BLUESTONE HEALTH AND REHABILITATION




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Bluestone Health and Rehabilitation has a Trust Grade of F, indicating significant concerns about the care provided, putting it in the poor category. It ranks #64 out of 122 facilities in West Virginia, placing it in the bottom half, which raises red flags for families considering options. The facility's performance is worsening, with issues increasing from 3 in 2024 to 28 in 2025. Staffing is a slight strength, with a turnover rate of 31%, which is better than the state average, but the overall staffing rating is only 2 out of 5 stars. However, the facility has concerning fines of $75,089, which is higher than 94% of West Virginia facilities, and there is less RN coverage than 83% of state facilities, meaning residents may not receive adequate nursing oversight. Specific incidents include a resident developing avoidable pressure ulcers without treatment and another resident experiencing emotional distress during transfers due to fear of a mechanical lift, highlighting both serious care deficiencies and the need for improvement at this facility.
- Trust Score
- F
- In West Virginia
- #64/122
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ○ Average
- 31% turnover. Near West Virginia's 48% average. Typical for the industry.
- Penalties ⚠ Watch
- $75,089 in fines. Higher than 85% of West Virginia facilities, suggesting repeated compliance issues.
- Skilled Nurses ⚠ Watch
- Each resident gets only 24 minutes of Registered Nurse (RN) attention daily — below average for West Virginia. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 62 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (31%)
17 points below West Virginia average of 48%
Facility shows strength in fire safety.
The Bad
Below West Virginia average (2.7)
Below average - review inspection findings carefully
15pts below West Virginia avg (46%)
Typical for the industry
Well above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 62 deficiencies on record
Feb 2025
4 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, resident representative interview, and staff interview the facility failed to ensure a resident who ente...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0559
(Tag F0559)
Could have caused harm · This affected 1 resident
Based on record review, family interview and staff interview the facility failed to notify the residents responsible party of a room change prior to moving the resident. This was a random opportunity ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview the facility failed to ensure all allegations of abuse and/or neglect was thoroughly ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Transfer
(Tag F0626)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on resident representative interview, staff interview, hospital staff interview, long term care ombudsman interview and re...
Read full inspector narrative →
Jan 2025
24 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
Based on record review, staff interview, and resident interview, the facility failed to provide services that are necessary to avoid emotional distress by transferring Resident #29 from the bed to a w...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
Based on resident interview, record review, and staff interview, the facility failed to allow residents to make choices important to them. This deficient practice had the potential to affect one (1) o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview, the facility failed to ensure a complete and accurate bed hold notice was given to t...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview, the facility failed to ensure Resident #60's and Resident #59's Minimum Data Set (MD...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to identify medical diagnoses of Major Depressive disorder on the Preadmission Screening and Resident Review (PASARR). This was found tr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to implement the care plan for Resident #19, by failing to identify triggers for behaviors. This was true for one (1) of twenty-one (21)...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on record review, observation, resident interview, and staff interview, the facility failed to provide Activities of Daily Living (ADL) care to dependent residents. This failed practice was foun...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview, the facility failed to prevent, identify, assess, and treat pressure ulcers in accor...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
Based on record review and staff interview the facility failed to ensure a resident who is fed by enteral means receives the appropriate treatment and services to prevent complications of enteral feed...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0741
(Tag F0741)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to implement non-pharmacological interventions for behaviors exhibited by Resident #19. This was true for one (1) of one (1) residents r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to monitor Resident #53 for psychotropic medication side effects in November of 2024, during which time, the resident had an unwitnessed...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
Based on record review, observation, and resident and staff interview, the facility failed to accommodate Resident #36's food preferences by serving her eggs. This was a random opportunity for discove...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to ensure complete and accurate medical records for two (4) of 21 residents in the long-term care survey sample. Resident #49 had an inc...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on resident interview, medical record review, staff interview and Resident Council Meeting discussion, the facility failed to ensure the resident shower room was at a comfortable temperature for...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
Based on record review and interviews, the facility failed to revise care plan for Resident #40 for one (1) on one (1) activities and Resident #19 and Resident #29 for behaviors. This failed practice ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected multiple residents
Based on record review and interviews, the facility failed to ensure residents were provided activities of interests that he/she was care planned for. This was found true for one (1) of six (6) reside...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
Based on record review and staff interview, the facility failed to ensure residents received treatment and care in accordance with professional standards of practice. This deficient practice had the p...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
Based on observation and staff interview, the facility failed to ensure the resident environment over which it had control was as free from accident hazards as possible. A storage room containing haza...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
Based on record review, staff interview and policy review, the facility failed to ensure a licensed pharmacist completed a monthly drug regimen review, reported any irregularities to the attending phy...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on resident interview, record review and staff interview, the facility failed to ensure food was served at a palatable tem...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and and staff interview, the facility failed to ensure food was stored and an served in a safe and sanitary...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation and staff interview, the facility failed to follow proper infection control practices, by dropping cartons of milk on the floor and placing them back in the cart with clean carton...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview, the facility failed to administer pneumococcal vaccines in accordance with Centers f...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected most or all residents
Based on record review and staff interview, the facility failed to complete an accurate facility assessment related to the overall acuity of care needed for its population. This failed practice was a ...
Read full inspector narrative →
Mar 2024
1 deficiency
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observations and staff interview, the facility failed to establish and maintain an infection prevention and control program designed to provide a safe, sanitary, and comfortable environment a...
Read full inspector narrative →
Jan 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation and staff interview, the facility failed to promote dignity during dining. Residents were not served lunch trays at the same time as roommates for dining within the residents' roo...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected 1 resident
Based on observation and staff interview the facility failed to serve food and drink that was palatable and at a safe and appetizing temperature for Resident # 54. This was a random opportunity for di...
Read full inspector narrative →
Aug 2023
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident interview, and staff interview, the facility failed to ensure residents had access to water that ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview, the facility failed to ensure residents were offered the pneumococcal immunization r...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
Based on observation and staff interview the facility failed to provide Residents on the second floor with a dignified dining experience. Residents were not served meals in the traditional dinnerware....
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident interview and staff interview, the facility failed to provide a clean and sanitary environment. T...
Read full inspector narrative →
Apr 2023
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
b) Resident room [ROOM NUMBER]
On 04/24/23 11:45 AM, the window blind in room [ROOM NUMBER] was found to be tied up with a bl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
.
b) Resident #207
On 04/24/23 at 1:10 PM, during the initial interview phase of the Long Term Care Survey Process, Resident #207 had an isolation caddy and door bag for personal protective equipment ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on record review, staff interview and resident interview, the facility failed to hold a care plan meeting and involve R ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
.
Based on record review, staff interview and resident interview, the facility failed to provide appropriate care for elevated blood glucose levels for one (1) of one (1) Resident reviewed for unneces...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation and staff interview the facility failed to ensure residents receive care, consistent with professional st...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
.
Based on observation, record review and staff interview the facility failed to ensure the environment is free from accident hazards. This was true for one (1) of one (1) resident reviewed for the ca...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
.
Based on observation, medical record review, and staff interview the facility failed to follow physicians' orders for ensuring the Foley Catheter collection bag was covered at all times. This was tr...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
.
Based on record review and staff interviews the facility failed to offer pneumococcal
immunizations to all residents. This was true for two (2) out of five (5) reviewed for immunizations. Resident I...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
.
b) Resident #207
On 04/24/23 at 1:10 PM, during the initial interview phase of the Long Term Care Survey Process, Resident #207 had an isolation caddy and door bag for personal protective equipment ...
Read full inspector narrative →
Oct 2022
18 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on resident interview, medical record review and staff interview the facility failed to provide the Resident the right t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on medical record review and staff interview, the facility failed to report residents who experienced serious bodily har...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
MDS Data Transmission
(Tag F0640)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on medical record review and staff interview, the facility failed to complete a discharge tracking form for Resident #3,...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
.
Based on record review and staff interview, the facility failed to ensure a complete and accurate Minimum Data Set (MDS) assessment for two (2) of 18 residents reviewed in the long-term care survey ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
.
Based on observation, record review, and staff interview, the facility failed to ensure the comprehensive care plan was updated when a change occurred for one (1) of 18 residents reviewed in the lon...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
.
Based on record review and staff interview, the facility failed to ensure monitoring of areas relating to nutritional status for one (1) of three (3) residents reviewed for the care area of nutritio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
.
Based on medical record review and staff interview, the facility's consultant pharmacist failed to identify and report to the physician when the physician ordered parameters for medication was not f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
.
Based on observation, record review and staff interview, the facility failed to ensure expired facility stock medications were removed from the medication room. This was a random opportunity for dis...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
.
Based on observation and staff interview, the facility failed to maintain the kitchen in a safe and sanitary manner in accordance with professional standards of practice. During the kitchen tour it ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on record review and staff interview, the facility failed to maintain an accurate and complete record for Resident #10. ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0849
(Tag F0849)
Could have caused harm · This affected 1 resident
.
Based on medical record review and staff interview, the facility failed to collaborate with hospice services to develop a coordinated care plan for one (1) of one (1) residents reviewed for the care...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on medical record review, observations and staff interview, the facility failed to complete a comprehensive care plan fo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY**
Based on medical record review, observations and staff interviews the facility failed to clarify and/or follow physician orders...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
.
Based on observation, staff interview and policy and procedure review the facility failed to maintain an environment free of accident hazards. These were random oppurtunities for discovery and had t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
.
Based on record review and staff interview, the facility failed to ensure the controlled substance count was completed and documented by two (2) nurses during shift change. This was a random opportu...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected multiple residents
.
Based on record review and staff interview, the Quality Assessment and Assurance Committee failed to develop and implement appropriate plans of action to correct identified quality deficiencies. Thi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0885
(Tag F0885)
Could have caused harm · This affected multiple residents
.
Based on record review and staff interview, the facility failed to ensure documentation of notification to resident representatives when a staff member tested positive for COVID-19, beginning an out...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected multiple residents
.
Based on record review and staff interview the facility failed to ensure the nursing daily staff postings were incomplete and/or inaccurate in the area of census, facility name, and HPPD. This was a...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What safeguards are in place to prevent abuse and neglect?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 31% turnover. Below West Virginia's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: Federal abuse finding, 2 harm violation(s), $75,089 in fines. Review inspection reports carefully.
- • 62 deficiencies on record, including 2 serious (caused harm) violations. Ask about corrective actions taken.
- • $75,089 in fines. Extremely high, among the most fined facilities in West Virginia. Major compliance failures.
- • Grade F (15/100). Below average facility with significant concerns.
About This Facility
What is Bluestone's CMS Rating?
CMS assigns BLUESTONE HEALTH AND REHABILITATION an overall rating of 2 out of 5 stars, which is considered below average nationally. Within West Virginia, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Bluestone Staffed?
CMS rates BLUESTONE HEALTH AND REHABILITATION's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 31%, compared to the West Virginia average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Bluestone?
State health inspectors documented 62 deficiencies at BLUESTONE HEALTH AND REHABILITATION during 2022 to 2025. These included: 2 that caused actual resident harm, 59 with potential for harm, and 1 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Bluestone?
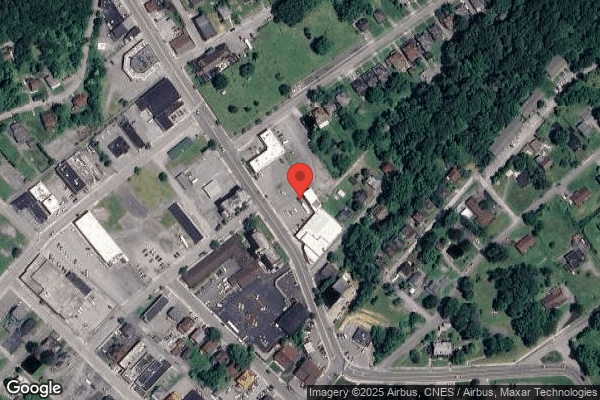
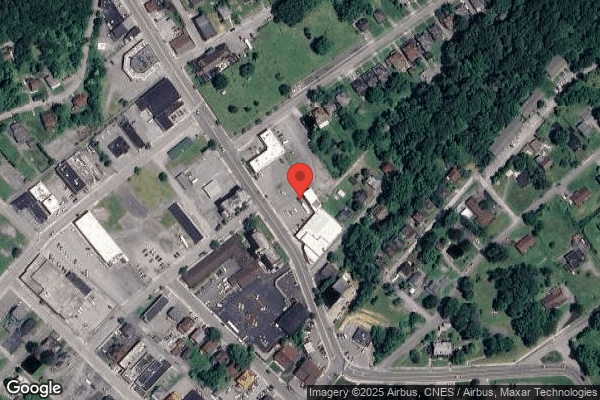
BLUESTONE HEALTH AND REHABILITATION is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by HILL VALLEY HEALTHCARE, a chain that manages multiple nursing homes. With 60 certified beds and approximately 58 residents (about 97% occupancy), it is a smaller facility located in BLUEFIELD, West Virginia.
How Does Bluestone Compare to Other West Virginia Nursing Homes?
Compared to the 100 nursing homes in West Virginia, BLUESTONE HEALTH AND REHABILITATION's overall rating (2 stars) is below the state average of 2.7, staff turnover (31%) is significantly lower than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Bluestone?
Based on this facility's data, families visiting should ask: "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the substantiated abuse finding on record and the below-average staffing rating.
Is Bluestone Safe?
Based on CMS inspection data, BLUESTONE HEALTH AND REHABILITATION has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in West Virginia. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Bluestone Stick Around?
BLUESTONE HEALTH AND REHABILITATION has a staff turnover rate of 31%, which is about average for West Virginia nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Bluestone Ever Fined?
BLUESTONE HEALTH AND REHABILITATION has been fined $75,089 across 6 penalty actions. This is above the West Virginia average of $33,830. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Bluestone on Any Federal Watch List?
BLUESTONE HEALTH AND REHABILITATION is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.