COMPLETE CARE AT DAWNVIEW LLC




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Complete Care at Dawnview LLC in Fort Ashby, West Virginia, has received a Trust Grade of F, indicating significant concerns about the facility. They rank #44 out of 122 nursing homes in the state, which places them in the top half, and #1 out of 2 in Mineral County, meaning there is only one other local option available. While the facility is showing an improving trend, with issues decreasing from 15 in 2023 to 11 in 2024, it still has a concerning staffing rating of 2 out of 5 stars and a high turnover of 61%, exceeding the state average of 44%. The facility has faced $46,232 in fines, which is higher than 86% of West Virginia facilities, suggesting ongoing compliance issues. Specific incidents raise red flags, such as a failure to protect a non-communicative resident from sexual abuse and a delay in reporting the allegation, which could affect all residents. Additionally, there were concerns about unsanitary conditions, with unclean wheelchairs observed in a foul state, indicating a lack of attention to hygiene. Despite some strengths like a decent quality measures rating of 4 out of 5 stars, the overall picture presents both significant weaknesses and areas needing improvement.
- Trust Score
- F
- In West Virginia
- #44/122
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 61% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ○ Average
- $46,232 in fines. Higher than 67% of West Virginia facilities. Some compliance issues.
- Skilled Nurses ○ Average
- Each resident gets 35 minutes of Registered Nurse (RN) attention daily — about average for West Virginia. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 40 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Near West Virginia average (2.7)
Meets federal standards, typical of most facilities
15pts above West Virginia avg (46%)
Frequent staff changes - ask about care continuity
Above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
13 points above West Virginia average of 48%
The Ugly 40 deficiencies on record
Nov 2024
8 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
b) Resident #38
-Resident Interview:
On 11/04/24 at 4:07 PM an interview was conducted with Resident #38 who reported that he had $100 missing from his lock box in his room. He reported that he wears ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed upon admission to identify a mental diagnosis for Resident #36 and related diagnoses of dementia and PTSD for Resident #42 on the PASARR...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0745
(Tag F0745)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview, the facility failed to follow the proper procedures to appoint a healthcare surrogat...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to maintain an accurate and complete record regarding transfer dates for Resident #28 and #36. This was true for two (2) of two (2) resi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation, record review and staff interview, the facility failed to provide a safe, clean, homelike environment regarding the storage of unclean wheelchairs. This was a random opportunity ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
b) Resident #18
Findings confirmed on 11/05/2024 by the Director of Nursing for Resident #18 included:
Hospice services were ordered for Resident #18 on 10/28/2024.
The Director of Nursing acknowled...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
Based on observation and staff interview, the facility failed to provide an accident and hazard free environment as possible by having a treatment cart which would not lock properly on three occasions...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, record review and staff interview, the facility failed to store and label food in accordance with professional standards for food service safety. This failed practice had the pot...
Read full inspector narrative →
Apr 2024
3 deficiencies
2 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** An IJ at F600 was called on 04/03/24 at 1:26 PM . A Plan of Correction (POC) was approved on 04/03/24 at 4:56 PM. The IJ was aba...
Read full inspector narrative →
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Report Alleged Abuse
(Tag F0609)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
An IJ at F609 was called on 04/03/24 at 1:26 PM . A Plan of Correction (POC) was approved on 04/03/24 at 4:56 PM. The IJ was a...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observations and staff interviews, the facility failed to ensure a resident maintained a continuous oxyg...
Read full inspector narrative →
Jan 2023
15 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
.
Based on observation, and staff interview, the facility failed to ensure care was provided in a manner to promote a resident's dignity. The facility failed to ensure staff covered a Foley catheter d...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
.
Based on observation, resident interview and staff interview, the facility failed to secure personal and medical information in a manner that protected a resident's health related information from t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
c) bedside table in disrepair
During an observation on 01/03/23 at 10:02 AM, Resident (R) #13 reported the trim around his bed...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
.
Based on observation, medical record review, and staff interview, the facility failed to develop and implement comprehensive person-centered care plans for residents with mental and psychosocial nee...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
.
Based on record review, staff and resident interview, the facility failed to provide treatment to a resident, in accordance to professional standards of practice, when the resident was assessed with...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
.
b) Resident #14
On 01/03/23 at 12:20 PM, based on staff observation, resident #14 observed with nasal cannula tubing running to her nose which had an attached tag which was dated for 11/27/22.
On 01...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0744
(Tag F0744)
Could have caused harm · This affected 1 resident
.
Based on observation, medical record review, family interview and staff interview, the facility failed to develop and implement comprehensive person-centered care plans for residents with dementia. ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
.
Based on policy review, staff interview and medical review, the facility failed to develop and maintain a policy for the monthly drug regimen review with time frames for the different steps in the p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
.
Based on medical record review and staff interview, the facility failed to ensure a resident's psychotropic medication was prescribed with an adequate indications for use. This is true for one of fi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
.
b) Resident #22
On 01/04/23 at 11:40 AM Resident #22 reported to staff in the resident council meeting that she had not received one or more doses of insulin just after Christmas, saying that she ha...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation and staff interview, the facility failed to ensure drugs and biologicals, used in the facility, were stor...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
.
b) Resident (R) #48
During an observation of medication administration on 01/04/23 at 08:10 AM, Quetiapine (Seroquel) 150 milligrams (mg) an atypical antipsychotic med used for treatment of schizoph...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
.
b) Resident (R) #48
During an observation of medication administration on 01/04/23 at 08:10 AM, Quetiapine (Seroquel) 150 milligrams (mg) an atypical antipsychotic med used for treatment of schizoph...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
.
Based on observation, medical record review, policy review and staff interview, the facility failed to maintain an effective infection control program. Residents were not given the opportunity to sa...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, staff interview, the facility failed to ensure residents' side rails were maintained in accordance with ...
Read full inspector narrative →
Sept 2021
14 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, record review, and staff interview, the facility failed to ensure resident dignity was protected. The facility failed to ensure the dignity of Resident #15, who was observed lyin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
.
Based on observation, resident interview and staff interview, the facility failed to ensure the call bell was in reach of Resident #11. This was a random opportunity for discovery. Resident identifi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
.
Based on resident interview, record review, and staff interview, the facility failed to ensure each resident had the opportunity to exercise his or her autonomy regarding things that were important ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on medical record review and staff interview, the facility failed to ensure a written Notice of Transfer / Discharge was...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on record review and staff interview the facility failed to accurately assess a Resident for oxygen use on the Minimum D...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
.
Based on record review and staff interview the facility failed to follow a physician order related to administration of a pain medication. This was true for one (1) of 16 sampled residents. Resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
.
Based on observation and staff interview the facility failed to provide incontinence care in a manner to promote comfort for the resident by failing to anchor Foley tubing to the resident's leg. Thi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
.
Based on observation, policy and procedure review and staff interview, the facility failed to provide tracheostomy care according to professional standards for one (1) of one (1) residents reviewed ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
.
Based on record review, review of policy and procedure, and staff interview, the facility failed to ensure monthly medication regimen reviews were completed on each resident by a licensed pharmacist...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected 1 resident
.
Based on observation and staff interview, the facility failed to maintain a geri chair for Resident #11 in a safe and sanitary manner. The geri chair arms did not have end cap closures and were cove...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
.
Based on observation and staff interview the facility failed to provide a safe and sanitary environment. This was a random opportunity for discovery. Resident identifier: #11. Facility census: 53.
F...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
.
Based on record review and staff interview, the facility failed to ensure five (5) of 16 residents reviewed during the long-term care survey process had a Physician Orders for Scope of Treatment (PO...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected multiple residents
.
Based on observation and staff interview the facility failed to ensure staffing information was available to all residents in the facility. This was a random opportunity for discovery. The failed pr...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY**
Based on observation and staff interview, the facility failed to perform proper hand hygiene during tracheotomy (trach) care; f...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 2 life-threatening violation(s), $46,232 in fines. Review inspection reports carefully.
- • 40 deficiencies on record, including 2 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • $46,232 in fines. Higher than 94% of West Virginia facilities, suggesting repeated compliance issues.
- • Grade F (26/100). Below average facility with significant concerns.
About This Facility
What is Complete Care At Dawnview Llc's CMS Rating?
CMS assigns COMPLETE CARE AT DAWNVIEW LLC an overall rating of 3 out of 5 stars, which is considered average nationally. Within West Virginia, this rating places the facility higher than 99% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Complete Care At Dawnview Llc Staffed?
CMS rates COMPLETE CARE AT DAWNVIEW LLC's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 61%, which is 15 percentage points above the West Virginia average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs. RN turnover specifically is 69%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Complete Care At Dawnview Llc?
State health inspectors documented 40 deficiencies at COMPLETE CARE AT DAWNVIEW LLC during 2021 to 2024. These included: 2 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death) and 38 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Complete Care At Dawnview Llc?
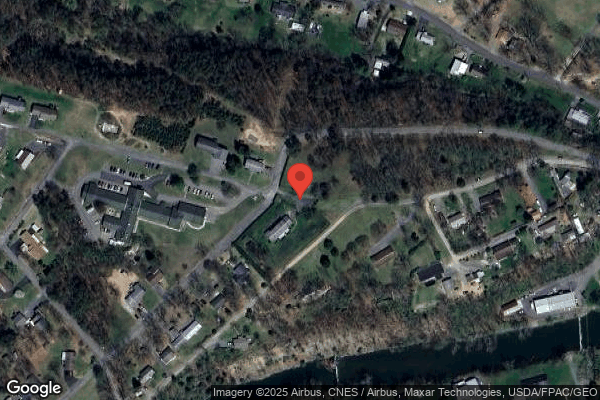
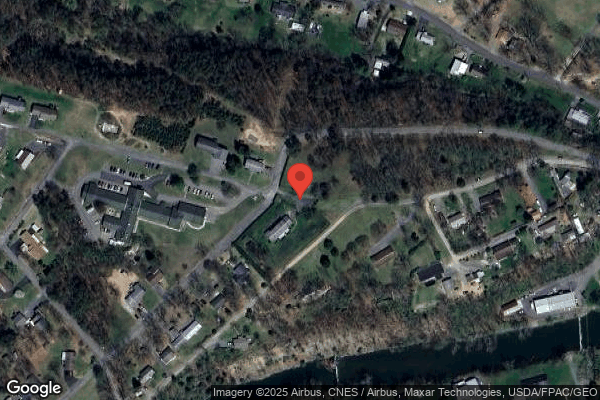
COMPLETE CARE AT DAWNVIEW LLC is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by COMPLETE CARE, a chain that manages multiple nursing homes. With 66 certified beds and approximately 57 residents (about 86% occupancy), it is a smaller facility located in FORT ASHBY, West Virginia.
How Does Complete Care At Dawnview Llc Compare to Other West Virginia Nursing Homes?
Compared to the 100 nursing homes in West Virginia, COMPLETE CARE AT DAWNVIEW LLC's overall rating (3 stars) is above the state average of 2.7, staff turnover (61%) is significantly higher than the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Complete Care At Dawnview Llc?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" These questions are particularly relevant given the facility's Immediate Jeopardy citations, the facility's high staff turnover rate, and the below-average staffing rating.
Is Complete Care At Dawnview Llc Safe?
Based on CMS inspection data, COMPLETE CARE AT DAWNVIEW LLC has documented safety concerns. Inspectors have issued 2 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility has a 3-star overall rating and ranks #1 of 100 nursing homes in West Virginia. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Complete Care At Dawnview Llc Stick Around?
Staff turnover at COMPLETE CARE AT DAWNVIEW LLC is high. At 61%, the facility is 15 percentage points above the West Virginia average of 46%. Registered Nurse turnover is particularly concerning at 69%. RNs handle complex medical decisions and coordinate care — frequent RN changes can directly impact care quality. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Complete Care At Dawnview Llc Ever Fined?
COMPLETE CARE AT DAWNVIEW LLC has been fined $46,232 across 2 penalty actions. The West Virginia average is $33,541. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Complete Care At Dawnview Llc on Any Federal Watch List?
COMPLETE CARE AT DAWNVIEW LLC is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.