BIRCH CREEK POST ACUTE & REHABILITATION




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Birch Creek Post Acute & Rehabilitation has a Trust Grade of C, which means it is average and sits in the middle of the pack among nursing homes. It ranks #94 out of 190 facilities in Washington, placing it in the top half, but is #12 out of 21 in Pierce County, indicating there are better local options. Unfortunately, the facility is worsening, with issues increasing from 22 in 2024 to 28 in 2025. Staffing is average, with a rating of 3 out of 5 stars and a turnover rate of 49%, which is close to the state average. While the facility has not incurred any fines, it has less registered nurse coverage than 79% of other facilities in Washington, meaning there may be less oversight for resident care. There have been some concerning incidents noted in inspections, including a serious case where a resident's significant health changes were not addressed in a timely manner, leading to hospitalization. Additionally, the facility has struggled with food safety practices, as observed food storage violations could lead to foodborne illness. Lastly, there are deficiencies in infection control measures, which pose risks to residents and staff alike. Overall, while there are some strengths, families should weigh these issues carefully when considering this facility for their loved ones.
- Trust Score
- C
- In Washington
- #94/190
- Safety Record
- Moderate
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 49% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Washington facilities.
- Skilled Nurses ○ Average
- Each resident gets 32 minutes of Registered Nurse (RN) attention daily — about average for Washington. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 66 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Near Washington average (3.2)
Meets federal standards, typical of most facilities
Near Washington avg (46%)
Higher turnover may affect care consistency
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 66 deficiencies on record
Aug 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide adequate monitoring and supervision and implem...
Read full inspector narrative →
Jul 2025
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to have a system in place that ensured fluid intake/outp...
Read full inspector narrative →
Jun 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .Based on interview and record review, the facility failed to thoroughly investigate an allegation of potential abuse and implem...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .Based on interview and record review, the facility failed to identify, and timely report an allegation of potential abuse for 1...
Read full inspector narrative →
Mar 2025
24 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to have psychotropic medication (medications that affect a person's ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to honor resident shower preferences for 1 of 3 sampled residents (R...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation and interview, the facility failed to provide a homelike environment in resident rooms for 2 of 4 hallway...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
.
Based on observation, interview, and record review, the facility failed to complete criminal background check prior to hire for 1 of 5 staff (Staff F) when reviewed for abuse and neglect prevention....
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to identify and report an allegation of abuse for 1 of 2 sampled res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interview, and record review, the facility failed to follow provider's order for 1 of 5 sampled resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 30
Review of the EHR showed Resident 30 admitted to the facility on [DATE] with diagnoses including cancer of the colon...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 64
Review of the EHR showed Resident 64 admitted to the facility on [DATE] with diagnoses that included disorder of mus...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 88
Review of the EHR showed Resident 88 admitted to the facility on [DATE] with diagnoses of cognitive communication de...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 82
Review of the EHR showed Resident 82 admitted to the facility on [DATE] with diagnoses of chronic obstructive pulmon...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to ensure enteral nutrition (the delivery of nutrients through a fee...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 82
Review of the EHR showed Resident 82 admitted to the facility on [DATE] with diagnoses of COPD and CHF. The resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to provide non-pharmacological interventions (health interventions/a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interview and record review, the facility failed to monitor behaviors related to psychotropic medication...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to obtain advanced directives (AD) and/or perform periodic reviews t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 22
Review of the EHR showed Resident 22 initially admitted to the facility on [DATE] with diagnoses to include diabete...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interview, and record review, the facility failed to ensure baseline care plans were developed and imple...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 77
Review of the EHR showed Resident 77 was admitted to the facility on [DATE] with diagnoses to include dementia (impa...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 77
Review of the EHR showed Resident 77 was admitted to the facility on [DATE] with diagnoses to include dementia with ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interview, and record review, the facility failed to ensure a safe environment was maintained related to...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to implement an effective antibiotic stewardship program to promote ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to ensure and document that each resident was informed about the ben...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to ensure and document that each resident was informed about the ben...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
.
Based on observation and interview, the facility failed to store and prepare food in manner which prevents food illness when reviewed for kitchen. This failure placed residents at risk for foodborne...
Read full inspector narrative →
Nov 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to ensure a skin condition was accurately assessed, treated and moni...
Read full inspector narrative →
Oct 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Staffing Data
(Tag F0851)
Could have caused harm · This affected 1 resident
.
Based on interview and record review, the facility failed to ensure that direct care staffing information was accurate and submitted timely to the Centers for Medicare and Medicaid Services (CMS), f...
Read full inspector narrative →
Jul 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interview, and record review the facility failed to provide necessary care and services to prevent the o...
Read full inspector narrative →
Jul 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to identify, report to administrator and investigate an allegation o...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interviews and record review, facility failed to provide care and treatment according to professional st...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observations, interviews and record reviews, the facility failed to ensure physician orders were clarified and treatm...
Read full inspector narrative →
May 2024
14 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected 1 resident
.
Based on interview and record review, the facility failed to resolve grievances brought forward by the resident council (RC) for 2 of 3 months (March and April 2024) when reviewed for resident counc...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview, observation, and record review, the facility failed to report to the administrator and investigate an alle...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interview, and record review, the facility failed to ensure services provided met professional standards...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
.
Based on observation, interview, and record review, the facility failed to ensure hearing aids were implemented and/or provided the necessary auditory (hearing) services in a timely manner for 1 of ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 22
Resident 22 admitted to the facility on [DATE] with diagnosis of chronic obstructive pulmonary disease (COPD, a long...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 22
Resident 22 admitted to the facility on [DATE] and was placed on hospice on 05/10/2024 with diagnosis of COPD.
Revie...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 11
Resident 11 was admitted to the facility on [DATE] with multiple diagnoses to include heart failure and depression. ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 22
Review of Resident 22's EHR showed the resident admitted on [DATE] and was placed on hospice on 05/10/2024 with a di...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0790
(Tag F0790)
Could have caused harm · This affected multiple residents
.
Based on observation, interview, and record review, the facility failed to provide dental services for 2 of 3 sampled residents (Resident 33 and 204) reviewed for dental services. This failure place...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interview, and record review, the facility failed to follow therapeutic diets for 3 of 5 sampled residen...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
.
Based on observation, interview, and record review the facility failed to ensure an effective infection prevention and control program was in place to prevent the transmission of communicable diseas...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Transfer Notice
(Tag F0623)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to provide written notification of the reason for transfer/discharge...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0625
(Tag F0625)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to provide a bed hold notice in writing at the time of transfer to t...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Pharmacy Services
(Tag F0755)
Minor procedural issue · This affected most or all residents
.
Based on observation, interview, and record review, the facility failed to consistently reconcile controlled medications in 3 of 3 medication carts (Medication Carts 400, 100, and 300) reviewed for ...
Read full inspector narrative →
Mar 2024
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on interview and record review, the facility failed to take timely action for 1 of 3 who experienced a significant chang...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to complete a thorough investigation on an unwitnessed fall for 1 of 3...
Read full inspector narrative →
Apr 2023
15 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to provide care in a manner that promoted resident dignity and respect for 1 of 1 resident (Resident 65) reviewed for dignity. Wh...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to have a system in place that ensured grievances were initiated, logged, addressed, and timely resolved in response to residents' verbal conve...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0638
(Tag F0638)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to ensure a Quarterly Minimum Data Set (MDS, an assessment tool) was completed within 14 days of the Assessment Reference Date (ARD) for 1 of 1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure assessments accurately reflected residents' health status for 3 of 22 sample residents (Residents 24, 37, and 42) reviewed. The faci...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to develop a comprehensive plan of care for 3 of 23 resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure that the environment was free from accident hazards for 1 of 4 residents (Resident 51) reviewed for accident hazards. T...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to periodically provide information and assistance in formulating an a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 110
Review of Resident 110's EHR on 04/25/2023 showed the resident discharged to the hospital on [DATE]. Further review...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 110
Review of progress notes in Resident 110's electronic health record (EHR) showed the resident was discharged to the...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to review and revised the plan of care after each assessment for 2 of ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure residents were provided care in accordance with...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0882
(Tag F0882)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure that the infection prevention and control program (IPCP) was overseen by a qualified individual with the time necessary to properly ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to offer and provide education on the risks and benefits of the pneumo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure residents had documented evidence in the medical record that...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to maintain an infection prevention and control program to help preven...
Read full inspector narrative →
Feb 2023
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow their process of completing personal inventory records, to s...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most Washington facilities.
- • 66 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • Grade C (55/100). Below average facility with significant concerns.
About This Facility
What is Birch Creek Post Acute & Rehabilitation's CMS Rating?
CMS assigns BIRCH CREEK POST ACUTE & REHABILITATION an overall rating of 3 out of 5 stars, which is considered average nationally. Within Washington, this rating places the facility higher than 0% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Birch Creek Post Acute & Rehabilitation Staffed?
CMS rates BIRCH CREEK POST ACUTE & REHABILITATION's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 49%, compared to the Washington average of 46%.
What Have Inspectors Found at Birch Creek Post Acute & Rehabilitation?
State health inspectors documented 66 deficiencies at BIRCH CREEK POST ACUTE & REHABILITATION during 2023 to 2025. These included: 1 that caused actual resident harm, 62 with potential for harm, and 3 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Birch Creek Post Acute & Rehabilitation?
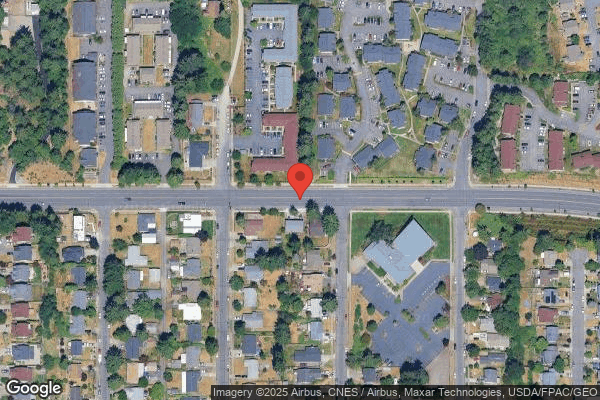
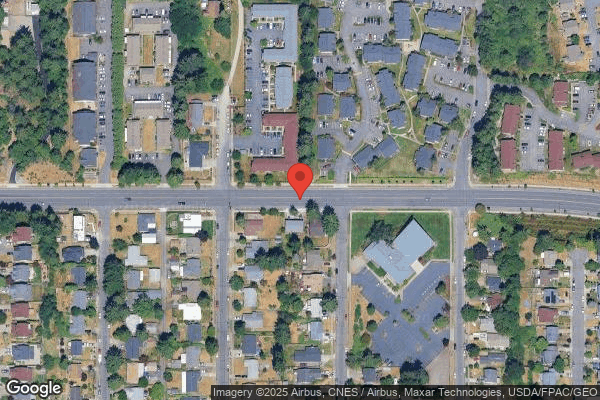
BIRCH CREEK POST ACUTE & REHABILITATION is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by HILL VALLEY HEALTHCARE, a chain that manages multiple nursing homes. With 124 certified beds and approximately 117 residents (about 94% occupancy), it is a mid-sized facility located in TACOMA, Washington.
How Does Birch Creek Post Acute & Rehabilitation Compare to Other Washington Nursing Homes?
Compared to the 100 nursing homes in Washington, BIRCH CREEK POST ACUTE & REHABILITATION's overall rating (3 stars) is below the state average of 3.2, staff turnover (49%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Birch Creek Post Acute & Rehabilitation?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Birch Creek Post Acute & Rehabilitation Safe?
Based on CMS inspection data, BIRCH CREEK POST ACUTE & REHABILITATION has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #100 of 100 nursing homes in Washington. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Birch Creek Post Acute & Rehabilitation Stick Around?
BIRCH CREEK POST ACUTE & REHABILITATION has a staff turnover rate of 49%, which is about average for Washington nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Birch Creek Post Acute & Rehabilitation Ever Fined?
BIRCH CREEK POST ACUTE & REHABILITATION has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Birch Creek Post Acute & Rehabilitation on Any Federal Watch List?
BIRCH CREEK POST ACUTE & REHABILITATION is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.