MILETREE CENTER




Inspected within the last 6 months. Data reflects current conditions.
MileTree Center in Spencer, West Virginia, has a Trust Grade of C, which means it is average-neither the best nor the worst option available. It ranks #52 out of 122 facilities in the state, placing it in the top half, but it is the second and last facility in Roane County, indicating limited local choices. The facility's trend is improving, with a decrease in issues from 15 in 2024 to 10 in 2025. However, staffing is a notable concern, receiving only 1 out of 5 stars, with a turnover rate of 54%, which is concerning for continuity of care. Recent inspection findings included issues with infection control, where a staff member failed to change gloves after using the phone, and inadequate assessments of residents' dental needs, revealing that some residents had untreated dental problems. While the facility has strengths, such as good health inspection scores, these weaknesses in staffing and care planning are important to consider.
- Trust Score
- C
- In West Virginia
- #52/122
- Safety Record
- Low Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 54% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ⚠ Watch
- $3,250 in fines. Higher than 82% of West Virginia facilities, suggesting repeated compliance issues.
- Skilled Nurses ⚠ Watch
- Each resident gets only 25 minutes of Registered Nurse (RN) attention daily — below average for West Virginia. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 41 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Near West Virginia average (2.7)
Meets federal standards, typical of most facilities
Near West Virginia avg (46%)
Higher turnover may affect care consistency
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 41 deficiencies on record
Aug 2025
10 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to notify a resident's legal representative, the resident's attending physician, and the dietician about a worsening Moisture-Associated...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview, the facility failed to provide an accurate Minimum Data Set (MDS) including all high...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on documentation review and staff interview the facility failed to ensure resident's Pre-admission Screening reflected a c...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to develop a care plan including all diagnoses for Resident #5 and #6. This is true for two (2) of five (5) residents reviewed under unn...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to revise a care plan when a psychotropic medication was discontinued and an incorrect diagnosis was listed for Resident #5. This was tr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to follow a physician's order for Resident #4 for side effect monitoring and behavior monitoring of a psychotropic medication. This was ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected 1 resident
Based on record review, staff interview and observations, the facility failed to ensure a resident was served food in the correct consistency according to the National Dysphagia Diet Levels as ordered...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0809
(Tag F0809)
Could have caused harm · This affected 1 resident
Based on record review the facility failed to provide at least three (3) meals daily, at regular times comparable to normal mealtime in the community in accordance with resident needs, preferences, re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to provide an accurate and complete medical record for Resident #10's Physician's Order for Scope of Treatment (POST) form and two (2) t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation and staff interview, the facility failed to maintain an infection control program while serving from the tray line in the resident dining room. This was a random opportunity for d...
Read full inspector narrative →
Jul 2024
15 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
b) Resident #36
On 07/09/24 at 11:40 AM, an observation of Resident #36 was made during the noon meal. Occupational Therapist Aide (OTA) #71 was standing while feeding Resident #36.
On 07/09/24 at 11...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to notify the ombudsman of multiple transfers to the hospital for Resident #10. This was true for one (1) of one (1) residents reviewed ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to provide bed hold notices of multiple transfers to the hospital for Resident #10. This was true for one (1) of one (1) residents revie...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
MDS Data Transmission
(Tag F0640)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to transmit a Minimum Data Set (MDS) upon discharge of Resident #22. This was true for one (1) of one (1) residents reviewed under the c...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on record review, and staff interview, the facility failed to provide activities of daily living (ADL's) to maintain good personal hygiene for dependent residents. This is true for 0ne (1) of th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on resident interview, record review, and staff interview the facility failed to provide an ongoing activity program whi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
.
Based on observation, record review and staff interview, the facility failed to follow physician's orders regarding the release of restraints. This was true for two (2) of two (2) residents reviewed...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on resident interview, staff interview and record review the facility failed to provide pain management consistent with ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to maintain an accurate and complete record regarding a transfer for Resident #10. This was true for one (1) of one (1) residents review...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on resident interview, observation, staff interview and record review the facility failed to complete an accurate assess...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
.
Based on record review and staff interview, the facility failed to develop and/or implement a comprehensive care plan for Resident #10 regarding a diagnosis of diabetes mellitus, Resident #20 for th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, record review and staff interview the facility failed to maintain acceptable parameters of nutrition whi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, record review and staff interview, the facility failed to record temperatures for the medication refrigerator. This was a random opportunity for discovery. Facility Census: 57.
...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected multiple residents
.
Based on resident interview, record review and staff interview the facility failed to assist residents in obtaining routine and emergency dental care. This failed practice was found true for (1) one...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and staff interview, the facility failed to maintain an appropriate infection control program for storage o...
Read full inspector narrative →
Mar 2023
16 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on medical record review and staff interview, the facility failed to ensure Advance Directive paperwork was kept on Resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
b) Resident #41's History of Trauma / Post-Traumatic Stress Disorder (PTSD)
A medical record review, completed on 03/08/23 at ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
.
Based on resident interview, record review, and staff interview, the facility failed to ensure a resident with decision-making capacity was informed of the initial plan for delivery of care and serv...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on record review and interview, the facility failed to develop and/or implement a person-centered comprehensive care pla...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
.
c) Resident #41
During an interview on 03/06/23 at 11:01 AM, Resident #41 reported she could not recall being invited to care plan meetings.
A record review, completed on 03/07/23 at 7:45 PM, reve...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on policy review, record review and staff interview, the facility failed to provide care and services in a timely fashio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
.
Based on observation, staff interview, and policy review, the facility failed to maintain an effective Infection Control program. Staff failed to wear a face shield during tracheostomy (trach) care ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0699
(Tag F0699)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on record review and staff interview, the facility failed to ensure a resident who was a trauma survivor received trauma...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
.
Based on record review, staff interview, the facility failed to have an accurate diagnosis for a psychotropic medication. This was true for one (1) of five (5) residents reviewed for Unnecessary med...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected 1 resident
.
Based on Interview and record review the facility failed to ensure all qualified staff had their food handler's card. This has the ability to affect all Residents that get their nutrition from the k...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
.
Based on observation and staff interview, the facility failed to complete labeling and dates on refrigerator items in accordance with professional standards for food service safety related to storag...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
.
Based on medical record review and staff interview, the facility failed to ensure a complete and accurate medical record. A Physician Order for Scope of Treatment Form (POST Form) was not filled out...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected multiple residents
.
Based on observation and staff interview, the facility failed to honor resident privacy when leaving an elopement binder containing resident pictures and elopement risk identification forms in the f...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected multiple residents
.
Based on review of facility grievances, facility reportables, and staff interview, the facility failed to ensure that all allegations of neglect were reported within 24 hours to appropriate state ag...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
.
Based on record review and staff interview, the facility failed to ensure monthly pharmacy medication reviews were completed by the consulting pharmacist and reviewed by the physician. This was true...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
.
e) A-Wing Observation
On 03/07/23 at 12:20 PM, an observation was made of the lunch time meal service on the A-Wing of the facility was made for the first cart food delivery. There was no opportuni...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No major safety red flags. No abuse findings, life-threatening violations, or SFF status.
- • $3,250 in fines. Lower than most West Virginia facilities. Relatively clean record.
- • 41 deficiencies on record. Higher than average. Multiple issues found across inspections.
- • Grade C (58/100). Below average facility with significant concerns.
About This Facility
What is Miletree Center's CMS Rating?
CMS assigns MILETREE CENTER an overall rating of 3 out of 5 stars, which is considered average nationally. Within West Virginia, this rating places the facility higher than 99% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Miletree Center Staffed?
CMS rates MILETREE CENTER's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 54%, compared to the West Virginia average of 46%.
What Have Inspectors Found at Miletree Center?
State health inspectors documented 41 deficiencies at MILETREE CENTER during 2023 to 2025. These included: 41 with potential for harm.
Who Owns and Operates Miletree Center?
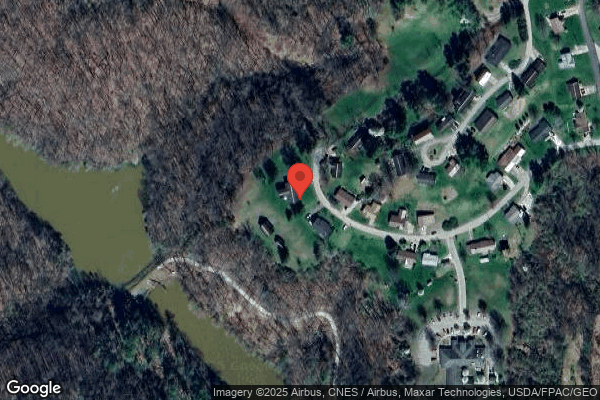
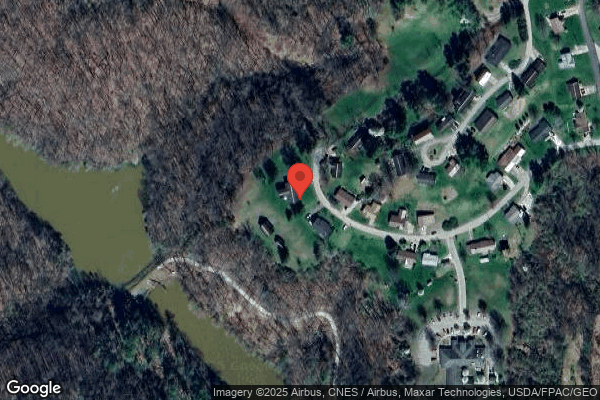
MILETREE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by GENESIS HEALTHCARE, a chain that manages multiple nursing homes. With 62 certified beds and approximately 57 residents (about 92% occupancy), it is a smaller facility located in SPENCER, West Virginia.
How Does Miletree Center Compare to Other West Virginia Nursing Homes?
Compared to the 100 nursing homes in West Virginia, MILETREE CENTER's overall rating (3 stars) is above the state average of 2.7, staff turnover (54%) is near the state average of 46%, and health inspection rating (4 stars) is above the national benchmark.
What Should Families Ask When Visiting Miletree Center?
Based on this facility's data, families visiting should ask: "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the below-average staffing rating.
Is Miletree Center Safe?
Based on CMS inspection data, MILETREE CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #1 of 100 nursing homes in West Virginia. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Miletree Center Stick Around?
MILETREE CENTER has a staff turnover rate of 54%, which is 8 percentage points above the West Virginia average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Miletree Center Ever Fined?
MILETREE CENTER has been fined $3,250 across 1 penalty action. This is below the West Virginia average of $33,111. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Miletree Center on Any Federal Watch List?
MILETREE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.