them. R121 stated that they took the lost and found clothing because that was the only option they were given and was told that they needed to have pictures of the clothing for the staff to be able to locate it.
The resident property list for R121 documented two pages listing multiple clothing items including pants, shirts, sweaters and shorts dated 1/6/23.
Review of the facility grievance logs from 1/1/23 to the present failed to evidence any documented grievances for R121.
On 7/9/24 at 11:32 a.m., an interview was conducted with OSM (other staff member) #13, housekeeping assistant/laundry. OSM #13 stated that when a resident reported missing clothing they found out the residents name, room number and got a description of the clothing that was missing. She stated that they searched for the clothing in the laundry and if not found they reported to their manager. She stated that she remembered looking for missing clothing that R121 reported and remembered a CNA (certified nursing assistant) bringing in the name and color of the clothing. She stated that she thought they found something.
On 7/10/24 at 10:10 a.m., an interview was conducted with CNA #2. CNA #2 stated that if a resident reported missing clothing they went to the laundry to search for the items. She stated if they were unable to find the item they reported it to the nurse. She stated that she was not aware of R121 missing any clothing.
On 7/10/24 at 10:15 a.m., an interview was conducted with LPN (licensed practical nurse) #3. LPN #3 stated that if a resident was missing clothing they searched the room for the clothing and if not found they notified the laundry and unit manager. She stated that if the clothing was still not found the social worker became involved and normally they replaced the items. She stated that she was not aware of R121 missing any clothing but did not work with them every day. She stated that all residents had a personal belongings inventory list kept at the nurses station which they were encouraged to keep up to date to track any belongings that may go missing.
On 7/10/24 at 2:28 p.m., an interview was conducted with OSM #14, EVS (environmental services)director. OSM #14 stated that when his staff had searched for a resident's missing clothing and were not able to find anything he reported it to the administrator and they normally replaced it. He stated that currently they were not completing grievances for missing clothing but they were starting the process. He stated that they asked families to send them pictures to help them identify missing clothing if possible. He stated that they had given R121 some of the lost and found clothing that would fit them. He stated that he had quarterly sessions for the residents to come look through unlabeled/unclaimed clothing in the dining room to see if anything was theirs and had put that in place when he came about 10 months ago but had told residents that there was not much that he could do for things that happened prior to him being in the position. He stated that after the quarterly sessions with lost and found the rest of the clothing was donated because they could only hold things for so long.
On 7/10/24 at 2:42 p.m., an interview was conducted with OSM #15, the director of discharge planning. OSM #15 stated that if a resident reported missing clothing they went to the laundry to look for the items and talked with the EVS director. She stated that if the items were not found they typically would get approval from administrator to replace them. She stated that all resident belongings were supposed to be documented on the property list and they encouraged the resident and the family to keep the list up to date. She stated that on admission the nurse completed the list and it was updated as new items came in. She stated that R121 had reported missing clothing to them and she knew that the laundry had worked to find the items. She stated that the laundry had informed them that they had given R121 some donated clothes and she had not personally replaced any of the missing clothing. She stated that she was not aware that all of R121's underwear was missing and that she did the shopping for R121 and would be able to get them some if they wanted her to.
The facility policy Personal Belongings dated 1/29/24, documented in part, .1. At the time of admission, a nursing staff member will assist the patient and their family in putting away and storing their personal belongings. All clothing should be marked with the patient's name (garment is to be marked on the inside of the garment with permanent ink) .4. If a patient is missing a personal item, the center will make every attempt to locate the item. Although the center is not responsible for personal possessions or valuables of the patients, a patient or their family is encouraged to meet with the administrator or other center administrative personnel regarding missing items or other concerns involving their personal belongings .
On 7/11/24 at approximately 9:12 a.m., ASM (administrative staff member) #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services and ASM #4, the regional vice president of operations were made aware of the concern.
No further information was presented prior to exit.
4. For Resident #32 (R32), Resident #34 (R34), and Resident #104 (R104), the facility staff failed to serve lunch in a homelike manner on 7/8/24. Staff left meal trays and plate lids sitting on the tables during the meal.
On R32's most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 6/27/24, the resident scored 14 out of 15 on the BIMS (brief interview for mental status), indicating the resident was cognitively intact for making daily decisions.
On R34's most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 5/29/24, the resident scored 15 out of 15 on the BIMS (brief interview for mental status), indicating the resident was cognitively intact for making daily decisions.
On R104's most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 5/20/24, the resident scored 11 out of 15 on the BIMS (brief interview for mental status), indicating the resident was moderately cognitively impaired for making daily decisions.
On 7/8/24 at 12:46 p.m., staff were observed serving meal trays to residents in the dining room. Staff removed meal trays from carts in the dining room and placed the meal trays on tables. After placing the meal trays on the tables, staff left the plate of food, beverage, and utensils on the meal trays, removed the plate lids and left the lids on the table for the duration of the meal.
On 7/8/24 at 12:58 p.m., an interview was conducted with R32, R34, and R104. All three residents stated they did not like the meal trays and plate lids being left on the table during meals because there was not enough room on the table.
On 7/10/24 at 1:41 p.m., an interview was conducted with CNA (certified nursing assistant) #1. CNA #1 stated the staff leaves meal trays and plate lids on the tables during resident meals. CNA #1 stated this was not homelike and would not be done in a restaurant or at home. CNA #1 stated the meal trays and plate lids could be placed back on the meal carts while residents eat their meals.
On 7/11/24 at 8:52 a.m., ASM (administrative staff member) #1 (the administrator) and ASM #2 (the director of nursing) were made aware of the above concern. The facility did not have a policy regarding dining.
No further information was presented prior to exit.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5. For Resident #56 (R56), the facility staff failed to implement a comprehensive care plan regarding splints.
R56 was admitted ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5. For Resident #56 (R56), the facility staff failed to implement a comprehensive care plan regarding splints.
R56 was admitted to the facility on [DATE] with diagnosis of traumatic brain injury, persistent vegetative state, seizures, and contractures of right and left hand.
On 7/8/24 at 3:20 p.m., 7/9/24 at 9:15 a.m., and on 7/10/24 at 10:15 a.m., R56 was observed lying in bed without the splint in her right or left hand.
A review of R56's care plan revealed, Nursing/Rehab Restorative: Splint, PROM (passive range of motion) first then apply splint. See pictures for BUE splints located in room, staff inservice provided. Wear all splints/positioner for four hours each shift (8 hours daily, as tolerated). Check for skin irritation/pain. It also revealed, BUE, as ordered/tolerated. Splint Trial.
On 7/11/24 at 10:23 a.m., LPN (licensed practical nurse) #2 was interviewed. She stated that the resident is contracted and should be wearing the splints but is not. She also stated that the purpose of the care plan is to be able to know what care to provide for a specific resident.
On 7/11/24 at approximately 12:00 p.m., ASM (administrative staff member) #1 (the administrator), ASM#2 (the director of nursing), ASM #3 (regional director of clinical services) and ASM #4 (regional vice president of operations) were made aware of the above concern.
A review of the facility policy, Care Planning, revealed in part, A licensed nurse, in coordination with the interdisciplinary team, develops and implements an individualized care plan for each patient in order to provide effective, person-centered care, and the necessary health-related care and services to attain or maintain the highest practical physical, mental, and psychosocial well-being of the patient.
No further information was provided prior to exit.
Based on observation, staff interview, clinical record review and facility document review, it was determined that the facility staff failed to develop and/or implement the comprehensive care plan for five of 50 residents in the survey sample, Residents #89, #13, #106, #86 and #56.
The findings include:
1. For Resident #89 (R89), the facility staff failed to implement the comprehensive care plan to assist with personal hygiene. R89 was observed having a brown substance underneath their fingernails on 7/8/24 at 12:47 p.m., 7/9/24 at 9:05 a.m. and 7/10/24 at 9:19 a.m.
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 6/18/24, the resident scored 11 out of 15 on the BIMS (brief interview for mental status) assessment, indicating the resident was moderately impaired for making daily decisions. Section GG coded R89 requiring substantial/maximal assistance for personal hygiene and dependent on staff for bathing.
The comprehensive care plan for R89 documented in part, ADLs (activities of daily living): [Name of R89] has an ADL self-care performance deficit r/t (related to) activity intolerance, muscle weakness, AMS (altered mental status) . Created on: 06/01/2020. Under Interventions it documented in part, . Bathing/Showering: The resident is a staff assist. Date Initiated: 10/26/2021 . Personal Hygiene/Oral Care: The resident is a staff assist. Resident is edentulous. Date Initiated: 10/26/2021 .
On 7/8/24 at 12:47 p.m., an observation was made of R89 in their room. R89 was observed lying in bed. Observation of R89's fingernails revealed that they were approximately one-quarter inch long with a brown substance underneath them.
Additional observations of R89's fingernails were made on 7/9/24 at 9:05 a.m. and 7/10/24 at 9:19 a.m. Observations revealed the brown substance remaining underneath the fingernails.
Review of the clinical record failed to evidence documentation of refusal of care during the dates of observations documented above.
On 7/10/24 at 10:10 a.m., an interview was conducted with CNA (certified nursing assistant) #2. CNA #2 stated that residents fingernails were evaluated during care provided each day and were cleaned underneath if observed to be dirty. She stated that fingernails were assessed for trimming on shower days and during baths.
On 7/10/24 at 10:15 a.m., an interview was conducted with LPN (licensed practical nurse) #3. LPN #3 stated that the purpose of the care plan was for staff to be able to look at it and see what the needs of the resident were. She stated that the care plan should be implemented because that its purpose was to be useful to care for the resident. LPN #3 stated that residents fingernails were assessed on shower days or when observed when working with the resident. She stated that the residents nails were cleaned underneath during daily care and if the resident refused it would be documented. LPN #3 observed R89's fingernails and stated, I see what you mean. LPN #3 asked R89 if they would allow them to clean underneath their nails and R89 stated yes.
On 7/11/2024 at approximately 9:12 a.m., ASM (administrative staff member) #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services and ASM #4, the regional vice president of operations were made aware of the concern.
The facility policy Care Planning dated 11/1/19 documented in part, A licensed nurse, in coordination with the interdisciplinary team, develops and implements an individualized care plan for each patient in order to provide effective, person-centered care, and the necessary health-related care and services to attain or maintain the highest practical physical, mental and psychosocial well-being of the patient .
No further information was presented prior to exit.
2. For Resident #13 (R13), the facility staff failed to implement the comprehensive care plan to provide oxygen as ordered.
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 6/13/24, the resident scored 7 out of 15 on the BIMS (brief interview for mental status) assessment, indicating the resident was severely impaired for making daily decisions. Section O documented R13 receiving oxygen at the facility.
The comprehensive care plan for R13 documented in part, Respiratory: [Name of R13] is at risk for respiratory complications secondary to supplementary oxygen requirement. Created on: 01/08/2024. Revision on: 01/08/2024. Under Interventions it documented in part, .administer oxygen as ordered. Date Initiated: 01/08/2024 .
The physician orders for R13 documented in part, Oxygen Therapy - Oxygen at 2L/min (liters per minute) via NC (nasal cannula) every day and night shift. Order Date: 01/08/2024.
On 7/8/24 at 1:07 p.m., an observation was made of R13 in their room. R13 was observed in bed wearing a hospital gown and an oxygen nasal cannula. The nasal cannula was observed to be attached to a portable oxygen tank placed in a rolling carrier beside R13's bed. Observation of the portable tank revealed the tank flow dial set at zero and the tank oxygen gauge reading empty. R13 was not able to be interviewed due to their cognition level. Additional observation of R13's nasal cannula attached to the portable oxygen tank set at zero was made on 7/8/24 at approximately 1:30 p.m.
On 7/10/24 at 10:15 a.m., an interview was conducted with LPN (licensed practical nurse) #3. LPN #3 stated that the purpose of the care plan was for staff to be able to look at it and see what the needs of the resident were. She stated that the care plan should be implemented because that its purpose was to be useful to care for the resident. LPN #3 stated that oxygen concentrators were used in resident's rooms and they used the portable oxygen tanks when residents were going out for appointments or going for therapy or activities. She stated that anytime a resident was using a portable tank they should get a full tank and it was checked every two hours to ensure that it was running low or empty. She stated that she was not sure why R13 was on the portable tank in their room and that perhaps the concentrator had malfunctioned but the portable oxygen should not have been empty or set to zero.
On 7/11/2024 at approximately 9:12 a.m., ASM (administrative staff member) #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services and ASM #4, the regional vice president of operations were made aware of the concern.
No further information was presented prior to exit.3. For Resident #106 (R106), the facility staff failed to implement the resident's comprehensive care plan for physician notification of a change in condition.
R106's comprehensive care plan dated 3/27/24 documented, CARE NEEDS: (Name of R106) has the following basic care needs: HX (History) of DM (Diabetes Mellitus) Type 1 .MD/NP/RP (Medical Doctor/Nurse Practitioner/Responsible Party) will be notified of the appropriate change in condition. A review of R106's clinical record revealed a physician's order dated 4/15/24 that documented to administer Lispro insulin (used to treat diabetes) based on a sliding scale dependent on the resident's blood sugar before meals and at bedtime. The order further documented to contact the physician if R106's blood sugar was greater than 400 or less than 60.
A review of R106's June 2024 and July 2024 MARs (medication administration records) revealed the following blood sugars on the following dates:
6/2/24 11:00 a.m.- 450
6/9/24 11:00 a.m.- 441
6/10/24 7:30 a.m.- 401
6/10/24 4:00 p.m.- 432
6/11/24 4:00 p.m.- 448
6/12/24 4:00 p.m.- 410
6/17/24 9:00 p.m.- 425
6/19/24 4:00 p.m.- 448
6/23/24 9:00 p.m.- 404
6/25/24 11:00 a.m.- 449
7/3/24 9:00 p.m.- 450
7/6/24 9:00 p.m.- 419
Further review of R106's clinical record (including the June 2024 and July 2024 MARs, nurses' progress notes, and change in condition notes) failed to reveal the facility staff contacted the physician regarding any of R106's above blood sugars that were greater than 400.
On 7/10/24 at 1:12 p.m., an interview was conducted with RN (registered nurse) #3. RN #3 stated the purpose of the care plan is, so staff is able to go in and see the issues with the resident. RN #3 stated the care plan tells the story of the resident and nurses have access to review residents' care plans to ensure they are implemented. RN #3 stated that if a resident has a physician's order to contact the physician for a blood sugar greater than a specified parameter, then when the nurse takes the blood sugar and the blood sugar is over the parameter, the nurse needs to call the physician to get new orders or maintain current orders, depending on what the physician wants to do. RN #3 stated nurses should evidence the physician notification by documenting a progress note or change in condition note.
On 7/11/24 at 8:52 a.m., ASM (administrative staff member) #1 (the administrator) and ASM #2 (the director of nursing) were made aware of the above concern.
No further information was presented prior to exit.
4. For Resident #86, the facility staff failed to implement the care plan for pressure injury (1) care.
The comprehensive care plan dated, 3/1/24, documented in part, Focus: Skin Impairment: The resident has a skin impairment: R/L (right/left) groin necrotizing fasciitis post-surgical, R/L ABD (abdominal) rash, L axilla hidradenitis, L/R scrotum hidradenitis, R lateral groin post-surgical necrotizing fasciitis, L groin post-surgical necrotizing fasciitis, sacrum pressure. The Interventions documented in part, Notify MD (medical doctor) as indicated. Observe area for signs of improvement or decline. Treatment as ordered.
The wound care nurse practitioner note dated 5/20/24 documented in part, Sacrum scar tissue.
The wound care physician notes dated, 5/31/24, documented in part, Sacrum - stage 2 (2) measuring approximately 1x1x 0.1 cm (centimeters) in size.
The physician order dated 5/31/24, documented, Sacrum: Cleanse with wound cleanser, pat dry. Apply silver alginate and cover with border gauze dressing every day shift for Pressure Stage 2.
The TAR (treatment administration record) for May, June and July 2024, documented the above order. The treatment was documented as having been administered as ordered.
The Skin Observation forms dated the following documented:
5/19/24 - no documentation of a sacrum pressure injury.
5/27/24 - no documentation of a sacrum pressure injury.
6/3/24 - sacrum - pressure - no measurements or stage.
6/10/24 - sacrum - pressure - stage II - no measurements.
6/17/24 - sacrum - pressure - no measurements or stage.
6/24/24 - sacrum - pressure - no measurements or stage.
7/1/24 - sacrum - pressure - no measurements or stage.
7/8/24 - sacrum - pressure - no measurements or stage.
7/9/24 - sacrum - pressure - stage II - no measurements.
An interview was conducted on 7/10/24 at 10:15 a.m. with LPN (licensed practical nurse) #3, she stated the purpose of the care plan is for staff to be able to look at it and see what the needs of the resident are. It should be implemented because that its purpose to be useful to care for the resident.
ASM #1, the administrator, ASM #2, ASM #3, the regional director of clinical services, and ASM #4, the regional vice president of operations, were made aware of the above concern on 7/11/24 at 9:00 a.m.
No further information was provided prior to exit.
(1) A pressure injury is localized damage to the skin and underlying soft tissue usually over a bony prominence or related to a medical or other device. The injury can present as intact skin or an open ulcer and may be painful. The injury occurs as a result of intense and/or prolonged pressure or pressure in combination with shear. The tolerance of soft tissue for pressure and shear may also be affected by microclimate, nutrition, perfusion, co-morbidities and condition of the soft tissue. This information was obtained from the following website: http://www.npuap.org/resources/educational-and-clinical-resources/npuap-pressure-injury-stages/.
(2) Stage 2 Pressure Injury: Partial-thickness skin loss with exposed dermis Partial-thickness loss of skin with exposed dermis. The wound bed is viable, pink or red, moist, and may also present as an intact or ruptured serum-filled blister. This information was obtained from the following website: http://www.npuap.org/resources/educational-and-clinical-resources/npuap-pressure-injury-stages/.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. For Resident #151 (R151), the facility staff failed to provide care and services for a skin tear on the right arm.
On the fo...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. For Resident #151 (R151), the facility staff failed to provide care and services for a skin tear on the right arm.
On the following dates and times, R151 was observed lying in bed with a dried blood on her left Geri sleeve by the inside elbow crease: 7/8/24 at 3:00 p.m. and 7/9/24 at 12:33 p.m.
On 7/8/24 at p.m., R151 was interviewed. She stated that the dried blood spot on her sleeves has been there longer than a day and that it is from a skin teary. She stated that it could possibly be due to the wheelchair.
A review of R151's physician's orders dated 6/14/24 revealed, Wound Consult PRN (as needed).
A review of R151's facility document, Skin Observation Tool-V2 dated 7/8/24, revealed R151 has a skin tear on the left elbow.
A review of R151's care plan revealed, Skin: [R151] has actual skin impairment with the potential for further skin impairments .Geri-Sleeves as tolerated .Treatment as ordered.
On 7/11/24 at 10:23 a.m., LPN (licensed practical nurse) #2 was interviewed. She stated that when a resident has a skin tear, they have to assess the tear, clean it and treat it. She also stated that they would notify the nurse and the supervisor. She also stated that if it is a new skin tear that they should let the nurse practitioner know. She added that for treatment they typically use a wound cleanser or whatever is ordered for the resident.
On 7/11/24 at approximately 12:00 p.m., ASM (administrative staff member) #1 (the administrator), ASM#2 (the director of nursing), ASM #3 (regional director of clinical services) and ASM #4 (regional vice president of operations) were made aware of the above concern.
No further information was provided prior to exit.
Based on staff interview, clinical record review and facility document review, it was determined that the facility staff failed to provide care and services to promote or maintain the highest level of well being for two of 50 residents in the survey sample; Residents #269 and #151.
The findings include:
1. For Resident #269, the facility staff failed to evidence that an IV antibiotic medication that was available, was administered as ordered on six occasions, on 7/13/23 (two doses), 7/14/23 (two doses) and 7/15/23 (two doses).
Resident #269 was admitted to the facility on [DATE] and discharged on 7/26/23. The resident was coded on the admission MDS dated [DATE] coded the resident as being cognitively intact in ability to make daily life decisions, scoring a 15 out of a possible 15 on the BIMS.
A review of the physician's orders and the MAR (Medication Administration Record) for July 2023 revealed the following regarding a medication Teflaro (1):
An order dated 7/11/23 for Teflaro IV (intravenous) 400 MG (milligrams) every 8 hours. A review of the MAR revealed this was scheduled for 12:00 AM, 8:00 AM, and 4:00 PM. It was documented that on 7/12/23, this medication was not administered at 12:00 AM, was administered at 8:00 AM, and was discontinued before the 4:00 PM dose was due.
An order dated 7/12/23 for Teflaro IV 400 MG three times a day. A review of the MAR revealed this was scheduled for 11:00 AM, 1:00 PM, and 9:00 PM. It was documented that on 7/12/23, this medication was administered at 1:00 PM and 9:00 PM. Between this order and the above previous order, the resident received all three doses due on 7/12/23 (at 8:00 AM, 1:00 PM, and 9:00 PM).
Further review of the MAR revealed that on 7/13/23, this medication was not administered at the 11:00 AM dose, was administered at 1:00 PM, and was discontinued before the 9:00 PM dose.
An order dated 7/13/23 for Teflaro IV 400 MG three times a day. A review of the MAR revealed this was scheduled for 12 AM, 6 AM, and 12 PM daily; and as documented above, the resident only received one of three doses on 7/13/23. The resident did not receive a morning dose (as evidenced by a blank spot on the MAR) or evening dose (as evidenced by an X marking out spots on the MAR), for either order / schedule that covered the date of 7/13/23.
Further review revealed documentation for all doses on 7/14/23 and the first two doses on 7/15/23 as U-SA. This coding was not in the legend. On 7/10/24 at 3:00 PM, ASM #3 (Administrative Staff Member) the Regional Director of Clinical Services, stated that this code means Unwitnessed self-administration which she stated was not possible given the medication and route, and that it must have been entered into the system incorrectly. She presented a nurse's note dated 7/14/23 at 2:38 PM which would account for the third dose due that date, which documented, MAR would not allow me to sign off on 1200 (noon) Teflaro While this validated that the one dose was administered on 7/14/23, there were no notes to validate the other two doses on 7/14/23 were administered or the first two doses on 7/15/24, before this administration coding was corrected. Therefore, out of the five doses that contained this coding error, there was no evidence that four of the doses were administered.
All together, the above reflected a total of six doses of the medication that were not evidenced as being administered.
On 7/10/24 at 2:22 PM, an interview was conducted with LPN #8 (Licensed Practical Nurse). She stated that she did not recall the resident. She stated that the only reason why it would not be administered would be if the facility does not have the medication. She stated that when the medication comes it will get started on that day so that the resident does not miss a dose. She stated that if the facility does not have it they let the Nurse Practitioner know the medication is not available and she would call the pharmacy upon admission to notify them of the medication that is needed and when it is next due so that they can send it immediately.
On 7/10/24 at 3:31 PM an interview was conducted with LPN #9. She stated that when a resident is admitted , they make sure the medication list from the hospital is approved through the Nurse Practitioner and then entered into the electronic medical record system. She stated that any orders for IV medications are printed out and faxed over as a stat delivery. She stated that if residents are not getting their doses they are not getting proper treatment. She stated that missed doses can impact the effectiveness of the treatment. She stated that the rights of medication administration, the right patient, right time, right dose, right medication, and right route was not being followed if there were missed doses.
On 7/10/24 at 3:00 PM, ASM #3 (Administrative Staff Member) the Regional Director of Clinical Services, provided the pharmacy delivery manifest of Teflaro. Based on the date, times, and quantity that was delivered, this evidenced the medication was available to be administered during the times above where there was no evidence that it was administered per order.
The facility policy, General Guidelines for Medication Administration documented, At a minimum, the 5 Rights - right resident, right drug, right dose, right route, and right time - should be applied to all medication administration Medications are administered in accordance with written orders of the prescriber
On 7/1/24 at 9:00 AM, ASM #1 (Administrative Staff Member) the administrator, ASM #2, the Director of Nursing, ASM #3 the Regional Director of Clinical Services, and ASM #4 the Regional [NAME] President of Operations, were made aware of the findings. No further information was provided by the end of the survey.
(1) Teflaro is an antibiotic medication administered by injection (intravenously).
Information obtained from https://medlineplus.gov/druginfo/meds/a611014.html
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, clinical record review and facility document review, it was determined that the facility staff failed ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, clinical record review and facility document review, it was determined that the facility staff failed to prevent one of 50 residents in the survey sample, Resident #269, from a significant medication error.
The findings include:
1. For Resident #269, the facility staff failed to ensure that Resident #269 was free of significant medication error on six occasions, on 7/13/23 (two doses), 7/14/23 (two doses) and 7/15/23 (two doses).
Resident #269 was admitted to the facility on [DATE] and discharged on 7/26/23. The resident was coded on the admission MDS dated [DATE] coded the resident as being cognitively intact in ability to make daily life decisions, scoring a 15 out of a possible 15 on the BIMS.
A review of the physician's orders and the MAR (Medication Administration Record) for July 2023 revealed the following regarding a medication Teflaro (1):
On 7/10/24 at 3:00 PM, ASM #3 (Administrative Staff Member) the Regional Director of Clinical Services, provided the pharmacy delivery manifest of Teflaro. Based on the date, times, and quantity that was delivered, this evidenced the medication was available to be administered during the times below where there was no evidence that it was administered per order, resulting in a significant medication error.
An order dated 7/11/23 for Teflaro IV (intravenous) 400 MG (milligrams) every 8 hours. A review of the MAR revealed this was scheduled for 12:00 AM, 8:00 AM, and 4:00 PM. It was documented that on 7/12/23, this medication was not administered at 12:00 AM, was administered at 8:00 AM, and was discontinued before the 4:00 PM dose was due.
An order dated 7/12/23 for Teflaro IV 400 MG three times a day. A review of the MAR revealed this was scheduled for 11:00 AM, 1:00 PM, and 9:00 PM. It was documented that on 7/12/23, this medication was administered at 1:00 PM and 9:00 PM. Between this order and the above previous order, the resident received all three doses due on 7/12/23 (at 8:00 AM, 1:00 PM, and 9:00 PM).
Further review of the MAR revealed that on 7/13/23, this medication was not administered at the 11:00 AM dose, was administered at 1:00 PM, and was discontinued before the 9:00 PM dose.
An order dated 7/13/23 for Teflaro IV 400 MG three times a day. A review of the MAR revealed this was scheduled for 12 AM, 6 AM, and 12 PM daily; and as documented above, the resident only received one of three doses on 7/13/23. The resident did not receive a morning dose (as evidenced by a blank spot on the MAR) or evening dose (as evidenced by an X marking out spots on the MAR), for either order / schedule that covered the date of 7/13/23.
Further review revealed documentation for all doses on 7/14/23 and the first two doses on 7/15/23 as U-SA. This coding was not in the legend. On 7/10/24 at 3:00 PM, ASM #3 stated that this code means Unwitnessed self-administration which she stated was not possible given the medication and route, and that it must have been entered into the system incorrectly. She presented a nurse's note dated 7/14/23 at 2:38 PM which would account for the third dose due that date, which documented, MAR would not allow me to sign off on 1200 (noon) Teflaro While this validated that the one dose was administered on 7/14/23, there were no notes to validate the other two doses on 7/14/23 were administered or the first two doses on 7/15/24, before this administration coding was corrected. Therefore, out of the five doses that contained this coding error, there was no evidence that four of the doses were administered.
All together, the above reflected a total of six doses of the medication that were not evidenced as being administered.
On 7/10/24 at 2:22 PM, an interview was conducted with LPN #8 (Licensed Practical Nurse). She stated that she did not recall the resident. She stated that the only reason why it would not be administered would be if the facility does not have the medication. She stated that when the medication comes it will get started on that day so that the resident does not miss a dose. She stated that if the facility does not have it they let the Nurse Practitioner know the medication is not available and she would call the pharmacy upon admission to notify them of the medication that is needed and when it is next due so that they can send it immediately.
On 7/10/24 at 3:31 PM an interview was conducted with LPN #9. She stated that when a resident is admitted , they make sure the medication list from the hospital is approved through the Nurse Practitioner and then entered into the electronic medical record system. She stated that any orders for IV medications are printed out and faxed over as a stat delivery. She stated that if residents are not getting their doses they are not getting proper treatment. She stated that missed doses can impact the effectiveness of the treatment. She stated that the rights of medication administration, the right patient, right time, right dose, right medication, and right route was not being followed if there were missed doses.
The facility policy, General Guidelines for Medication Administration documented, At a minimum, the 5 Rights - right resident, right drug, right dose, right route, and right time - should be applied to all medication administration Medications are administered in accordance with written orders of the prescriber
On 7/1/24 at 9:00 AM, ASM #1 (Administrative Staff Member) the administrator, ASM #2, the Director of Nursing, ASM #3 the Regional Director of Clinical Services, and ASM #4 the Regional [NAME] President of Operations, were made aware of the findings. No further information was provided by the end of the survey.
(1) Teflaro is an antibiotic medication administered by injection (intravenously).
Information obtained from https://medlineplus.gov/druginfo/meds/a611014.html
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observations, staff interview, and facility document review, it was determined that the facility staff failed to maintain one of one kitchen in a safe and sanitary manner.
The findings inclu...
Read full inspector narrative →
Based on observations, staff interview, and facility document review, it was determined that the facility staff failed to maintain one of one kitchen in a safe and sanitary manner.
The findings include:
On 7/8/24 at 11:20 AM during the kitchen facility task, observations of food debris including crumbs, onion skins, lettuce and paper on floor of the kitchen. Observations of the freezer temp logs revealed there was no evidence of a second freezer temperature on 7/7/24 and no morning freezer temperature on 7/8/24.
An interview on 7/8/24 at 11:30 AM with OSM (other staff member) # 3 the food services manager.
When asked about the freezer temp logs, OSM #3 stated, they are to be done at the beginning and end of each shift. These were not done. We are short two staff today. When asked about the kitchen floor cleanliness, OSM #3 stated, it needs swept. When asked if it was cleaned the evening before, OSM #3 stated, it should have been, but I do not know.
On 7/11/24 at 9:10 AM, ASM (administrative staff member) #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services and ASM #4, the vice president of operations was made aware of the finding.
The facility's Food Storage, Cold policy revealed the following, The Dining Services Director monitors that all frozen foods will be stored at temperature maintain frozen state, target temperature is 10 degree or below. The Dining Services Director ensures that an accurate thermometer will be kept in each refrigerator and freezer. A written record of daily temperatures is recorded.
To ensure the provision of high-quality meals and to meet regulations governing temperatures with regard to safety and sanitation.
No further information was provided prior to exit.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, resident interview, clinical record review and facility document review, it was determined the facilit...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, resident interview, clinical record review and facility document review, it was determined the facility staff failed to implement infection control practices for four of four residents in medication administration and one of one infection control program, Residents #45, #25, #132, #118 and the facility.
The findings include:
1.The facility staff failed to follow infection control practices for Resident #45. The blood glucose (BG) glucometer was not cleaned prior to or after use on Resident #45's during the medication administration observation.
Resident #45 was admitted to the facility on [DATE] with diagnosis that included but were not limited to: diabetes mellitus (DM), vascular dementia and congestive heart failure.
The most recent MDS (minimum data set) assessment, a quarterly assessment, with an ARD (assessment reference date) of 6/28/24, coded the resident as scoring a 09 out of 15 on the BIMS (brief interview for mental status) score, indicating the resident was moderately cognitively impaired. A review of the MDS Section GG-functional abilities and goals coded the resident as requiring max assist for bed mobility, transfer, hygiene/bathing and supervision for eating.
A review of the care plan dated 10/6/23, which revealed, FOCUS: The resident is at risk for complications and blood glucose fluctuations related to diagnosis of diabetes mellitus. INTERVENTIONS: Administer medications as ordered. Labs as ordered.
A review of the physician orders dated 4/15/24 revealed, Accu-Chek's AC (before meals) and HS (at bedtime). Notify MD for BS (blood sugar) less then 60 and more than 400.
On 7/9/24 at 8:15 AM, during medication pass, observed RN (registered nurse) #2, take the blood glucometer (Medline Even Care G3) from the medication cart and perform a fingerstick on Resident #45. Glucometer was not cleaned prior to or after the fingerstick on Resident #45.
On 7/9/24 at 8:26 AM, RN #2 was asked the process for cleaning the glucometer. RN #2 stated, it is to be cleaned before and after each resident use. RN #2 took an alcohol wipe and cleaned the glucometer. When asked if what the manufacturers recommended cleaning product is for the glucometer, RN #2 stated, we are to use the bleach wipes. I did not have any so I used the alcohol swab.
On 7/11/24 at 9:10 AM, ASM (administrative staff member) #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services and ASM #4, the vice president of operations was made aware of the finding.
A review of the facility's Blood Glucose Monitoring policy revealed Device must be cleaned and disinfected between patients, according to manufacturer recommendations. According to the Medline Even Care G3 Blood Glucose Monitoring System User's Guide: The meter should be disinfected after use on each patient. This blood glucose monitoring system may only be used for testing multiple patients when standard precautions and the manufacturer's disinfection procedures are followed. Cleaning and Disinfecting Procedures for the Meter: The Even Care G3 Meter should be cleaned and disinfected between each patient. The following products have been approved for cleaning and disinfecting the Even Care G3 Meter. Dispatch Hospital Cleaner Disinfectant Towels with Bleach, Medline Micro-Kill Wipes with Alcohol, Chlorox HealthCare Bleach Germicidal Disinfectant Wipes and Medline Micro-Kill Bleach Germicidal Bleach Wipes.
No further information was provided prior to exit.
2.The facility staff failed to follow infection control practices for Resident #25. The blood glucose (BG) glucometer was not cleaned prior to or after use on Resident #25's during the medication administration observation.
Resident #25 was admitted to the facility on [DATE] with diagnosis that included but were not limited to: diabetes mellitus (DM), dementia and atrial fibrillation.
The most recent MDS (minimum data set) assessment, a quarterly assessment, with an ARD (assessment reference date) of 5/26/24, coded the resident as scoring a 15 out of 15 on the BIMS (brief interview for mental status) score, indicating the resident was not cognitively impaired. A review of the MDS Section GG-functional abilities and goals coded the resident as requiring supervision for bed mobility, transfer, hygiene/bathing and set-up for eating.
A review of the care plan dated 9/3/18, which revealed, FOCUS: The resident is at risk for complications related to diagnosis of diabetes mellitus. INTERVENTIONS: Accu-Chek's as ordered.
A review of the physician orders dated 2/5/24 revealed, Accu-Chek's every 12 hours.
On 7/9/24 at 8:21 AM, during medication pass, observed RN (registered nurse) #2, take the blood glucometer (Medline Even Care G3) from the medication cart and perform a fingerstick on Resident #25. Glucometer was not cleaned prior to or after the fingerstick on Resident #25.
On 7/9/24 at 8:26 AM, RN #2 was asked the process for cleaning the glucometer. RN #2 stated, it is to be cleaned before and after each resident use. RN #2 took an alcohol wipe and cleaned the glucometer. When asked if what the manufacturers recommended cleaning product is for the glucometer, RN #2 stated, we are to use the bleach wipes. I did not have any so I used the alcohol swab.
On 7/11/24 at 9:10 AM, ASM (administrative staff member) #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services and ASM #4, the vice president of operations was made aware of the finding.
A review of the facility's Blood Glucose Monitoring policy revealed Device must be cleaned and disinfected between patients, according to manufacturer recommendations.
No further information was provided prior to exit.
3. The facility staff failed to follow infection control practices for Resident #132. RN (registered nurse) #2 used her fingers for two medications in Resident #132's medication administration observation.
On 7/9/24 at 8:35 AM, during medication pass, observed RN (registered nurse) #2, drop Eliquis 5 milligram (mg) on paper on top of medication cart and use 2 fingers to pick it up and place it in a medication cup. Then RN #2 was observed opening the narcotic box and withdrew the Tramadol 50 mg card and popped 1 Tramadol directly into her hand, then place the Tramadol in the medication cup.
When asked the process for withdrawing medications and placing them in a cup, RN #2 stated, they should be popped directly into the cup and not touched. When asked about the Tramadol, RN #2 stated, it was a narcotic, what was I to do, I cannot drop it.
On 7/11/24 at 9:10 AM, ASM (administrative staff member) #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services and ASM #4, the vice president of operations was made aware of the finding.
A review of the facility's Medication Administration policy revealed Medications are administered as prescribed in accordance with good nursing principles and practices. The person administering medications adheres to good hand hygiene which includes washing hands thoroughly.
No further information was provided prior to exit.
5. The facility staff failed to evidence communication with the local health department during outbreaks of communicable diseases.
During the facility entrance conference on 7/8/24 at 11:15 a.m., a request was made for the name and contact information of the facility's local health department contact for outbreaks of communicable disease.
On 7/10/24 at 4:46 p.m., LPN (licensed practical nurse) #4, the facility infection preventionist, was interviewed. When asked the process for notifying the local health department during a communicable disease outbreak, LPN #4 stated: We haven't been notifying the local health department. She stated she has only been in this position for two weeks, and she does not know whom to contact in the local health department. She stated she had called two different places [on 7/10/24] and had still not been able to get accurate information about whom to contact in the local health department.
On 7/11/24 at 9:20 a.m., ASM (administrative staff member) #1, the administrator, ASM #2, the director of nursing, ASM #3, the regional director of clinical services, and ASM #4, the regional vice president of operations, were informed of these concerns.
A review of the facility policy, Infection Outbreak Standards of Practice, revealed, in part: Outbreaks are to be reported to the Center's local health department.
No further information was provided prior to exit.
4. For Resident #118 (R118), the facility staff failed to prepare and administer medications in a sanitary manner.
A review of R118's clinical record revealed the following physician's orders:
7/1/24- Klor-Con (potassium chloride) (1) 20 milliequivalents- two tablets by mouth in the morning.
7/8/24- Gabapentin (2) 200 milligrams- one capsule by mouth two times a day.
On 7/9/24 at 8:28 a.m., LPN (licensed practical nurse) #3 was observed preparing R118's medications in the hall. While preparing medications, LPN #3 dropped a tablet of Klor-Con and a capsule of Gabapentin on top of the medication cart then picked up the pills (with a gloved hand) and placed the pills in a medication cup. After LPN #3 finished preparing medications, she administered the medications, including the Klor-Con tablet and Gabapentin capsule to R118.
On 7/9/24 at 5:37 p.m., an interview was conducted with LPN #3. LPN #3 stated she had cleaned the top of the medication cart but administered medications to two other residents in between cleaning the top of the medication cart and preparing R118's medications. LPN #3 stated she could not be sure that the top of the medication cart was not contaminated when she dropped the pills. LPN #3 stated she should have disposed of the Klor-Con tablet and Gabapentin capsule in the sharps container because the pills were cross contaminated if the top of the medication cart was dirty.
On 7/11/24 at 8:52 a.m., ASM (administrative staff member) #1 (the administrator) and ASM #2 (the director of nursing) were made aware of the above concern.
References:
(1) Potassium is essential for the proper functioning of the heart, kidneys, muscles, nerves, and digestive system. Usually, the food you eat supplies all of the potassium you need. However, certain diseases (e.g., kidney disease and gastrointestinal disease with vomiting and diarrhea) and drugs, especially diuretics ('water pills'), remove potassium from the body. Potassium supplements are taken to replace potassium losses and prevent potassium deficiency. This information was obtained from the website: https://medlineplus.gov/druginfo/meds/a601099.html.
(2) Gabapentin capsules, tablets, and oral solution are used along with other medications to help control certain types of seizures in people who have epilepsy. Gabapentin capsules, tablets, and oral solution are also used to relieve the pain of postherpetic neuralgia (PHN; the burning, stabbing pain or aches that may last for months or years after an attack of shingles). This information was obtained from the website: https://medlineplus.gov/druginfo/meds/a694007.html.