AVAMERE AT PACIFIC RIDGE




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Avamere at Pacific Ridge has received a Trust Grade of F, indicating significant concerns about the care provided. With a state rank of #166 out of 190 facilities in Washington, they fall in the bottom half, and #18 out of 21 in Pierce County suggests limited local options that are better. The facility is worsening, with reported issues increasing from 15 in 2024 to 29 in 2025. Although staffing is rated average with a turnover rate of 54%, the RN coverage is concerning, as it is lower than 98% of state facilities, which raises alarms about the quality of care. Notably, there have been serious incidents, including a resident who suffered aspiration pneumonia due to improper tube feeding and another who fell and fractured a shoulder because the required two-person assistance was not provided. While there are some average staffing metrics, the overall quality and safety concerns present significant risks for residents.
- Trust Score
- F
- In Washington
- #166/190
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 54% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $57,783 in fines. Lower than most Washington facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 31 minutes of Registered Nurse (RN) attention daily — about average for Washington. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 76 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Washington average (3.2)
Significant quality concerns identified by CMS
Near Washington avg (46%)
Higher turnover may affect care consistency
Above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 76 deficiencies on record
May 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0627
(Tag F0627)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to develop a discharge plan that addressed all of the needs for a resi...
Read full inspector narrative →
Mar 2025
27 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to have signed consent prior to administering mood altering medicati...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to obtain an advanced directive (AD, a legal document that establish...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interview, and record review, the facility failed to conduct an assessment and signed consent for the us...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
MDS Data Transmission
(Tag F0640)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to transmit resident minimum data set (MDS, an assessment tool) to t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to ensure the minimum data set (MDS, a required assessment tool) acc...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interview, and record review, the facility failed to develop comprehensive care plans for 2 of 19 sample...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to ensure a resident's care plan was revised and accurately reflecte...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 59
Resident 59 admitted to the facility on [DATE] with diagnoses that included dementia (a group of symptoms affecting ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 425
Resident 425 admitted to the facility on [DATE] with diagnoses that included cerebral infarction (stroke), hemipleg...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 425
Resident 425 admitted to the facility on [DATE] with diagnoses that included cerebral infarction (stroke), hemipleg...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interview, and record review, the facility failed to provide services to increase range of motion or to ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interview, and record review, the facility failed to ensure a bathroom emergency call light (a system us...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to monitor and consistently document weights per provider orders for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interview, and record review, the facility failed to provide prompt dental services for 2 of 3 sampled r...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interview, and record review, the facility failed to make needed repairs to maintain a homelike environm...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to provide a written bed-hold notice, at the time of transfer to the...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 421
Resident 421 admitted to the facility on [DATE] with diagnoses that included adult failure to thrive (a decline in ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 4
Review of the EHR showed Resident 4 admitted to the facility on [DATE] with diagnoses to include dementia (a loss of ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 19
Review of the EHR showed Resident 19 admitted to the facility on [DATE] with diagnoses that included hemiplegia and ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interview, and record review, the facility failed to ensure proper storage and labeling of medications i...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interview, and record review, the facility failed to ensure proper fit and use of personal protective eq...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to offer and provide influenza and/or pneumococcal vaccines for 3 of...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to offer and provide Covid-19 vaccines for 2 of 5 sampled residents ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected multiple residents
.
Based on interview and record review, the facility failed to ensure oversight of certified nurse assistants (CNA) received 12 hours of in-service training per year as required and were provided mand...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to ensure Pre-admission Screening and Resident Review (PASARR, a men...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interview, and record review, the facility failed to provide food in an individualized manner when the t...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
.
Based on observation and interview, the facility failed to maintain sanitary food storage and preparation areas when reviewed for kitchen. This failure placed residents at risk of foodborne illness,...
Read full inspector narrative →
Jan 2025
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Tube Feeding
(Tag F0693)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure enteral nutrition (the delivery of nutrients th...
Read full inspector narrative →
Jul 2024
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on observation, interview and record review, the facility failed to provide the required care planned supervision to prevent accidents/falls for 3 of 5 residents (Resident 1, 2 and 3) reviewed f...
Read full inspector narrative →
Apr 2024
14 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interview, and record review, the facility failed to have system and timely resolution of a grievance fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Review of the Minimum Data Set (MDS) 3.0 Resident Assessment Instrument (RAI) Manual showed OPEN LESION(S) OTHER THAN ULCERS, RA...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interview, and record review, the facility failed to ensure nursing staff were following provider's orde...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 40
Review on 04/23/2024 of Resident 40's EHR showed the resident admitted on [DATE] with diagnoses of dysthymic disorde...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interview, and record review, the facility failed to have a clear system in place to monitor and accurat...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to ensure freedom from unnecessary pain medication for 1 of 5 sample...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation and interview, the facility failed to maintain a homelike environment in resident areas for 3 of 4 halls ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to ensure enteral nutrition (the delivery of nutrients through a fee...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interview, and record review, the facility failed to provide pharmaceutical services (including procedur...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to consistently monitor residents' behaviors and/or medication side ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
.
Based on observation, interview, and record review, the facility failed to consistently maintain the medication refrigerator temperature logs in 2 of 2 medication rooms (medication rooms 100/200 hal...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation and interview, the facility failed to maintain a call light system that allowed residents to call for hel...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0625
(Tag F0625)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to provide a bed hold notice in writing at the time of transfer to t...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Transfer Notice
(Tag F0623)
Minor procedural issue · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to provide written notification of the reason for transfer/discharge...
Read full inspector narrative →
Sept 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0691
(Tag F0691)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure care and treatment of an ileostomy (an opening in the body f...
Read full inspector narrative →
Jun 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to implement an effective discharge plan for one of three residents (Resident 1) reviewed for discharge plans. Failure to ensure necessary hom...
Read full inspector narrative →
Mar 2023
29 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide reasonable accommodation of resident needs and...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide information and assistance to assist a resident in establishing an advanced directive (AD, a legal document in which a person speci...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to report witnessed and documented incidents of intimidation and verbal abuse by Resident 51 against multiple unidentified residents to the St...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to complete a significant change in condition assessment (SCCA) for 1 ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure Pre-admission Screening and Resident Review (PASRR) assessme...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 24
Review of the electronic health record (EHR) showed Resident 24 originally admitted on [DATE], was sent out to the h...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 4
Observation on 03/13/2023 at 9:34 AM showed Resident 4 in bed awake with the room lights off.
Observation on 03/13/20...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 324
Review of Resident 324's EHR showed the resident admitted on [DATE] with diagnoses to include right diabetic foot i...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to identify medications at bedside as an accident hazard and ensure the environment was free from accident hazards for 1 of 2 residents (Residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure residents received appropriate assistance with...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility did not follow recommendations from the registered dietician to maintain nutr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 121
Observation and interview on 03/13/2023 at 12:02 PM showed Resident 121 resting in bed with oxygen on at 2L/min thr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 121
Review on 03/14/2023 at 1:27 PM of Resident 121's Electronic Medical Record (EMR) showed the resident had a weight ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to complete required annual performance reviews for 1 of 1 (Staff X) Certified Nursing Assistants (CNA) reviewed, that had been employed by th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews and record review, the facility failed to provide routine dental care for 1 of 2 residents (Re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure nurse aides (CNAs) received 12 hours of in-service training per year as required and were provided mandatory dementia management tra...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to ensure the facility was maintained in a homelike and safe manner for 4 of 4 halls (Halls 100, 200, 300 and 400) when reviewed for Environment...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to properly notify the Office of the State Long-Term Care Ombudsman of...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide a bed hold notice in writing at the time of transfer to the...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 52
Review of Resident 52's EMR on 03/17/2023 showed the resident was admitted to the facility on [DATE] with diagnoses ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 69
Review of Resident 69's EMR on 03/16/2023 showed that Resident 69 was admitted to the facility on [DATE] with diagno...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 17
Review of the annual MDS on 03/17/2023 showed that Resident 17 admitted to the facility on [DATE] with multiple diag...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 13
Observations on 03/13/2023 and 03/14/2023 showed Resident 13 with long nails.
During an interview on 03/14/2023 at 1...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to have sufficient staff to provide and supervise care as...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 327
Review of the EHR showed Resident 327 admitted on [DATE] with an order for ceftriaxone (an antibiotic) intravenousl...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
Food Quality
Resident 50
During an interview on 03/13/2023 at 11:11 AM, Resident 50 stated that they had only eaten one meal at the facility because it was inedible. Resident 50 further stated that th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to maintain an infection prevention and control program to help prevent the transmission of communicable diseases and infections by completing...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to offer, educate, and obtain consent for influenza and pneumococcal vaccines for 5 of 5 residents (Residents 17, 39, 46, 47, and 48) reviewed...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure 5 of 5 residents (Residents 17, 39, 46, 47, and 48) reviewed for Covid-19 (a highly infectious respiratory illness caused by a virus...
Read full inspector narrative →
Mar 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure care was consistently provided as ordered to resident's feed...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 2 harm violation(s), $57,783 in fines. Review inspection reports carefully.
- • 76 deficiencies on record, including 2 serious (caused harm) violations. Ask about corrective actions taken.
- • $57,783 in fines. Extremely high, among the most fined facilities in Washington. Major compliance failures.
- • Grade F (20/100). Below average facility with significant concerns.
About This Facility
What is Avamere At Pacific Ridge's CMS Rating?
CMS assigns AVAMERE AT PACIFIC RIDGE an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Washington, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Avamere At Pacific Ridge Staffed?
CMS rates AVAMERE AT PACIFIC RIDGE's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 54%, compared to the Washington average of 46%. RN turnover specifically is 82%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Avamere At Pacific Ridge?
State health inspectors documented 76 deficiencies at AVAMERE AT PACIFIC RIDGE during 2023 to 2025. These included: 2 that caused actual resident harm, 72 with potential for harm, and 2 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Avamere At Pacific Ridge?
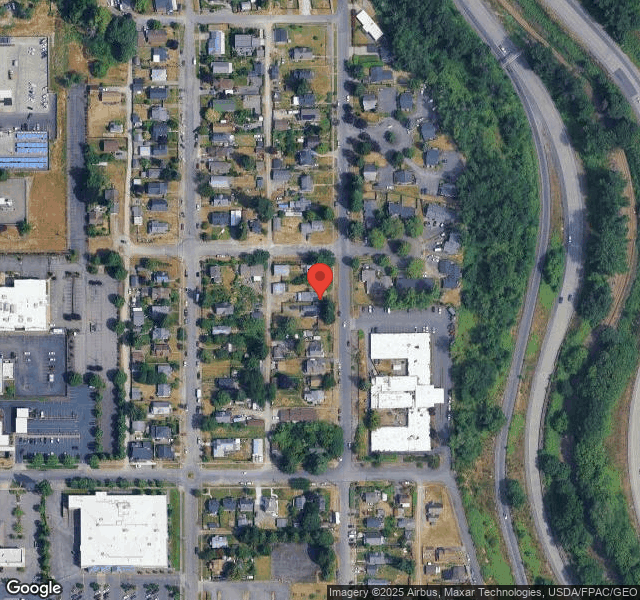
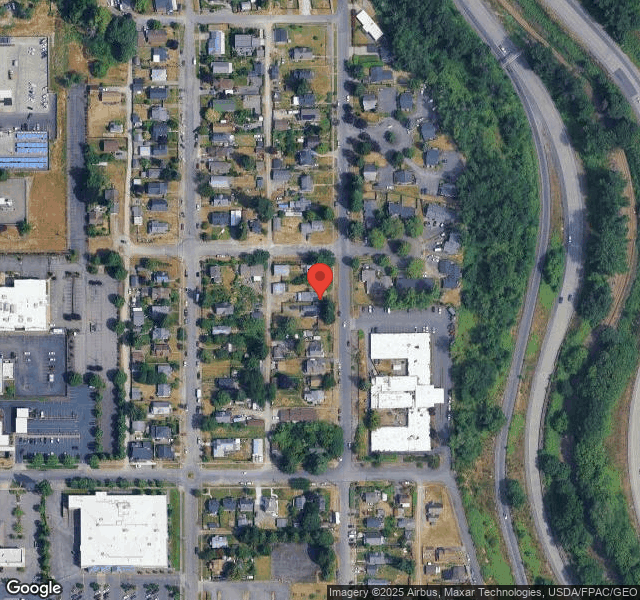
AVAMERE AT PACIFIC RIDGE is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by AVAMERE, a chain that manages multiple nursing homes. With 102 certified beds and approximately 69 residents (about 68% occupancy), it is a mid-sized facility located in TACOMA, Washington.
How Does Avamere At Pacific Ridge Compare to Other Washington Nursing Homes?
Compared to the 100 nursing homes in Washington, AVAMERE AT PACIFIC RIDGE's overall rating (1 stars) is below the state average of 3.2, staff turnover (54%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Avamere At Pacific Ridge?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Avamere At Pacific Ridge Safe?
Based on CMS inspection data, AVAMERE AT PACIFIC RIDGE has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Washington. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Avamere At Pacific Ridge Stick Around?
AVAMERE AT PACIFIC RIDGE has a staff turnover rate of 54%, which is 8 percentage points above the Washington average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Avamere At Pacific Ridge Ever Fined?
AVAMERE AT PACIFIC RIDGE has been fined $57,783 across 3 penalty actions. This is above the Washington average of $33,657. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Avamere At Pacific Ridge on Any Federal Watch List?
AVAMERE AT PACIFIC RIDGE is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.